Abstract
The use of mathematical modeling to represent, analyze, make predictions or providing information on data obtained in drug research and development has made pharmacometrics an area of great prominence and importance. The main purpose of pharmacometrics is to provide information relevant to the search for efficacy and safety improvements in pharmacotherapy. Regulatory agencies have adopted pharmacometrics analysis to justify their regulatory decisions, making those decisions more efficient. Demand for specialists trained in the field is therefore growing. In this review, we describe the meaning, history, and development of pharmacometrics, analyzing the challenges faced in the training of professionals. Examples of applications in current use, perspectives for the future, and the importance of pharmacometrics for the development and growth of precision pharmacology are also presented.





Similar content being viewed by others
References
Barrett JS, Fossler MJ, Cadieu KD, et al. Pharmacometrics: a multidisciplinary field to facilitate critical thinking in drug development and translational research settings. J Clin Pharmacol. 2008;48(5):632–49.
Chan PLS, Holford NHG. Drug treatment effects on disease progression. Annu Rev Pharmacol Toxicol. 2001;41:625–59.
Gobburu JV, Lesko LJ. Quantitative disease, drug, and trial models. Ann Rev Pharmacol Toxicol. 2008;49:291–301.
Eddy DM, Archimedes SL. A trial-validated model of diabetes. Diabetes Care. 2003;26:3093–101.
Bangs A. Predictive biosimulation and virtual patients in pharmaceutical R and D. Stud Health Technol Inform. 2005;111:37–42.
Landersdorfer CB, Jusko WJ. Pharmacokinetic/pharmacodynamic modelling in diabetes mellitus. Clin Pharmacokinet. 2008;47:417–48.
Danhof M, de Jongh J, De Lange EC, et al. Mechanism-based pharmacokinetic-pharmacodynamic modeling: biophase distribution, receptor theory, and dynamical systems analysis. Annu Rev Pharmacol Toxicol. 2007;47:357–400.
Sheiner LB. Learning versus confirming in clinical drug development. Clin Pharmacol Ther. 1997;61:275–91.
Breimer DD, Danhof M. Relevance of the application of pharmacokinetic pharmacodynamic modelling concepts in drug development. The ‘wooden shoe’ paradigm. Clin Pharmacokinet. 1997;32:259–67.
Minto C, Schnider T. Expanding clinical applications of population pharmacodynamic modelling. Br J Clin Pharmacol. 1998;46:321–33.
Derendorf H, Meibohm B. Modeling of pharmacokinetic/pharmacodynamic (PK/PD) relationships: concepts and perspectives. Pharm Res. 1999;16:176–85.
Balant LP, Gex FM. Modelling during drug development. Eur J Pharm Biopharm. 2000;50:13–26.
Holford NH, Kimko HC, Monteleone JP, et al. Simulation of clinical trials. Annu Ver Pharmacol Toxicol. 2000;40:209–34.
Bonate PL. Clinical trial simulation in drug development. Pharm Res. 2000;17:252–6.
Sheiner LB, Steimer JL. Pharmacokinetic/pharmacodynamic modeling in drug development. Annu Rev Pharmacol Toxicol. 2000;40:67–95.
Aarons L, Karlsson MO, Mentre F, et al. Role of modelling and simulation in phase I drugdevelopment. Eur J Pharm Sci. 2001;13(2):115–22.
Meibohm B, Derendorf H. Pharmacokinetic/pharmacodynamic studies in drug product development. J Pharm Sci. 2002;91:18–23.
Stanski DR, Rowland M, Sheiner LB. Getting the dose right: report from the tenth European Federation of Pharmaceutical Sciences (EUFEPS) conference on optimizing drug development. J Pharmacokinet Pharmacodyn. 2005;32:199–211.
Florian J, Jadhav PR, Amur S, et al. Boceprevir dosing for late responders and null responders: the role of bridging data between treatment-naïve and -experienced subjects. Hepatology. 2013. https://doi.org/10.1002/hep.25843.
Fourie Zirkelbach J, Jackson AJ, Wang Y, et al. Use of partial AUC (PAUC) to evaluate bioequivalence—a case study with complex absorption: methylphenidate. Pharm Res. 2013. https://doi.org/10.1007/s11095-012-0862-x.
Huang SM, Abernethy DR, Wang Y, et al. The utility of modeling and simulation in drug development and regulatory review. J Pharm Sci. 2013;102:2912.
Lee JY, Wang Y. Use of a biomarker in exposure-response analysis to support dose selection for fingolimod. CPT Pharmacometrics Syst Pharmacol. 2013;2:1.
Sun W, Laughren TP, Zhu H, et al. Development of a placebo effect model combined with a dropout model for bipolar disorder. J Pharmacokinet Pharmacodyn. 2013;40:359.
Yang J, Zhao H, Garnett C, et al. The combination of exposure-response and case-control analyses in regulatory decision making. J Clin Pharmacol. 2013;53:160.
Younis IR, Laughren TP, Wang Y, et al. An integrated approach for establishing dosing recommendations: paliperidone for the treatment of adolescent schizophrenia. J Clin Psychopharmacol. 2013;33:152.
Liu J, Chan-Tack KM, Jadhav P, et al. Why did the FDA approve efavirenz 800 mg when co-administered with rifampin? Int J Clin Pharmacol Ther. 2014;52:446.
Ma L, Zhao L, Xu Y, et al. Clinical endpoint sensitivity in rheumatoid arthritis: modeling and simulation. J Pharmacokinet Pharmacodyn. 2014;41:537.
Dykstra K, Mehrotra N, Tornøe CW, et al. Reporting guidelines for population pharmacokinetic analyses. J Clin Pharmacol. 2015;42:301.
Khurana M, Vaidyanathan J, Marathe A, et al. Canagliflozin use in patients with renal impairment-utility of quantitative clinical pharmacology analyses in dose optimization. J Clin Pharmacol. 2015;55:647.
Lon HK, DuBois DC, Earp JC, et al. Modeling effects of dexamethasone on disease progression of bone mineral density in collagen-induced arthritic rats. Pharmacol Res Perspect. 2015;3:e00169.
Zhou D, Li H, Wang Y, et al. Quantitative characterization of circadian rhythm of pulmonary function in asthmatic patients treated with inhaled corticosteroids. J Pharmacokinet Pharmacodyn. 2015;42:391.
Mulugeta Y, Barrett JS, Nelson R, et al. Exposure matching for extrapolation of efficacy in pediatric drug development. J Clin Pharmacol. 2016;56:1326.
Yu J, Chung S, Zadezensky I, et al. Utility of exposure-response analysis in regulatory decision on the selection of starting dose of pasireotide for cushing disease. J Clin Pharmacol. 2016;56:1035.
Zhuang L, He Y, Xia H, et al. Gentamicin dosing strategy in patients with end-stage renal disease receiving haemodialysis: evaluation using a semi-mechanistic pharmacokinetic/pharmacodynamic model. J Antimicrob Chemother. 2016;71:1012.
Earp JC, Mehrotra N, Peters KE, et al. Esomeprazole FDA approval in children with GERD: exposure-matching and exposure-response. J Pediatr Gastroenterol Nutr. 2017;65:272.
Li L, Wang Y, Uppoor RS, et al. Exposure-response analyses of blood pressure and heart rate changes for methylphenidate in healthy adults. J Pharmacokinet Pharmacodyn. 2017;44:245.
Li H, Yu J, Liu C, et al. Time dependent pharmacokinetics of pembrolizumab in patients with solid tumor and its correlation with best overall response. J Pharmacokinet Pharmacodyn. 2017;44:403.
Li L, Zhang Y, et al. Exposure-response modeling and power analysis of components of ACR response criteria in rheumatoid arthritis (part 1: binary model). J Clin Pharmacol. 2017;57:1097.
Liu C, Yu J, Li H, et al. Association of time-varying clearance of nivolumab with disease dynamics and its implications on exposure-response analysis. Clin Pharmacol Ther. 2017;101:657.
Paterniti MO, Bi Y, Rekić D, et al. Acute exacerbation and decline in forced vital capacity are associated with increased mortality in idiopathic pulmonary fibrosis. Ann Am Thorac Soc. 2017;14:1395.
Chaikin P, Rhodes GR, Bruno R, et al. Pharmacokinetics/pharmacodynamics in drug development: an industrial perspective. J Clin Pharmacol. 2000;40:1428–38.
Reigner BG, Williams PE, Patel IH, et al. An evaluation of the integration of pharmacokinetic and pharmacodynamic principles in clinical drug development. Experience within Hoffmann La Roche. Clin Pharmacokinet. 1997;33:142–52.
Gieschke R, Steimer JL. Pharmacometrics: modelling and simulation tools to improve decision making in clinical drug development. Eur J Drug Metab Pharmacokinet. 2000;25:49–58.
Olson SC, Bockbrader H, Boyd RA, et al. Impact of population pharmacokinetic pharmacodynamic analyses on the drug development process: experience at Parke Davis. Clin Pharmacokinet. 2000;38:449–59.
Blesch KS, Gieschke R, Tsukamoto Y, et al. Clinical pharmacokinetic/pharmacodynamic and physiologically based pharmacokinetic modeling in new drug development: the capecitabine experience. Invest New Drugs. 2003;21:195–223.
Lockwood P, Ewy W, Hermann D, et al. Application of clinical trial simulation to compare proof of concept study designs for drugs with a slow onset of effect; an example in Alzheimer’s disease. Pharm Res. 2006;23:2050–9.
Peck CC, Barr WH, Benet LZ, et al. Opportunities for integration of pharmacokinetics, pharmacodynamics, and toxicokinetics in rational drug development. Clin Pharmacol Ther. 1992;51:465–73.
Noble D, Levin J, Scott W. Biological simulations in drug discovery. Drug Discov Today. 1999;4:10–6.
Lesko LJ, Rowland M, Peck CC, et al. Optimizing the science of drug development: opportunities for better candidate selection and accelerated evaluation in humans. Pharm Res. 2000;17:1335–44.
Drusano GL, Louie A, Deziel M, et al. The crisis of resistance: identifying drug exposures to suppress amplification of resistant mutant subpopulations. Clin Infect Dis. 2006;42:525–32.
Hutmacher MM, Mukherjee D, Kowalski KG, et al. Collapsing mechanistic models: an application to dose selection for proof of concept of a selective irreversible antagonist. J Pharmacokinet Pharmacodyn. 2005;32:501–20.
Danhof M. Systems pharmacology—towards the modeling of network interactions. Eur J Pharm Sci. 2016;30(94):4–14.
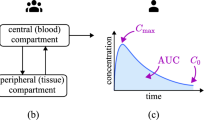
Mould DR, Upton RN. Basic concepts in population modeling, simulation, and model-based drug development—part 2: introduction to pharmacokinetic modeling methods. CPT: Pharm Syst Pharmacol. 2013;2:1–16.
Mould DR, Upton RN. Basic concepts in population modeling, simulation, and model-based drug development—part 3: introduction to pharmacodynamic modeling methods. CPT: Pharm Syst Pharmacol. 2014;3:1–18.
Ait-Oudhia S, Mager DE, Straubinger RM. Application of pharmacokinetic and pharmacodynamic analysis to the development of liposomal formulations for oncology. Pharmaceutics. 2014;6(1):137–74.
Jones H, Rowland-Yeo K. Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development. CPT Pharmacometrics Syst Pharmacol. 2013;2(8):e63.
U.S. Food and Drug Administration. Application of physiologically-based pharmacokinetic modeling to support dosing recommendations—the US Food and Drug Administration experience. 2016. https://www.ema.europa.eu/documents/presentation/presentation-application-physiologicallybased-pharmacokinetic-modeling-support-dosing_en.pdf. Accessed 22 Sept 2021.
Kimko H, Peck C. Clinical trial simulations: applications and trends. Berlin: Springer; 2011.
Liu X, Ward RM. Pharmacometrics in pediatrics. Ther Innov Regul Sci. 2019;53(5):579–83.
Bortz DM, Nelson PW. Model selection and mixed-effects modeling of HIV infection dynamics. Bull Math Biol. 2006;68:2005–25.
Pillai G, Gieschke R, Goggin T, et al. A semimechanistic and mechanistic population PK-PD model for biomarker response to ibandronate, a new bisphosphonate for the treatment of osteoporosis. Br J Clin Pharmacol. 2004;58(6):618–31.
Mostafavi S, Baranzini S, Oksernberg J, et al. Predictive modeling of therapy response in multiple sclerosis using gene expression data. Conf Proc IEEE Eng Med Biol Soc. 2006;1:5519–22.
Van der Helm-van Mil AH, le Cessie S, van Dongen H, et al. A prediction rule for disease outcome in patients with recentonset undifferentiated arthritis: how to guide individual treatment decisions. Arthritis Rheum. 2007;56:433–40.
Barton P, Jobanputra P, Wilson J, et al. The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumor necrosis factor in rheumatoid arthritis. Health Technol Assess. 2004;8:1–91.
Winter W, DeJongh J, Post T, et al. A mechanism-based disease progression model for comparison of long-term effects of pioglitazone, metformin and gliclazide on disease processes underlying Type 2 diabetes mellitus. J Pharmacokinet Pharmacodyn. 2006;33:313–43.
Gaitonde PG, Chien JY, Schmidt S. Drug-systems-disease model to predict treatment-outcome in type 2 diabetes mellitus. Clin Pharmacol Ther. 2015;97:S40–1.
Hurtado FKG, Garhyan P, Chien JY, et al. Development of a mechanism-based drug-disease modeling platform for type 2 diabetes mellitus. Clin Pharmacol Ther. 2016;99:S37.
Srinvas N, Maffuid K, Kashuba ADM. Clinical pharmacokinetics and pharmacodynamics of drugs in the central nervous system. Clin Pharmacokinet. 2018;54:1059–74.
Conrado DJ, Nicholas T, Tsai K, et al. Dopamine transporter neuroimaging as an enrichment biomarker in early Parkinson’s disease clinical trials: a disease progression modeling analysis. Clin Transl Sci. 2018;11:63–70.
Romero K, Conrado D, Burton J, et al. Molecular neuroimaging of the dopamine transporter as a patient enrichment biomarker for clinical trials for early Parkinson’s disease. Clin Transl Sci. 2019;12:240–6.
Stephenson D, Hill D, Cedarbaum MJ, et al. The qualification of an enrichment biomarker for clinical trials targeting early stages of Parkinson’s disease. J Park Dis. 2019;9:553–63.
Burger D, Agarwala S, Child M, et al.: Effect of rifampin on steadystate pharmacokinetics of atazanavir and ritonavir in healthy subjects. In: 12th Conference on Retroviruses and Opportunistic Infections, Boston, MA, 22–25 Feb 2005.
Zamek-Gliszczynski MJ, Chu X, Polli JW, et al. Understanding the transport properties of metabolites: case studies and considerations for drug development. Drug Metab Dispos. 2014;42(4):650–64.
Zanger Ulrich M, Matthias S. Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138(1):103–41.
Li M, Zhu L, Chen L, et al. Assessment of drug–drug interactions between voriconazole and glucocorticoids. J Chemother. 2018;30(5):296–303.
Back D, Marzolini C. The challenge of HIV treatment in an era of polypharmacy. J Int AIDS Soc. 2020;23(2):e25449.
Marzolini C, Rajoli R, Battegay M, et al. Physiologically based pharmacokinetic modeling to predict drug–drug interactions with efavirenz involving simultaneous inducing and inhibitory effects on cytochromes. Clin Pharmacokinet. 2017;56(4):409–20.
Dong M, Fukuda T, Selim S, et al. Clinical trial simulations and harmacometrics analysis in pediatrics: application to inhaled loxapine in children and adolescents. Clin Pharmacokinet. 2017;56:1207–17.
van Hasselt JG, van Eijkelenburg NK, Beijnen JH, et al. Design of a drug-drug interaction study of vincristine with azole antifungals in pediatric cancer patients using clinical trial simulation. Pediatr Blood Cancer. 2014;61:2223–9.
Wharton GT, Murphy MD, Avant D, et al. Impact of pediatric exclusivity on drug labeling and demonstrations of efficacy. Pediatrics. 2014;134:e512–8.
Ward RM, Drover DR, Hammer GB, et al. The pharmacokinetics of methadone and its metabolites in neonates, infants, and children. Pediatr Anaesth. 2014;24:591–601.
Li M, Gehring R, Riviere JE, et al. Probabilistic physiologically based pharmacokinetic model for penicillin G in milk from dairy cows following intramammary or intramuscular administrations. Toxicol Sci. 2018;164(1):85–100.
Buur J, Baynes R, Smith G, et al. Use of probabilistic modeling within a physiologically based pharmacokinetic model to predict sulfamethazine residue withdrawal times in edible tissues in swine. Antimicrob Agents Chemother. 2006;2006(50):2344–51.
DeWoskin RS, Sweeney LM, Teeguarden JG, et al. Comparison of PBTK model and biomarker based estimates of the internal dosimetry of acrylamide. Food Chem Toxicol. 2013;58:506–21.
Henri J, Carrez R, Meda B, et al. A physiologically based pharmacokinetic model for chickens exposed to feed supplemented with monensin during their lifetime. J Vet Pharmacol Ther. 2017;40:370–82.
Lin Z, Li M, Gehring R, et al. Development and application of a multiroute physiologically based pharmacokinetic model for oxytetracycline in dogs and humans. J Pharm Sci. 2015;104:233–43.
Ho DD, Neumann AU, Perelson AS, et al. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature. 1995;1995(373):123–6.
Perelson AS, Neumann AU, Markowitz M, et al. HIV-1 dynamics in vivo: virion clearance rate, infected cell life-span, and viral generation time. Science. 1996;271:1582–6.
Nowak MA, Bonhoeffer S, Shaw GM, et al. Anti-viral drug treatment: dynamics of resistance in free virus and infected cell populations. J Theor Biol. 1997;184:203–17.
Murray JM, Kaufmann G, Kelleher AD, et al. A model of primary HIV-1 infection. Math Biosci. 1998;154:57–85.
Kramer I. Modeling the dynamical impact of HIV on the immune system: viral clearance, infection, and AIDS. Math Comput Model. 1999;29:95–112.
Perelson AS, Nelson PW. Mathematical analysis of HIV-1 dynamics in vivo. SIAM Rev. 1999;41:3–44.
Wodarz D, Lloyd AL, Jansen VAA, et al. Dynamics of macrophage and T cell infection by HIV. J Theor Biol. 1999;196:101–13.
Stafford MA, Corey L, Cao Y, et al. Modeling plasma virus concentration during primary HIV infection. J Theor Biol. 2000;203:285–301.
Callaway DS, Perelson AS. HIV-1 infection and low steady state viral loads. Bull Math Biol. 2002;64:29–64.
Herz AVM, Bonhoeffer S, Anderson RM, et al. Viral dynamics in vivo: limitations on estimates of intracellular delay and virus decay. Proc Natl Acad Sci USA. 1996;93:7247–51.
Grossman Z, Feinberg M, Kuznetsov V, et al. HIV infection: how effective is drug combination treatment? Immunol Today. 1998;19:528–32.
Mittler JE, Sulzer B, Neumann AU, et al. Influence of delayed viral production on viral dynamics in HIV-1 infected patients. Math Biosci. 1998;152:143–63.
Nelson PW, Murray JD, Perelson AS. A model of HIV-1 pathogenesis that includes an intracellular delay. Math Biosci. 2000;163:201–15.
Nelson PW, Perelson AS. Mathematical analysis of delay differential equation models of HIV-1 infection. Math Biosci. 2002;179:73–94.
Lloyd AL. The dependence of viral parameter estimates on the asumed viral load life cycle: Limitations of studies of viral load data. Proc R Soc Lond Ser B. 2001;268:847–54.
Liu Stephanie N, Desta Z, et al. Probenecid-Boosted Tenofovir: a physiologically-based pharmacokinetic model-informed strategy for on-demand HIV preexposure prophylaxis. CPT Pharmacometrics Syst Pharmacol. 2019. https://doi.org/10.1002/psp4.12481.
Riggs MM, Cremers S. Pharmacometrics and systems pharmacology for metabolic bone diseases. Br J Clin Pharmacol. 2019;85(6):1136–46.
Post TM, Schmidt S, Peletier LA, et al. Application of a mechanism-based disease systems model for osteoporosis to clinical data. J Pharmacokinet Pharmacodyn. 2013;40(2):143–56.
Ross DS, Mehta K, Cabal A. Mathematical model of bone remodeling captures the antiresorptive and anabolic actions of various therapies. Bull Math Biol. 2017;79(1):117–42.
Cremers SCLM, Pillai G, Papapoulos SE. Pharmacokinetics/pharmacodynamics of bisphosphonates: use for harmacometr of intermittent therapy for osteoporosis. Clin Pharmacokinet. 2005;44(6):551–70.
Peterson MC, Riggs MM. A physiologically based mathematical model of integrated calcium homeostasis and bone remodeling. Bone. 2010;46(1):49–63.
Pivonka P, Zimak J, Smith DW, et al. Model structure and control of bone remodeling: a theoretical study. Bone. 2008;43(2):249–63.
Post TM, Freijer JI, DeJongh J, et al. Disease system analysis: basic disease progression models in degenerative disease. Pharm Res. 2005;22(7):1038–49.
Riggs M M, Gillespie W R, Gastonguay M R, et al. Extension of a multiscale model of calcium homeostasis and bone remodeling to include the progressive effects of estrogen loss during menopause transition [Conference presentation]. In: National Institute of General Medical Sciences, Quantitative and System Pharmacology Workshop II, Bethesda, MD, 9 September 2010.
Lien YTK, Madrasi K, Samant S, et al. Establishment of a disease-drug trial model for postmenopausal osteoporosis: a zoledronic acid case study. J Clin Pharmacol. 2020;60(2):86–102.
Kassahun K, McIntosh I, Koeplinger K, et al. Disposition and metabolism of the cathepsin K inhibitor odanacatib in humans. Drug Metab Dispos. 2014;42(5):818–27.
Zajic S, Stone JA, Jaworowicz D. Semi-mechanistic PK/PD model of the effect of odanacatib, a cathepsin K inhibitor, on bone turnover to characterize lumbar spine and distal forearm bone mineral density in a phase IIb study of postmenopausal women. PAGE Abstr Annu Meet Popul Approach Gr Eur. 2011;20:2190.
Zajic S, Rossenu S, Hreniuk D, et al. The absolute bioavailability and effect of food on the pharmacokinetics of odanacatib: a stable-label i.v./oral study in healthy postmenopausal women. Drug Metab Dispos. 2016;44(9):1450–8.
Ma B, Luo B, Euler DH, et al. Applicability of in vitro-in vivo translation of cathepsin K inhibition from animal species to human with the use of free-drug hypothesis. Naunyn Schmiedebergs Arch Pharmacol. 2017;390(4):435–41.
Gaitonde P, Hurtado FK, Garhyan P, et al. Development and qualification of a drug-disease modeling platform to characterize clinically relevant endpoints in type 2 diabetes trials. Clin Pharmacol Ther. 2018;104(4):699–708.
Mandema JW, Cox E, Alderman J. Therapeutic benefit of Eletriptan compared to Suma triptan for the acute relief of migraine pain results of a model based meta analysis that accounts for encapsulation. Cephalalgia. 2005;25:715–25.
Samtani M. Simple pharmacometric tools for oral anti diabetic drug development: competitive landscape for oral non insulin therapies in type 2 diabetes. Biopharm Drug Dispos. 2010;31:162–77.
Normand SL. Meta analysis: formulating, evaluating, combining, and reporting. Stat Med. 1999;18:321–59.
Berry DA, Berry SM, McKellar J, et al. Comparison of the dose response relation ships of 2 lipid lowering agents: a Bayesian meta analysis. Am Heart J. 2003;145:1036–45.
Heard RN. The spectrum of multiple sclerosis. Curr Allergy Asthma Rep. 2007;7:280–4.
Novakovic AM, Thorsted A, Schindler E, et al. Pharmacometric analysis of the relationship between absolute lymphocyte count and expanded disability status scale and relapse rate, efficacy end points, in multiple sclerosis trials. J Clin Pharmacol. 2018;58(10):1284–94.
Hu X, Hang Y, Cui Y, et al. Population-based pharmacokinetic and exposure-efficacy analyses of peginterferon beta-1a in patients with relapsing multiple sclerosis. J Clin Pharmacol. 2017;57(8):1005–16.
U.S. Food and Drug Administration. General clinical pharmacology considerations for pediatric studies for drugs and biological products—draft guidance for industry. 2014.
European Medicines Agency (EMA). Concept paper on extrapolation of efficacy and safety in medicine development. EMA. 2013. Accessed from https://www.ema.europa.eu/en/documents/scientific-guideline/concept-paper-extrapolation-efficacy-safety-medicine-development_en.pdf
Kearns GL, Abdel-Rahman SM, Alander SW, et al. Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med. 2003;349:1157–67.
Stockmann C, Barrett JS, Roberts JK, et al. Use of modeling and simulation in the design and conduct of pediatric clinical trials and the optimization of individualized dosing regimens. CPT Pharmacometrics Syst Pharmacol. 2015;4:630–40.
Vinks AA, Emoto C, Fukuda T. Modeling and simulation in pediatric drug therapy: application of pharmacometrics to define the right dose for children. Clin Pharmacol Ther. 2015;98:298–308.
Mehrotra N, Bhattaram A, Earp JC, et al. Role of quantitative clinical pharmacology in pediatric approval and labeling. Drug Metab Dispos. 2016;44(7):924–33.
Ogungbenro K, Aarons L, CRESim. A physiologically based pharmacokinetic model for clobazam and stiripentol in adults and children. Pharm Res. 2015;32:144–57.
Ogungbenro K, Aarons L, CRESim. Physiologically based pharmacokinetic modelling of methotrexate and 6-mercaptopurine in adults and children. Part 1: methotrexate. J Pharmacokinet Pharmacodyn. 2014;41:159–71.
Maharaj AR, Barrett JS, Edginton AN. A workflow example of PBPK modeling to support pediatric research and development: case study with lorazepam. AAPS J. 2013;15:455–64.
Jiang XL, Zhao P, Barrett JS, et al. Application of physiologically based pharmacokinetic modeling to predict acetaminophen metabolism and pharmacokinetics in children. CPT Pharmacometrics Syst Pharmacol. 2013;2:e80.
Leong R, Vieira MLT, Zhao P, et al. Regulatory experience with physiologically based pharmacokinetic modeling for pediatric drug trials. Clin Pharmacol Ther. 2012;91:926–31.
Life Science Leader. 2021. https://www.lifescienceleader.com/doc/why-animal-health-is-the-next-big-growth-area-0001. Accessed 14 Oct 2021
Li M, Gehring R, Riviere JE, Lin Z. Probabilistic physiologically based pharmacokinetic model for penicillin G in milk from dairy cows following intramammary or intramuscular administrations. Toxicol Sci. 2018;164(1):85–100.
Cox SR, Liao S, Payne-Johnson M, et al. Population pharmacokinetics of mavacoxib in osteoarthritic dogs. J Vet Pharmacol Ther. 2011;34(1):1–11.
European Medicines Agency (EMA). CVMP assessment report for CYTOPOINT (EMEA/V/C/003939/0000). 2017. Accessed from https://www.ema.europa.eu/en/documents/assessment-report/cytopoint-epar-public-assessment-report_en.pdf.
Ridker PM, Tardif JC, Amarenco P, et al. Lipid-reduction variability and antidrug-antibody formation with bococizumab. N Engl J Med. 2017;376(16):1517–26.
Jones HM, Zhang Z, Jasper P, et al. A physiologically-based pharmacokinetic model for the prediction of monoclonal antibody pharmacokinetics from in vitro data. CPT Pharmacometrics Syst Pharmacol. 2019;8(10):738–47.
Sahota T, Danhof M, Della PO. The impact of composite AUC estimates on the prediction of systemic exposure in toxicology experiments. J Pharmacokinet Pharmacodyn. 2016;42:251–61.
Tan Y-M, Worley RR, Leonard JA, et al. Challenges associated with applying physiologically based pharmacokinetic modeling for public health decision-making. Toxicol Sci. 2018;162(2):341–8.
Bonate PL. PK-PD Modeling and Simulation, 2nd Ed Allerheiligen, SRB. Clin Pharmacol Ther. 2014;96(4):413–5.
Acknowledgements
The authors would like to thank Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Pró-reitoria de Pesquisa Pós-graduação (PROPPI/UFOP) for providing financial support.
Author information
Authors and Affiliations
Contributions
LCB: Conceptualization, Data curation, Writing—original draft, review and editing; LP Co-supervision, Writing—review and editing; CMC: Writing—review and editing, Supervision, Funding acquisition, Project administration, Resources.
Corresponding author
Ethics declarations
Conflict of interest
Authors state no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bandeira, L.C., Pinto, L. & Carneiro, C.M. Pharmacometrics: The Already-Present Future of Precision Pharmacology. Ther Innov Regul Sci 57, 57–69 (2023). https://doi.org/10.1007/s43441-022-00439-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43441-022-00439-4