Abstract
Anatomic ACL reconstruction is the reasonable approach to restore stability without loss of motion after ACL tear. To mimic the normal ACL like a ribbon, our preferred procedures is the anatomic rectangular tunnel (ART) technique with a bone-patellar tendon-bone (BTB) graft or the anatomic triple bundle (ATB) procedure with a hamstring (HS) tendon graft. It is important to create tunnel apertures inside the attachment areas to lessen the tunnel widening. To identify the crescent-shaped ACL femoral attachment area, the upper cartilage margin, the posterior cartilage margin and the resident’s ridge are used as landmarks. To delineate the C-shaped tibial insertion, medial intercondylar ridge, Parson’s knob and anterior horn of the lateral meniscus are helpful. In ART-BTB procedure which is suitable for male patients engaged in contact sports, the parallelepiped tunnels with rectangular apertures are made within the femoral and tibial attachment areas. In ATB-HS technique which is mainly applied to female athletes engaged in non-contact sports including skiing or basketball, 2 femoral and 3 tibial round tunnels are created inside the attachment areas. These techniques make it possible for the grafts to run as the native ACL without impingement to the notch or PCL. After femoral fixation with an interference screw or cortical fixation devices including Endobutton, the graft is pretensioned in situ by repetitive manual pulls at 15–20° of flexion, monitoring the graft tension with tensioners on a tensioning boot installed on the calf. Tibial fixation with pullout sutures is achieved using Double Spike Plate and a screw at the pre-determined amount of tension of 10–20N. While better outcomes with less failure rate are being obtained compared to those in the past, higher graft tear rate remains a problem. Improved preventive training may be required to avoid secondary ACL injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament reconstruction (ACLR) is a common surgical procedure in orthopaedic practice. It is our strong belief that a graft that is placed to mimic the native ACL is functionally capable of properly stabilizing the knee without loss of motion. Thus, anatomic graft placement is the key to successful ACLR.
In order to precisely mimic the fiber orientation of the native ACL, which is a flat ribbon-like structure [1], simply creating a single round tunnel in the attachment area is far from ideal. The tunnel aperture(s) should be adjusted to the shape of the attachment area, and the selected graft should be shaped to the tunnel.
Currently, the two autogenous grafts most widely used for ACLR are (1) the bone–patellar tendon–bone (BTB) graft and (2) the multi-strand soft tissue graft consisting of the medial hamstring tendon (HST).
In this instructional lecture, we discuss the procedure for accomplishing anatomic ACLR using a BTB or HST graft, including (1) how to create proper bone tunnels based on the anatomy, (2) graft selection and preparation, and (3) graft tensioning and fixation.
ACL attachment areas and their landmarks
Femoral attachment area
Iwahashi et al. [2] histologically demonstrated that the direct insertion of the ligament to the femur was located in a crescent-shaped fovea at the superior-posterior margin of the lateral wall of the intercondylar notch, and they provided a schema of the area by reconstituting the oblique-axial CT sections. Three landmarks are noted to delineate the crescent-shaped femoral insertion: the resident’s ridge, anteriorly; the upper cartilage margin, superiorly; and the posterior cartilage margin, posteriorly (Fig. 1).
Tibial attachment area
Berg used the term "Parson’s knob" (tuberculum intercondylare tertium) to describe the anterior border of the tibial insertion; we would personally propose to name it the “anterior intercondylar ridge of the tibia” [3]. Purnell et al. [4] showed that the medial intercondylar ridge could be used as a bony landmark for the medial border of the tibial insertion. Siebold et al. [1] clarified the relationship of the tibial insertion between the ACL and the anterior horn of the lateral meniscus. As such, three landmarks are suggested for delineating the tibial insertion of a long triangular shape: the anterior intercondylar ridge, anteriorly; the medial intercondylar ridge, medially; and the anterior horn of the lateral meniscus, laterally (Fig. 2).
Rationale for anatomic grafting
-
1.
The grafts should not completely fill the attachment areas, as grafts used for ACLR become hypertrophic after implantation [5], and because their mechanical properties are greater than those of the native ACL [6].
-
2.
The grafts must be off-centered inside the areas for them to properly function in stabilizing the knee. It should also be noted that deformation of the grafts occurs based on tensile force.
-
3.
Tunnel apertures should be created inside the attachment areas, not only for mimicking the native ACL, but also for keeping them inside the areas with greater cortical thickness in order to maintain robustness [7].
Graft selection
In Japan, the choice of available allografts is limited, and realistic options for autogenous grafts are confined to (1) bone–patellar tendon–bone (BTB) grafts, (2) multi-strand soft tissue medial hamstring tendon grafts (HST), and (3) quadriceps tendon–bone (QTB) grafts. As the QTB graft is generally reserved in our practice for patients undergoing repeat revision ACLR, one of the first two grafts is usually selected for primary ACLR.
The BTB graft is a suitable ACLR candidate not only because of its shape, but also because of its mechanical properties, as described previously. However, patients should be aware that BTB graft harvest site morbidity is relatively high, and a small number of our female patients have suffered arthrofibrosis postoperatively. As integration of the bone plug within the bone tunnel wall occurs very early in the anatomic rectangular tunnel (ART) ACLR procedure [8], however, this graft is appropriate for male athletes with high motivation for returning to strenuous/contact sports, including football or judo.
The HST graft is also a suitable alternative. While harvest graft site morbidity is lower with the HST, tendon-to-bone tunnel integration is less successful, as evidenced by postoperative femoral tunnel enlargement observed in second-look arthroscopy or CT [9, 10] (Fig. 3). As such, this graft is better tailored to individuals with less strenuous activity, such as female athletes engaged in non-contact sports, including skiing or basketball. It should be noted, however, that there is a wide variation among individuals in the size of the medial hamstring tendon [11], and patients with hypoplastic hamstring tendons can be treated with the BTB graft despite the greater risk of graft harvest site morbidity.
Operative setting
For arthroscopic identification of the femoral attachment area or resident’s ridge through the anteromedial portal, we recommend keeping the distal thigh horizontal using a leg holder, with the calf hanging freely.
ACLR with bone–patellar tendon–bone graft
A gold standard: bone–patellar tendon–bone (BTB) graft
A BTB graft is morphologically suitable for mimicking the native ACL in revision or primary ACLR. Biomechanically, a 10-mm wide BTB graft has sufficient maximum tensile load (1.2× that of normal ACL) with bone-tendon junctions and bone plugs [6].
Anatomic rectangular tunnel ACL reconstruction (ART ACLR)
We developed an anatomic rectangular tunnel ACL reconstruction (ART ACLR) method using a BTB graft with a bone plug 5 mm in thickness to mimic the natural fiber arrangement inside the native ACL and to minimize tunnel size (Figs. 4, 5) [12, 13]. With this technique, we were able to pursue the concept of the double-bundle ACLR with a single BTB graft. As the crescent-shaped ACL femoral attachment area located at the superior-posterior margin of the lateral wall of the notch is less than 10 mm in width [14, 15], this technique makes it possible to create a robust tunnel aperture inside an attachment area with greater cortical thickness [7]. Biomechanically, this reconstruction technique is superior to the conventional transtibial tunnel single-bundle procedure [16].
This procedure is advantageous for revision ACLR as well, not only for avoiding overlapping tunnels in the case of improperly placed tunnels from a previous surgery, but also to leave more space between the old and new tunnels, as the cross-sectional area of the tunnels of 50 mm2 (5 × 10 mm) in ART ACLR is less than that in a conventional 10-mm round tunnel technique with an area of 79 mm2 (π × 52 mm). Hypothetically, since tunnel encroachment is less of an issue, the ART ACLR technique could be applied as a one-stage revision procedure after failed primary ACLR [17].
Bone–patellar tendon–bone (BTB) graft harvest and preparation
As the width of the patellar tendon is relatively consistent among individuals, a graft with a width of 10 mm is suitable for 90 % of our patients. Therefore, in this section, we describe graft harvesting using a width of 10-mm. However, an 8-mm graft is applied for small female patients, while a 13-mm graft is used for large male patients.
The graft is harvested through a 5–6 cm longitudinal skin incision just medial to the patellar tendon from the central portion of the medial half of the patellar tendon. As the central portion of the tendon is shorter than the lateral or medial side, the graft has longer and shorter sides in its tendinous portion. The longer sides are assigned to the anteromedial portion of the graft, and the shorter sides to the posterolateral portion (Fig. 6a).
The harvested graft is prepared as follows: the bone plug from the tibia is shaped into a parallelepiped 5 mm thick × 10 mm wide × 15 mm long so as to snugly pass the graft sizing template (BTB sizer: # E0014050-11, Smith & Nephew plc, Andover, MA, USA) and to be used for the femoral socket/tunnel. The patellar bone block is left as a triangular pillar for the tibial tunnel (Fig. 6b).
To minimize graft harvest site morbidity, the defect in the tibial tubercle due to bone plug harvesting should be filled with cancellous bone obtained at the time the tibial tunnel is created.
Femoral socket/tunnel preparation
Exposure of the ACL femoral attachment area
While the posterior third of the lateral wall of the notch is viewed through the anteromedial portal, the fibrous tissue, including the ACL stump on the superior–posterior half of the lateral wall of the intercondylar notch, is thoroughly removed using a radiofrequency device through the far anteromedial (FAM) portal, which is created 2–2.5 cm posterior to the anteromedial portal and just above the medial meniscus [15, 18]. Mechanical shavers are not utilized so as to preserve subtle undulation of the bony surface around the attachment area. After the area is cleaned, the crescent-shaped attachment area is clearly delineated by the resident’s ridge anteriorly, the upper cartilage margin superiorly, and the posterior cartilage margin, posteriorly (Fig. 7a) [15].
Inside-out creation of the tunnel through the far anteromedial portal
A microfracture awl is used to mark two points at a distance of 5 mm in the center of the attachment area along its long axis (Fig. 7a). Two parallel guide pins are then drilled using a cannulated dilator (Smith & Nephew, # E0014050-2) or manually from these points to the lateral femoral cortex via the far anteromedial portal, with the knee flexed over 140°. The proximal pin is over-drilled with a 5.0 mm cannulated drill bit to the lateral femoral cortex, while the distal pin is over-drilled to a depth of 20 mm. The continuous two round holes are dilated into a 5 × 10 × 22 mm parallelepiped socket, using the lower pin as a guide, with the 5 × 10 mm cannulated dilator (Smith & Nephew, # E0014050-2) (Fig. 7b). The socket is then rasped to make the wall smooth and flat with the knee deeply flexed.
Notchplasty is not required unless marginal osteophytes are formed.
Outside-in creation of the tunnel through the lateral incision
For a knee with passive flexion less than 140°, this approach is recommended in order to avoid blowout of the tunnel. While the ACL femoral attachment area is viewed via the anteromedial portal, a central guide pin is drilled into the center of the area from the lateral femoral cortex using an anterolateral entry femoral guide (Smith & Nephew # 6901189 or 7210984) via the anterolateral portal. A 10-mm skin protection cannula is installed over the guide pin via a 2-cm lateral femoral incision (Fig. 8a). With the aid of a 10-mm offset drill guide (Smith & Nephew E0014050-7), two guide pins are drilled parallel to the central pin along the long axis of the attachment area or the resident’s ridge. After the central pin is removed, two guide pins are over-drilled with a 5-mm drill bit. With the dilator at 5 × 10 mm from the lateral femoral cortex, the two drill holes are dilated into one rectangular tunnel in outside-in fashion (Fig. 8b).
Tibial tunnel preparation
Exposure of the ACL tibial attachment area
While the ACL tibial remnant and/or attachment area is viewed via the anteromedial portal, the stump is cut with a shaver to 3–5 mm in length. The ACL tibial attachment area can be delineated by viewing the anterior and medial margin of the residual fibers of the ACL, as well as the anterior horn of the lateral meniscus.
Outside-in creation of the half-rectangular tibial tunnel
As the attachment area is viewed through the anteromedial portal, the tip of the tibial drill guide (Smith & Nephew #7205519) is placed through the FAM portal to the center of the area (Fig. 9a). A lateral-plain radiograph is taken to determine the positional relationship between the pin and Parson’s knob designating the anterior border of the area (Fig. 9b). The pin is over-drilled halfway, or 2–2.5 cm, with a 10-mm cannulated drill bit or a bone dowel harvester for a bone plug to be grafted to defects in the graft harvest site. The anteromedial and posterolateral pins are drilled in line with the long axis of the attachment area at a 5-mm distance using the 10-mm offset drill guide (Smith & Nephew #E0014050-7). The central pin is removed, and they are then over-drilled with a 5.0 mm cannulated drill bit, followed by dilation into a 5 × 10 mm rectangle to the articular surface with the dilator (Smith & Nephew E0014050-2) (Fig. 9c, d).
Graft tensioning and fixation
With the use of two leading sutures, the graft is passed from the tibial tunnel to the femoral socket, with its parallelepiped bone plug kept on the top and with its cancellous bone surface maintained anteriorly.
For femoral fixation, a 6 mm × 20–30 mm interference screw is used in outside-in fashion through the 5-mm hole from the lateral femoral cortex to the bottom of the socket using a 6.5-mm skin protector (Smith & Nephew #6901106) via an additional small lateral femoral incision. For inside-out interference fixation, the screw is introduced through the far anteromedial portal. Otherwise, other pullout techniques are utilized, including a DSP (double spike plate; Meira Corporation, Aichi, Japan) and screw through an additional 3–4-cm lateral skin incision [19].
After femoral fixation, the relationship between the notch in extension and the posterior cruciate ligament (PCL) in flexion should be observed. If placement of the graft is anatomically correct, there is no impingent of the graft against the notch or PCL (Fig. 10).
Tibial fixation is achieved with a modified pullout suture technique using the DSP system at an optional/predetermined amount of initial tension. According to our cadaveric experiment, the mean laxity-match tension for the ART ACLR knees was 8.6 ± 4.8 N, and the recommended initial tension to the graft at the time of its final fixation could be reasonably assumed to be 10–20 N [16].
The tensioning sutures distally connected to the DSP are tied to a tensioner mounted on the metal-shell boot fixed to the tibia with a bandage (Fig. 11a). The creep of the construct is then meticulously removed by repetitive manual pulls of the graft suture with the knee flexed 15–20°. After the tensioner reading is stabilized at the intended level of 10–20 N for 2 min, the graft is temporarily fixed by hammering the DSP bottom spikes into the tibial cortex, and the DSP is secured with a screw (Fig. 11b). Care is taken to remove the periosteum in the area where the DSP is placed.
Postoperative rehabilitation
The knee is splint-immobilized at 10° flexion for 1 week, followed by passive and active range of motion (ROM) exercises. Partial weight-bearing is allowed at 2 weeks, followed by full weight-bearing at 4–5 weeks. Full extension or flexion exceeding 130° is not permitted until 5 weeks. Jogging is recommended at 3 months. Return to strenuous activity is not allowed until 6 months.
ACLR with hamstring tendon (HST) graft
Multi-strand soft tissue grafts without bone plugs
The most common graft procedure involves the use of multi-strand soft tissue grafts, including the semitendinosus tendon, given their greater ease of handling as well as the lower degree of surgical invasiveness. Biomechanically, the four-strand semitendinosus tendon graft has adequate maximum tensile load (2.8× that for the normal ACL) [6].
Three ACL bundles and their attachment areas
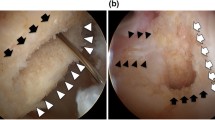
Norwood and Cross described three ACL bundles—the anteromedial (AM), intermediate (IM), and posterolateral (PL) [20]—which we have arthroscopically observed in our practice as well (Fig. 12). Otsubo et al. [21] elucidated the attachment areas of the three ACL bundles, while Fujie et al. [22] clarified the biomechanical functions of each bundle.
In 2004, we developed an anatomic triple-bundle ACL reconstruction (ATB ACLR) procedure with a semitendinosus tendon graft to mimic three bundles inside the native ACL (Fig. 13) [23–25], as opposed to the double-bundle ACLR that had been performed between 1999 and 2004. Two double-looped semitendinosus tendon grafts via two femoral tunnels and three tibial tunnels made it possible to more closely mimic the triangular tibial footprint than was possible with the double-bundle ACLR (Fig. 14a, b).
Semitendinosus graft harvesting and preparation
The entire semitendinosus tendon, including the distal periosteum, is harvested through a 4-cm oblique skin incision 3–4 cm medial to the tibial tubercle. The tendon is transected into two halves to make two double-looped grafts 55–70 mm in length and 5–6 mm in diameter. An ENDOBUTTON CL (Smith & Nephew, 72200146–72200149) is connected to the loop end, and thick polyester or polyethylene sutures (#3–5) are placed in each free end of the graft using baseball glove or whip stitches (Fig. 14c).
Femoral tunnel preparation
After exposure of the ACL femoral attachment area as previously described in the ART BTB procedure, the area is transversely divided into an upper proximal section for the AM + IM graft(s) and lower posterior section for the PL graft. The centers of the two sections are marked with an awl. With the anterolateral entry femoral guide (Smith & Nephew # 6901189 or 7210984) through the anterolateral portal, guide pins are drilled from the lateral cortex to the marked centers through small skin incisions 1 cm in length.
The two pins are over-drilled with cannulated drill bits matched in diameter with graft diameters in outside-in fashion through a 7-mm skin muscle-protective cannula (Smith & Nephew #6901106) (Fig. 15a).
Tibial tunnel preparation
With the attachment area viewed through the anteromedial portal, a guide pin is inserted from the medial tibial cortex to the center of the area using a tibial drill guide set at a 45° angle (Smith & Nephew # 7205517, 7205519) (Fig. 9). The pin is over-drilled with a 10-mm cannulated drill bit to remove only the cortical bone. Using the 10-mm offset drill guide (Smith & Nephew E0014050-7), AM and IM guide pins are drilled inside the anterior section of the attachment area in line with the coronal plane. The PL pin is then drilled just lateral to the medial intercondylar ridge. After removal of the central pin, AM and IM guide pins are over-drilled with 4.5 and 5.0-mm cannulated drill bits, respectively, and the PL pin is over-drilled with a 5.0–6.0 mm cannulated drill bit (Fig. 15b).
Graft passage and femoral fixation
The PL looped graft with the ENDOBUTTON on the top is passed as a whole through the posterior tibial tunnel to the lower femoral drill hole and fixed to the femur by turning the button. Care is taken to ensure that at least 12.5 mm of the graft is inside the tunnel.
The upper loop end with the ENDOBUTTON CL of the bifurcated anterior graft (AM + IM grafts) is passed through the FAM portal to the upper femoral tunnel. Each free end of the two anterior grafts is introduced into the joint, and pulled into the anterolateral tibial tunnel as the IM graft and into the anteromedial tunnel as the AM graft in inside-out fashion. Femoral fixation is achieved by turning the ENDOBUTTON.
The implanted graft shows no impingement against the roof or wall of the intercondylar notch or the PCL (Fig. 16).
Tibial fixation
First, the posterolateral graft sutures are manually tensioned as a whole and tied to a small-sized DSP. The two anterior graft sutures are then tensioned and tied together to the other DSP. The two tensioning sutures connected to the two DSPs are each tied to one of two tensioners mounted to a metal tensioning boot fixed to the tibia with a bandage (Fig. 11a). Each graft is pre-tensioned to remove creep of the construct, as previously described, and adjusted to 10–15 N [25, 26]. Finally, each graft is fixed with DSPs and two cancellous screws (Fig. 17).
Postoperative rehabilitation
The knee is splint-immobilized at 10° flexion for 2 weeks, followed by passive and active ROM exercises. Partial weight-bearing is allowed at 2–3 weeks, followed by full weight-bearing at 4–5 weeks. Full extension or flexion exceeding 130° is not permitted until 5 weeks. Jogging is recommended at 3–4 months. Return to strenuous activity is not allowed until 7 months.
Clinical outcomes
Previous studies from our group on outcomes after double-bundle ACL reconstructions suggested that outcomes improved as the anatomical accuracy of graft placement increased [27]. In actuality, a current CT-based study from our institution has shown that anteriorly located and internally rotated tibia of preoperative knees was over-constrained (posterior displacement with external tibial rotation) at 3 weeks after ATB ACLR, but returned to normal position by 6 months [28]. Thus, better data on patient outcomes are now available, although the current procedures have not yet been reported.
While there is a concern regarding higher rates of graft rupture following anatomic ACLR compared to those for less anatomic ACLRs performed in the previous century [29], subsequent meniscal damage after ACLR has been drastically reduced. Patients with totally stable knees who returned to more strenuous sports were at higher risk of graft rupture. Improved rehabilitation or proprioceptive training may be required to prevent secondary ACL injury, and it is important that patients are informed of risk management measures.
Conclusion
The goal of ACL reconstruction should be to mimic the native ACL by means of grafting (Fig. 18), and thus surgery should be anatomy-based. Emphasis is placed on tunnel apertures inside the attachment areas, proper graft choice and preparation, and appropriate graft tensioning and fixation. Our objective is to restore the health of the knee by means of anatomically real ACL grafting.
References
Siebold R, Schumacher P, Fernandez F, Smigielski R, Fink C, Brehmer A, Kirsch J. Flat midsubstance of the anterior cruciate ligament with tibial “C”-shaped insertion site. Knee Surg Sports Traumatol Arthosc. 2014. doi:10.1007/s00167-014-3058-6.
Iwahashi T, Shino K, Nakata K, Otsubo H, Suzuki T, Amano H, Nakamura N. Direct ACL insertion to the femur assessed by histology and three-dimensional volume-rendered computed tomography. Arthroscopy. 2010;26(9 Suppl):S13–20.
Berg EE. Parson’s knob (tuberculum intercondylare tertium). A guide to tibial anterior cruciate ligament insertion. Clin Orthop Relat Res. 1993;292:229–31.
Purnell ML, Larson AI, Clancy WG. Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med. 2008;36(11):2083–90.
Hamada M, Shino K, Horibe S, Mitsuoka T, Toritsuka Y, Nakamura N. Changes in cross-sectional area of hamstring anterior cruciate ligament grafts as a function of time following transplantation. Arthroscopy. 2005;21(8):917–22.
Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66(3):344–52.
Hutchinson MR, Ash SA. Resident’s ridge: assessing the cortical thickness of the lateral wall and roof of the intercondylar notch. Arthroscopy. 2003;19(9):931–5.
Suzuki T, Shino K, Nakamura N, Iwahashi T, Nakata K, Tanaka Y, Nakagawa S, Kinugasa K, Yamashita T. Early integration of a bone plug in the femoral tunnel in rectangular tunnel ACL reconstruction with a bone–patellar tendon–bone graft: a prospective computed tomography analysis. Knee Surg Sports Traumatol Arthosc. 2011;19(Suppl 1):S29–35.
Otsubo H, Shino K, Nakamura N, Nakata K, Nakagawa S, Koyanagi M. Arthroscopic evaluation of ACL grafts reconstructed with the anatomical two-bundle technique using hamstring tendon autograft. Knee Surg Sports Traumatol Arthosc. 2007;15(6):720–8.
Tachibana Y, Mae T, Shino K, Kanamoto T, Sugamoto K, Yoshikawa H, Nakata K. Morphological changes in femoral tunnels after anatomic anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthosc. 2014. doi:10.1007/s00167-014-3252-6.
Hamada M, Shino K, Mitsuoka T, Abe N, Horibe S. Cross-sectional area measurement of the semitendinosus tendon for anterior cruiciate ligament reconstruction. Arthroscopy. 1998;14(7):696–701.
Shino K, Nakata K, Nakamura N, Toritsuka Y, Nakagawa S, Horibe S. Anatomically-oriented ACL Reconstruction with a bone–patellar tendon graft via rectangular socket/tunnels: a snug-fit and impingement-free grafting technique. Arthroscopy. 2005;21(11):1402.
Shino K, Nakata K, Horibe S, Nakamura N, Toritsuka Y, Nakagawa S, Suzuki T. Rectangular tunnel double-bundle anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft to mimic natural fiber arrangement. Arthroscopy. 2008;24(10):1178–83.
Feretti M, Ekdahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23(11):1218–25.
Shino K, Suzuki T, Iwahashi T, Mae T, Nakata K, Nakamura N, Nakagawa S. The resident’s ridge as an arthroscopic landmark for anatomical femoral tunnel drilling in ACL reconstruction. Knee Surg Sports Traumatol Arthosc. 2010;18(9):1164–8.
Suzuki T, Shino K, Otsubo H, Suzuki D, Mae T, Fujimiya M, Yamashita T, Fujie H. Biomechanical comparison between the rectangular-tunnel and the round-tunnel anterior cruciate ligament reconstruction procedures with a bone patellar tendon bone graft. Arthroscopy. 2014;30(10):1294–302.
Shino K, Mae T, Nakamura N. Revision ACL reconstruction with rectangular tunnel technique. Clin Orthop Relat Res. 2012;470(3):843–52.
Shino K, Horibe S, Hamada M, Nakamura N, Nakata K, Mae T, Toritsuka Y. Allograft anterior cruciate ligament reconstruction. Tech Knee Surg. 2002;1:78–85.
Shino K, Mae T, Maeda A, Miyama T, Shinjo H, Kawakami H. Graft fixation with pre-determined tension using a new device, the double spike plate. Arthroscopy. 2002;18(8):908–11.
Norwood LA, Cross MJ. Anterior cruciate ligament: functional anatomy of its bundles in rotatory instabilities. Am J Sports Med. 1979;7(1):23–6.
Otsubo H, Shino K, Suzuki D, Suzuki T, Kamiya T, Watanabe K, Fujimiya M, Iwahashi T, Yamashita T. The arrangement and the attachment areas of three ACL bundles. Knee Surg Sports Traumatol Arthosc. 2012;20(1):127–34.
Fujie H, Otsubo H, Fukano S, Suzuki T, Suzuki D, Mae T, Shino K. Mechanical functions of the three bundles consisting of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthosc. 2011;19(Suppl 1):S47–53.
Shino K, Nakata K, Nakamura N, Mae T, Ohtsubo H, Iwahashi T, Nakagawa S. Anatomic ACL reconstruction using two double-looped hamstring tendon grafts via twin femoral and triple tibial tunnels. Oper Tech Orthop. 2005;15:130–4.
Tanaka Y, Shino K, Horibe S, Nakamura N, Nakagawa S, Mae T, Otsubo H, Suzuki T, Nakata K. Triple-bundle ACL grafts evaluated by second-look arthroscopy. Knee Surg Sports Traumatol Arthosc. 2012;20(1):95–101.
Mae T, Shino K, Matsumoto N, Yoneda K, Yoshikawa H, Nakata K. Immediate postoperative anterior knee stability: double- versus triple-bundle anterior cruciate ligament reconstructions. Arthroscopy. 2013;29(2):213–9.
Mae T, Shino K, Matsumoto N, Natsu-ume T, Yoneda K, Yoshikawa H, Yoneda M. Anatomic double-bundle anterior cruciate ligament reconstruction using hamstring tendons with minimally required initial tension. Arthroscopy. 2010;26(10):1289–95.
Toritsuka Y, Amano H, Kuwano M, Iwai T, Mae T, Ohzono K, Shino K. Outcome of double-bundle ACL reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthosc. 2009;17(5):456–63.
Matsuo T, Mae T, Shino K, Kita K, Tachibana Y, Sugamoto K, Yoshikawa H, Nakata K. Tibiofemoral relationship following anatomic triple-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthosc. 2014;22(9):2128–35.
Mae T, Shino K, Matsumoto N, Yoneda K, Yoshikawa H, Nakata K. Risk factors for ipsi-lateral graft rupture or contralateral anterior cruciate ligament tear after anatomic double-bundle reconstruction. A-P Smart. 2014;1(3):90–5.
Acknowledgments
One of the authors (KS) has received funding from Smith & Nephew, Inc., Andover, MA, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Shino, K., Mae, T. & Tachibana, Y. Anatomic ACL reconstruction: rectangular tunnel/bone–patellar tendon–bone or triple-bundle/semitendinosus tendon grafting. J Orthop Sci 20, 457–468 (2015). https://doi.org/10.1007/s00776-015-0705-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-015-0705-9