Abstract
Background
There are no prospective trials comparing the two main reconstructive options after colectomy for Ulcerative colitis, ileal pouch anal anastomosis and ileorectal anastomosis. An attempt on a randomized controlled trial has been made but after receiving standardized information patients insisted on choosing operation themselves.
Methods
Adult Ulcerative colitis patients subjected to colectomy eligible for both ileal pouch anastomosis and ileorectal anastomosis are asked to participate and after receiving standardized information the get to choose reconstructive method. Patients declining reconstruction or not considered eligible for both methods will be followed as controls. The CRUISE study is a prospective, non-randomized, multi-center, open-label, controlled trial on satisfaction, QoL, function, and complications between ileal pouch anal anastomosis and ileorectal anastomosis.
Discussion
Reconstruction after colectomy is a morbidity-associated as well as a resource-intensive activity with the sole purpose of enhancing function, QoL and patient satisfaction. The aim of this study is to provide the best possible information on the risks and benefits of each reconstructive treatment.
Trial registration
ClinicalTrials.gov Identifier: NCT05628701
Similar content being viewed by others
Introduction
Ulcerative Colitis (UC) is a chronic inflammatory bowel disease (IBD) restricted to the mucosa of the rectum and colon [1, 2]. The corner stone of UC treatment is pharmacological [3]. For about 10–15% of patients with UC medical treatment is not sufficient to induce/maintain remission or dysplasia/cancer occurs, and a colectomy will eventually be required [4, 5]. Although there are instances where a proctocolectomy with concomitant reconstruction is performed the recommended strategy for UC is usually a subtotal colectomy and reconstruction at a later stage [6, 7]. In a subtotal colectomy the distal colon is divided just above the promontory of the sacrum leaving a rectal remnant. The colon is removed and the terminal ileum is brought out through the abdominal wall as a stoma.
After subtotal colectomy there are four available options for patients. A reasonable option is to not proceed for further surgery and leave the rectum in place—the patient will live with a permanent ileostomy. Another option is the ileal pouch anal anastomosis (IPAA) where the rectum is removed and a pouch is created from the distal part of the ileum which is stapled or sutured to the anal canal or just above [8]. The IPAA is considered the gold standard reconstruction after subtotal colectomy [9]. A third option is the ileorectal anastomosis (IRA) where the rectum is left in place and the terminal ileum is stapled or handsewn to the top of the rectal remnant [10]. Then, for the rare instances that the patient is not suitable for either IPAA or IRA but still wants to avoid a stoma appliance, the Kock pouch is an option. The Kock pouch is a continent ileostomy that is actively emptied with a tube through the abdominal wall [11]. However, the Kock pouch is not commonly performed compared to the above options and will not be evaluated in this study. In a nationwide register study comparing Sweden and England only 46% and 33% of patients treated with colectomy received any reconstruction, respectively [12]. Whether the patients were offered reconstruction is unknown.
There are no randomized controlled trials (RCT) comparing IRA to IPAA. In a decision model using a Markov simulation in comparing IRA with IPAA in UC, the former was the preferred treatment option when quality-adjusted life-years were the outcome, while higher life-years was true for the latter [13]. An attempt of an RCT was conducted in Sweden led by Linköping starting late 2000 but after receiving adequate and standardized preoperative information the patients insisted on choosing surgical method, with a similar spread between the two options, and refused to be randomized. Therefore, the study was stopped. No protocol or results where, unfortunately, ever published from that RCT.
Method/design
Study objectives
To compare, in a prospective setting, patient satisfaction, QoL, function, and complications between IRA and IPAA and permanent stoma among patients with UC subjected to subtotal colectomy.
This study aims to answer what type of reconstruction, if any, UC-patients asks for following a colectomy, their satisfaction with the treatment, postoperative function and QoL. The results may have a large impact on future treatment recommendations.
Study design
The CRUISE study is a prospective, non-randomized, non-blinded, multi-center, controlled trial on satisfaction, QoL, function, and complications between IRA and IPAA and permanent stoma among adult UC patients subjected to subtotal colectomy. All adult UC patients scheduled for a subtotal colectomy will be asked for informed consent. The patients will then be presented standardized written and video recorded information on the available reconstructive options. If the patient meets the inclusion criteria, their preferred choice of IRA or IPAA will assign them to one of the study arms. Patients that do not meet the inclusion criteria or fulfill any of the exclusion criteria (e.g. not suitable for an IRA) or refrain reconstruction will be asked to participate as controls.
Endpoints
The primary endpoint is satisfaction with the choice of reconstructive method or permanent stoma. Secondary endpoints are QoL, sexual function, bowel function and complications.
Study population
The study population consists of all adult UC patients subjected to subtotal colectomy and eligible for both IRA and IPAA presenting at any of the participating centers.
Inclusion criteria are patients with UC aged between 18 and 60, scheduled for or have previously undergone subtotal colectomy and ileostomy. Patients should have sufficient rectal compliance and controllable inflammation in the rectal using topical 5-ASA only (Fig. 1).
Exclusion criteria are rectal inflammation of Mayo Score > 1 [14], poor sphincter function, perianal disease, uncertainty regarding UC diagnosis (IBD-U or possible Crohn’s disease), previous colorectal cancer or severe dysplasia (reported to the cancer registry), PSC diagnosis or > 2 year since subtotal colectomy (Fig. 1).
Sample size
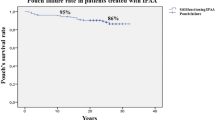
The only available study on patient satisfaction, our primary outcome, between IRA and IPAA reports 98% and 88% satisfaction for the methods respectively [15]. However, they only asked the IRA patients that still had their IRA in place after a mean of 11 years making it a little difficult to interpret. Another study compared QALYs between IRA and IPAA and reports a mean of 33.42 for IRA and a mean of 31.57 for IPAA [13]. With an estimated 3 SD (it was 2.8 for IRA and 4.5 for IPAA) and the significance level 0.05 and 80% power that difference would require 43 patients in each group to demonstrate a difference. Due to the mentioned shortcomings of the study comparing satisfaction we regard the latter study more relevant and decided to aim at a minimum of 50 patients in each group. Deliberately a little over the power estimation to avoid any effect of possible loss to follow-up.
Participating centers
Patients will be enrolled from three tertiary referral centers in Sweden (Linköping University hospital, Linköping, Sweden; Karolinska University hospital, Stockholm, Sweden; Sahlgrenska (Östra) University hospital, Gothenburg, Sweden) and one tertiary referral center in the UK (St Mark’s Hospital and Academic Institute, Harrow, UK).
Ethics
The study was approved by the regional ethics review board in Stockholm, Sweden (Dnr: 2017/124–31/2, 2018/2224–32) and The London Brent Research Ethics Committee (REC), UK (reference number: 18/LO/1190). The study is conducted in accordance with the Helsinki declaration and good clinical practice.
Trial registration
The protocol is registered and published at ClinicalTrials.gov Identifier: NCT05628701.
Study outline
Recruitment
After colectomy, patients will receive standardized written as well as oral information from a consultant regarding the collection of QoL measurements, functional scores and the different treatment modalities before being asked for consent to participate in the study. The patient will be prescribed topical 5-ASA according to local principles, usually 500–1000 mg twice daily. 3–6 months after the colectomy patients will be subjected to rectal endoscopic examination to assess rectal inflammation and compliance and sphincter function. Inflammation is assessed by Mayo score while the assessment of rectal compliance and sphincter function is based on patient history and the subjective evaluation by the responsible surgeon. Based on these factors it is determined if the patient is eligible for IRA as well as IPAA. Patients that are deemed eligible for both reconstructions, and otherwise fulfill inclusion criteria, will be analyzed in the study arms and will henceforth be referred to as the study arms in contrast to the controls (Fig. 2).
IRA
The IRA can be performed both as an open or laparoscopic procedure, of which the latter is more common and preferred in modern practice. The ileostomy is closed, and the neoterminal ileum is in most cases anastomosed to the tip of the rectal remnant in the abdomen using a circular transanal stapling device or in some cases a handsewn anastomosis will be performed. The reconstruction is rarely protected by a temporary diverting loop ileostomy.
IPAA
The IPAA can be performed both as an open or, preferably as a laparoscopic or robotic procedure. A trans-anal minimal invasive method (TaTME) may be used to facilitate proctectomy [16]. A pouch is constructed with the last part of the distal ileum and then anastomosed to the anal canal, or to a small rectal remnant, usually 1–2 cm in length, often referred to as the rectal cuff. The anastomosis is often created with a transanal circular stapling device but can also be hand sutured if needed. In most, but not all cases, the reconstruction is protected by a temporary loop ileostomy. In those instances, the loop closure, when bowel continuity is restored, will be considered the index operation in the study. Technical aspects of the creation of the pouch was at the discretion of the individual surgeon, however recorded in the clinical report form.
Controls
In order to obtain a comprehensive overview of all UC patients that undergo colectomy, patients that decline reconstruction or those eligible only for one method of reconstruction (e.g. only IPAA due to refractory proctitis) will be asked to participate as controls.
Failure
Patients converted from IRA to IPAA or from either reconstruction to a permanent ileostomy will be analyzed in an “intention-to-treat” manner.
Data collection
Instruments
General QoL will be assessed with the SF-36 form [17], IBD specific QoL with the SHS [18], bowel function with the Öresland score [19], female sexual function with the FSFI-6 [20], male sexual function with IIEF-5 [21]. In addition to these validated forms questions on whether or not the patients are satisfied with their choice of operation, would choose it again and recommend it to others and questions on fertility and reproduction will be asked. Early complications will be measured according to the Clavien-Dindo scale [22].
Data will also be obtained on smoking status, UC medication, age, indication for colectomy (chronic active disease/acute flare/dysplasia), BMI, endoscopic status in pouch/rectum, reoperations and for each operation: operation technique, operative time, bleeding, perioperative complications and hospital stay.
The data is collected and managed using REDCap (Research Electronic Data Capture) [23, 24] hosted at the Karolinska Institute, Stockholm, Sweden.
Time frame
Baseline data will be collected after colectomy for all patients. The reconstructed patients will then be followed at 2 months, 6 months, 1 year, 2 years and 5 years. Those patients that receive a loop ileostomy at reconstruction will also be followed 2 months after reconstruction before closure of the loop. For those patients the loop closure is considered the index operation. The patients that choose to (or are deemed to) keep their end ileostomies will be followed at 6 months, 1 year, 2 years and 5 years after colectomy (Fig. 3). The recruiting of patients started in March 2017.
Statistical analysis
Analysis will be conducted according to the intention-to-treat principal. The primary outcome satisfaction, a proportion, will be compared with chi-square test. For the primary outcome two-tailed tests will be applied since the null hypothesis is that there is no difference between the two reconstructive methods. Secondary outcomes assumed to be normally distributed will be compared between the two study arms using t-tests. Functional and QoL variables will be analyzed with mixed model ANOVA analysis. Time to failure will be analyzed with multivariate cox-regression analysis. Kaplan–Meier curves will be constructed and compared with log-rank tests. Repeating events, such as reoperations, will be analyzed with multivariate Poisson-regression.
There is no data and safety monitoring committee since all treatment is according to established practice. We do not plan to perform any interim analysis.
From a statistical point of view our choice of primary endpoint is not optimal because we have no reason to expect any difference between the two study arms. Still, to our opinion, this is the most important outcome measure.
Discussion
Reconstruction after colectomy is a morbidity-associated as well as a resource-intensive activity with the sole purpose of enhancing function, QoL and patient satisfaction. The actual disease has already been treated with the colectomy. Hence it is crucial to provide patients and care givers with the best possible information on the risks and benefits of each reconstructive treatment. They should be informed of what to expect if they choose to keep their end ileostomy permanently. There are no prospective head-to-head comparisons between IRA and IPAA in UC patients published.
The aspects to consider when evaluating a reconstruction after colectomy are early as well as late complications of the reconstruction, bowel function as well as urogenital and sexual function, quality of life (QoL), patient satisfaction as well as risk of failure and/or rectal cancer. There are also patient preferences which must be considered.
The IRA is easier to perform and does not require pelvic dissection, but instead the preserved rectum demands continuous topical medication and the risk for rectal cancer remains [25,26,27]. Hence, patients with an IRA needs to be surveilled for cancer and patients with increased colorectal cancer risk (i.e. patients with previous colorectal cancer or primary sclerosing cholangitis (PSC) are not considered suitable for IRA [25].
Early complications generally refers to complications within 30 days of surgery and they are most often graded according to the Clavien-Dindo scale [22]. In most studies a Clavien-Dindo score of 3b (a complication requiring intervention under general anesthesia) is considered to be of clinical significance. For IPAA, Clavien-Dindo scores of 3b or worse are reported in between 10–18% of patients [28, 29]. The only available report on early complications after IRA reports a 12.4% incidence of Clavien-Dindo 3a (a complication requiring intervention under local/regional anesthesia) or worse [30].
Considering late complications, pouchitis for IPAA is reported in between 36–48% of cases [31,32,33] with increasing cumulative numbers over time and up to 70% at 20 years follow up [33]. Some degree of proctitis at some point is reported in between 59–76% of IRA cases [34, 30]. There is to our knowledge only one report that specifies reoperation rates after IPAA and none on IRA. In the only available publication Wasmuth et al., reports a reoperation rate of 33% after a mean follow-up of 10 years and estimates that 52% of IPAA patients will have had at least one reoperation after 20 years [35].
Regarding bowel function, the main issues are continence, number of bowel movements, need to evacuate the bowel during nighttime and urgency to evacuate the bowel. For IRA, between three and six bowel movements per 24 h have been reported [30, 36,37,38,39] while for IPAA between five and seven bowel movements are reported [30, 40]. Need for night-time evacuation have been reported in 13–41% of IRA patients and 53% of IPAA patients. Among IRA patients, faecal incontinence is reported in 5% of patients and seepage or need for protective pads for 11–19% of patients [36, 39]. For the IPAA patient these figures are 14% and 32–39% [39, 41] Urgency is reported in 33–68% of IRA patients compared with 16–23% of IPAA patients [36, 39, 42, 43].
The pelvic dissection associated with IPAA constitutes a risk for impaired sexual function and impaired fecundity. Sexual function is described and compared in different ways in IPAA studies and the results are difficult to compare [44,45,46,47,48,49]. In female patients with an IPAA, sexual dysfunctions is reported in up to 50% of cases [44, 45] using validated sexual function forms, e.g. the FSFI [20, 21, 50, 51]. Fewer problems are reported among male IPAA patients and there are even reports of improved sexual function after surgery [52, 53]. There is, to our knowledge, very little published on the impact of IRA on sexual function [25]. However, Moreira et al., reported a tendency towards better sexual function among IRA patients compared to IPAA patients [39]. The actual reproductive rate is referred to as fecundity. Female UC patients are reported not to have impaired fertility compared to the general population [54]. Fecundity in female UC patients dropped from normal levels to 0.2 after IPAA [55] and infertility rates have been reported to increase from 20 to 63% after IPAA in a meta-analysis consisting of studies with both UC and FAP patients [56]. There is a reasonable hope that laparoscopic surgery may reduce the functional problems after IPAA but that remains to be further investigated [57, 58]. It was previously suggested that IRA does not reduce fecundity/fertility [59, 60] In contrast, Challine and colleagues recently compared fecundity between females subjected to IRA and IPAA and found no significant difference between the two [61]. This was in turn contradicted by the findings from the Swedish national cohort published by Druvefors [62]. In the French cohort they found reduced fecundity among females subjected to open surgery compared to laparoscopic regardless of IPAA or IRA [61] while the number of laparoscopic procedures was to few to render further analysis in the Swedish material [62].
In reconstructive surgery, the goal is to improve quality of life (QoL). Still, it is not obvious how to assess and compare QoL in surgery for UC [63]. In studies comparing IPAA to end ileostomy, an improved body image was reported among the IPAA patients but otherwise similar satisfaction and QoL [64,65,66,67]. There are several studies investigating how QoL develops over time in IPAA patients. It appears that the QoL of the IPAA patients is somewhat impaired in the first months after surgery but then improves [68, 69] and the QoL of the IPAA patients appears to be good in the long-term [42, 70]. Available studies comparing QoL in IRA to IPAA reports similar [15, 71] QoL between the two procedures but one study reported more urgency affecting work and dietary restrictions among the IRA patients [72].
Failure, defined as excisions or permanent deviation, is reported in between 4–9% of IPAA cases at 5 years and 7–19% at 10 years [30, 73,74,75,76,77,78] and reports with longer follow up indicates a continuing annual failure rate of around 2% even after 15 years [79]. The reported failure rates for IRA are 10–16% at 5 years and 24–31% at 10 years [30, 34, 39, 80, 81]. One should remember that after excising a poorly functioning IRA it is possible to construct an IPAA. However, the options after excising an IPAA are either a redo IPAA or an end ileostomy [82].
The obvious limitation with our study design is the lack of randomization. As mentioned in the introduction we have made an attempt to randomize between IRA and IPAA but after receiving detailed information, patients decline randomization and insist on choosing a reconstructive method themselves, with similar numbers opting for IRA and IPAA. We do not consider it a risk, but a fact, that some degree of selection bias will occur as some patients are more concerned regarding pelvic surgery, and its possible consequences, while others are more concerned by the need of anti-inflammatory medication, endoscopic surveillance and the risk of rectal cancer. We aim to minimize such effects with the provision of standardized information whenever possible. Because this is a multicenter study the same consultant cannot present the oral information to every patient. Instead, all patients will be shown the same information video by the consultant IBD Surgeon.
We do, however, see an upside to the lack of randomization. It is of interest to see what patients choose when presented with standardized information and if there are any demographic patterns in the choice of reconstructive method. Furthermore, we do not think that IRA will necessarily be a better choice than IPAA but rather it will be equally good in the selected cohorts eligible for either restorative procedure. Patient involvement may also increase the chance of a favorable outcome.
Another question that we hope to address is if there are any differences in the outcome of IPAA between the patients that were eligible for both IRA and IPAA and the patients that had IPAA as their only restorative option, i.e. will the level of proctitis affect the outcome of IPAA.
The multinational setting of the study will also allow for detection of possible differences in the attitude towards functional outcomes and complication patterns between the Swedish and English UC population. It will also improve the external validity of our study.
Conclusion
Because we have failed to enroll patients in an RCT we believe this is the best available way to compare the outcomes between IRA and IPAA. This design will also provide a good overview of the entire UC population that required colectomy.
Trial status
As of September 28, 2022, we have enrolled 37 IRA patients and 11 IPAA patients in the study arms and 23 IPAA and 18 ileostomy patients in the control arms.
Availability of data and materials
Not applicable, no data, only protocol.
Abbreviations
- IBD:
-
Inflammatory bowel disease
- UC:
-
Ulcerative Colitis
- CD:
-
Crohn’s disease
- IBD-U:
-
Inflammatory Bowel Disease-Unclassified
- QoL:
-
Quality of Life
- CI:
-
Continent ileostomy
- IPAA:
-
Ileal pouch anal anastomosis
- IRA:
-
Ileorectal anastomosis
- PSC:
-
Primary Sclerosing Cholangitis
- RCT:
-
Randomized controlled trial
- SF-36:
-
Short form 36 item
- SHS:
-
Short health scale
- FSFI:
-
Female Sexual Function Index
- IIEF:
-
International Index of Erectile Dysfunction
- TaTME:
-
Trans anal total mesorectal excision
References
Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ. Ulcerative colitis. Lancet. 2012;380(9853):1606–19.
Magro F, Rodrigues A, Vieira AI, Portela F, Cremers I, Cotter J, Correia L, Duarte MA, Tavares ML, Lago P, et al. Review of the disease course among adult ulcerative colitis population-based longitudinal cohorts. Inflamm Bowel Dis. 2012;18(3):573–83.
Raine T, Bonovas S, Burisch J, Kucharzik T, Adamina M, Annese V, et al. ECCO guidelines on therapeutics in ulcerative colitis: medical treatment. J Crohns Colitis. 2022;16(1):2–17.
Solberg IC, Lygren I, Jahnsen J, Aadland E, Hoie O, Cvancarova M, Bernklev T, Henriksen M, Sauar J, Vatn MH, et al. Clinical course during the first 10 years of ulcerative colitis: results from a population-based inception cohort (IBSEN Study). Scand J Gastroenterol. 2009;44(4):431–40.
Parragi L, Fournier N, Zeitz J, Scharl M, Greuter T, Schreiner P, Misselwitz B, Safroneeva E, Schoepfer AM, Vavricka SR, et al. Colectomy Rates in Ulcerative Colitis are Low and Decreasing: 10-year Follow-up Data From the Swiss IBD Cohort Study. J Crohns Colitis. 2018;12(7):811–8.
Risto A, Abdalla M, Myrelid P. Staging Pouch Surgery in Ulcerative Colitis in the Biological Era. Clin Colon Rectal Surg. 2022;35(1):58–65.
Zittan E, Wong-Chong N, Ma GW, McLeod RS, Silverberg MS, Cohen Z. Modified Two-stage Ileal Pouch-Anal Anastomosis Results in Lower Rate of Anastomotic Leak Compared with Traditional Two-stage Surgery for Ulcerative Colitis. J Crohns Colitis. 2016;10(7):766–72.
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J. 1978;2(6130):85–8.
Oresland T, Bemelman WA, Sampietro GM, Spinelli A, Windsor A, Ferrante M, Marteau P, Zmora O, Kotze PG, Espin-Basany E, et al. European evidence based consensus on surgery for ulcerative colitis. J Crohns Colitis. 2015;9(1):4–25.
Aylett SO. Conservative surgery in the treatment of ulcerative colitis. Br Med J. 1953;2(4850):1348–51.
Kock NG, Brevinge H, Philipson BM, Ojerskog B. Continent ileostomy. The present technique and long term results. Ann Chir Gynaecol. 1986;75(2):63–70.
Worley G, Nordenvall C, Askari A, Pinkney TD, Burns EM, Akbar A, Olén O, Ekbom A, Bottai M, Myrelid P, et al. Restorative Surgery after Colectomy for Ulcerative Colitis in England and Sweden: Observations from a Comparison of Nationwide Cohorts. Colorect Dis. 2018;20(9):804–12.
de Buck van Overstraeten A, Brar MS, Khorasani S, Dossa F, Myrelid P. Ileorectal Anastomosis Versus IPAA for the Surgical Treatment of Ulcerative Colitis: A Markov Decision Analysis. Dis Colon Rectum. 2020;63(9):1276–84.
Paine ER. Colonoscopic evaluation in ulcerative colitis. Gastroenterol Rep. 2014;2(3):161–8.
Tonelli F, Di Martino C, Giudici F. Could Total Colectomy with Ileorectal Anastomosis Be an Alternative to Total Proctocolectomy with Ileal Pouch-Anal Anastomosis in Selected Ulcerative Colitis Patients? Gastroenterol Res Pract. 2016;2016:5832743.
Lask A, Biebl M, Dittrich L, Fischer A, Adler A, Tacke F, Aigner F, Schmuck R, Chopra S, Knoop M, et al. Safety of transanal ileal pouch-anal anastomosis for ulcerative colitis: a retrospective observational cohort study. Patient Safety in Surgery. 2021;15(1):31.
McHorney CA, Ware JE Jr, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63.
Hjortswang H, Jarnerot G, Curman B, Sandberg-Gertzen H, Tysk C, Blomberg B, Almer S, Strom M. The Short Health Scale: a valid measure of subjective health in ulcerative colitis. Scand J Gastroenterol. 2006;41(10):1196–203.
Öresland T, Fasth S, Nordgren S, Hultén L. The clinical and functional outcome after restorative proctocolectomy. A prospective study in 100 patients. Int J Colorectal Dis. 1989;4(1):50–6.
Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): Cross-Validation and Development of Clinical Cutoff Scores. J Sex Marital Ther. 2005;31(1):1–20.
Rosen R, Cappelleri J, Smith M, Lipsky J, Peña B. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11(6):319–26.
Dindo D, Demartines N, Clavien P-A. Classification of Surgical Complications. Ann Surg. 2004;240(2):205–13.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Myrelid P, Oresland T. A reappraisal of the ileo-rectal anastomosis in ulcerative colitis. J Crohns Colitis. 2015;9(6):433–8.
Abdalla M, Landerholm K, Andersson P, Andersson RE, Myrelid P. Risk of Rectal Cancer After Colectomy for Patients With Ulcerative Colitis: A National Cohort Study. Clin Gastroenterol Hepatol. 2017;15(7):1055-1060.e1052.
Uzzan M, Kirchgesner J, Oubaya N, Amiot A, Gornet JM, Seksik P, Nancey S, Cotte E, Allez M, Boschetti G, et al. Risk of Rectal Neoplasia after Colectomy and Ileorectal Anastomosis for Ulcerative Colitis. J Crohns Colitis. 2017;11(8):930–5.
Hermanson M, Bengtson J, Croix HDL, Lindholm E, Block M. Ileal pouch-anal anastomosis; 18 years of experience and outcomes across two generations of surgeons at a tertiary center in Sweden. Scand J Gastroenterol. 2022;57(4):401–5.
Baker DM, Folan AM, Lee MJ, Jones GL, Brown SR, Lobo AJ. A systematic review and meta-analysis of outcomes after elective surgery for ulcerative colitis. Colorectal Dis. 2021;23(1):18–33.
Andersson P, Norblad R, Soderholm JD, Myrelid P. Ileorectal anastomosis in comparison with ileal pouch anal anastomosis in reconstructive surgery for ulcerative colitis–a single institution experience. J Crohns Colitis. 2014;8(7):582–9.
Penna C, Dozois R, Tremaine W, Sandborn W, LaRusso N, Schleck C, Ilstrup D. Pouchitis after ileal pouch-anal anastomosis for ulcerative colitis occurs with increased frequency in patients with associated primary sclerosing cholangitis. Gut. 1996;38(2):234–9.
Fazio VW, Kiran RP, Remzi FH, Coffey JC, Heneghan HM, Kirat HT, Manilich E, Shen B, Martin ST. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013;257(4):679–85.
Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR. Results at up to 20 years after ileal pouch–anal anastomosis for chronic ulcerative colitis. Br J Surg. 2007;94:333–40.
Pastore RL, Wolff BG, Hodge D. Total abdominal colectomy and ileorectal anastomosis for inflammatory bowel disease. Dis Colon Rectum. 1997;40(12):1455–64.
Wasmuth HH, Trano G, Endreseth B, Rydning A, Wibe A, Myrvold HE. Long-term surgical load in patients with ileal pouch-anal anastomosis. Colorectal Dis. 2009;11(7):711–8.
Börjesson L, Lundstam U, Öresland T, Brevinge H, Hultén L. The place for colectomy and ileorectal anastomosis: a valid surgical option for ulcerative colitis? Tech Coloproctol. 2006;10(3):237–41 (discussion 241).
Gallone L, Olmi L, Marchetti V. Use of topical rectal therapy to preserve the rectum in surgery of ulcerative colitis. World J Surg. 1980;4(5):609–13.
Elton C, Makin G, Hitos K, Cohen CR. Mortality, morbidity and functional outcome after ileorectal anastomosis. Br J Surg. 2003;90(1):59–65.
da Luz MA, Kiran RP, Lavery I. Clinical outcomes of ileorectal anastomosis for ulcerative colitis. Br J Surg. 2010;97(1):65–9.
de Zeeuw S, Ahmed Ali U, Donders RA, Hueting WE, Keus F, van Laarhoven CJ. Update of complications and functional outcome of the ileo-pouch anal anastomosis: overview of evidence and meta-analysis of 96 observational studies. Int J Colorectal Dis. 2012;27(7):843–53.
Farouk R, Pemberton JH, Wolff BG, Dozois RR, Browning S, Larson D. Functional outcomes after ileal pouch-anal anastomosis for chronic ulcerative colitis. Ann Surg. 2000;231(6):919–26.
Berndtsson I, Lindholm E, Oresland T, Borjesson L. Long-term outcome after ileal pouch-anal anastomosis: function and health-related quality of life. Dis Colon Rectum. 2007;50(10):1545–52.
Block M, Börjesson L, Lindholm E, Öresland T. Pouch design and long-term functional outcome after ileal pouch–anal anastomosis. Br J Surg. 2009;96:527–32.
van Balkom KA, Beld MP, Visschers RG, van Gemert WG, Breukink SO. Long-term results after restorative proctocolectomy with ileal pouch-anal anastomosis at a young age. Dis Colon Rectum. 2012;55(9):939–47.
Ogilvie JW Jr, Goetz L, Baxter NN, Park J, Minami S, Madoff RD. Female sexual dysfunction after ileal pouch-anal anastomosis. Br J Surg. 2008;95(7):887–92.
Berndtsson I, Oresland T, Hulten L. Sexuality in patients with ulcerative colitis before and after restorative proctocolectomy: a prospective study. Scand J Gastroenterol. 2004;39(4):374–9.
Koivusalo A, Pakarinen MP, Natunen J, Ashorn M, Rintala RJ, Sipponen T, Kolho KL. Sexual functions in adulthood after restorative proctocolectomy for paediatric onset ulcerative colitis. Pediatr Surg Int. 2009;25(10):881–4.
Larson DW, Davies MM, Dozois EJ, Cima RR, Piotrowicz K, Anderson K, Barnes SA, Harmsen WS, Young-Fadok TM, Wolff BG, et al. Sexual function, body image, and quality of life after laparoscopic and open ileal pouch-anal anastomosis. Dis Colon Rectum. 2008;51(4):392–6.
Hueting WE, Gooszen HG, van Laarhoven CJ. Sexual function and continence after ileo pouch anal anastomosis: a comparison between a meta-analysis and a questionnaire survey. Int J Colorectal Dis. 2004;19(3):215–8.
Rosen CBJHSLR. The Female Sexual Function Index (FSFI): A Multidimensional Self-Report Instrument for the Assessment of Female Sexual Function. J Sex Marital Ther. 2000;26(2):191–208.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–30.
Lindsey I, George BD, Kettlewell MG, Mortensen NJ. Impotence after mesorectal and close rectal dissection for inflammatory bowel disease. Dis Colon Rectum. 2001;44(6):831–5.
Gorgun E, Remzi FH, Montague DK, Connor JT, O’Brien K, Loparo B, Fazio VW. Male sexual function improves after ileal pouch anal anastomosis. Colorectal Dis. 2005;7(6):545–50.
Korelitz BI. Inflammatory bowel disease and pregnancy. Gastroenterol Clin North Am. 1998;27(1):213–24.
Ording Olsen K, Juul S, Berndtsson I, Oresland T, Laurberg S. Ulcerative colitis: female fecundity before diagnosis, during disease, and after surgery compared with a population sample. Gastroenterology. 2002;122(1):15–9.
Rajaratnam SG, Eglinton TW, Hider P, Fearnhead NS. Impact of ileal pouch-anal anastomosis on female fertility: meta-analysis and systematic review. Int J Colorectal Dis. 2011;26(11):1365–74.
Beyer-Berjot L, Maggiori L, Birnbaum D, Lefevre JH, Berdah S, Panis Y. A total laparoscopic approach reduces the infertility rate after ileal pouch-anal anastomosis: a 2-center study. Ann Surg. 2013;258(2):275–82.
Bartels SA, D’Hoore A, Cuesta MA, Bensdorp AJ, Lucas C, Bemelman WA. Significantly increased pregnancy rates after laparoscopic restorative proctocolectomy: a cross-sectional study. Ann Surg. 2012;256(6):1045–8.
Mortier PE, Gambiez L, Karoui M, Cortot A, Paris JC, Quandalle P, Colombel JF. Colectomy with ileorectal anastomosis preserves female fertility in ulcerative colitis. Gastroenterol Clin Biol. 2006;30(4):594–7.
Olsen KO, Juul S, Bulow S, Järvinen HJ, Bakka A, Björk J, Öresland T, Laurberg S. Female fecundity before and after operation for familial adenomatous polyposis. Br J Surg. 2003;90(2):227–31.
Challine A, Voron T, O'Connell L, Chafai N, Debove C, Collard M, et all. Does An Ileo-anal anastomosis decrease the rate of successful pregnancy compared to an Ileorectal anastomosis? a national study of 1,491 patients. Ann Surg 2022. In print. https://doi.org/10.1097/sla.0000000000005569.
Druvefors E, Myrelid P, Andersson RE, Landerholm K. P180 Ileorectal anastomosis preserves female fertility after colectomy in Ulcerative Colitis. Journal of Crohn’s and Colitis. 2023;17(Supplement_1):i334–5.
Murphy PB, Khot Z, Vogt KN, Ott M, Dubois L. Quality of Life After Total Proctocolectomy With Ileostomy or IPAA: A Systematic Review. Dis Colon Rectum. 2015;58(9):899–908.
Jimmo B, Hyman NH. Is ileal pouch-anal anastomosis really the procedure of choice for patients with ulcerative colitis? Dis Colon Rectum. 1998;41(1):41–5.
Pemberton JH, Phillips SF, Ready RR, Zinsmeister AR, Beahrs OH. Quality of life after Brooke ileostomy and ileal pouch-anal anastomosis. Comparison of performance status. Ann Surg. 1989;209(5):620–6 (discussion 626-628).
Wang JY, Hart SL, Wilkowski KS, Lee JW, Delmotte EC, del Rosario KM, del Rosario AS, Varma MG. Gender-specific differences in pelvic organ function after proctectomy for inflammatory bowel disease. Dis Colon Rectum. 2011;54(1):66–76.
Camilleri-Brennan J, Munro A, Steele RJ. Does an ileoanal pouch offer a better quality of life than a permanent ileostomy for patients with ulcerative colitis? J Gastrointest Surg. 2003;7(6):814–9.
Muir AJ, Edwards LJ, Sanders LL, Bollinger RR, Koruda MJ, Bachwich DR, Provenzale D. A prospective evaluation of health-related quality of life after ileal pouch anal anastomosis for ulcerative colitis. Am J Gastroenterol. 2001;96(5):1480–5.
Berndtsson I, Oresland T. Quality of life before and after proctocolectomy and IPAA in patients with ulcerative proctocolitis - a prospective study. Colorectal Dis. 2003;5(2):173–9.
Lorenzo G, Maurizio C, Maria LP, Tanzanu M, Silvio L, Mariangela P, Gilberto P. Ileal pouch-anal anastomosis 20 years later: is it still a good surgical option for patients with ulcerative colitis? Int J Colorectal Dis. 2016;31(12):1835–43.
Pica R, Cassieri C, Pronio AM, Zippi M, Avallone EV, Montesani C, Occhigrossi G, Paoluzi P. Quality of life in ulcerative colitis patients treated medically versus patients undergoing surgery. Eur Rev Med Pharmacol Sci. 2014;18(5):693–8.
da Luz MA, Lavery IC. Ileorectal anastomosis and proctocolectomy with end ileostomy for ulcerative colitis. Clin Colon Rectal Surg. 2010;23(4):269–73.
Fazio VW, Tekkis PP, Remzi F, Lavery IC, Manilich E, Connor J, Preen M, Delaney CP. Quantification of risk for pouch failure after ileal pouch anal anastomosis surgery. Ann Surg. 2003;238(4):605–14 (discussion 614-607).
Lepisto A, Luukkonen P, Jarvinen HJ. Cumulative failure rate of ileal pouch-anal anastomosis and quality of life after failure. Dis Colon Rectum. 2002;45(10):1289–94.
Tulchinsky H, Hawley PR, Nicholls J. Long-term failure after restorative proctocolectomy for ulcerative colitis. Ann Surg. 2003;238(2):229–34.
Tekkis PP, Lovegrove RE, Tilney HS, Smith JJ, Sagar PM, Shorthouse AJ, Mortensen NJ, Nicholls RJ. Long-term failure and function after restorative proctocolectomy - a multi-centre study of patients from the UK National Ileal Pouch Registry. Colorectal Dis. 2010;12(5):433–41.
Leowardi C, Hinz U, Tariverdian M, Kienle P, Herfarth C, Ulrich A, Kadmon M. Long-term outcome 10 years or more after restorative proctocolectomy and ileal pouch-anal anastomosis in patients with ulcerative colitis. Langenbecks Arch Surg. 2010;395(1):49–56.
Ikeuchi H, Uchino M, Matsuoka H, Bando T, Matsumoto T, Tomita N, Syoji Y, Kusunoki M, Yamamura T, Utsunomiya J. Surgery for ulcerative colitis in 1,000 patients. Int J Colorectal Dis. 2010;25(8):959–65.
Kiran RP, El-Gazzaz G, Remzi FH, Church JM, Lavery IC, Hammel J, Fazio VW. Influence of age at ileoanal pouch creation on long-term changes in functional outcomes. Colorectal Dis. 2011;13(2):184–90.
Lepistö A, Järvinen HJ. Fate of the rectum after colectomy with ileorectal anastomosis in ulcerative colitis. Scand J Surg SJS Offic Organ Finnish Surg Soc Scand Surg Soc. 2005;94(1):40–2.
Uzzan M, Cosnes J, Amiot A, Gornet JM, Seksik P, Cotte E, Tiret E, Panis Y, Treton X. Long-term Follow-up After Ileorectal Anastomosis for Ulcerative Colitis: A GETAID/GETAID Chirurgie Multicenter Retrospective Cohort of 343 Patients. Ann Surg. 2017;266(6):1029–34.
Landerholm K, Abdalla M, Myrelid P, Andersson RE. Survival of ileal pouch anal anastomosis constructed after colectomy or secondary to a previous ileorectal anastomosis in ulcerative colitis patients: a population-based cohort study. Scand J Gastroenterol 2017:52(5):531–35.
Acknowledgements
Mr Guy Worley made considerable contributions in the start-up of the study in the UK.
Funding
Open access funding provided by Linköping University. The study was financed by grants from: The Swedish state under the agreement between the Swedish government and the county councils (the ALF-agreement), The Bengt Ihre research fund and the “Magtarmfonden” research fund. None of the funders have had any role in the current study.
Author information
Authors and Affiliations
Contributions
Guarantor: Mr Risto had full access to all of the data in the study and takes responsibility for the integrity study. Study concept and design: All co-authors. Interpretation of results: All co-authors. Drafting of the manuscript: Risto. Figures and tables: Risto and Nordenvall. Critical revision of the manuscript for important intellectual content: All co-authors. Final approval of the version to be submitted: All co-authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the regional ethics review board in Stockholm, Sweden (Dnr: 2017/124–31/2, 2018/2224–32) and The London Brent Research Ethics Committee (REC), UK (18/LO/1190). Written consent is/will be signed by all participating patients.
Consent for publication
Not applicable, no individual data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Risto, A., Nordenvall, C., Deputy, M. et al. Colectomy reconstruction for ulcerative colitis in Sweden and England: a multicenter prospective comparison between ileorectal anastomosis and ileal pouch-anal anastomosis after colectomy in patients with ulcerative colitis. (CRUISE-study). BMC Surg 23, 96 (2023). https://doi.org/10.1186/s12893-023-01984-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-01984-x