Abstract
Despite the abundance of research on the risk factors for mortality following hip fracture surgery, there has been a dearth of studies on prediction models in this population. The objective of this research was to explore the influencing factors and construct a clinical nomogram to predict one-year postoperative mortality in patients with hip fracture surgeries. Using the Ditmanson Research Database (DRD), we included 2333 subjects, aged ≥ 50 years who underwent hip fracture surgery between October, 2008 and August, 2021. The endpoint was all-cause mortality. A least absolute shrinkage and selection operator (LASSO) derived Cox regression was performed to select the independent predictors of one-year postoperative mortality. A nomogram was built for predicting one-year postoperative mortality. The prognostic performance of nomogram was evaluated. On the basis of tertiary points in a nomogram, the patients were divided into low, middle and high risk groups, and compared by the Kaplan–Meier analysis. Within 1 year after hip fracture surgery, 274 patients (11.74%) died. Variables retained in the final model comprised age, sex, length of stay, RBC transfusions, hemoglobin, platelet, and eGFR. The AUC for one-year mortality predictions were 0.717 (95% CI = 0.685–0.749). The Kaplan–Meier curves were significantly different among the three risk groups (p < 0.001). The nomogram showed good calibration. In summary, we explored the one-year postoperative mortality risk in geriatric patients with a hip fracture and developed a prediction model that could help clinicians identify patients at high risk of postoperative mortality.
Similar content being viewed by others
Introduction
Hip fracture is a major and increasing global health concern. Based on the epidemiologic projections, it is estimated that there will be 2.6 million individuals will suffer a hip fracture by 20251. The number of hip fractures expected to increase to 6.3 million by 2050 as life expectancy of the world population increases2. They have been associated with increased morbidity, loss of independence, high rate of institutionalization, and mortality3. Mortality is considered the most serious consequence, the one-year mortality after hip fractures surgery is high, ranging between 15 and 36%4,5,6,7. Therefore, it is critical to explore prognostic factors to identify patients with hip fracture who have a high risk of death as early as possible.
Advanced age, male sex, high comorbidity burden, frailty, low functional status or reduced mobility, cognitive impairment and time-to-surgery have been identified as significant predictors of postoperative mortality in hip fracture patients3,5,8. In spite of this knowledge, it could be a challenge to obtain an overview risk profile of each patient in clinical practice. In view of the importance of early identification of adverse prognosis in hip fracture for patient treatment and management, an increasing number of researchers and policymakers tend to rely on predictive models.
As far as we know, several research groups have developed surgery-specific or hip fracture-specific risk prediction models9,10. For instance, the Orthopaedic version of the Physiologic and Operative Severity Score for the enUmeration of Mortality and morbidity (O-POSSUM)11 and The Estimation of Physiologic Ability and Surgical Stress (E-PASS)12,13 can be aid to predict mortality, however, their intricate formulas are not easy to apply in a busy clinical setting and some of these data in these models are not easily available and must be specifically collected14. Some models which are specifically designed for early mortality after hip fracture [as the Nottingham Hip Fracture Score (NHFS)]13,15 are simple and faster to use, however none of them showed excellent discrimination.
While predictors for postoperative mortality of hip fracture have been diffusely studied, research pertaining to risk prediction models is limited. The nomogram has been accepted as a reliable tool to create a simple intuitive graph of a statistical predictive model that quantifies the risk of a clinical event. Herein, we conducted this retrospective study to investigate the predictors for one-year postoperative mortality and constructed a corresponding clinical nomogram to predict high-risk ones.
Patients selection and methods
Data source
We conducted a retrospective cohort study of hip fracture surgery patients with the data retrieved from the electronic medical record database [Ditmanson Research Database (DRD)] at Ditmanson Medical Foundation Chia-Yi Christian Hospital, a regional hospital in southern Taiwan.
Ethics statement
This study was approved by the Institutional Review Board of the Ditmanson Medical Foundation Chia-Yi Christian Hospital, Taiwan (CYCH-IRB No: 2019063). Informed consent was waived by the Institutional Review Board of the Ditmanson Medical Foundation Chia-Yi Christian Hospital because of the retrospective nature of the study and the analysis used anonymous clinical data. All of the methods were performed in accordance with relevant guidelines and regulations, including any relevant details.
Patients selection
A total of 2333 patients underwent hip fracture surgery between October, 2008 and August, 2021. The eligibility criteria were: (1) ages ≥ 50 years; (2) introchanteric (ICD-9-CM Code 820.2, 820.20, 820.21, 820.3, 820.30, 820.31; ICD-10 Code S72.1), subtrochanteric (ICD-9-CM Code 820.22, 820.32; ICD-10 Code S72.2), or femoral neck fractures (ICD-9-CM Code 820.0, 820.1, 820.8, 820.9; ICD-10 Code S72.0); (3) recipients of surgeries including partial hip replacement, open or closed reduction internal fixation; (4) caused by a low-energy injury (such as osteoporosis and fall). We excluded patients who were below age 50 years, patients with pathological fractures, multiple fractures or multiple trauma, conservative treatment, and loss of data.
Predictor variables and primary outcome
The following patient demographics were extracted from the DRD: age, sex, length of stay, intensive care unit (ICU), operation time, type of anaesthesia, RBC transfusions, surgical procedure performed, type of hip fracture, time from injury to operation, preoperative clinical variables including comorbidities [eg. diabetes mellitus (DM), hypertension, congestive heart failure, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), cancer, and dementia], and admission laboratory data (eg. RBC, WBC count, hemoglobin, hematocrite, platelet, BUN, creatinine, and eGFR). The estimated glomerular filtration rate (eGFR) was determined according to serum Cr levels and sex using the calculation method used in a previous study16. The main outcome was the occurrence of death at one-year after surgery for hip fracture. The dates of mortality were obtained in reference to the Taiwan Death Registry database.
Statistical analysis
All statistical analyses were performed using the R programming language and environment (http://www.r-project.org/). Results were considered statistically significant for a 2-tailed test if p-value < 0.05. Continuous variables were presented as the mean ± standard deviation (SD), and were compared using the Student's t test whereas categorical variables was presented by percentages and comparisons of categorical data were examined by Chi square test. If a potential predictor had more than 5% missing data, multiple imputation was used as a method to handle the missing values17. We divided continuous variables into classification variables, which makes the model more objective and simpler. The cut-off value of the classification variable was age, length of stay, operation time and the normal value of clinical laboratory examination. The cut-off value of numeric values as follows: age was 85 years, length of stay was 15 days, operation time was 90 min, WBC was 3.5 and 9.9*103/μL, hemoglobin was 10 g/dL, RBC transfusions was 2 units, platelet was 100*109/L and eGFR was 60 mL/min/1.73 m2. The duration of hospitalization was assessed in terms of days, and was determined by calculating the difference between the date of admission and the date of discharge18. Patients who had a hospital stay of 15 days or more were classified as having a prolonged length of stay19,20,21. A least absolute shrinkage and selection operator (LASSO) derived Cox regression followed by ten-fold cross-validation of variables were used to identify the predictors for one-year postoperative mortality. Multivariate Cox regression was further performed to assess the prognostic value of selected variables. Univariate and multivariate Cox proportional hazards models were used to calculate hazard ratios (HRs) and 95% confidence interval (CI) for one-year postoperative mortality. Survival curves were depicted using the Kaplan–Meier method. These variables were further applied to build a nomogram for estimating the one-year survival ratios of one-year postoperative mortality using the rms package in R. The concordance index (C-index) and AUC curve were used to appraise the performance of the nomogram. After internal validation by bootstrapping, a calibration curve was used to evaluate the calibration of the nomogram by contrasting the actual risk and predicted risk. According to the net benefit and threshold probabilities, the clinical usefulness of the nomogram was estimated using the decision curve analysis (DCA).
Results
Patients’ characteristics
The demographics and clinical characteristics in the hip fracture patients who were alive and dead one-year postoperatively are compared in Table 1. Patients who died within one-year postoperatively tended to be older (81.09 years vs 77.73 years, p < 0.001), more often male (47.45% vs 30.45%, p < 0.001), longer length of stay (8.72 days vs 6.51 days, p < 0.001). Trochanteric fractures, spinal anaesthesia alone, RBC transfusions > 2 units and time from injury to operation ≧ 48 h were slightly more common among patients who died (p < 0.05), while the operation type and operation blood loss did not differ significantly (p > 0.05). There were significant difference in the comorbidities, including congestive heart failure, chronic kidney disease, and cancer, and in laboratory parameters, including RBC hemoglobin, hematocrite, BUN, creatinine and eGFR (p < 0.05) between survivors and nonsurvivors.
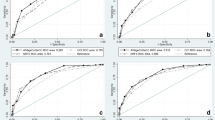
Predictive factor selection
LASSO regression identified 7 predictors associated with postoperative mortality after hip fracture from 19 demographics and clinical characteristics, including age, sex, length of stay, RBC transfusions, hemoglobin, platelet and eGFR (Fig. 1). Then, we presented these predictors into multiple cox proportional hazard regression to quantify the association strength with postoperative mortality after hip fracture (Table 2).
(a) Predictor selection using the LASSO Cox regression analysis; (b) seven risk factors selected using LASSO Cox regression analysis. The two dotted vertical lines were drawn at the optimal scores by minimum criteria and 1-s.e. criteria (at minimum criteria including age, sex, length of stay, RBC transfusions, hip fracture type, type of anaesthesia, operation time, diabetes mellitus, congestive heart failure, chronic obstructive pulmonary disease, cancer, dementia, hemoglobin, platelet, eGFR and WBC count; at 1-s.e. criteria including age, sex, length of stay, RBC transfusions, hemoglobin, platelet, and eGFR).
Nomogram as a tool for visualization
To facilitate the clinical service, we converted the complex mathematical model into a nomogram (Fig. 2). It was necessary to sum the scores of variables included in the model. And then a vertical line at the total score was drawn and making it intersect with the one line representing the predicted mortality. The corresponding values of the point of intersection were the predicted one-year mortality of individuals. For example, a more than 85-year-old male patient, length of stay more than 15 days, RBC transfusions more than 2 unit, hemoglobin more than 10 g/dL, eGFR more than 60 mL/min /1.73 m2, and platelet more than 100 (1000/μL) had about a total score of 240, with a 1-year survival of 62% (Supplementary Table 1). It could be seen that nomogram was more convenient to use in clinical practice than mathematical formulas.
Establishment of nomograms for predicting postoperative mortality
The nomogram for predicting one-year survival was constructed based on the abovementioned predictors, as presented in Fig. 2. The predictive value of the nomogram was assessed by AUC. The AUC for one-year mortality predictions were 0.717 (95% CI = 0.685–0.749, Fig. 3). The calibration curves revealed good consistency between the nomograms’ predicted values and actual observations, with all calibration curve close to the 45-degree line (Fig. 4). DCA revealed that the nomogram had an excellent positive net clinical benefit within a specific threshold range, demonstrating the good clinical utility of nomogram (Fig. 5).
Risk stratification based on the novel nomogram
To reveal the independent discrimination ability of the simple-to-use postoperative mortality nomogram, we subdivided the patients into high- (score > 92), middle- (50—92), and low-risk (score < 50) groups according to the total risk scores in the study group. The patients in the three different risk subgroups showed significant differences in postoperatively mortality (p < 0.05, Fig. 6).
Discussion
This retrospective cohort analysis used LASSO Cox regression analysis to identify independent risk factors of one-year postoperative mortality in geriatric patients with a hip fracture. The nomogram has been accepted as a reliable tool to create a simple intuitive graph of a statistical predictive model that quantifies the risk of a clinical event22,23. Numerous studies have indicated their potential value in clinical practice24,25. The following seven variables were included in the simplified model: age, sex, length of stay, RBC transfusions, hemoglobin, platelet and eGFR. This nomogram has a good discriminative and calibration capabilities. Moreover, all variables in the model are easily available, which guarantees the clinical utility of this nomogram.
As predicted, age and sex had an influence on mortality in patients with hip fracture. This study, as well as others, shows that mortality after hip fracture were increased with increasing age19,26,27,28. Moreover, multiple studies have shown the gender differences in mortality in patients with hip fracture. Our results are similar to other studies, that men had higher mortality risk than women. Reasons for sex differences remain unclear. Many scholars consider that male gender have poor lifestyle, like smoking and drinking, which are often associated with hypertension, coronary heart disease, COPD and other basic diseases, and their average life expectancy is shorter than that of female gender29. Therefore, males should be had higher mortality rates than females. Some have postulated that men seem to be sicker and frailer than women at this point in time of fracture, making them more vulnerable to postoperative mortality secondary to infections such as pneumonia and influenza29,30. Even though age and gender are non-modifiable factors, abundant comprehensive geriatric assessment, or intervention in geriatric male patients with hip fracture may be indispensable to diminish adverse outcomes.
The present study found that hemoglobin, platelet, and eGFR, which are easily accessible and convenient laboratory tests, reflected well the risk of mortality of patients after hip fracture surgery. The admission hemoglobin levels < 10 g/dL was found as a significant predictor of mortality in previous studies31,32,33. Our findings are concordance with those studies. These low hemoglobin concentration patients commonly also receives packed red cell blood transfusions during their hospital admission. Previous authors considered that the degree of anemia is a marker of underlying comorbid illness burden and physiologic reverse, so it perchance a significant mortality predictor34. The relationship between platelet and hip fracture remains unknown. Only one research has focus on preoperative platelet thresholds in orthopaedic trauma surgery and they found that a notably increased mortality at platelet levels below 150,000 μL, with the largest risk of complications observed at platelet counts < 100,000 μL35. Our results also showed that hip fracture with platelet levels below 100,000 μL had a higher risk of mortality than those ≧ 100,000 μL.
Previous studies also have presented that poor renal function is a predictor of mortality in hip fracture patients36,37,38,39. A study by Gulin et al.40 found that patients less than 85 years of age with eGFR < 55.4 mL/min/1.73 m2 had almost ten times higher mortality rates. A couple of studies denoted eGFR as a predictor of mortality in patients with hip fracture after surgery. According to a multivariate statistical analysis, presented an association between CKD stage 4 (CKD-EPI equation) and higher mortality risk at 1 year41,42. Our study did find that patients who had admission GFR < 60 mL/min/1.73 m2 had a mortality risk 2.01 times greater than those who had GFR more than 60 mL/min/1.73 m2. We considered hemoglobin concentration and GFR level to be modifiable factors. Because these possible causes of low hemoglobin concentration and low GFR level are potentially treatable and could reduce the mortality rate.
There are some limitations in our study. First, because of selection bias, our single-center retrospective study may limit the applicability of the model to other regions. Second, the nomogram showed medium prediction accuracy may suggest that other factors should be included. Some candidate variables were discarded because the missing values were greater than 20%. These may have inevitably caused bias. Finally, our predictive model lacks validation of an external population. Prospective, multicenter or population-based, large sample cohort studies are needed to validate our model further in the future.
Conclusion and future directions
We constructed a convenient nomogram model to predict the postoperatively mortality of hip fracture patients at one-year, based on objective demographics and laboratory results, which can not only assist physicians with reasonable assessments and treatments but also help patients with consultation. The nomogram constructed suggests that age, sex, length of stay, RBC transfusions, hemoglobin, platelet, and eGFR are all significant predictors for one-year postoperative mortality risk in geriatric patients with a hip fracture.
Data availability
The data that support the findings of this study are available from Ditmanson Medical Foundation Chia-Yi Christian Hospital. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the corresponding author with the permission of Ditmanson Medical Foundation Chia-Yi Christian Hospital.
Abbreviations
- CI:
-
Confidence interval
- C-index:
-
Concordance index
- DCA:
-
Decision curve analysis
- DRD:
-
Ditmanson Research Database
- E-PASS:
-
Estimation of Physiologic Ability and Surgical Stress
- HRs:
-
Hazard ratios
- LASSO:
-
Least absolute shrinkage and selection operator
- NHFS:
-
Nottingham Hip Fracture Score
- O-POSSUM:
-
Operative Severity Score for the enUmeration of Mortality and morbidity
- SD:
-
Standard deviation
References
Gullberg, B., Johnell, O. & Kanis, J. A. World-wide projections for hip fracture. Osteoporos. Int. 7, 407–413 (1997).
Curtis, E. M. et al. Epidemiology of fractures in the United Kingdom 1988–2012: Variation with age, sex, geography, ethnicity and socioeconomic status. Bone 87, 19–26 (2016).
Marks, R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970–2009. Int. J. Gen. Med. 3, 1–17 (2010).
Moran, C. G., Wenn, R. T., Sikand, M. & Taylor, A. M. Early mortality after hip fracture: Is delay before surgery important?. J. Bone Joint Surg. Am. 87, 483–489 (2005).
Kimura, A. et al. Predictive factors of mortality of patients with fragility hip fractures at 1 year after discharge: A multicenter, retrospective study in the northern Kyushu district of Japan. J. Orthop. Surg. (Hong Kong). https://doi.org/10.1177/2309499019866965 (2019).
Lee, T. C. et al. One-year readmission risk and mortality after hip fracture surgery: A national population-based study in Taiwan. Aging Dis. 8, 402–409 (2017).
Civinini, R. et al. Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit”. Int. Orthop. 43, 187–192 (2019).
Liu, Y., Wang, Z. & Xiao, W. Risk factors for mortality in elderly patients with hip fractures: A meta-analysis of 18 studies. Aging Clin. Exp. Res. 30, 323–330 (2018).
Karres, J., Heesakkers, N. A., Ultee, J. M. & Vrouenraets, B. C. Predicting 30-day mortality following hip fracture surgery: Evaluation of six risk prediction models. Injury 46, 371–377 (2015).
Karres, J., Eerenberg, J. P., Vrouenraets, B. C. & Kerkhoffs, G. Prediction of long-term mortality following hip fracture surgery: Evaluation of three risk models. Arch. Orthop. Trauma Surg. https://doi.org/10.1007/s00402-022-04646-4 (2022).
Blay-Dominguez, E. et al. O-POSSUM score predicts morbidity and mortality in patients undergoing hip fracture surgery. Rev. Esp. Cir. Ortop. Traumatol. (Engl. Ed.) 62, 207–215 (2018).
Hirose, J., Mizuta, H., Ide, J., Nakamura, E. & Takada, K. E-PASS for predicting postoperative risk with hip fracture: A multicenter study. Clin. Orthop. Relat. Res. 466, 2833–2841 (2008).
Zhang, P. et al. Risk factor analysis for in-hospital death of geriatric hip fracture patients. Saudi Med. J. 43, 197–201 (2022).
Pallardo-Rodil, B., Gomez-Pavon, J. & Menendez-Martinez, P. Hip fracture mortality: Predictive models. Med. Clin. (Barc.) 154, 221–231 (2020).
Olsen, F. et al. Validation of the Nottingham Hip Fracture Score (NHFS) for the prediction of 30-day mortality in a Swedish cohort of hip fractures. Acta Anaesthesiol. Scand. 65, 1413–1420 (2021).
Mula-Abed, W. A., Al-Rasadi, K. & Al-Riyami, D. Estimated glomerular filtration rate (eGFR): A serum creatinine-based test for the detection of chronic kidney disease and its impact on clinical practice. Oman Med. J. 27, 108–113. https://doi.org/10.5001/omj.2012.23 (2012).
Madley-Dowd, P., Hughes, R., Tilling, K. & Heron, J. The proportion of missing data should not be used to guide decisions on multiple imputation. J. Clin. Epidemiol. 110, 63–73 (2019).
Trunfio, T. A., Borrelli, A. & Improta, G. Is it possible to predict the length of stay of patients undergoing hip-replacement surgery?. Int. J. Environ. Res. Public Health 19, 2569. https://doi.org/10.3390/ijerph19106219 (2022).
Nikkel, L. E. et al. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: Retrospective cohort study. BMJ 351, 6246. https://doi.org/10.1136/bmj.h6246 (2015).
Schneider, A. M., Denyer, S. & Brown, N. M. Risk factors associated with extended length of hospital stay after geriatric hip fracture. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 5, e2100073. https://doi.org/10.5435/JAAOSGlobal-D-21-00073 (2021).
Raksakietisak, M. et al. Patients with osteoporotic hip fractures: Factors affecting length of hospital stay (LOS) and outcome. J. Med. Assoc. Thai 95, 917–924 (2012).
Zhou, Z. R. et al. In-depth mining of clinical data: The construction of clinical prediction model with R. Ann. Transl. Med. 7, 796. https://doi.org/10.21037/atm.2019.08.63 (2019).
Balachandran, V. P., Gonen, M., Smith, J. J. & DeMatteo, R. P. Nomograms in oncology: More than meets the eye. Lancet Oncol. 16, e173-180. https://doi.org/10.1016/S1470-2045(14)71116-7 (2015).
Lu, X. et al. A new nomogram model for predicting 1-year all-cause mortality after hip arthroplasty in nonagenarians with hip fractures: A 20-year period retrospective cohort study. Front. Surg. 9, 926745. https://doi.org/10.3389/fsurg.2022.926745 (2022).
Chen, X., Liu, X., Pan, J., You, P. & Ren, S. Preoperative risk factors for predicting postoperative human serum albumin infusion after hip fracture surgery: Development and validation of a nomogram. Balkan Med. J. 40, 40–50 (2023).
Chatterton, B. D., Moores, T. S., Ahmad, S., Cattell, A. & Roberts, P. J. Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint . 97-B, 246–251 (2015).
Kilci, O. et al. Postoperative mortality after hip fracture surgery: A 3 years follow up. PLoS ONE 11, e0162097. https://doi.org/10.1371/journal.pone.0162097 (2016).
Ariza-Vega, P., Kristensen, M. T., Martin-Martin, L. & Jimenez-Moleon, J. J. Predictors of long-term mortality in older people with hip fracture. Arch. Phys. Med. Rehabil. 96, 1215–1221 (2015).
Penrod, J. D. et al. The association of race, gender, and comorbidity with mortality and function after hip fracture. J. Gerontol. A Biol. Sci. Med. Sci. 63, 867–872 (2008).
Wehren, L. E. et al. Gender differences in mortality after hip fracture: The role of infection. J. Bone Miner. Res. 18, 2231–2237 (2003).
Yombi, J. C. et al. Low haemoglobin at admission is associated with mortality after hip fractures in elderly patients. Bone Joint J. 101-B, 1122–1128 (2019).
Praetorius, K. et al. Low levels of hemoglobin at admission are associated with increased 30-day mortality in patients with hip fracture. Geriatr. Orthop. Surg. Rehabil. 7, 115–120 (2016).
Sayed-Noor, A., Al-Amiry, B., Alwan, A., Knutsson, B. & Barenius, B. The association of on-admission blood hemoglobin, C-reactive protein, and serum creatinine with 2-year mortality of patients with femoral neck fractures. Geriatr. Orthop. Surg. Rehabil. 12, 21514593211037760. https://doi.org/10.1177/21514593211037758 (2021).
Halm, E. A. et al. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J. Orthop. Trauma 18, 369–374 (2004).
Varady, N. H., Yeung, C. M., Amen, T. B., Schwab, P. E. & Chen, A. F. Preoperative platelet and international normalized ratio thresholds and risk of complications after primary hip fracture surgery. J. Am. Acad. Orthop. Surg. 29, e396–e403. https://doi.org/10.5435/JAAOS-D-19-00793 (2021).
Akesson, M. H. J., Hommel, A., Grubb, A. A. & Bentzer, P. Markers of renal function at admission and mortality in hip fracture patients—a single center prospective observational study. Scand. J. Clin. Lab. Invest. 81, 201–207 (2021).
Ho, C. A., Li, C. Y., Hsieh, K. S. & Chen, H. F. Factors determining the 1-year survival after operated hip fracture: A hospital-based analysis. J. Orthop. Sci. 15, 30–37 (2010).
Mosfeldt, M. et al. Value of routine blood tests for prediction of mortality risk in hip fracture patients. Acta Orthop. 83, 31–35 (2012).
Bombaci, H. et al. Preoperative indicators affecting postoperative mortality in elderly patients with hip fractures. Acta Orthop. Traumatol. Turc. 46, 425–429 (2012).
Gulin, T. et al. Advanced age, high beta-CTX levels, and impaired renal function are independent risk factors for all-cause one-year mortality in hip fracture patients. Calcif. Tissue Int. 98, 67–75 (2016).
Pajulammi, H. M., Luukkaala, T. H., Pihlajamaki, H. K. & Nuotio, M. S. Decreased glomerular filtration rate estimated by 2009 CKD-EPI equation predicts mortality in older hip fracture population. Injury 47, 1536–1542 (2016).
Khan, S. K., Rushton, S. P., Courtney, M., Gray, A. C. & Deehan, D. J. Elderly men with renal dysfunction are most at risk for poor outcome after neck of femur fractures. Age Ageing 42, 76–81 (2013).
Acknowledgements
This study was supported by grants from the Ditmanson Medical Foundation Chia-Yi Christian Hospital Research Program (R112-01). The authors thank the help from the Clinical Data Center, Ditmanson Medical Foundation Chia-Yi Christian Hospital for providing administrative and technical support. This study is based in part on data from the Ditmanson Research Database (DRD) provided by Ditmanson Medical Foundation Chia-Yi Christian Hospital. The interpretation and conclusions contained herein do not represent the position of Ditmanson Medical Foundation Chia-Yi Christian Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the design of the study, interpretation of the results, and development of the final manuscript. C.Y.W., and H.Y.Y. conceived the study. H.Y.Y. and CFT performed the statistical analyses. C.Y.W., C.F.T., and H.Y.Y. criticized and revised manuscript content. C.Y.W. and H.Y.Y. wrote the manuscript with contributions from all coauthors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, CY., Tsai, CF. & Yang, HY. Utilizing a nomogram to predict the one-year postoperative mortality risk for geriatric patients with a hip fracture. Sci Rep 13, 11091 (2023). https://doi.org/10.1038/s41598-023-38297-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-38297-1
- Springer Nature Limited