Abstract
Background
The Dutch Working Party on Antibiotic Policy (SWAB) in collaboration with relevant professional societies, has updated their evidence-based guidelines on empiric antibacterial therapy of sepsis in adults.
Methods
Our multidisciplinary guideline committee generated ten population, intervention, comparison, and outcome (PICO) questions relevant for adult patients with sepsis. For each question, a literature search was performed to obtain the best available evidence and assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system. The quality of evidence for clinically relevant outcomes was graded from high to very low. In structured consensus meetings, the committee formulated recommendations as strong or weak. When evidence could not be obtained, recommendations were provided based on expert opinion and experience (good practice statements).
Results
Fifty-five recommendations on the antibacterial therapy of sepsis were generated. Recommendations on empiric antibacterial therapy choices were differentiated for sepsis according to the source of infection, the potential causative pathogen and its resistance pattern. One important revision was the distinction between low, increased and high risk of infection with Enterobacterales resistant to third generation cephalosporins (3GRC-E) to guide the choice of empirical therapy. Other new topics included empirical antibacterial therapy in patients with a reported penicillin allergy and the role of pharmacokinetics and pharmacodynamics to guide dosing in sepsis. We also established recommendations on timing and duration of antibacterial treatment.
Conclusions
Our multidisciplinary committee formulated evidence-based recommendations for the empiric antibacterial therapy of adults with sepsis in The Netherlands.
Similar content being viewed by others
Background
Sepsis is currently defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [1,2,3,4]. Sepsis and septic shock are common reasons for intensive care unit (ICU) admission and associated with high mortality rates, even at long-term follow-up [5,6,7,8,9,10,11,12]. Worldwide in 2017, nearly 50 million cases of sepsis were recorded resulting in 11 million sepsis-related deaths [13]. In the Netherlands the estimated annual number of admissions for severe sepsis in Dutch ICU’s was 7700–9500 in 2004 [14]. The incidence of sepsis may have risen in recent decennia, possibly due to ageing and increasing numbers of immunocompromised patients [6, 8, 15]. Antibacterial treatment is an essential part of effective sepsis management. Inappropriate or delayed antibacterial treatment in patients with sepsis and septic shock have been associated with increased morbidity and mortality [16,17,18,19,20,21].
The Dutch Working Party on Antibiotic Policy (SWAB), initiated by the Dutch Association of Internal Medicine, the Dutch Society for Medical Microbiology and the Dutch Association of Hospital Pharmacists, coordinates activities in the Netherlands intending to optimize antibiotic use, to contain the development of antimicrobial resistance, and to limit the costs of antibiotic use. The general objective of the SWAB sepsis guidelines is to guide medical professionals in the empirical antibacterial treatment for adults with sepsis and septic shock in hospitals. The current guidelines on empirical antibacterial therapy of sepsis in the Netherlands is an update of the SWAB sepsis guidelines published in 2010 [22].
Providing evidence-based recommendations on empirical antibacterial therapy in sepsis is challenging. There is considerable heterogeneity among sepsis studies as to included patients (comorbidities, disease severity, source of infection), microbiological characteristics (availability of culture results, pathogens involved, local antimicrobial resistance), interventions (drug dosing, source control, timing of treatment) as well as to the outcome parameters assessed. In particular, antimicrobial resistance is much lower in the Netherlands than in other countries [23,24,25]. Another important consideration is that most trials and meta-analyses on antibacterial therapy are not powered to assess relevant outcomes such as adverse events and the development of antimicrobial resistance [26,27,28].
In this publication, we summarize the most important literature and changes in recommendations for the antibacterial treatment of adults with sepsis.
Methods
For a complete description of the methodology of the guideline, we refer to the original document. In short, the guideline was written according to the Appraisal of Guidelines for Research and Evaluation (AGREE II) instrument [29].
A multidisciplinary guideline committee consisting of experts delegated from relevant professional societies followed a guideline development process comparable to that of the Infectious Diseases Society of America (IDSA), which includes a systematic method of grading both the quality of evidence (very low, low, moderate, and high) and the strength of the recommendation (weak or strong) [30]. We aimed to provide an overview of the quality of available evidence and give evidence-based recommendations for antibacterial treatment of sepsis in adults (≥ 18 years old). We restricted the guideline to the most important causes of sepsis, i.e., pneumonia, abdominal infections, urinary tract infections, complicated skin and soft tissue infections, as well as to sepsis in general or of (yet) unknown origin. Neutropenic sepsis, sepsis due to viral or fungal infections, sepsis in patients with prosthetic material or long term central venous catheters, sepsis due to osteomyelitis, meningitis, mediastinitis and endocarditis and children were outside the scope of the guideline.
The committee generated ten population, intervention, comparison, and outcomes (PICO) questions relevant for adult patients with sepsis in the Netherlands (Table 1). For each question we reviewed existing national and international guidelines and performed additional pragmatic literature searches. For evidence on drug resistance in the Netherlands, the guideline committee used surveillance data from 2017 in the NethMap annual report 2018 [23]. Reports of the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guided the interpretation of susceptibility test results [31].
Included guidelines and studies were assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system. We graded the quality of evidence for clinically relevant outcomes from high to very low. In structured consensus meetings, the committee formulated recommendations as strong or weak. When evidence could not be obtained, recommendations could be provided based on opinions and experiences (good practice statements).
The draft guideline was submitted to the members of relevant professional societies for external review. The guideline working group adjusted the guideline according to comments in the external review through group discussion. Both comments and responses of the committee are available at www.swab.nl. The final version received formal approval from the SWAB executive board.
Results
Causative bacterial pathogens in sepsis and their antibiotic susceptibility
Which bacteria are most frequently isolated from patients with sepsis in The Netherlands?
In the Netherlands, the most commonly cultured pathogens in blood cultures are coagulase-negative staphylococci (CNS) (34%), Escherichia coli (23%), Staphylococcus aureus (10%), Klebsiella pneumonia (4%) and Enterococcus faecalis/faecium (5%) [23]. In patients with sepsis and ICU admission, gram-negative pathogens were more likely to be involved [32, 33]. Of note, Acinetobacter baumannii was not an important cause of sepsis due to hospital-acquired pneumonia (HAP) or ventilator-associated pneumonia (VAP) as it was hardly isolated in respiratory cultures of hospitalized patients in Dutch surveillance data [23]. Reported pathogens in sepsis due to intra-abdominal infections were E. coli, enteric anaerobes, other Enterobacterales, Enterococcus spp. and Streptococcus spp. [34]. In central line-associated bloodstream infections (CLABSI), the most reported pathogens were CNS, gram-negative bacteria (fermenters and non-fermenters), S. aureus, Enterococcus spp. and Candida albicans [35, 36].
What are the resistance patterns of the most frequently isolated bacteria in patients with sepsis in The Netherlands?
A Dutch study among 648 intensive care unit (ICU) patients with non-pneumonia derived sepsis reported microbiological culture results of (surveillance) samples obtained two days before until two days after ICU admission. Resistance percentages of pathogenic bacteria in these patients were 10% for 3rd generation cephalosporins, 8% for ciprofloxacin, 6% for gentamicin, 2% for piperacillin-tazobactam, and 0.5% for meropenem [37]. Dutch surveillance data showed that the rate of extended-spectrum beta-lactamase (ESBL)-producing bacteria in blood cultures has increased over the past years. In 2017, 6% of E. coli and 10% of K. pneumoniae blood isolates were resistant to 3rd generation cephalosporins (Table 2) [23]. The prevalence of carbapenem resistance in all E. coli and K. pneumoniae isolates was stable over five years and low at 0.03% and 0.42%. The risk of methicillin-resistant S. aureus (MRSA) bacteraemia has remained stable over the last ten years and low at 1% of all S. aureus bacteraemias [23].
Which patients are at risk for sepsis due to third-generation cephalosporin-resistant Enterobacterales (3GCR-E) or Pseudomonas aeruginosa in the Netherlands?
One systematic review summarized colonization and risk of subsequent bacteraemia with ESBL-producing Enterobacterales in patients with solid and haematological malignancies [38]. Patients with known colonization with an ESBL-producing Enterobacterales as detected by surveillance cultures (mostly at admission) were 13 times more likely to develop a bacteraemia with these pathogens compared to patients not that were not colonized. Two specific risk factors for sepsis due to 3GCR-E have been externally validated by in a Dutch retrospective study of 9442 episodes in which blood cultures were drawn and iv antibacterial therapy was started [39]. Positive predictive values (PPV) of prior (90 days and 1 year) colonization with 3GCR-E were 7.4% and 6.1% for predicting bacteraemia and 34.4% and 28.2% for predicting any culture-positive infection with 3GCR-E. PPVs of prior (30 days) treatment with cephalosporins or fluoroquinolones were 1.3% for predicting bacteraemia and 6.9% for predicting any culture-positive infection with 3GCR-E. No other studies were found that externally validated predictors for sepsis due to 3GCR-E or P. aeruginosa.
Based on currently available evidence, we concluded that prior (1 year) infection or colonization is the strongest and most common risk factor predicting subsequent infection with 3GCR-E [38, 40,41,42]. It was challenging to provide general recommendations on other risk factors that should be taken into account to guide the decision to start empirical antibiotic therapy in sepsis directed against 3GCR-E or P. aeruginosa. Until high-quality and externally validated prediction rules are available, the guideline committee recommends that the following factors should be taken into account to decide if empirical antibacterial therapy against 3GCR-E in patients with sepsis is appropriate: local prevalence of 3GCR-E [43], whether the sepsis is hospital-acquired [40, 44, 45], and to a lesser extent healthcare-associated, versus community-acquired, whether the patient received prior (2 months) antibiotic treatment and whether or not the patient receives selective decontamination of the digestive tract (SDD) [40, 45, 46]. It is essential to realize the limitations of using risk factors for the decision to treat for 3GCR-E, to weigh potential risk factors against the associated risk of overtreatment and to ensure antibiotic de-escalation if possible.
In addition, the committee regarded the high colonization rate with highly resistant micro-organisms (HRMO) in travellers from highly endemic countries such as the Indian subcontinent as another risk factor to consider in the choice of empirical antibiotic therapy in patients with sepsis. As many travellers will not be colonized anymore after several months, we suggest including three months prior travel to highly endemic countries in the individual risk assessment (https://resistancemap.cddep.org). The committee felt that the risk of 3GCR-E involvement to be high in patients with sepsis recently hospitalized abroad for > 24 h. There is no strong evidence to support this statement, but it is in accordance to national infection prevention guidelines on which patients to screen for HRMO [47]. We therefore included this as a separate suggestion.
Regarding P. aeruginosa, the committee suggests to empirically start targeted treatment in patients with sepsis when prior (1-year) cultures showed P. aeruginosa. In addition, we suggest covering P. aeruginosa in patients with sepsis due to HAP/VAP or suspected infected central venous catheter (CVC) infection.
Empirical antibacterial therapy in sepsis
What is the importance of appropriate empirical therapy in patients with sepsis?
The importance of appropriate empirical antibacterial therapy in patients with sepsis has been supported by systematic reviews of observational studies only [21, 48, 49]. The reported effect has been consistent and includes reduced mortality, costs and length of hospital stay, although with considerable heterogeneity between studies [21, 48, 49]. Very low quality evidence showed a trend towards improved outcomes of appropriate empirical therapy in patients with sepsis due to HRMO and anaerobic pathogens [43, 50,51,52]. For Enterococcus spp, empirical treatment strategies in community-acquired intra-abdominal infections showed no difference in clinical outcomes comparing antibiotic regimens with and without activity against Enterococci [52]. There is no clear evidence to support or refute empirical treatment of enterococci in hospital-acquired intra-abdominal infections, patients that have no adequate source control, immunocompromised patients and patients with sepsis [52].
Based on the available evidence, the committee strongly recommends empirical broad-spectrum antibacterial therapy for patients presenting with sepsis to cover all pathogenic bacteria that are likely to be involved. Prior (< 1 year), relevant cultures and local distribution of pathogens associated with sepsis and their antimicrobial susceptibilities should guide the ultimate choice. Although there is a lack of strong evidence, the committee suggests to empirically cover HRMO when these are likely to be involved and to cover anaerobic bacteria in patients presenting with abdominal sepsis or necrotizing soft tissue infections. We suggest against the routine empirical treatment of anaerobic bacteria in sepsis due to aspiration pneumonia, unless empyema or a lung abscess is suspected. Similarly we recommend against the routine empirical treatment of enterococci, but to consider treatment in individual patients with sepsis, such as those who have a high likelihood of enterococcal involvement based on recent relevant cultures and those with recent complicated intra-abdominal surgery or a suspected CVC infection and substantial exposure to broad spectrum antibiotics.
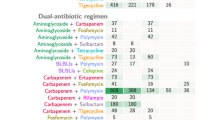
What is the effect of double active empirical antibacterial therapy compared to monotherapy in patients with sepsis?
We defined double active antibacterial therapy as treatment with two classes of antibiotics, both targeting the known or suspected causing pathogen(s) (e.g., ceftriaxone and an aminoglycoside to target gram-negative pathogens) and with the specific purpose to accelerate pathogen clearance rather than to broaden antimicrobial coverage.
Pooled data in a meta-analysis showed no additional effect on all-cause mortality and clinical failure of beta-lactam plus aminoglycoside double active therapy compared to the same or a different beta-lactam when given as monotherapy in patients with sepsis [53]. An increased risk of clinical failure and nephrotoxicity for beta-lactam plus aminoglycoside double active therapy compared to a different beta-lactam given as monotherapy was reported [53]. Other meta-analyses and randomized trials also showed no additional effect of empirical double active antibacterial therapy compared to empirical monotherapy on clinical outcomes in patients with sepsis and septic shock [54], patients with S. aureus bacteraemia [55], patients with severe P. aeruginosa infections [53, 56, 57], and patients with VAP [58, 59].
Based on these data the committee recommends against the use of double active antibacterial therapy in patients with sepsis and septic shock, provided that the chosen single antibacterial agent is active against the most likely pathogens involved. In line, we suggest against double active antibacterial therapy in patients with sepsis due to P. aeruginosa and S. aureus.
What is the optimal choice of empirical therapy in patients with sepsis in The Netherlands
Most trials in patients with severe infections compared cephalosporins, carbapenems, piperacillin-tazobactam and some fluoroquinolones. Clinical outcomes did not consistently support that one of these classes of antibiotics is considerably more effective than others in patients with sepsis. Aminoglycoside-based regimens for sepsis due to HAP or VAP were associated with lower clinical response rates [59]. For sepsis due to intra-abdominal infections, aminoglycoside monotherapy was less effective compared to beta-lactam treatment [60, 61]. One large randomized multicentre trial (MERINO) compared definitive therapy with piperacillin-tazobactam to meropenem in patients with bloodstream infections caused by ceftriaxone-resistant, piperacillin-tazobactam and meropenem sensitive E. coli and K. pneumonia [62]. The 30-day all-cause mortality was 12.3% in patients treated with piperacillin-tazobactam and 3.7% in patients treated with meropenem. There were no trials available on optimal antibiotic treatment of sepsis and high likelihood of S. aureus involvement.
The guideline committee concluded that based on the current data about efficacy and safety of beta-lactams, the experience with beta-lactams and the large number of trials using a beta-lactam, beta-lactams are most appropriate as empirical and definite therapy in the majority of patients with sepsis. Based on the available literature, fluoroquinolones are acceptable alternatives when the risk of fluoroquinolone resistance is considered low. However, clinicians should be aware that the use of fluoroquinolones has significant disadvantages regarding toxicity and the development of resistance [63,64,65,66]. Regarding aminoglycosides, the committee expresses their concerns on potential lower efficacy and higher toxicity risk, but settled that current (lack of) evidence still supports short-term (i.e., maximum of 2 days) aminoglycoside treatment added to a beta-lactam agent in patients with sepsis with the only purpose of increasing the empirical antibacterial spectrum of activity until susceptibility results are available. This strategy is therefore mainly applicable to gram-negative bacteria such as 3GCR-E or P. aeruginosa. Although questions remain, the committee found the evidence on the difference in mortality in the MERINO trial convincing enough to currently recommend against the use of BL/BI and specifically piperacillin-tazobactam for the treatment of sepsis in patients at risk of or with proven involvement of 3GCR Enterobacterales [62].
The choice of empirical sepsis therapy is primarily based on the source of infection. Empirical treatment strategies should be further dictated by the likelihood of involvement of a resistant causative pathogen, by the desire to prevent overuse of reserve antibiotics from a stewardship perspective and by risks of toxicity and other potential adverse events for the patient. The committee therefore provided pragmatic suggestions and alternative strategies for patients with low risk of 3GCR-E involvement and patients at increased or high risk of involvement of 3GCR-E (Additional file 1: Tables S1 and S2). Recommendations are also summarized in Fig. 1. If a definite diagnosis is established one should be referred to other guidelines for empiric antibiotic therapy, e.g., current community-acquired pneumonia (CAP) guidelines do apply in the case of pneumonia-derived sepsis [67].
Flow chart of guideline recommendations on empirical antibiotic treatment of sepsis. *For the diagnosis and non-antibiotic treatment of sepsis we refer to the Dutch guideline ‘Sepsis fase 1’ [4]. **For this guideline, 3GC includes ceftriaxone and cefotaxime and does not include the anti-pseudomonal cephalosporin ceftazidime. ***Guidelines on skin and soft tissue infections [109, 110]. 3GCR-E: 3rd generation cephalosporin-resistant Enterobacterales; 2GC: second generation cephalosporin; 3GC: 3rd generation cephalosporin; SDD: selective decontamination of the digestive tract. CVC: central venous catheter; CAP: community-acquired pneumonia; VAP: ventilator-associated pneumonia; HAP: hospital-acquired pneumonia
What is the optimal empirical antibacterial therapy of sepsis in patients with a penicillin allergy?
Accumulating data from observational cohort studies indicate that true penicillin allergy in patients with a reported penicillin allergy is relatively rare and that avoiding beta-lactams negatively affects treatment outcome [68, 69]. The committee set up a pragmatic approach based on available observational studies including a strong recommendation to obtain information (i.e., medical history and skin test results) about the presumed allergy if possible (Table 3).
Timing and duration of antibacterial therapy in sepsis
What is the optimal timing of empirical antibacterial therapy in patients with sepsis?
In the previous edition of the SWAB sepsis guidelines, it was recommended to start antibacterial therapy in adult patients with severe sepsis and septic shock as soon as possible, preferably within the first hour of presentation [22]. The recommendation was mainly based on the results of one study showing that each hour delay in antibiotic therapy resulted in an average decrease in survival of 7.6% [19], an observation that was underlined by other retrospective observational studies [70,71,72,73]. However, a more recent meta-analysis, which included the aforementioned observational studies, did not show a significant mortality benefit of administering antibiotics within 3 h of ER triage or within 1 h of shock recognition in sepsis [74]. In line, a randomized trial on this topic could not demonstrate an effect of faster (prehospital) antibiotic administration for sepsis on outcome in a Dutch setting [32]. This study however only included a small number of patients with septic shock.
Based on available evidence, the committee deemed it reasonable to state that in patients with septic shock, antibiotics should be administered as soon as possible [71, 72]. On the other hand, in sepsis patients without shock, rapid antibiotic administration should be weighed against the negative impact of potentially unjustified antibiotic use when the patient turns out not to suffer from sepsis [75,76,77].
The guidelines committee therefore agreed not to recommend a specific timeframe in which antibiotics should be administered in patients with sepsis and septic shock. In line with a Dutch trial on the impact of emergency department staff training on time to antibiotic administration and with an earlier Infectious Disease Society of America (IDSA) position statement, the committee recommends that the administration of antibacterial treatment in patients with sepsis or septic shock should be initiated promptly with health care systems working to reduce that time to as short as feasible [32, 75].
What is the optimal duration of antibacterial treatment for sepsis?
Several meta-analyses [59, 78, 79], an RCT [80] and a large propensity-adjusted observational study [81] consistently showed that shorter duration of treatment is as effective and safe as the traditional, longer duration of treatment, in patient with sepsis. Similar results have been found in patients with mild to moderate-severe CAP [67], pyelonephritis [82], uncomplicated cellulitis [83], and bacteraemia [84]. In line, indirect evidence from the studies on PCT-guided discontinuation of antibacterial treatment in patients with sepsis in the ICU setting also suggests that shorter antibacterial treatment duration is safe without a negative effect on mortality [85,86,87,88]. These data, together with the potential adverse effects of antibiotic overuse, strengthened the committee to generally suggest durations of antibiotic therapy in most patients with sepsis that are shorter than historical treatment durations. Table 4 shows recommended treatment durations based on source of infection. Based on available evidence [85, 89,90,91], the committee suggests using PCT levels to support shortening the duration of antibacterial therapy in patients with sepsis if the optimal duration of antibiotic therapy is unclear.
Studies showed conflicting findings on the efficacy and safety of antibiotic de-escalation (ADE) [92,93,94,95]. Within the SWAB sepsis guideline committee there was consensus that ADE is appropriate in many clinical situations. In line with other relevant guidelines the committee recommends to consider ADE in all patients who are on sepsis treatment after 48 h of treatment [88, 96]. We also suggest this would include patients in whom only limited or indirect cultures show no causative pathogen. In contrast, with current conflicting evidence, including the negative outcomes of ADE in one trial on ICU length of stay the committee felt it is defendable not to perform ADE in selected individual patients [95].
Pharmacokinetic and pharmacodynamic considerations in sepsis
In patients with sepsis, should we recommend pharmacokinetic/pharmacodynamic dosing optimization for empirical antibacterial therapy?
Many pathophysiological changes typical for sepsis patients can alter the pharmacokinetic properties of antibiotics and can lead to inadequate antibiotic concentrations when using standard antibiotic dosing schedules [97,98,99,100,101,102]. These pathophysiologic changes include kidney dysfunction, augmented renal clearing (the enhanced renal function sometimes seen in critically ill patients), hypoalbuminemia and increased third space due to fluid therapy [96, 98]. Drug concentrations of hydrophilic antibacterial agents (such as beta-lactams, aminoglycosides and vancomycin) are generally more sensitive to pharmacokinetic changes in patients with sepsis than lipophilic antibacterial agents (such as fluoroquinolones). In addition, patients with sepsis may generally be at higher risk to be infected with bacteria with higher MICs in comparison to other patients [98].
Pooled RCT data in patients with sepsis showed that extended or continuous infusion of beta-lactams in general was associated with decreased all-cause mortality, increased clinical cure with no effect on adverse events and development of resistance compared to intermittent infusion. Evidence was particularly strong for extended infusion of piperacillin-tazobactam and meropenem [103,104,105]. There was lack of evidence for the effect of pharmacokinetic/pharmacodynamic (PK/PD)-based dosing on clinical outcomes of aminoglycosides, vancomycin and ciprofloxacin and in obese patients. The committee felt that the available evidence supports a recommendation of PK/PD-based dosing [96, 98, 106,107,108]. Since EUCAST recommendations on breakpoints are generally accepted and based on PK/PD principles, we followed the EUCAST dosing recommendations for specific pathogens (Additional file 1: Table S3) [31]. We recommended therapeutic drug monitoring (TDM) for all patients on aminoglycoside and vancomycin treatment.
For a complete list of guidelines recommendations, see Table 5. A flow chart is provided in Fig. 1, which summarizes the given recommendations on the empirical antibacterial treatment of sepsis. See Text box 1 for a summary of all the new recommendations compared with the 2010 guideline. The full guidelines text, literature review and rebuttal of the received commentaries are available at www.swab.nl.
Conclusions
We described the most important findings and recommendations of our multidisciplinary guideline committee for the 2020 SWAB sepsis guidelines. We formulated 55 recommendations on the antibacterial management of sepsis in adults in total. One crucial revision is the distinction between low, increased and high risk of infection with Enterobacterales resistant to third generation cephalosporins (3GRC-E) to guide the choice of empirical therapy. Other new topics included empirical antibacterial therapy in patients with a reported penicillin allergy and the role of pharmacokinetics and pharmacodynamics to guide dosing in sepsis.
Availability of data and materials
Literature searches are available from the corresponding author upon request.
References
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM, Shankar-Hari M, Singer M, et al. Assessment of clinical criteria for sepsis: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):762–74.
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD, Singer M. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):775–87.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
van Zanten AR, Sankatsing SU, de Regt MJ, Derde LP, Klijn A, Schellaars R, Wilting RM, et al. Guideline Sepsis fase 1 (2020). Available at: https://richtlijnendatabase.nl/richtlijn/sepsis_fase_1/vroege_herkenning_van_dreigende_sepsis.html.
Vincent JL, Marshall JC, Namendys-Silva SA, Francois B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–6.
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–10.
Finfer S, Bellomo R, Lipman J, French C, Dobb G, Myburgh J. Adult-population incidence of severe sepsis in Australian and New Zealand intensive care units. Intensive Care Med. 2004;30(4):589–96.
Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, Kadri SS, Angus DC, Danner RL, Fiore AE, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318(13):1241–9.
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34(2):344–53.
Davis JS, He V, Anstey NM, Condon JR. Long term outcomes following hospital admission for sepsis using relative survival analysis: a prospective cohort study of 1,092 patients with 5 year follow up. PLoS ONE. 2014;9(12): e112224.
Dreiher J, Almog Y, Sprung CL, Codish S, Klein M, Einav S, Bar-Lavie Y, Singer PP, Nimrod A, Sachs J, et al. Temporal trends in patient characteristics and survival of intensive care admissions with sepsis: a multicenter analysis*. Crit Care Med. 2012;40(3):855–60.
Paoli CJ, Reynolds MA, Sinha M, Gitlin M, Crouser E. Epidemiology and costs of sepsis in the United States-an analysis based on timing of diagnosis and severity level. Crit Care Med. 2018;46(12):1889–97.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, Colombara DV, Ikuta KS, Kissoon N, Finfer S, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–11.
van Gestel A, Bakker J, Veraart CP, van Hout BA. Prevalence and incidence of severe sepsis in Dutch intensive care units. Crit Care. 2004;8(4):R153-162.
Kadri SS, Rhee C, Strich JR, Morales MK, Hohmann S, Menchaca J, Suffredini AF, Danner RL, Klompas M. Estimating ten-year trends in septic shock incidence and mortality in united states academic medical centers using clinical data. Chest. 2017;151(2):278–85.
Barie PS, Hydo LJ, Shou J, Larone DH, Eachempati SR. Influence of antibiotic therapy on mortality of critical surgical illness caused or complicated by infection. Surg Infect (Larchmt). 2005;6(1):41–54.
Kumar A, Ellis P, Arabi Y, Roberts D, Light B, Parrillo JE, Dodek P, Wood G, Kumar A, Simon D, et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136(5):1237–48.
Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118(1):146–55.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589–96.
Vazquez-Guillamet C, Scolari M, Zilberberg MD, Shorr AF, Micek ST, Kollef M. Using the number needed to treat to assess appropriate antimicrobial therapy as a determinant of outcome in severe sepsis and septic shock. Crit Care Med. 2014;42(11):2342–9.
Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother. 2010;54(11):4851–63.
SWAB guidelines for Antibacterial therapy of adult patients with Sepsis (2010). Available at: http://www.swab.nl/swab/cms3.nsf/uploads/65FB380648516FF2C125780F002C39E2/$FILE/swab_sepsis_guideline_december_2010.pdf.
NethMap 2018—Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands in 2017. Availabl at: https://www.swab.nl/swab/cms3.nsf/uploads/AF0C15331EF7438AC12582BF00389A16/$FILE/NethMap-Maran%202018.pdf.
van der Steen M, Leenstra T, Kluytmans JA, van der Bij AK. Trends in expanded-spectrum cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae among Dutch Clinical Isolates, from 2008 to 2012. PLoS ONE. 2015;10(9): e0138088.
Vlek AL, Frentz D, Haenen A, Bootsma HJ, Notermans DW, Frakking FN, de Greeff SC, Leenstra T. Detection and epidemiology of carbapenemase producing Enterobacteriaceae in the Netherlands in 2013–2014. Eur J Clin Microbiol Infect Dis. 2016;35(7):1089–96.
Bakhit M, Jones M, Baker J, Nair R, Yan K, Del Mar C, Scott AM. Reporting of adverse events, conflict of interest and funding in randomised controlled trials of antibiotics: a secondary analysis. BMJ Open. 2021;11(7): e045406.
Phillips R, Hazell L, Sauzet O, Cornelius V. Analysis and reporting of adverse events in randomised controlled trials: a review. BMJ Open. 2019;9(2): e024537.
Tacconelli E, Cataldo MA, Paul M, Leibovici L, Kluytmans J, Schröder W, Foschi F, De Angelis G, De Waure C, Cadeddu C, et al. STROBE-AMS: recommendations to optimise reporting of epidemiological studies on antimicrobial resistance and informing improvement in antimicrobial stewardship. BMJ Open. 2016;6(2): e010134.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. J Clin Epidemiol. 2010;63(12):1308–11.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;62(4):e1-50.
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 8.0 2018. Available at: http://www.eucast.org/clinical_breakpoints/.
Alam N, Oskam E, Stassen PM, Exter PV, van de Ven PM, Haak HR, Holleman F, Zanten AV, Leeuwen-Nguyen HV, Bon V, et al. Prehospital antibiotics in the ambulance for sepsis: a multicentre, open label, randomised trial. Lancet Respir Med. 2018;6(1):40–50.
Klein Klouwenberg PM, Cremer OL, van Vught LA, Ong DS, Frencken JF, Schultz MJ, Bonten MJ, van der Poll T. Likelihood of infection in patients with presumed sepsis at the time of intensive care unit admission: a cohort study. Crit Care. 2015;19:319.
Sartelli M, Catena F, Ansaloni L, Leppaniemi A, Taviloglu K, van Goor H, Viale P, Lazzareschi DV, Coccolini F, Corbella D, et al. Complicated intra-abdominal infections in Europe: a comprehensive review of the CIAO study. World J Emerg Surg. 2012;7(1):36.
Altorf-van der Kuil W, Schoffelen AF, de Greeff SC, Thijsen SF, Alblas HJ, Notermans DW, Vlek AL, van der Sande MA, Leenstra T. National laboratory-based surveillance system for antimicrobial resistance: a successful tool to support the control of antimicrobial resistance in the Netherlands. Euro Surveill. 2017; 22(46).
PREZIES - Referentiecijfers 2012 t/m 2016: lijnsepsis. Available at: https://www.rivm.nl/sites/default/files/2021-06/Referentiecijfers%202016.pdf.
Ong DSY, Frencken JF, Klein Klouwenberg PMC, Juffermans N, van der Poll T, Bonten MJM, Cremer OL. Short-course adjunctive gentamicin as empirical therapy in patients with severe sepsis and septic shock: a prospective observational cohort study. Clin Infect Dis. 2017;64(12):1731–6.
Alevizakos M, Karanika S, Detsis M, Mylonakis E. Colonisation with extended-spectrum beta-lactamase-producing Enterobacteriaceae and risk for infection among patients with solid or haematological malignancy: a systematic review and meta-analysis. Int J Antimicrob Agents. 2016;48(6):647–54.
Rottier WC, Bamberg YR, Dorigo-Zetsma JW, van der Linden PD, Ammerlaan HS, Bonten MJ. Predictive value of prior colonization and antibiotic use for third-generation cephalosporin-resistant Enterobacteriaceae bacteremia in patients with sepsis. Clin Infect Dis. 2015;60(11):1622–30.
Rottier WC, van Werkhoven CH, Bamberg YRP, Dorigo-Zetsma JW, van de Garde EM, van Hees BC, Kluytmans J, Kuck EM, van der Linden PD, Prins JM et al. Development of diagnostic prediction tools for bacteraemia caused by third-generation cephalosporin-resistant enterobacteria in suspected bacterial infections: a nested case-control study. Clin Microbiol Infect 2018.
Detsis M, Karanika S, Mylonakis E. ICU acquisition rate, risk factors, and clinical significance of digestive tract colonization with extended-spectrum beta-lactamase-producing Enterobacteriaceae: a systematic review and meta-analysis. Crit Care Med. 2017;45(4):705–14.
Bruyere R, Vigneron C, Bador J, Aho S, Toitot A, Quenot JP, Prin S, Charles PE. Significance of prior digestive colonization with extended-spectrum beta-lactamase-producing Enterobacteriaceae in patients with ventilator-associated pneumonia. Crit Care Med. 2016;44(4):699–706.
Carrara E, Pfeffer I, Zusman O, Leibovici L, Paul M. Determinants of inappropriate empirical antibiotic treatment: systematic review and meta-analysis. Int J Antimicrob Agents. 2018;51(4):548–53.
Cardoso T, Almeida M, Carratala J, Aragao I, Costa-Pereira A, Sarmento AE, Azevedo L. Microbiology of healthcare-associated infections and the definition accuracy to predict infection by potentially drug resistant pathogens: a systematic review. BMC Infect Dis. 2015;15:565.
Johnson SW, Anderson DJ, May DB, Drew RH. Utility of a clinical risk factor scoring model in predicting infection with extended-spectrum beta-lactamase-producing enterobacteriaceae on hospital admission. Infect Control Hosp Epidemiol. 2013;34(4):385–92.
de Smet AM, Kluytmans JA, Blok HE, Mascini EM, Benus RF, Bernards AT, Kuijper EJ, Leverstein-van Hall MA, Jansz AR, de Jongh BM, et al. Selective digestive tract decontamination and selective oropharyngeal decontamination and antibiotic resistance in patients in intensive-care units: an open-label, clustered group-randomised, crossover study. Lancet Infect Dis. 2011;11(5):372–80.
Dutch Working party on Infection Prevention (WIP)—highly resistant micro-organisms (HRMO) in hospitals(2017). Available at: https://www.rivm.nl/sites/default/files/2018-11/130424%20BRMO.pdf.
Marquet K, Liesenborgs A, Bergs J, Vleugels A, Claes N. Incidence and outcome of inappropriate in-hospital empiric antibiotics for severe infection: a systematic review and meta-analysis. Crit Care. 2015;19:63.
Raman G, Avendano E, Berger S, Menon V. Appropriate initial antibiotic therapy in hospitalized patients with gram-negative infections: systematic review and meta-analysis. BMC Infect Dis. 2015;15:395.
Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME. Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum beta-lactamases: a systematic review and meta-analysis. J Antimicrob Chemother. 2012;67(12):2793–803.
Rottier WC, Ammerlaan HS, Bonten MJ. Effects of confounders and intermediates on the association of bacteraemia caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae and patient outcome: a meta-analysis. J Antimicrob Chemother. 2012;67(6):1311–20.
Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, Chang PK, O’Neill PJ, Mollen KP, Huston JM, et al. The surgical infection society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017;18(1):1–76.
Paul M, Lador A, Grozinsky-Glasberg S, Leibovici L. Beta lactam antibiotic monotherapy versus beta lactam-aminoglycoside antibiotic combination therapy for sepsis. Cochrane Database Syst Rev. 2014;1:CD003344.
Brunkhorst FM, Oppert M, Marx G, Bloos F, Ludewig K, Putensen C, Nierhaus A, Jaschinski U, Meier-Hellmann A, Weyland A, et al. Effect of empirical treatment with moxifloxacin and meropenem vs meropenem on sepsis-related organ dysfunction in patients with severe sepsis: a randomized trial. JAMA. 2012;307(22):2390–9.
Thwaites GE, Scarborough M, Szubert A, Nsutebu E, Tilley R, Greig J, Wyllie SA, Wilson P, Auckland C, Cairns J, et al. Adjunctive rifampicin for Staphylococcus aureus bacteraemia (ARREST): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2018;391(10121):668–78.
Vardakas KZ, Tansarli GS, Bliziotis IA, Falagas ME. beta-Lactam plus aminoglycoside or fluoroquinolone combination versus beta-lactam monotherapy for Pseudomonas aeruginosa infections: a meta-analysis. Int J Antimicrob Agents. 2013;41(4):301–10.
Hu Y, Li L, Li W, Xu H, He P, Yan X, Dai H. Combination antibiotic therapy versus monotherapy for Pseudomonas aeruginosa bacteraemia: a meta-analysis of retrospective and prospective studies. Int J Antimicrob Agents. 2013;42(6):492–6.
Arthur LE, Kizor RS, Selim AG, van Driel ML, Seoane L. Antibiotics for ventilator-associated pneumonia. Cochrane Database Syst Rev. 2016;10:CD004267.
Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, Napolitano LM, O’Grady NP, Bartlett JG, Carratala J, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–111.
Bailey JA, Virgo KS, DiPiro JT, Nathens AB, Sawyer RG, Mazuski JE. Aminoglycosides for intra-abdominal infection: equal to the challenge? Surg Infect (Larchmt). 2002;3(4):315–35.
Falagas ME, Matthaiou DK, Karveli EA, Peppas G. Meta-analysis: randomized controlled trials of clindamycin/aminoglycoside vs. beta-lactam monotherapy for the treatment of intra-abdominal infections. Aliment Pharmacol Ther. 2007;25(5):537–56.
Harris PNA, Tambyah PA, Lye DC, Mo Y, Lee TH, Yilmaz M, Alenazi TH, Arabi Y, Falcone M, Bassetti M, et al. Effect of piperacillin-tazobactam vs meropenem on 30-day mortality for patients with E coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA. 2018;320(10):984–94.
EMA - Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics (2018). Available at: https://www.ema.europa.eu/en/documents/press-release/disabling-potentially-permanent-side-effects-lead-suspension-restrictions-quinolone-fluoroquinolone_en.pdf.
Etminan M, Sodhi M, Ganjizadeh-Zavareh S, Carleton B, Kezouh A, Brophy JM. Oral fluoroquinolones and risk of mitral and aortic regurgitation. J Am Coll Cardiol. 2019;74(11):1444–50.
Lee CC, Lee MG, Hsieh R, Porta L, Lee WC, Lee SH, Chang SS. Oral fluoroquinolone and the risk of aortic dissection. J Am Coll Cardiol. 2018;72(12):1369–78.
Yu X, Jiang DS, Wang J, Wang R, Chen T, Wang K, Cao S, Wei X. Fluoroquinolone use and the risk of collagen-associated adverse events: a systematic review and meta-analysis. Drug Saf. 2019;42(9):1025–33.
Wiersinga WJ, Bonten MJ, Boersma WG, Jonkers RE, Aleva RM, Kullberg BJ, Schouten JA, Degener JE, van de Garde EMW, Verheij TJ, et al. Management of community-acquired pneumonia in adults: 2016 guideline update from the Dutch Working Party on Antibiotic Policy (SWAB) and Dutch Association of Chest Physicians (NVALT). Neth J Med. 2018;76(1):4–13.
Blumenthal KG, Parker RA, Shenoy ES, Walensky RP. Improving clinical outcomes in patients with methicillin-sensitive Staphylococcus aureus bacteremia and reported penicillin allergy. Clin Infect Dis. 2015;61(5):741–9.
MacFadden DR, LaDelfa A, Leen J, Gold WL, Daneman N, Weber E, Al-Busaidi I, Petrescu D, Saltzman I, Devlin M, et al. Impact of reported beta-lactam allergy on inpatient outcomes: a multicenter prospective cohort study. Clin Infect Dis. 2016;63(7):904–10.
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, Artigas A, Schorr C, Levy MM. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42(8):1749–55.
Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, Lemeshow S, Osborn T, Terry KM, Levy MM. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376(23):2235–44.
Liu VX, Fielding-Singh V, Greene JD, Baker JM, Iwashyna TJ, Bhattacharya J, Escobar GJ. The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med. 2017;196(7):856–63.
Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997–1000.
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe sepsis and septic shock: a systematic review and meta-analysis. Crit Care Med. 2015;43(9):1907–15.
Kalil AC, Gilbert DN, Winslow DL, Masur H, Klompas M. Infectious Diseases Society of America (IDSA) POSITION STATEMENT: why IDSA did not endorse the surviving sepsis campaign guidelines. Clin Infect Dis. 2018;66(10):1631–5.
Klompas M, Calandra T, Singer M. Antibiotics for sepsis-finding the equilibrium. JAMA. 2018;320(14):1433–4.
Singer M. Antibiotics for sepsis: does each hour really count, or is it incestuous amplification? Am J Respir Crit Care Med. 2017;196(7):800–2.
Dimopoulos G, Poulakou G, Pneumatikos IA, Armaganidis A, Kollef MH, Matthaiou DK. Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest. 2013;144(6):1759–67.
Pugh R, Grant C, Cooke RP, Dempsey G. Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults. Cochrane Database Syst Rev 2015(8):CD007577.
Yahav D, Franceschini E, Koppel F, Turjeman A, Babich T, Bitterman R, Neuberger A, Ghanem-Zoubi N, Santoro A, Eliakim-Raz N, et al. Seven versus fourteen days of antibiotic therapy for uncomplicated gram-negative bacteremia: a non-inferiority randomized controlled trial. Clin Infect Dis. 2018;69:1091.
Chotiprasitsakul D, Han JH, Cosgrove SE, Harris AD, Lautenbach E, Conley AT, Tolomeo P, Wise J, Tamma PD. Comparing the outcomes of adults with enterobacteriaceae bacteremia receiving short-course versus prolonged-course antibiotic therapy in a multicenter, propensity score-matched cohort. Clin Infect Dis. 2018;66(2):172–7.
Eliakim-Raz N, Yahav D, Paul M, Leibovici L. Duration of antibiotic treatment for acute pyelonephritis and septic urinary tract infection– 7 days or less versus longer treatment: systematic review and meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2013;68(10):2183–91.
Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164(15):1669–74.
Havey TC, Fowler RA, Daneman N. Duration of antibiotic therapy for bacteremia: a systematic review and meta-analysis. Crit Care. 2011;15(6):R267.
Wirz Y, Meier MA, Bouadma L, Luyt CE, Wolff M, Chastre J, Tubach F, Schroeder S, Nobre V, Annane D, et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomized trials. Crit Care (London, England). 2018;22(1):191.
Iankova I, Thompson-Leduc P, Kirson NY, Rice B, Hey J, Krause A, Schonfeld SA, DeBrase CR, Bozzette S, Schuetz P. Efficacy and safety of procalcitonin guidance in patients with suspected or confirmed sepsis: a systematic review and meta-analysis. Crit Care Med. 2018;46(5):691–8.
de Jong E, van Oers JA, Beishuizen A, Vos P, Vermeijden WJ, Haas LE, Loef BG, Dormans T, van Melsen GC, Kluiters YC, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16(7):819–27.
Schuts EC, Hulscher ME, Mouton JW, Verduin CM, Cohen Stuart JW, Overdiek JW, van der Linden PD. SWAB Guidelines for Antimicrobial Stewardship 2016. Available at: https://swab.nl/en/exec/file/download/81.
Lam SW, Bauer SR, Fowler R, Duggal A. Systematic review and meta-analysis of procalcitonin-guidance versus usual care for antimicrobial management in critically ill patients: focus on subgroups based on antibiotic initiation, cessation, or mixed strategies. Crit Care Med. 2018;46(5):684–90.
Meier MA, Branche A, Neeser OL, Wirz Y, Haubitz S, Bouadma L, Wolff M, Luyt CE, Chastre J, Tubach F, et al. Procalcitonin-guided antibiotic treatment in patients with positive blood cultures: a patient-level meta-analysis of randomized trials. Clin Infect Dis. 2018;69:388.
Pepper DJ, Sun J, Rhee C, Welsh J, Powers JH 3rd, Danner RL, Kadri SS. Procalcitonin-guided antibiotic discontinuation and mortality in critically ill adults: a systematic review and meta-analysis. Chest. 2019;155(6):1109–18.
Paul M, Dickstein Y, Raz-Pasteur A. Antibiotic de-escalation for bloodstream infections and pneumonia: systematic review and meta-analysis. Clin Microbiol Infect. 2016;22(12):960–7.
Tabah A, Cotta MO, Garnacho-Montero J, Schouten J, Roberts JA, Lipman J, Tacey M, Timsit JF, Leone M, Zahar JR, et al. A systematic review of the definitions, determinants, and clinical outcomes of antimicrobial de-escalation in the intensive care unit. Clin Infect Dis. 2016;62(8):1009–17.
Guo Y, Gao W, Yang H, Ma C, Sui S. De-escalation of empiric antibiotics in patients with severe sepsis or septic shock: a meta-analysis. Heart Lung. 2016;45(5):454–9.
Leone M, Bechis C, Baumstarck K, Lefrant JY, Albanese J, Jaber S, Lepape A, Constantin JM, Papazian L, Bruder N, et al. De-escalation versus continuation of empirical antimicrobial treatment in severe sepsis: a multicenter non-blinded randomized noninferiority trial. Intensive Care Med. 2014;40(10):1399–408.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45(3):486–552.
Varghese JM, Roberts JA, Lipman J. Antimicrobial pharmacokinetic and pharmacodynamic issues in the critically ill with severe sepsis and septic shock. Crit Care Clin. 2011;27(1):19–34.
Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, Hope WW, Farkas A, Neely MN, Schentag JJ, et al. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14(6):498–509.
Roberts JA, Webb S, Paterson D, Ho KM, Lipman J. A systematic review on clinical benefits of continuous administration of beta-lactam antibiotics. Crit Care Med. 2009;37(6):2071–8.
Goncalves-Pereira J, Povoa P. Antibiotics in critically ill patients: a systematic review of the pharmacokinetics of beta-lactams. Crit Care. 2011;15(5):R206.
Bos JC, van Hest RM, Misticio MC, Nunguiane G, Lang CN, Beirao JC, Mathot RAA, Prins JM. Pharmacokinetics and pharmacodynamic target attainment of benzylpenicillin in an adult severely ill sub-Saharan African patient population. Clin Infect Dis. 2018;66(8):1261–9.
Bos JC, Prins JM, Misticio MC, Nunguiane G, Lang CN, Beirao JC, Mathot RAA, van Hest RM. Pharmacokinetics and pharmacodynamic target attainment of ceftriaxone in adult severely ill sub-Saharan African patients: a population pharmacokinetic modelling study. J Antimicrob Chemother. 2018;73(6):1620–9.
Vardakas KZ, Voulgaris GL, Maliaros A, Samonis G, Falagas ME. Prolonged versus short-term intravenous infusion of antipseudomonal beta-lactams for patients with sepsis: a systematic review and meta-analysis of randomised trials. Lancet Infect Dis. 2018;18(1):108–20.
Roberts JA, Abdul-Aziz MH, Davis JS, Dulhunty JM, Cotta MO, Myburgh J, Bellomo R, Lipman J. Continuous versus intermittent beta-lactam infusion in severe sepsis. A meta-analysis of individual patient data from randomized trials. Am J Respir Crit Care Med. 2016;194(6):681–91.
Rhodes NJ, Liu J, O’Donnell JN, Dulhunty JM, Abdul-Aziz MH, Berko PY, Nadler B, Lipman J, Roberts JA. Prolonged infusion piperacillin-tazobactam decreases mortality and improves outcomes in severely Ill patients: results of a systematic review and meta-analysis. Crit Care Med. 2018;46(2):236–43.
Blot S, Koulenti D, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, Kaukonen KM, Martin C, Montravers P, Rello J, et al. Does contemporary vancomycin dosing achieve therapeutic targets in a heterogeneous clinical cohort of critically ill patients? Data from the multinational DALI study. Crit Care. 2014;18(3):R99.
Bakke V, Sporsem H, Von der Lippe E, Nordoy I, Lao Y, Nyrerod HC, Sandvik L, Harvig KR, Bugge JF, Helset E. Vancomycin levels are frequently subtherapeutic in critically ill patients: a prospective observational study. Acta Anaesthesiol Scand. 2017;61(6):627–35.
Taccone FS, Laterre PF, Dugernier T, Spapen H, Delattre I, Wittebole X, De Backer D, Layeux B, Wallemacq P, Vincent JL, et al. Insufficient beta-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care. 2010;14(4):R126.
Necrotiserende wekedeleninfecties 2015. Available at: https://richtlijnendatabase.nl/richtlijn/necrotiserende_wekedeleninfecties/startpagina_-_nwdi.html.
Lavrijsen AP, Damstra RJ, van Dissel JT, Draijer LW, van Everdingen JJ, Go PM, Kwa D, Komen DJ. Richtlijn cellulitis en erysipelas van de onderste extremiteiten 2013.
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, Cook CH, O’Neill PJ, Mazuski JE, Askari R, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372(21):1996–2005.
Hassinger TE, Guidry CA, Rotstein OD, Duane TM, Evans HL, Cook CH, O’Neill PJ, Mazuski JE, Askari R, Napolitano LM, et al. Longer-duration antimicrobial therapy does not prevent treatment failure in high-risk patients with complicated intra-abdominal infections. Surg Infect (Larchmt). 2017;18(6):659–63.
Rattan R, Allen CJ, Sawyer RG, Askari R, Banton KL, Claridge JA, Cocanour CS, Coimbra R, Cook CH, Cuschieri J, et al. Patients with complicated intra-abdominal infection presenting with sepsis do not require longer duration of antimicrobial therapy. J Am Coll Surg. 2016;222(4):440–6.
Montravers P, Tubach F, Lescot T, Veber B, Esposito-Farese M, Seguin P, Paugam C, Lepape A, Meistelman C, Cousson J, et al. Short-course antibiotic therapy for critically ill patients treated for postoperative intra-abdominal infection: the DURAPOP randomised clinical trial. Intensive Care Med. 2018;44(3):300–10.
van Lent AU, Bartelsman JF, Tytgat GN, Speelman P, Prins JM. Duration of antibiotic therapy for cholangitis after successful endoscopic drainage of the biliary tract. Gastrointest Endosc. 2002;55(4):518–22.
SWAB Guidelines for Antimicrobial Therapy of Complicated Urinary Tract Infections in Adults 2013. Available at: https://www.swab.nl/swab/cms3.nsf/uploads/41949F6BD9ED10EDC1257B7F00212560/$FILE/revised%20uti%20guideline%20FINAL%20010413.pdf.
Verduin K, Ammerlaan H, Blaauw G, Bleeker-Rovers CP, van Drie-Pierik RJ, Ekkelenkamp M, Glaudemans AW, van Hout D. Richtlijn Staphylococcus aureus bacteriëmie 2019 (NVMM). Available at: https://richtlijnendatabase.nl/richtlijn/staphylococcus_aureus_bacteriemie/startpagina.html.
SWAB Guidelines on Antibacterial Therapy of Patients with Bacterial Central Nervous System Infections 2012. Available at: https://www.swab.nl/swab/cms3.nsf/uploads/FE54A057082AA54CC1257A2B00293B1D/$FILE/SWAB_CNSguideline_%20June12.pdf.
Acknowledgements
The Guidelines Committee would like to thank all individuals and societies who contributed to the development of these guidelines.
Funding
This projected was funded by the Dutch Working Party on Antibiotic Policy (SWAB), Leiden, the Netherlands.
Author information
Authors and Affiliations
Contributions
All authors contributed to the project conception and design. Data collection and first analysis were performed by ES, HIB, JJH, MGJB, MK, JS and WJW. The first draft of the manuscript was written by ES, HIB, MGJB, MK, PDL, DCM, JAS, JMP, WJW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Members of the preparatory committee reported the following potential conflicts of interest: ES: None; HIB: None; JJH: None; MGJB: Chair Stichting Werkgroep Antibioticabeleid, Chair COIG Infectieziekten en Immuniteit, NIV; MB: Institutional payment for consultancy / advisory board for Johnson&Johnson, Bard, Acelity, Gore, Institutional grants Johnson&Johnson, Mylan, Bard, Acelity, LifeCell/Allergan, New Compliance; MJMB: Consultant for Janssen Vaccines, (paid to UMCU), Research funding Janssen Vaccines, Immunexpress, Vedanta, (paid to UMCU), research funding Innovative Medicines Initiative (paid to UMCU); DD: None; RGW: Board member EAACI (European Academy of Allergy and Clinical Imunology), president UEMS Section and Board of Allergology, member of several national and international guideline committees; NPJ: Research funding ZonMW, Sanquin, Horizon2020, CSL Behring (not related to the current guideline); MK: None; PDL: Treasurer Stichting Werkgroep Antibioticabeleid; DCM: None; PP: Consultancy board memberships (not related to the current guideline), chair SepsisNet Nederland Foundation (unpaid); JAS: Member Wetenschappelijke Adviesraad (paid), Radboud Center Infectious Diseases, ESGAP (ESCMID) secretary, SWAB member, unrestricted educational Grant MSD; JRR: Curriculum-, en implementatiecommissie NVSHA, visitatiecommissie NVSHA, member of local sepsis guideline committee; ARHZ: Head of ICU & Research, Ziekenhuis Gelderse Valei, Ede, chair SKMS guideline Sepsis, research grants Adrenoss, Nutricia, Beacon, Cardinal Health, lectures (paid) not related to antibacterial therapy of Abbott, Baxter, BBraun, Fresenius-Kabi, Lyric, Nutricia, Nestle. The SKMS Sepsis guideline has been developed parallel to the SWAB sepsis guideline. JMP: editor in chief digital guideline antimicrobial therapy “SWAB ID”, (paid to AMC), member Wetenschappelijke Adviesraad Zorginstituut Nederland, CG (paid), member Board Stichting de Merel (non-profit, paid to AMC); WJW: Research funding from NWO, ZonMW and Horizon2020 (not related to the current guideline).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
sTable 1. Alternative empirical treatment strategies in sepsis and low estimated risk of involvement of 3GCR-E. sTable 2. Alternative empirical treatment strategies in sepsis and increased or high estimated risk of involvement of 3GCR-E. sTable 3. Recommended iv doses of empirical antibacterial treatment for sepsis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sieswerda, E., Bax, H.I., Hoogerwerf, J.J. et al. The 2021 Dutch Working Party on Antibiotic Policy (SWAB) guidelines for empirical antibacterial therapy of sepsis in adults. BMC Infect Dis 22, 687 (2022). https://doi.org/10.1186/s12879-022-07653-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07653-3