Abstract
Introduction
Several prognostic models have been developed for mortality in hip fracture patients, but their accuracy for long-term prediction is unclear. This study evaluates the performance of three models assessing 30-day, 1-year and 8-year mortality after hip fracture surgery: the Nottingham Hip Fracture Score (NHFS), the model developed by Holt et al. and the Hip fracture Estimator of Mortality Amsterdam (HEMA).
Materials and methods
Patients admitted with a fractured hip between January 2012 and June 2013 were included in this retrospective cohort study. Relevant variables used by the three models were collected, as were mortality data. Predictive performance was assessed in terms of discrimination with the area under the receiver operating characteristic curve and calibration with the Hosmer–Lemeshow goodness-of-fit test. Clinical usefulness was evaluated by determining risk groups for each model, comparing differences in mortality using Kaplan–Meier curves, and by assessing positive and negative predictive values.
Results
A total of 344 patients were included for analysis. Observed mortality rates were 6.1% after 30 days, 19.1% after 1 year and 68.6% after 8 years. The NHFS and the model by Holt et al. demonstrated good to excellent discrimination and adequate calibration for both short- and long-term mortality prediction, with similar clinical usefulness measures. The HEMA demonstrated inferior prediction of 30-day and 8-year mortality, with worse discriminative abilities and a significant lack of fit.
Conclusions
The NHFS and the model by Holt et al. allowed for accurate identification of low- and high-risk patients for both short- and long-term mortality after a fracture of the hip. The HEMA performed poorly. When considering predictive performance and ease of use, the NHFS seems most suitable for implementation in daily clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are associated with high mortality and represent a significant burden on both patients and healthcare systems [1,2,3]. As life expectancy continues to increase worldwide, so does the impact of hip fractures on our society [4, 5]. Patient characteristics related to high mortality following a fracture of the hip are well established and include age, gender, comorbidities and pre-fracture residency and mobility [6,7,8,9]. However, mortality risk assessment for the individual patient at the time of admission remains a challenge.
Risk prediction models can help identify hip fracture patients with a high or low probability of survival. Validated prognostic tools could be used to counsel patients and their families on prognosis, guide clinical decision making and inform surgeons and anaesthesiologists. Furthermore, prediction models can correct for differences in baseline variables and be of value when comparing quality of care between caregivers, hospitals or different time periods.
Several models for predicting mortality after hip fracture surgery have been developed. In our evaluation of six prediction models, the Nottingham Hip Fracture Score (NHFS) and the model by Holt and colleagues [10, 11] showed promising results but demonstrated a lack of fit, indicating a possible need for recalibration [12]. Our subsequently developed prediction model, the Hip fracture Estimator of Mortality Amsterdam (HEMA), demonstrated reasonable predictive performance but has not yet undergone external validation [13].
The NHFS, the model by Holt et al. and the HEMA all demonstrate adequate prediction of early mortality after hip fracture surgery in initial studies. For a risk model to be useful in clinical practice, however, external validation is required [14, 15]. Furthermore, the ability of these models to predict long-term mortality after a fracture of the hip has yet to be determined.
The aim of this study is to evaluate these risk prediction models for mortality in hip fracture patients and to compare their predictive performance for short- and long-term mortality.
Patients and methods
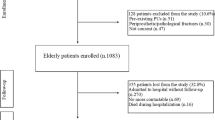
This retrospective cohort study included all patients with a fractured hip admitted to the Tergooi hospital between January 2012 and June 2013. This hospital is a level 2 trauma centre located in Hilversum, The Netherlands. Surgical treatment was in accordance to current national guidelines. Patients with a periprosthetic femoral fracture or slipped capital femoral epiphysis were excluded, as were severe trauma patients (Injury Severity Score ≥ 16) and patients who were treated non-operatively. Three risk prediction models for mortality were evaluated.
Nottingham Hip Fracture Score
The NHFS was developed in 2008 and underwent recalibration in 2012 to correct for overestimation of mortality in high-risk groups [11, 16]. The NHFS consists of seven variables and calculates the risk of mortality after hip fracture surgery using age, gender, serum haemoglobin, Abbreviated Mental Test Score (AMTS), whether the patient is living in an institution, the number of comorbidities and a history of malignancy. Between 1 and 4 points are attributed to each variable, with a maximum score of 10. Several studies evaluating the NHFS have proposed classification of patients into risk groups based on the aggregate score [17,18,19].
Holt et al.
Holt and colleagues used data from the Scottish Hip Fracture Audit to analyse variables associated with mortality in hip fracture patients [10]. In their 2008 paper, the authors propose a prediction formula using preoperative variables and their logistic regression coefficients. The prediction model uses six variables to predict mortality after hip fracture surgery: age, American Society of Anesthesiologists (ASA) score, gender, pre-fracture residence, pre-fracture mobility and fracture type. Each variable has multiple subdivisions with according scores.
Hip fracture estimator of mortality Amsterdam
We developed the HEMA in 2018 using nine variables to estimate mortality after hip fracture surgery: age, in-hospital fracture, signs of malnutrition, a history of myocardial infarction, congestive heart failure, renal failure, malignancy, current pneumonia and serum urea level [13]. Between 0.5 and 2 points are scored for each variable. Patients can be classified into low-, intermediate- and high-risk groups based on cumulative scores.
Data for the models were retrospectively collected from digital and paper medical records. Patient characteristics and comorbidities were recorded, as were laboratory results and operative variables. Individual mortality risk predictions by the three models were calculated for all patients. A history of cognitive impairment was used as a substitute for the AMTS, since this score was not available for the patients in our dataset. Any other missing values were not substituted but scored as negative in the calculation of individual mortality risks, reflecting the use of a prediction model in daily clinical practice.
The primary outcome of this study was mortality. Individual survival data were verified using the hospital’s administration records and through national databases. Thirty-day mortality was defined as death within 30 days following hip fracture surgery. To evaluate long-term survival and prediction, 1-year and 8-year mortality were assessed. Eight-year mortality was chosen as the endpoint for this study based on average life expectancies in the Netherlands. In 2012, life expectancy was 7.4 years for men and 9.1 years for women at age 81 [20]. This retrospective study and the use of clinical data was approved by the local ethical review board of our hospital. Due to the retrospective and observational nature of the research, individual informed consent was not required.
Statistical analysis
Discrimination, calibration and clinical usefulness were analysed to assess predictive performance of the three models.
Discrimination is the ability of a model to separate patients who experienced the designated outcome from those who did not. It was evaluated using the Area Under the receiver operating characteristic Curve (AUC) [21]. Perfect discrimination is represented by an AUC of 1.00 whereas random predictions would result in an AUC of 0.50. When assessing mortality prediction, an AUC of 0.70 or higher is considered adequate discrimination, and an AUC ≥ 0.80 is considered good [22].
Calibration is a measure of how well predictions agree with observed outcomes. It was assessed using the Hosmer–Lemeshow goodness-of-fit test, which divides cases into prediction deciles and compares predicted versus observed mortality rates within these groups [23]. The Hosmer–Lemeshow test is significant when the differences are greater than would be expected by chance, indicating a lack of fit [23].
Clinical usefulness refers to a model’s capacity to aid in clinical decision making and depends on correct classification of patients [15, 24]. It was evaluated by determining low-, intermediate- and high-risk groups for each model based on cumulative scores and predicted mortality rates. Differences in mortality between risk groups were assessed with Kaplan–Meier curves, plotting survival after hip fracture surgery over time. Additionally, the positive predictive value (PPV) and negative predictive value (NPV) were evaluated for high-risk and low-risk groups, respectively. PPV is defined as the likelihood that a person with a positive result truly has the designated outcome; it is the probability of death for a patient in the high-risk group. NPV refers to the probability of survival for a patient in the low-risk group.
A p value of < 0.05 was considered statistically significant. All analyses were performed with SPSS Statistics, version 26.0 (IBM, NY, USA).
Results
A total of 344 surgically treated patients with a fractured hip were included between January 2012 and June 2013. Patient characteristics and operative variables are described in Table 1. Median age was 81 years, 70.3% of patients were female, and the majority of patients had an ASA score of 2 (52.9%) or 3 (28.2%). Most patients were operated on the day following admission. Twenty-one patients (6.1%) died within 30 days following hip fracture surgery. Mortality rates were 19.1% after 1 year and 68.6% after 8 years (Table 1).
Variables for the three prediction models are described in Table 2, as are their respective cut-off values and attributed points. Prevalence of the variables as a proportion of the total dataset is reported as well. The NHFS uses seven variables and has a subdivision for age, attributing 0 to 4 points per value. The model by Holt et al. uses six variables with 23 subdivisions, attributing either positive or negative values to two decimal places for each option. The HEMA uses nine variables with no further subdivision and attributes between 0 and 2 points. With all models, risk prediction as a percentage can be calculated with the cumulative point scores and the logistic regression formula (Table 2).
Discrimination
Table 3 displays performance measures of the three prognostic models. There was a statistically significant difference in discrimination between the model by Holt et al. and the HEMA for 30-day mortality (p = 0.039). There were no significant differences between the NHFS and the other two models for 30-day mortality. Discrimination for 1-year mortality did not differ significantly between the three prediction models. Discriminative performances of both the NHFS and the model by Holt et al. were significantly better than that of the HEMA when predicting 8-year mortality (p < 0.001).
Calibration
The NHFS and the model by Holt et al. demonstrated adequate calibration for 30-day, 1-year and 8-year mortality. The Hosmer–Lemeshow goodness-of-fit test was significant for the HEMA in 30-day and 8-year mortality predictions, indicating a lack of fit (Table 3).
Clinical usefulness
Table 4 describes classification of risk groups using cut-off values for cumulative scores and predicted mortality rates. Risk groups and their proportion in the dataset are described (Table 4). Positive predictive values for the high-risk groups and negative predictive values for the low-risk groups are reported. Death rates in the high-risk group ranged between 14.9 and 17.9% after 30 days and between 40.5 and 48.7% after 1 year. At 8 years, mortality rates in the high-risk group resulted in a PPV of 94.5–98.6%. Survival in the low-risk group was 96.8–100% after 30 days, 89.1–95.4% after 1 year and 40.5–74.7% after 8 years (Table 3). The Kaplan–Meier curves displayed in Fig. 1 graph cumulative survival for low-, intermediate-, and high-risk groups for each risk prediction model over the 8-year period.
Discussion
This external validation study evaluates the performance of three risk prediction models mortality following hip fracture surgery: the NHFS, the model by Holt et al. and the HEMA. Thirty-day, 1-year and 8-year mortality were assessed.
When predicting 30-day mortality, the NHFS and the model by Holt et al. demonstrated good discriminative ability. The HEMA showed adequate discrimination, but performed significantly worse than the model by Holt et al. Furthermore, the HEMA had a significant lack of fit. At 30 days, positive predictive values were limited for all risk models. Negative predictive values were high, particularly for the NHFS; all low-risk patients survived after 30 days.
One-year mortality prediction was similar between the three models. Discrimination was adequate without significant differences, and all models demonstrated sufficient calibration. While the PPV increased, the NPV decreased only slightly.
Prediction of 8-year mortality by the NHFS and the model by Holt et al. resulted in good to excellent discrimination and adequate calibration. The HEMA performed poorly with inferior discriminative abilities and a significant miscalibration. The PPV was high for all models. The NPV decreased most notably in the HEMA where only 40.5% of low-risk patients survived after 8 years. In contrast, 8-year survival rates of low-risk patients were 72.4% and 74.7% for NHFS and the model by Holt et al., respectively.
The NHFS has been validated in numerous papers for both 30-day and 1-year mortality [25,26,27,28,29]. It is the most commonly studied prediction model for mortality in hip fracture patients and frequently demonstrates adequate predictive performance in line with our findings, although several authors have reported on the need for recalibration [16, 18, 30]. With only seven variables, the NHFS is easy to use and even available as a smart phone application [31]. The inclusion of the Abbreviated Mental Test Score makes implementation slightly more complex, leading to some suggesting substitution of the variable with a history of cognitive impairment [32].
The model by Holt and colleagues was developed around the same time as the NHFS but did not receive the same level of attention, despite similar predictive qualities [10, 12]. This might be due to a few issues [33]. First, the model lacks a proper name. Second, no follow-up studies were undertaken to validate the model. Last, its many subdivisions and intricate scoring system might preclude use in daily clinical practice, where time is often limited.
The HEMA was developed by us more recently and while initial results were promising, no external validation was undertaken until now [13]. In this current study, the HEMA demonstrates poor predictive performance when compared to both other models, which might be attributed to several factors. A model developed in a cohort with relatively few cases is at risk of containing variables with high impact but rare occurrence, leading to less reliable predictions [34, 35]. The HEMA uses multiple uncommon variables such as in-hospital fracture and pneumonia at admission. Additionally, several well established risk factors used by other prediction models, such as gender and pre-fracture residency, are markedly absent from the HEMA model. In this study, the lesser performance of the HEMA is reflected in inferior discrimination and a lack of fit for both short- and long-term mortality predictions, as well as in its limited ability of identifying low-risk patients.
Recent years have seen an abundance of publications on risk prediction models for mortality in hip fracture patients [28, 32, 36,37,38,39,40,41]. Although new models are proposed every year, their added benefit to patient care remains unclear, since these models have not yet proven their worth in daily clinical practice [42]. A prediction model is only of value when it can assist patients and caregivers in clinical decision making. To accomplish this, adequate identification of high- and low-risk patients is essential.
Identification of hip fracture patients at high risk of early mortality remains challenging. In our study, the majority of patients in high-risk groups were alive after 1 year. If risk models are to be used for guidance in end-of-life discussions with patients and their families about treatment options and the possibility of palliative care, accurate identification of patients at very high risk of early mortality is crucial. It seems that as of now, however, no risk prediction model is able to identify this small subgroup of patients.
Identifying low-risk patients has been more promising. In our study, the low-risk subgroups of the NHFS and model by Holt et al. consisted of about a third of all patients. After 8 years, their chance of survival was more than two times higher than average. The difference in mortality between risk groups was most prominent in the NHFS, where the 8-year survival rate of low-risk patients was around 50 times higher than that of high-risk patients (72.4% versus 1.4%). Validated long-term predictions for low-risk patients might make models suitable for aiding in clinical decision making, e.g. when considering hemiarthroplasty versus total hip arthroplasty in the treatment of displaced intracapsular hip fractures [43].
There are several limitations to this study. Due to its retrospective nature, the AMTS was not available for our population. The variable was replaced by cognitive impairment, an independent risk factor for mortality in hip fracture patients and well documented in our medical records [32, 44]. Additionally, sample size was limited due to an 18-month period. Small sample size would be particularly detrimental for development of a risk model, however, less so for validation purposes [45]. Strengths of this study include its comprehensive assessment of risk models and their predictive performance. The evaluation of clinical usefulness measures using risk groups provides useful additional information for clinical decision making. Lastly, completeness of long-term survival data allowed for accurate analysis and visualisation using Kaplan–Meier curves.
Conclusion
To our knowledge, this is the first study examining mortality predictions in hip fracture patients over such an extended period of time. The HEMA demonstrated inferior predictive performance. The NHFS and the model by Holt et al. were reliable prediction models for short- and long-term mortality following a fracture of the hip. Both models allowed for adequate identification of low- and high-risk patients. The NHFS combines accurate prediction with ease of use and has been validated in multiple external validation studies. Further research should focus on the implementation of the NFHS in daily practice and study its ability to improve on clinical decision making.
References
Prieto-Alhambra D, Moral-Cuesta D, Palmer A, Aguado-Maestro I, Bardaji MFB, Brañas F et al (2019) The impact of hip fracture on health-related quality of life and activities of daily living: the SPARE-HIP prospective cohort study. Arch Osteoporos 14:56
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Veronese N, Maggi S (2018) Epidemiology and social costs of hip fracture. Injury 49:1458–1460
Abrahamsen B, Laursen HVB, Skjødt MK, Jensen MH, Vestergaard P (2020) Age at hip fracture and life expectancy in Denmark—secular trends over two decades. Bone 130:115083
Chen IJ, Chiang CY, Li YH, Chang CH, Hu CC, Chen DW et al (2015) Nationwide cohort study of hip fractures: time trends in the incidence rates and projections up to 2035. Osteoporos Int 26:681–688
Xu BY, Yan S, Low LL, Vasanwala FF, Low SG (2019) Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review. BMC Musculoskelet Disord 20:568
Chang W, Lv H, Feng C, Yuwen P, Wei N, Chen W et al (2018) Preventable risk factors of mortality after hip fracture surgery: systematic review and meta-analysis. Int J Surg 52:320–328
Smith T, Pelpola K, Ball M, Ong A, Myint PK (2014) Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing 43:464–471
Hu F, Jiang C, Shen J, Tang P, Wang Y (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 43:676–685
Holt G, Smith R, Duncan K, Finlayson DF, Gregori A (2008) Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the scottish hip fracture audit. J Bone Joint Surg Br 90:1357–1363
Maxwell MJ, Moran CG, Moppett IK (2008) Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth 101:511–517
Karres J, Heesakkers NA, Ultee JM, Vrouenraets BC (2015) Predicting 30-day mortality following hip fracture surgery: evaluation of six risk prediction models. Injury 46:371–377
Karres J, Kieviet N, Eerenberg JP, Vrouenraets BC (2018) Predicting early mortality after hip fracture surgery: the hip fracture estimator of mortality Amsterdam. J Orthop Trauma 32:27–33
Cowley LE, Farewell DM, Maguire S, Kemp AM (2019) Methodological standards for the development and evaluation of clinical prediction rules: a review of the literature. Diagn Progn Res 3:16
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N et al (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138
Moppett IK, Parker M, Griffiths R, Bowers T, White SM, Moran CG (2012) Nottingham Hip Fracture Score: longitudinal and multi-assessment. Br J Anaesth 109:546–550
Lisk R, Yeong K, Fluck D, Fry CH, Han TS (2020) The ability of the Nottingham hip fracture score to predict mobility, length of stay and mortality in hospital, and discharge destination in patients admitted with a hip fracture. Calcif Tissue Int 107:319–326
Rushton PR, Reed MR, Pratt RK (2015) Independent validation of the Nottingham Hip Fracture Score and identification of regional variation in patient risk within England. Bone Jt J. 97-b:100–103
Chinoy MA, Gulzar Naqvi SZ, Khan MA, Ahmed SK, Muhammad MG (2020) Nottingham Hip Fracture Score as a predictor of 3 months postoperative mortality in patients undergoing surgical fixation of hip fractures: a prospective study. J Pak Med Assoc 70(Suppl 1):S3-s5
CBS Statistics Netherlands. Life expectancy; gender, age. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/37360ned Accessed 29 Sep 2022.
Steyerberg EW, Vergouwe Y (2014) Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J 35:1925–1931
von Meijenfeldt GC, van Beek SC, Bastos Gonçalves F, Verhagen HJ, Zeebregts CJ, Vahl AC et al (2017) Development and external validation of a model predicting death after surgery in patients with a ruptured abdominal aortic aneurysm: the Dutch aneurysm score. Eur J Vasc Endovasc Surg 53:168–174
Lemeshow S, Hosmer DW Jr (1982) A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol 115:92–106
Vergouwe Y (2003) Validation of clinical prediction models: theory and applications in testicular germ cell cancer [Ph.D. thesis]: Erasmus University Rotterdam
Marufu TC, Mannings A, Moppett IK (2015) Risk scoring models for predicting peri-operative morbidity and mortality in people with fragility hip fractures: qualitative systematic review. Injury 46:2325–2334
Pallardo Rodil B, Gómez Pavón J, Menéndez MP (2020) Hip fracture mortality: predictive models. Med Clin (Barc) 154:221–231
Thorne G, Hodgson L (2021) Performance of the Nottingham Hip Fracture Score and Clinical Frailty Scale as predictors of short and long-term outcomes: a dual-centre 3-year observational study of hip fracture patients. J Bone Miner Metab 39(3):494–500.https://doi.org/10.1007/s00774-020-01187-x
Menéndez-Colino R, Gutiérrez Misis A, Alarcon T, Díez-Sebastián J, Díaz de Bustamante M, Queipo R et al (2020) Development of a new comprehensive preoperative risk score for predicting 1-year mortality in patients with hip fracture: the HULP-HF score. Comparison with 3 other risk prediction models. Hip Int 31(6):804–811. https://doi.org/10.1177/1120700020947954
Wiles MD, Moran CG, Sahota O, Moppett IK (2011) Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br J Anaesth 106:501–504
Doherty WJ, Stubbs TA, Chaplin A, Reed MR, Sayer AA, Witham MD et al (2021) Prediction of postoperative outcomes following hip fracture surgery: independent validation and recalibration of the Nottingham hip fracture score. J Am Med Dir Assoc 22:663–9.e2
News: There is now an app for The Nottingham Hip Fracture Score. 2013.
Nijmeijer WS, Folbert EC, Vermeer M, Slaets JP, Hegeman JH (2016) Prediction of early mortality following hip fracture surgery in frail elderly: the Almelo Hip Fracture Score (AHFS). Injury 47:2138–2143
Cook DA, Bordage G (2016) Twelve tips on writing abstracts and titles: how to get people to use and cite your work. Med Teach 38:1100–1104
Van Calster B, McLernon DJ, van Smeden M, Wynants L, Steyerberg EW (2019) Calibration: the Achilles heel of predictive analytics. BMC Med 17:230
Van Calster B, Nieboer D, Vergouwe Y, De Cock B, Pencina MJ, Steyerberg EW (2016) A calibration hierarchy for risk models was defined: from utopia to empirical data. J Clin Epidemiol 74:167–176
Harman H, Walton TJ, Chan G, Stott P, Ricketts DM, Rogers BA (2021) Predicting 30-day mortality after hip fracture: the G4A calibrated prognostic tool. Hip Int. https://doi.org/10.1177/1120700021998959
Schuijt HJ, Smeeing DPJ, Würdemann FS, Hegeman JH, Geraghty OC, Houwert RM et al (2020) Development and internal validation of a prediction model for in-hospital mortality in geriatric patients with a hip fracture. J Orthop Trauma 34:656–661
van de Ree CL, Gosens T, van der Veen AH, Oosterbos CJ, Heymans MW, de Jongh MA (2020) Development and validation of the Brabant Hip Fracture Score for 30-day and 1-year mortality. Hip Int 30:354–362
Traven SA, Reeves RA, Althoff AD, Slone HS, Walton ZJ (2019) New five-factor modified frailty index predicts morbidity and mortality in geriatric hip fractures. J Orthop Trauma 33:319–323
Endo A, Baer HJ, Nagao M, Weaver MJ (2018) Prediction model of in-hospital mortality after hip fracture surgery. J Orthop Trauma 32:34–38
Bliemel C, Sielski R, Doering B, Dodel R, Balzer-Geldsetzer M, Ruchholtz S et al (2016) Pre-fracture quality of life predicts 1-year survival in elderly patients with hip fracture-development of a new scoring system. Osteoporos Int 27:1979–1987
Dawe H (2017) Modernising hip fracture anaesthesia. Open Orthop J 11:1190–1199
Ekhtiari S, Gormley J, Axelrod DE, Devji T, Bhandari M, Guyatt GH (2020) Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fracture: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am 102:1638–1645
Chiu HC, Chen CM, Su TY, Chen CH, Hsieh HM, Hsieh CP et al (2018) Dementia predicted one-year mortality for patients with first hip fracture: a population-based study. Bone Jt J. 100-b:1220–1226
Wynants L, Bouwmeester W, Moons KG, Moerbeek M, Timmerman D, Van Huffel S et al (2015) A simulation study of sample size demonstrated the importance of the number of events per variable to develop prediction models in clustered data. J Clin Epidemiol 68:1406–1414
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the hospital’s ethical review board.
Informed consent
Individual informed consent was not required due to the retrospective and observational nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Karres, J., Eerenberg, JP., Vrouenraets, B.C. et al. Prediction of long-term mortality following hip fracture surgery: evaluation of three risk models. Arch Orthop Trauma Surg 143, 4125–4132 (2023). https://doi.org/10.1007/s00402-022-04646-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04646-4