Abstract
We analyzed the effects of bicruciate-retaining total knee arthroplasty (BCR-TKA) on knee kinematics and cruciate ligament forces. Patients (N = 15) with osteoarthritis (OA) and an intact anterior cruciate ligament (ACL) underwent magnetic resonance imaging and single-plane fluoroscopy to measure tibiofemoral kinematics during two deep knee bend activities before and after BCR-TKA: (1) weight-bearing squat; (2) non-weight-bearing cross-legged sitting. Forces in ligament bundles were calculated using VivoSim. The dynamic range of varus-valgus angulation decreased from 3.9 ± 4.4° preoperatively to 2.2 ± 2.7° postoperatively. Preoperatively, the medial femoral condyle translated anteriorly from 10° to 50° of flexion, and posteriorly beyond 50° of flexion. Postoperatively, the medial and lateral femoral condyles translated posteriorly throughout flexion in a medial pivot pattern. ACL forces were high in extension and decreased with flexion pre- and postoperatively. PCL forces increased with flexion preoperatively and did not change significantly postoperatively. Preoperatively, ACL forces correlated with anteroposterior translation of the femoral condyles. Postoperatively, PCL forces correlated with anteroposterior translation of the lateral femoral condyle. BCR-TKA altered knee kinematics during high flexion activity which correlated significantly with changes in cruciate ligament forces.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) induces significant changes in knee kinematics1,2. While total knee arthroplasty (TKA) is successful in relieving pain and partially restoring function, cruciate-retaining, cruciate-sacrificing, and cruciate-substituting TKA designs do not restore normal knee kinematics3. These abnormal kinematics have been attributed to the sacrifice of the anterior cruciate ligament. Bicruciate-retaining total knee arthroplasty (BCR-TKA) designs attempt to recreate normal knee movement by preserving both the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL). Studies have found that knees that underwent BCR-TKA exhibited kinematics and stability similar to normal knees4,5,6,7. A few studies have also reported favourable patient satisfaction and long-term survivorship and function of knees after BCR-TKA8,9,10. However, not all reports have been universally positive. Studies have reported that clinical outcomes after BCR-TKA did not differ from the outcomes reported for knees that underwent ACL-sacrificing TKA11,12. Moreover, several studies demonstrated that knee kinematics during treadmill walking after BCR-TKA were not the same as normal knees and that anterior cruciate ligament forces were higher in cadavers implanted with BCR-TKA13,14. However, the change in knee kinematics and cruciate ligament force after BCR-TKA is largely unknown. Moreover, the relationship between knee kinematics and cruciate ligament force remains unknown.
Many people desire the ability to perform high knee flexion activities such as squatting, kneeling, gardening, sitting on the floor, or practicing yoga. Additionally, studies have linked high knee flexion function to clinical outcomes, patient satisfaction, or expectation after TKA15,16. Therefore, evaluating high knee flexion activities is clinically relevant. A previous study demonstrated that knee kinematics after BCR-TKA differed depending on the type of high-flexion activities17. However, whether the cruciate ligament force in BCR-TKA knees differs depending on the high-flexion activities remains unknown.
This study was designed to analyze the effects of BCR-TKA implantation on knee kinematics and cruciate ligament force during high knee flexion activities and to determine if knee kinematics were linked to cruciate ligament forces. We therefore studied two types of high flexion activities: a closed-kinetic chain deep knee bend (squatting) and an open-kinetic chain high flexion (sitting cross-legged). Our null hypothesis was that implantation with a BCR-TKA and the type of high knee flexion activity would not change kinematics or ligament forces in the cruciate ligaments.
Results
All components of KOOS increased significantly postoperatively; HKA angle also increased from 172° to 178° (Table 1).
Kinematic changes
Preoperatively knee flexion ranged from 0.3 ± 8.3° to 118.7 ± 12.4° during squatting. Postoperative knee flexion ranged from –4.7 ± 4.3° to 115.7 ± 12.4° during squatting and from –1.7 ± 2.3° to 115.7 ± 12.4° during cross-legged sitting. Maximum knee extension, but not knee flexion, increased significantly postoperatively (p = 0.02).
During squatting, the femur rotated externally relative to the tibia before and after BCR-TKA (Fig. 1A). The net range of external rotation of the femur reduced from 9.7 ± 4.8° preoperatively to (2.3 ± 4.8°) after BCR-TKA. In early flexion, the BCR femoral component was more externally rotated relative to the preoperative femoral rotation. During postoperative cross-legged sitting, relative to the rotation in extension, the femur rotated internally up to 70° of flexion, followed by external rotation beyond 70° of flexion. From 80° to 110° of flexion, the femoral external rotation during squatting was greater than that during cross-legged sitting (Fig. 2A).
BCR implantation also significantly changed varus-valgus angulation during the squatting activity (Fig. 1B). In extension, the varus angulation reduced from an average of 9.1 ± 4.5° to 0.3 ± 1.5°. BCR implantation also affected the change in varus angulation with flexion. With further flexion, preoperatively, the knees angulated toward less varus; while postoperatively, the knees angulated toward greater varus. The dynamic range of varus-valgus angulation was also significantly different: decreasing from a total range of 3.9 ± 4.4° preoperatively to 2.2 ± 2.7° postoperatively. There were minimal differences in varus-valgus angulation with cross-legged sitting except at maximum flexion that resulted in greater varus angulation than squatting (Fig. 2B).
AP translation
To analyze femoral rollback and to identify the pivot pattern, we tracked the AP positions of the medial and lateral femoral condyles relative to the proximal tibial plane (Figs. 3 and 4). The relative translation of the femoral condyles is reflected in the shape of the curves in Figs. 3 and 4. While squatting preoperatively, the medial femoral condyle translated further anteriorly from 10° to 50° of flexion (3.9 ± 9.8%), and changed towards relative posterior translation beyond 50° of flexion (17.0 ± 8.2%). On the other hand, postoperatively, the medial femoral condyle translated relatively posteriorly throughout flexion for a total of 12.0 ± 10.9%. The net translation was computed as the difference between AP position in extension and that in flexion. Sitting cross-legged resulted in greater net posterior translation of the medial femoral condyle (total of 17.9 ± 11.4% posterior translation) than squatting (Fig. 4A).
The lateral femoral condyle translated posteriorly with flexion resulting in a medial pivot pattern, although the net posterior translation reduced postoperatively (range of 41.1 ± 10.5%, preoperatively; 21.9 ± 7.1% postoperatively, Fig. 3B). While squatting, the femur was more posteriorly located than during cross-legged sitting from 40° to maximum flexion (Fig. 4B).
Cruciate ligament forces
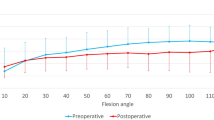
To analyze the effect of BCR design on cruciate ligaments, we calculated tensile forces generated during squatting and cross-legged sitting. Tension in both bundles of the ACL was highest in extension preoperatively and remained high postoperatively. Postoperatively, however, at 30° of flexion, greater forces were generated in the pACL (p = 0.04, Fig. 5). Squatting generated greater tension in the aACL bundle than did cross-legged sitting at 40° of flexion (Fig. 6, p = 0.04).
Anterior cruciate ligament (ACL) force during postoperative activities in bicruciate-retaining total knee arthroplasty: (A) Anteromedial bundle of the ACL (aACL); (B) Posterolateral bundle of the ACL (pACL). *A significant difference between knees during squatting and knees during cross-legged sitting (p ≤ 0.05).
In contrast to the ACL, tension in both PCL bundles increased with flexion and did not change significantly postoperatively, or with activity (Figs. 7 and 8).
Correlation between the kinematics and cruciate ligament force
We used linear regression to determine whether knee kinematic patterns were associated with ligament tensile forces (Table 2). Preoperatively the ACL forces in both bundles correlated highly with the AP translation of the medial and lateral femoral condyles during squatting. Whereas, postoperatively the PCL forces correlated highly AP translation of lateral femoral condyle during postoperative squatting.
Discussion
We analyzed the effects of bicruciate-retaining total knee arthroplasty (BCR-TKA) on knee kinematics and cruciate ligament forces in order to identify changes induced postoperatively and to correlate knee kinematics with forces in the cruciate ligaments. The most important findings of this study were that (1) BCR-TKA reduced femoral external rotation and AP translation with flexion; (2) Preoperatively, ACL forces correlated highly with AP translation of the femur during squatting; and (3) Postoperatively, only PCL forces correlated highly with AP translation of the lateral femoral condyle during squatting.
OA of the knee significantly affects knee kinematics1,2,18. These kinematic changes were not fully restored after traditional ACL-sacrificing surgery3. While BCR designs have been developed to retain the ACL, BCR-TKA also does not restore normal knee kinematics13,19,20. Our previous study demonstrated that knees after BCR-TKA with an anatomical articular surface showed lower femoral external rotation and lateral posterior translation with flexion than normal knees during squatting19. Normal knees during squatting displayed large femoral external rotation at early-flexion called screw-home movement21,22, and medial-pivot motion followed by femoral rollback22. In a cadaveric study, Hamada et al. reported that the screw-home movement of the intact knee was retained after initial implantation of the BCR-TKA femoral component but was lost after the BCR-TKA tibial component was implanted23.
Knee kinematic patterns are highly relevant to clinical outcomes. Van Onsem et al. reported that patients with a poor patient-reported outcome measure (PROM) after TKA experience more anterior translation on the medial side followed by a medial mid-flexion instability and less posterior translation on the lateral side in high-flexion than patients with good PROM scores24. Twiggs et al. reported a varus angular change from 10° to 90° flexion of between 0° and 4° had a significant improvement in postoperative KOOS pain score in cruciate-retaining TKA (CR-TKA)25. In our study, BCR-TKA eliminated the anterior translation of the medial condyle, preserved the medial pivot pattern, and corrected the preoperative varus angulation. Improvement in the positive features of knee kinematics during high flexion activities may improve PROM scores after BCR-TKA.
ACL forces were high only in the early range of flexion. Preoperatively, posterior translation of the femur positively correlated with higher ACL force during squatting. Postoperatively, the high ACL force in early flexion and consistent posterior femoral translation during flexion indicated that the ACL was actively providing stability against paradoxical anterior translation. Okada et al. found the ACL in situ force against 100 N of anterior force in BCR-TKA knees to be statistically comparable with that in intact knees at all flexion angles13. Furthermore, Sabouret et al. reported that ACL-retaining TKA remained functional and provided adequate stability at the 22-year follow-up26. These results support the positive influence of ACL retention in BCR-TKA on clinical outcomes.
Forces in the PCL increased with flexion and posterior translation of the lateral femoral condyle correlated with reduced PCL force during postoperative squatting. Tsai et al. reported that the PCL in BCR-TKA with symmetrical articular surfaces was significantly overstretched in deep flexion positions27. These results were similar to a prior study of CR-TKA28, which also reported overstretching of the PCL in CR TKA during deep flexion. This overstretching was attributed to reduced femoral rollback secondary to kinematic conflict. The BCR-TKA design used in our study had an anatomical articular surface, which presumably reduced kinematic conflict and reduced the potential for overstretching of the PCL.
The type of high-flexion activity also had an effect on knee kinematics. Squatting induced greater femoral external rotation and cross-legged sitting generated more varus angulation at maximum flexion, as we have previously reported17. In addition, this kinematic difference, depending on the type of high-flexion activity, was similar to that of normal knees22. ACL forces during cross-legged sitting also tended to be lower than those during squatting. Henning et al. reported significant differences in ACL strain between closed-kinetic-chain and open-kinetic-chain activities29. Therefore, different types of high-flexion activities are likely to have distinct effects on ACL forces.
This study has some limitations. First, the study did not directly compare BCR-TKA with ACL-sacrificing designs. However, the kinematics of ACL-sacrificing designs have been extensively documented. Second, the study cohort had a relatively short mean follow-up duration of 8.1 months. Kinematics and ligament forces at longer-term follow-up may differ from those of this study.
This is the first study to report in vivo ligament forces before and after BCR-TKA. BCR-TKA resulted in significant changes in knee kinematics during deep knee bend activities. These kinematic changes correlated significantly with changes in cruciate ligament forces. These results are valuable to develop appropriate ligament balancing strategies and to enhance and develop BCR knee designs.
Methods
A total of 15 knees in 13 patients (3 males and 10 females), who underwent BCR-TKA (Journey II XR, Smith & Nephew, Memphis, TN, USA), were enrolled in this study. The patients provided informed consent to participate in the study after institutional review board approval (provided by The University of Tokyo Institutional Ethics Review Board). The following methods were carried out in accordance with relevant guidelines and regulations.
Knee kinematics were recorded fluoroscopically while each patient performed a closed-kinetic chain deep knee bend (squatting) and an open-kinetic chain high flexion activity (sitting cross-legged)17. Preoperative kinematics (within one month of surgery) were recorded during squatting. Postoperative kinematics (at least six months after BCR-TKA) were recorded during squatting and sitting cross-legged. Kinematics during cross-legged sitting were not recorded preoperatively, as most patients found it painful to perform this activity. The activity was performed at a natural pace under fluoroscopic surveillance in the sagittal plane. The mean duration of postoperative follow-up was 8.1 ± 8.2 months. At postoperative fluoroscopic analysis, the mean age was 72.3 ± 5.9 years. The mean body height was 157.4 ± 6.9 cm and the mean body weight was 60.2 ± 7.9 kg. All patients underwent BCR-TKA to treat bicompartmental or tricompartmental OA with an intact ACL. Presence of an intact ACL was confirmed using preoperative magnetic resonance imaging (MRI). The Knee Injury and Osteoarthritis Outcome Scores (KOOS)30,31 and hip-knee-ankle angle (HKA) were recorded pre- and postoperatively (Table 1). The sequential motion was recorded as a series of digital X-ray images (1024 × 1024 × 12 bits/pixel, 7.5-Hz serial spot images as a DICOM file) using a 17-inch (43-cm) flat panel detector system (ZEXIRA DREX-ZX80, Toshiba, Tokyo, Japan). Furthermore, all images were processed by dynamic range compression, thereby enabling edge-enhanced images. To estimate the spatial position and orientation of the knee automatically, a two-dimensional/three-dimensional (2D/3D) registration technique32 was employed based on a contour-based registration algorithm using single-view fluoroscopic images and 3D computer-aided design (CAD) models. The estimated accuracy of relative motion between metal components was ≤ 0.5° in rotation and ≤ 0.4 mm in translation32.
We used the same local coordinate system for preoperative and postoperative analysis by constructing 3D bone models from preoperative and postoperative computed tomography (CT) scans. In BCR-TKA knees, extraction of the bony contour creation was difficult because of metal artefact in the CT scans. Thus, 2D/3D registration of femoral and tibial implants was performed initially; subsequently 2D/3D registration of femoral and tibial bone models was performed as previously reported19. The relative position between the implant and the bone was matched using surface registration between preoperative 3D bone models and 3D implant and bone models created from postoperative CTs (Fig. 9)19. Estimated accuracy for the relative motion between the femoral and tibial 3D bone models was ≤ 1° in rotation and ≤ 1 mm in translation22. The local coordinate system for the femur and tibia was constructed as previously described22. Knee rotations were described using the joint rotational convention of Grood and Suntay33.
A two-dimensional/three-dimensional (2D/3D) registration and the cruciate ligament force analysis in bicruciate-retaining total knee arthroplasty (images generated by visualization software developed at Osaka University, Osaka, Japan). Red lines at the bottom row indicate the cruciate ligament models: (A) Preoperative squatting; (B) Postoperative squatting; (C) Postoperative cross-legged sitting.
The femoral and tibial attachment areas of the anteromedial and posterolateral bundles of the ACL (aACL and pACL), and the anterolateral and posteromedial bundles of the posterior cruciate ligament (aPCL and pPCL) were identified using the osseous landmark from preoperative CT and MRI data)34,35,36. The accuracy of the attachment area is 0.7 ± 0.1 mm36. Tensile forces in each cruciate ligament bundle were calculated using commercially available software (VivoSim v1, Advanced Mechanical Technology Incorporated, Watertown, MA, USA; https://amti.biz/index.aspx). The path of each ligament was approximated as a straight line (Fig. 9); the effects of ligament-bone contact were neglected. VivoSim computes tensile forces in each ligament bundle based on the strain calculated by the relative movement of the bony attachments points during knee flexion. Tensile force is computed for each bundle using properties described by a nonlinear force–strain curve37,38,39. The parameters used (initial stiffness values and reference lengths of the ligament bundles) were based on the data reported by Shelburne et al39,40. The properties of the model ligaments were adapted to match measurements of knee-joint laxity in the intact and ACL-deficient knee obtained from previous cadaver studies38,41.
Femoral rotation and varus-valgus angle relative to the tibia, anteroposterior (AP) translation of the medial sulcus (medial side), and lateral epicondyle (lateral side) of the femur on the plane perpendicular to the tibial mechanical axis in each flexion angle were evaluated22. AP translation was calculated as a percentage relative to the proximal AP dimension of the tibia19,22. External rotation was denoted as positive; internal rotation as negative. Valgus angulation was defined as positive; varus as negative. Positive or negative values of AP translation were defined as anterior or posterior to the axis of the tibia, respectively. Cruciate ligament forces for each flexion angle were calculated. To investigate whether ligament forces were related to knee kinematics, for each activity, we computed the change in femoral rotation, varus-valgus angulation, and AP position of the femoral condyles and change in ligament forces for each ligament bundle for selected flexion ranges as follows: aACL: change from 10° to 60° flexion; pACL: change from 10° to 30° flexion; aPCL: change from 60° to maximum flexion; pPCL: change from 30° to maximum flexion. These ranges of flexion were selected because forces are more likely to be generated in the ACL and PCL within these ranges. We then evaluated the correlation between change in each kinematic parameter and change in force for each cruciate ligament bundle. All the values were expressed as mean ± standard deviation.
Statistical analyses
Results were analyzed using SPSS version 24 (IBM Corp., Armonk, NY, USA). Repeated measure analysis of variance (ANOVA) and post hoc pairwise comparison (Bonferroni test) were used to analyse all evaluated items except the knee flexion angle, KOOS, HKA, and correlation. A paired t-test (parametric data) and Wilcoxon signed-rank test (non-parametric data) were used to compare knee flexion angle and each subscale in KOOS and HKA. Pearson’s Correlation Coefficient was used to analyze the correlation between differences in knee kinematics and corresponding differences in cruciate ligament force. A p-value ≤ 0.05 was considered statistically significant. Power analysis using G*Power 3.142 indicated that nine knees would be required to generate a power at 0.8 at an alpha of 0.05.
References
Hamai, S. et al. Knee kinematics in medial osteoarthritis during in vivo weight-bearing activities. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 27, 1555–1561. https://doi.org/10.1002/jor.20928 (2009).
Kawashima, K. et al. In vivo three-dimensional motion analysis of osteoarthritic knees. Mod. Rheumatol. Jpn. Rheum. Assoc. 23, 646–652. https://doi.org/10.1007/s10165-012-0703-0 (2013).
Angerame, M. R., Holst, D. C., Jennings, J. M., Komistek, R. D. & Dennis, D. A. Total knee arthroplasty kinematics. J. Arthroplast. 34, 2502–2510. https://doi.org/10.1016/j.arth.2019.05.037 (2019).
Moro-oka, T. A., Muenchinger, M., Canciani, J. P. & Banks, S. A. Comparing in vivo kinematics of anterior cruciate-retaining and posterior cruciate-retaining total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 15, 93–99. https://doi.org/10.1007/s00167-006-0134-6 (2007).
Stiehl, J. B., Komistek, R. D., Cloutier, J. M. & Dennis, D. A. The cruciate ligaments in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplasties. J. Arthroplast. 15, 545–550 (2000).
Halewood, C., Traynor, A., Bellemans, J., Victor, J. & Amis, A. A. Anteroposterior laxity after bicruciate-retaining total knee arthroplasty is closer to the native knee than ACL-resecting TKA: a biomechanical cadaver study. J. Arthroplast. 30, 2315–2319. https://doi.org/10.1016/j.arth.2015.06.021 (2015).
Heyse, T. J. et al. Kinematics of a bicruciate-retaining total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 25, 1784–1791. https://doi.org/10.1007/s00167-016-4414-5 (2017).
Pritchett, J. W. Anterior cruciate-retaining total knee arthroplasty. J. Arthroplast. 11, 194–197 (1996).
Pritchett, J. W. Patients prefer a bicruciate-retaining or the medial pivot total knee prosthesis. J. Arthroplast. 26, 224–228. https://doi.org/10.1016/j.arth.2010.02.012 (2011).
Pritchett, J. W. Bicruciate-retaining total knee replacement provides satisfactory function and implant survivorship at 23 years. Clin. Orthop. Relat. Res. 473, 2327–2333. https://doi.org/10.1007/s11999-015-4219-8 (2015).
Jenny, J. Y. & Jenny, G. Preservation of anterior cruciate ligament in total knee arthroplasty. Arch. Orthop. Trauma Surg. 118, 145–148 (1998).
Migaud, H. et al. Influence of the tibial slope on tibial translation and mobility of non-constrained total knee prosthesis. Rev. Chir. Orthop. Reparatrice Appar. Mot. 82, 7–13 (1996).
Okada, Y. et al. ACL function in bicruciate-retaining total knee arthroplasty. J. Bone Jt. Surg. Am. 100, e114. https://doi.org/10.2106/jbjs.18.00099 (2018).
Tsai, T. Y. et al. Bi-cruciate retaining total knee arthroplasty does not restore native tibiofemoral articular contact kinematics during gait. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 37, 1929–1937. https://doi.org/10.1002/jor.24333 (2019).
Noble, P. C., Conditt, M. A., Cook, K. F. & Mathis, K. B. The John Insall award: patient expectations affect satisfaction with total knee arthroplasty. Clin. Orthop. Relat. Res. 452, 35–43. https://doi.org/10.1097/01.blo.0000238825.63648.1e (2006).
Nakahara, H. et al. Correlations between patient satisfaction and ability to perform daily activities after total knee arthroplasty: why aren’t patients satisfied?. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 20, 87–92. https://doi.org/10.1007/s00776-014-0671-7 (2015).
Kono, K. et al. In vivo kinematics of bicruciate-retaining total knee arthroplasty with anatomical articular surface under high-flexion conditions. J. Knee Surg. https://doi.org/10.1055/s-0039-1696959 (2019).
Fiacchi, F. et al. In vivo kinematics of medial unicompartmental osteoarthritic knees during activities of daily living. Knee 21(Suppl 1), S10–S14. https://doi.org/10.1016/s0968-0160(14)50003-8 (2014).
Kono, K. et al. Bicruciate-retaining total knee arthroplasty reproduces in vivo kinematics of normal knees to a lower extent than unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA https://doi.org/10.1007/s00167-019-05754-2 (2019).
Arauz, P., Klemt, C., Limmahakhun, S., An, S. & Kwon, Y. M. Stair climbing and high knee flexion activities in Bi-cruciate retaining total knee arthroplasty: in vivo kinematics and articular contact analysis. J. Arthroplast. 34, 570–576. https://doi.org/10.1016/j.arth.2018.11.013 (2018).
Hallen, L. G. & Lindahl, O. The, “screw-home” movement in the knee-joint. Acta Orthop. Scand. 37, 97–106 (1966).
Kono, K. et al. In vivo three-dimensional kinematics of normal knees during different high-flexion activities. Bone Jt. J. 100-b, 50–55. https://doi.org/10.1302/0301-620x.100b1.bjj-2017-0553.r2 (2018).
Hamada, D. et al. Native rotational knee kinematics are lost in bicruciate-retaining total knee arthroplasty when the tibial component is replaced. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 26, 3249–3256. https://doi.org/10.1007/s00167-018-4842-5 (2018).
Van Onsem, S., Verstraete, M., Van Eenoo, W., Van Der Straeten, C. & Victor, J. Are TKA kinematics during closed kinetic chain exercises associated with patient-reported outcomes? A preliminary analysis. Clin. Orthop. Relat. Res. 478, 255–263. https://doi.org/10.1097/corr.0000000000000991 (2019).
Twiggs, J. G. et al. Patient-specific simulated dynamics after total knee arthroplasty correlate with patient-reported outcomes. J. Arthroplast. 33, 2843–2850. https://doi.org/10.1016/j.arth.2018.04.035 (2018).
Sabouret, P., Lavoie, F. & Cloutier, J. M. Total knee replacement with retention of both cruciate ligaments: a 22-year follow-up study. Bone Jt. J. 95-b, 917–922. https://doi.org/10.1302/0301-620x.95b7.30904 (2013).
Tsai, T. Y. et al. In-vivo elongation of anterior and posterior cruciate ligament in Bi-cruciate retaining total knee arthroplasty. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 36, 3239–3246. https://doi.org/10.1002/jor.24132 (2018).
Yue, B., Varadarajan, K. M., Rubash, H. E. & Li, G. In vivo function of posterior cruciate ligament before and after posterior cruciate ligament-retaining total knee arthroplasty. Int. Orthop. 36, 1387–1392. https://doi.org/10.1007/s00264-011-1481-6 (2012).
Henning, C. E., Lynch, M. A. & Glick, K. R. Jr. An in vivo strain gage study of elongation of the anterior cruciate ligament. Am. J. Sports Med. 13, 22–26. https://doi.org/10.1177/036354658501300104 (1985).
Roos, E. M. & Lohmander, L. S. The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual. Life Outcomes 1, 64. https://doi.org/10.1186/1477-7525-1-64 (2003).
Nakamura, N. et al. Cross-cultural adaptation and validation of the Japanese knee injury and osteoarthritis outcome score (KOOS). J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 16, 516–523. https://doi.org/10.1007/s00776-011-0112-9 (2011).
Yamazaki, T. et al. Improvement of depth position in 2-D/3-D registration of knee implants using single-plane fluoroscopy. IEEE Trans. Med. Imag. 23, 602–612 (2004).
Grood, E. S. & Suntay, W. J. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J. Biomech. Eng. 105, 136–144 (1983).
Inou, Y., Tomita, T., Kiyotomo, D., Yoshikawa, H. & Sugamoto, K. What kinds of posterior cruciate ligament bundles are preserved in cruciate-retaining total knee arthroplasty? A three-dimensional morphology study. J. Knee Surg. 32, 989–994. https://doi.org/10.1055/s-0038-1675184 (2018).
Shino, K., Mae, T. & Tachibana, Y. Anatomic ACL reconstruction: rectangular tunnel/bone-patellar tendon-bone or triple-bundle/semitendinosus tendon grafting. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 20, 457–468. https://doi.org/10.1007/s00776-015-0705-9 (2015).
Lee, Y. S., Seon, J. K., Shin, V. I., Kim, G. H. & Jeon, M. Anatomical evaluation of CT-MRI combined femoral model. Biomed. Eng. Online 7, 6. https://doi.org/10.1186/1475-925x-7-6 (2008).
Blankevoort, L. & Huiskes, R. Ligament-bone interaction in a three-dimensional model of the knee. J. Biomech. Eng. 113, 263–269 (1991).
Pandy, M. G., Sasaki, K. & Kim, S. A Three-dimensional musculoskeletal model of the human knee joint. Part 1: theoretical construct. Comput. Methods Biomech. Biomed. Eng. 1, 87–108. https://doi.org/10.1080/01495739708936697 (1998).
Shelburne, K. B., Kim, H. J., Sterett, W. I. & Pandy, M. G. Effect of posterior tibial slope on knee biomechanics during functional activity. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 29, 223–231. https://doi.org/10.1002/jor.21242 (2011).
Shelburne, K. B. & Pandy, M. G. A musculoskeletal model of the knee for evaluating ligament forces during isometric contractions. J. Biomech. 30, 163–176. https://doi.org/10.1016/s0021-9290(96)00119-4 (1997).
Shelburne, K. B., Pandy, M. G., Anderson, F. C. & Torry, M. R. Pattern of anterior cruciate ligament force in normal walking. J. Biomech. 37, 797–805. https://doi.org/10.1016/j.jbiomech.2003.10.010 (2004).
Faul, F., Erdfelder, E., Buchner, A. & Lang, A. G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods 41, 1149–1160. https://doi.org/10.3758/brm.41.4.1149 (2009).
Author information
Authors and Affiliations
Contributions
D.D.D., T.T., and K.K. conceptualized and designed the study and are guarantors of the integrity of the entire study. H.I. and K.K. acquired the data. K.K. and D.D.D. analyzed and interpreted the data. K.K. and D.D.D. drafted the article. H.I. and T.Y. provided the study materials, while S.K. and K.K. were responsible for the statistical analysis. D.D.D. obtained funding. Sh.T., Sa.T., and D.D.D. provided administrative, technical, and logistical support. All authors critically revised the article for important intellectual content and approved the final version to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kono, K., Inui, H., Tomita, T. et al. In vivo kinematics and cruciate ligament forces in bicruciate-retaining total knee arthroplasty. Sci Rep 11, 5645 (2021). https://doi.org/10.1038/s41598-021-84942-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-84942-y
- Springer Nature Limited
This article is cited by
-
Effect of floor and chair sit-to-stand motions on determination of optimal surgical site for anterior cruciate ligament reconstruction surgery
Journal of Mechanical Science and Technology (2024)
-
Bicruciate-retaining total knee arthroplasty procedure reduced tensile force in the middle and posterior components of lateral collateral ligament during deep knee flexion activities with no effect on tensile force of the medial collateral ligament
Knee Surgery, Sports Traumatology, Arthroscopy (2023)
-
Cruciate ligament force of knees following mobile-bearing unicompartmental knee arthroplasty is larger than the preoperative value
Scientific Reports (2021)