Abstract
Introduction
Using data from patients residing in Salford, UK, we aimed to compare healthcare resource utilisation (HCRU) and direct healthcare costs between patients with moderate to severe (M-S) or severe osteoarthritis (OA) pain and those without OA.
Methods
Patients with a M-S OA pain event within a period of chronic pain were indexed from the Salford Integrated Record (SIR) between 2010 and 2017. Patients with a severe pain event formed an OA subcohort. Patients in each OA pain cohort were independently matched to patients without OA, forming two control cohorts. HCRU, prescribed analgesic drugs, and total direct costs per UK standardised tariffs were calculated for the year post-index. Multivariable models were used to identify drivers of healthcare cost.
Results
The M-S OA pain and control cohorts each comprised 3123 patients; the severe OA pain and control cohorts each comprised 1922 patients. Patients in both OA pain cohorts had a significantly higher mean number of general practitioner encounters, inpatient, outpatient, and accident and emergency visits, and were prescribed a broader range of analgesic drugs in the year post-index than respective controls. Mean healthcare costs of all types were significantly higher in the M-S and severe OA pain cohorts vs controls (total: M-S £2519 vs £1379; severe £3389 vs £1397). Paracetamol (M-S: 40% of patients had at least one prescription; severe: 50%) and strong opioids (34% and 59%) were the analgesics most prescribed to patients with OA pain. In all cohorts, multivariable models showed that a higher age at index, the presence of gout, osteoporosis, type 2 diabetes, or coronary artery disease, significantly contributed towards higher healthcare costs.
Conclusion
In the population of Salford, UK, patients with M-S OA pain had significantly higher annual HCRU and costs compared with matched controls without OA; generally, these were even higher in patients with severe OA pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study ? |
There is a lack of research evaluating the healthcare resource utilisation (HCRU) and associated costs of moderate to severe and severe osteoarthritis (OA) pain in the United Kingdom (UK). The aim of this analysis was to quantify this burden at a local level among patients treated in Salford, UK. |
What was learned from the study ? |
Four cohorts of patients were indexed from the Salford Integrated Record (SIR), which represents a unique database of complete primary and secondary care data from a metropolitan UK health region: (1) patients with moderate to severe OA pain and (2) matched controls; (3) patients with severe OA pain and (4) matched controls. Specific pain scoring for OA is not recorded in the SIR, so the level of OA pain was inferred from healthcare utilisation behaviour. Patients in the control groups were from the general population without OA and were matched to each patient with OA pain by age, sex, and comorbidity burden using propensity scoring. |
Patients with moderate to severe OA pain had a significantly higher mean number of general practitioner encounters, inpatient admissions, and outpatient and accident and emergency visits than controls, and they utilised a broader range of analgesic drug classes. |
Almost twofold higher healthcare costs were observed in patients with moderate to severe OA pain than controls. In general, HCRU and costs were even higher in patients with severe OA pain, demonstrating that the burden increases alongside pain intensity. In all cohorts, multivariable models showed that a higher age at index, the presence of gout, osteoporosis, type 2 diabetes, or coronary artery disease significantly contributed towards higher healthcare cost. |
This study demonstrates the significant local burden of moderate to severe and severe OA pain in Salford, which may also be indicative of that in the wider UK. |
Digital Features
This article is published with digital features, including a graphical plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.19140035.
Introduction
Over one-third of the United Kingdom (UK) population is thought to experience chronic pain, with more than 10% struggling to take part in daily activities [1, 2]. Chronic pain presents as a significant national and personal burden [3,4,5,6]. Musculoskeletal conditions, including osteoarthritis (OA), are an important risk factor for chronic pain in the UK [5, 7,8,9,10]. A substantial proportion of those with OA (40–60%) experience moderate to severe pain [11,12,13,14,15,16,17]. As OA is a relatively common condition, OA pain is a significant burden to not only the patient but also the healthcare system and economy as a whole [11,12,13,14,15,16]. Previous findings from various countries (most commonly the United States) have consistently shown higher healthcare resource utilisation (HCRU) and costs in patients with chronic OA pain compared with the general population [6, 13, 15, 18,19,20,21,22,23,24,25,26].
There is a lack of data reporting on the use of healthcare resources and associated costs for patients with moderate to severe OA pain in the UK [2]. These are likely to differ from those reported in the United States due to the nature of the regional healthcare systems and treatment pathways [2]. A recent analysis of linked data for primary (Clinical Practice Research Datalink [CPRD]) and secondary (Hospital Episode Statistics [HES]) care in England showed that patients with moderate to severe OA pain consistently used more healthcare services compared with control patients without OA [27]. This included significantly more general practitioner (GP) consultations, outpatient attendances, accident and emergency (A&E) visits, inpatient stays, and a significantly higher overall direct cost (+ £4778 per patient over 2 years) [27]. Although linked CPRD-HES data are available for patients located across England, many health services are managed at a local level, and there are regional differences in the incidence and management of OA, possibly for socioeconomic reasons [28,29,30]. Understanding the local burden of OA pain could help regions of the UK better understand and adapt to the specific needs of their patients.
The Salford Integrated Record (SIR) is a unique database of deidentified Electronic Healthcare Records from the population of Salford, Greater Manchester, UK [31,32,33]. It is a comprehensive repository of primary and secondary healthcare utilisation for approximately 251,000 people, including data from 45 GP surgeries and a large university teaching hospital [31, 33]. The aim of this analysis was to better understand the HCRU and cost burden associated with moderate to severe and severe OA pain in patients treated in Salford, UK, using the rich data included in the SIR. We hypothesised that HCRU and cost will be higher in patients with OA pain than in those without OA, and that HCRU and costs will increase with OA pain severity.
Methods
Study
This was a retrospective, longitudinal, matched-cohort study using data from the SIR. Salford is a relatively deprived metropolitan borough of Greater Manchester in North-West England [34]. The SIR contains complete primary and secondary public healthcare data for all patients (excluding ~ 3% of the population who have opted out) in the Salford region from around 2008. Primary data completeness has been verified against third-party data extracts. A verification prior to the use of the SIR for pragmatic trials of respiratory drugs has been published [31]. Secondary data in the SIR replicate that used for hospital reimbursement. The quality, coverage, and completeness of SIR data are considered to be of a very high standard, and the SIR has previously been used in a number of high-quality studies [31, 35, 36]. When the SIR was developed, mental and sexual health data were excluded due to sensitivity; some other conditions were also erroneously removed (inguinal hernia, angina, and some strokes). The SIR does not routinely capture out-of-area hospital data (which is mainly a limitation for cardiac surgery). It also does not capture data for patients living in Salford and registered with out-of-area GP practices, but it does include patients living outside Salford and registered with GP practices within Salford.
The study protocol was examined by the SIR Review Board as part of the data extract request application process. No separate ethics committee review process was required. The study was conducted in accordance with all legal and regulatory requirements, as well as with scientific purpose, value, and rigour. It followed generally accepted research practices described in the Guidelines for Good Pharmacoepidemiology Practices, Good Practices for Outcomes Research, and the Declaration of Helsinki.
Cohorts
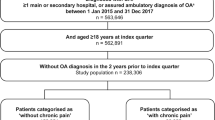
Patients ≥ 18 years old with at least one moderate to severe or severe pain event within an episode of chronic pain (see definition below) were indexed from the SIR between 1 January 2010 and 31 December 2017 (Fig. 1) [27]. Patients must have had at least one prior diagnosis of OA in their recorded medical history, as defined by read or International Classification of Diseases 10th revision codes (see Table S1 in the electronic supplementary material for details). A chronic pain episode was initiated when a patient attended a GP consultation relating to OA pain. This must have been followed by similar pain-related consultations with a GP or specialist in rheumatology, orthopaedics, or pain management in the following 3–12 months. The chronic pain episode ended when no further consultations were recorded in a 12-month period. Patients were indexed in the moderate to severe OA pain cohort if they had at least one moderate to severe pain event during a chronic pain episode, defined as (1) referral or attendance to a rheumatology, orthopaedics, or pain management department; (2) a surgical or non-surgical invasive procedure for OA in secondary care; (3) at least two prescriptions for nonsteroidal anti-inflammatory drugs (NSAIDs), including at least two different NSAIDs, within a 3-month period; (4) at least two prescriptions for opioids within a 3-month period; or (5) an A&E visit relating to pain followed by a GP visit relating to OA pain in the following 14 days. Patients who met criterion 2, 4, or 5 were additionally indexed in the severe OA pain cohort. Patients may have been indexed in both the moderate to severe and severe OA pain cohorts, but their index dates for each cohort may be different.
Study design. aOA diagnosis defined through International Classification of Disease, 10th revision codes or read codes at any time in the patient’s medical history (see Table S1). Note that surgical interventions were assessed in the 2 years post-index; however, this was a secondary analysis, and patients were not required to have 2 years of follow-up. OA osteoarthritis
Each patient with OA was matched by age, sex, and Charlson Comorbidity Index (CCI) to the nearest patient (control) who did not have a diagnosis of OA at any point in their medical history. Comorbidities were taken from the patient’s recorded medical history prior to the index date. Most controls were exact matches, and the remainder were matched to the nearest neighbour using logistic-regression-based propensity scoring. Matching was done independently for the moderate to severe and severe OA pain cohorts. The two control cohorts did not generally contain the same patients; however, a patient could be indexed in both control cohorts if matched to the same or different patients with OA pain. Controls were assigned a pseudo-index date equal to the patient they were matching. All indexed patients (OA or control) must have been continuously registered with a GP in Salford for 12 months prior and 12 months following index, as indicated by any acute prescription or face-to-face practice appointment.
Outcomes
The primary aim of the study was to compare HCRU and costs for the 12 months following index in patients with moderate to severe OA pain vs controls from the general patient population without OA. A secondary aim was to compare these outcomes in the subgroup of patients with severe OA pain.
In this study, HCRU included GP encounters, inpatient admissions, outpatient visits, and A&E attendances for any reason. Some subtypes of encounter/visit are presented. Total direct healthcare costs included the cost of these HCRUs plus the cost of prescribed analgesic drugs. Factors associated with increased healthcare costs were evaluated using multivariable analyses.
We additionally conducted some exploratory analyses of the proportion of patients with surgical interventions in the 2 years post-index, the factors associated with the risk of surgical interventions, and the number of prescriptions for specific types of analgesic drugs in the 12 months post-index (see Table S2 in the electronic supplementary material for definitions of the HCRU and cost outcomes).
Statistical Analysis
Demographics and clinical characteristics at index, HCRU, analgesic drug use, and costs during the 12 months post-index were summarised descriptively. Means were compared by t test, and categorical variables were compared using the chi-squared test. Comorbidities of interest included asthma, coronary artery disease, cerebrovascular disease, depression (inferred from antidepressant prescriptions in the patient’s recorded medical history), fibromyalgia, gout, hyperlipidaemia, hypertension, osteoporosis, psoriatic arthritis, rheumatoid arthritis, ankylosing spondylitis, and type 2 diabetes. Throughout the analyses, a standardised difference (STD) of > 0.1 was considered meaningful.
Predictors of higher healthcare cost in each cohort were analysed by multivariable analyses in Stata 15, initially using a two-part model but reverting to a generalised linear model with log link and underlying gamma distribution if the two-part model had problems converging. Both provided a mean, 95% confidence interval, and p value for the OA pain vs control cohorts. Only eight of the 3123 patients in the moderate to severe OA pain cohort and none of the 1922 in the severe OA pain cohort had zero healthcare costs. Overall, 430 patients in the moderate to severe control cohort and 250 in the severe control cohort had zero cost. Covariates included in the initial regression model were age, sex, body mass index (BMI; both categorical and continuous), smoking status, CCI, and the comorbidities of interest. After backward elimination, the final models included only covariates with p < 0.05. Interaction terms with p < 0.15 were also retained.
The proportion of patients with surgical procedures for OA in the 2 years following index and the mean time from index to first OA-related surgical intervention were summarised descriptively. Predictors of risk for an OA-related surgical procedure were assessed using the Cox proportional hazards model. The statistical significance of the models was evaluated using the likelihood ratio test, the Wald test, and log-rank statistics.
Results
A plain language summary of this study is available as Fig. S1.
Cohorts
In total, 12,534 patients with OA were identified across primary and secondary SIR data (Fig. 2). Of these, 3123 patients met the inclusion criteria for the moderate to severe OA pain cohort, and 1922 of these additionally met the inclusion criteria for the severe OA pain cohort. Two matching control cohorts were independently formed. The median follow-up duration was 45 months for the moderate to severe OA pain and matching control cohorts (n = 2402 and n = 3123, respectively, had ≥ 24 months follow-up), and 47 months for the severe OA pain and matching control cohorts (n = 1513 and n = 1922, respectively, had ≥ 24 months follow-up).
Baseline Characteristics
Patients with moderate to severe OA pain were predominantly female (61%) with a mean age of 63 years at index (Table 1). In the severe OA pain cohort, 65% of patients were female with a mean age of 64 years at index. Along with CCI (median score of 3 in all cohorts), these variables were used to match individual controls to patients with OA pain. Due to incomplete matching, there were minor differences in the mean age (1 year) and proportion of female patients (< 1% of patients) between the OA pain cohorts and respective control cohorts. Patients in both the moderate to severe and severe OA pain cohorts had significantly higher BMI than those in the control cohorts (p < 0.001; STD 0.325–0.439 for continuous and categorical measures), and a range of comorbidities of interest were significantly more prevalent, namely asthma, depression, fibromyalgia, gout, hyperlipidaemia, hypertension, osteoporosis, psoriatic arthritis, rheumatoid arthritis, and ankylosing spondylitis (p < 0.01; STD 0.071–0.570; Table S3).
Interestingly, type 2 diabetes was significantly less prevalent in both cohorts with OA pain, although also with a relatively small magnitude of difference (p < 0.001; STD 0.196–0.212). Depression (derived from an antidepressant prescription in the patient’s recorded medical history) had the largest STD in the moderate to severe OA pain vs control cohorts (0.481) and in the severe OA pain vs control cohorts (0.570).
HCRU
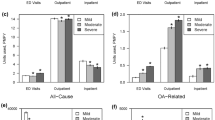
Patients with moderate to severe OA pain or severe OA pain had a higher mean number of GP encounters, inpatient admissions, outpatient visits, and A&E attendances as compared with matched patients in the control cohorts (p < 0.05; STD 0.051–0.453; Fig. 3; Table 2). The STDs between OA and control cohorts were generally larger for those with the severe OA pain (0.125–0.453) than for those with moderate to severe OA pain (0.051–0.360). Data on subtypes of encounter/visit are included in Table 2.
Mean HCRU per patient in the 12 months post-index. Number above the bar (+ SD) indicates the mean in the 12 months post-index. All comparisons with the respective control are p < 0.05. Moderate to severe OA pain and matched control cohorts each comprise 3123 patients. Severe OA pain and matched control cohorts each comprise 1922 patients. A&E accident and emergency, GP general practitioner, HCRU healthcare resource utilisation, OA osteoarthritis, SD standard deviation
GP Encounters
A higher proportion of patients with moderate to severe OA pain had at least one face-to-face GP practice appointment (86% vs 66%) or GP telephone consultation (50% vs 39%) compared with patients in the control cohort (Table 2). Although the trends were the same for the severe OA pain and respective control cohorts, the magnitude of these differences was larger for practice appointments and telephone consultations than between the moderate to severe OA pain and control cohorts (Table 2).
Inpatient Admissions
More than double the proportion of patients in the moderate to severe OA pain (43%) and severe OA pain cohorts (53%) had one or more inpatient admission than in the respective control cohorts (both 21%; Table 2). The mean number of admissions per patient was significantly higher in the moderate to severe OA pain cohort than the control cohort for day cases (STD 0.129) and elective admissions (STD 0.427), but not for non-elective admissions (p > 0.05; Table 2). Results for the severe OA pain and matched control cohort were similar (all p < 0.01; Table 2).
Among patients with at least one inpatient stay of any kind, mean length of stay was significantly lower in those with moderate to severe OA pain (4.64 days ± 10.61) or severe OA pain (5.69 days ± 14.21) than in the respective control cohorts (10.28 days ± 18.85 and 10.52 days ± 19.08; both p < 0.001; STD 0.369 and 0.288; Table 2). The largest STDs were seen for elective surgeries, which would include most OA-related surgical interventions (STD for OA pain vs control cohorts: 0.381 and 0.417 for moderate to severe and severe, respectively).
OA-Related Surgical Interventions in the 24 Months Post-Index
Overall, 13.4% of patients in the moderate to severe OA pain cohort had one or more total joint replacements over the 24 months post-index: 6.1% had one or more intra-articular joint injections, 1.5% had one or more arthroscopies, 0.6% had one or more arthrodesis surgeries, and 0.7% had osteotomies. Twelve patients with moderate to severe OA pain had two procedures each.
A slightly higher proportion of patients in the severe OA pain cohort had one or more of each type of surgical intervention (22.2% had one or more total joint replacements, 9.9% had one or more intra-articular joint injections, 2.7% had one or more arthroscopies, 1.2% had one or more arthrodesis surgeries, and 1.0% had osteotomies). Thirteen patients with severe OA pain had two procedures each.
As might be expected, hardly any procedures were recorded for patients in the control cohort (no more than four patients had one or more of each surgical intervention type in each cohort).
Excluding patients who had a surgical intervention on the day of index, the mean time from index to first OA-related surgical intervention was estimated to be 256.87 days (standard deviation [SD] 202.25) in the moderate to severe OA pain cohort and 281.68 days (198.24) in the severe OA pain cohort. A Cox proportional hazards model was used to examine the factors that influenced the risk of having an OA-related surgical intervention (Fig. 4). The model for the moderate to severe OA pain cohort showed osteoporosis (hazard ratio [HR] 0.64; associated with 36% less risk), fibromyalgia (HR 0.59; associated with 41% less risk), and age at index (HR 1.01; associated with 1% extra risk per year older) to be significant (p < 0.05) predictors of a post-index OA-related surgical intervention. Surgical intervention was a criterion for inclusion in the study for both moderate to severe and severe OA pain cohorts. As a high proportion of the patients with severe OA pain (n = 344/1922) were indexed on this criterion, the hazards model was not pursued.
Hazard ratio for the risk of OA-related surgical interventions in the cohort of patients with moderate to severe OA pain. Includes 512 first surgical events that took place after the index date for patients with a full set of covariates. Global p = 0.01 from log-rank test. n = 3123 except for comparison groups: female, n = 1903; male, n = 1220; current smoker, n = 518; former smoker, n = 982; never smoked, n = 1198. Data for unknown/missing smoking status not shown (hazard ratio 1.47 vs current smoker; 95% CI 0.20, 10.62). *p < 0.05. BMI body mass index, CCI charlson comorbidity index, CI confidence interval
Outpatient Admissions
Overall, 97% of patients in the moderate to severe OA pain cohort and 91% of those in the severe OA pain cohort had at least one outpatient visit, compared with 57% and 58%, respectively, in the matched control cohorts (Table 2). As might be expected, the proportions of patients with at least one orthopaedic and specialist pain management clinic visit were approximately tenfold higher per patient in the OA pain cohorts than in the control cohorts (p < 0.001; STD 0.335–1.309; Table 2). The difference in the proportion of patients with at least one physiotherapy visit was over sevenfold (32% of patients in each of the OA cohorts compared with 5% in each of the control cohorts; STD 0.576 and 0.621, respectively) and over fivefold for rheumatology (19% and 16% in the moderate to severe and severe OA pain cohorts, respectively, compared with 3% in the control cohorts; STD 0.311–0.355). The mean number of visits per patient was significantly higher for patients in the OA pain cohorts than in the control cohorts for all outpatient specialities except psychotherapy (both OA pain cohorts) and cardiology (in the severe OA pain cohort).
A&E Attendance
Similar to other types of HCRU, the proportion of patients with at least one A&E attendance was higher in the moderate to severe OA pain and severe OA pain cohorts, respectively, vs their respective controls (28% vs 22% and 32% vs 20%; Table 2). The mean (± SD) number of A&E attendances that led to hospitalisation per patient was similar in the moderate to severe OA pain and control cohorts (0.19 ± 0.59 vs 0.21 ± 0.68, p = 0.165; STD 0.035) but higher in the severe OA pain cohort (0.26 ± 0.74 vs 0.19 ± 0.61, p < 0.001; STD 0.096).
Utilisation of Analgesic Drugs
Patients with OA pain utilised a broader range of prescribed analgesic drugs in the 12 months post-index compared with controls. Prescribed drugs were classed as (1) adjuvants, (2) non-opioids, or (3) opioids. The proportion of patients prescribed drugs from any two of the classes was higher in the moderate to severe (33%) and severe (44%) OA pain cohorts than in the control cohorts (11% and 12%, respectively). Findings were similar for the proportions of patients prescribed drugs from all three classes (19% of the moderate to severe and 32% of the severe OA pain cohorts vs 4% in the control cohorts). All subtypes of analgesic drugs had a significantly higher mean number of prescriptions per patient in the chronic OA pain cohorts compared with the control cohorts, except for anxiolytics and hypnotics in the moderate to severe OA pain cohort (Table 3). This included antidepressants, though the proportions of patients with prescriptions in the 12 months post-index were much lower than those identified in prior medical records (Table 3 and Table S3). The three most widely used analgesic drug types in patients with chronic OA pain were paracetamol (at least one prescription for 40% of patients in the moderate to severe vs 50% in the severe OA pain cohorts), strong opioids (34% vs 59%), and oral NSAIDs (30% vs 31%; Table 3).
Direct Healthcare Costs
The total direct healthcare cost in the 12 months following index was significantly higher in patients with moderate to severe OA pain as compared with patients in the control cohort (£2519 SD: £3511 vs £1379 SD: £3787, p < 0.001; STD 0.312; Fig. 5; Table 4). The difference was even greater between the severe OA pain and control cohorts (£3389 SD: £4464 vs £1397 SD: £3884; p < 0.001; STD 0.476).
Direct healthcare costs in the 12 months post-index. Bar annotations indicate means in the 12-months post-index. All comparisons with the respective control are p < 0.001. Moderate to severe OA pain and matched control cohorts each comprise 3123 patients. Severe OA pain and matched control cohorts each comprise 1922 patients. A&E accident and emergency, GP general practitioner, OA osteoarthritis
The largest contributors to healthcare cost were inpatient admissions and outpatient visits, though all types of cost were significantly higher in the OA pain cohorts than in the respective control cohorts (STD 0.090–0.522). Cost components with the highest STDs were analgesic drugs (STD 0.314–0.522) and inpatient admissions (STD 0.270–0.434).
Univariate analyses showed all covariates (age, sex, BMI [both categorical and continuous], CCI, smoking status, and the comorbidities of asthma, coronary artery disease, cerebrovascular disease, depression, fibromyalgia, gout, hyperlipidaemia, hypertension, osteoporosis, psoriatic arthritis, rheumatoid arthritis, spondylitis, and type 2 diabetes) to be associated with a significant increase in total mean healthcare cost for the OA pain cohorts, except for sex in the severe OA pain cohort (see Table S4 in the electronic supplementary material).
The multivariable model produced total mean healthcare costs similar to those derived from descriptive statistics (£2484 for patients with moderate to severe OA pain; £1497 for their matched controls; £3413 for patients with severe OA pain; £1507 for their controls). Many of the variables identified in the univariate analysis were also considered significant predictors of higher healthcare costs in one or both multivariable analyses (see Table S5 in the electronic supplementary material).
Marginal contributions to overall healthcare costs from each variable for the moderate to severe OA pain cohort are shown in Table 5 and Table S6 in the electronic supplementary material, and are shown for the severe OA pain cohort in Table 6 and Table S7 in the electronic supplementary material. Being in the moderate to severe OA pain cohort was associated with a £987 higher mean healthcare cost in the 12 months following index than a matched control. Being in the severe OA pain cohort was associated with a £1906 higher cost than a matched control. When the OA pain and control cohorts are viewed together, the biggest contributors to cost were the comorbidities of gout (£353 in the moderate to severe OA pain cohort and £1970 in the control cohort; £108 in the severe OA pain cohort and £1875 in the control cohort; calculated as marginal costs for patients with vs without in each cohort) and osteoporosis (moderate to severe OA pain: £362; control: £1927; severe OA pain: £1010; control: £2217). Type 2 diabetes was associated with a considerable marginal cost in all cohorts, which was most notable in patients in the control cohorts (£532 in the moderate to severe OA pain and £949 in control cohorts; £293 in severe OA pain and £739 in control cohorts); as was coronary artery disease (£226 in the moderate to severe OA pain and £547 in control cohorts; £778 in the severe OA pain and control cohorts). Each year older at index was associated with a £29 higher healthcare cost in the moderate to severe OA pain model and a £25 higher healthcare cost in the severe OA pain model.
Discussion
This retrospective, longitudinal, matched-cohort study using data from the SIR showed that patients residing in Salford, UK, with moderate to severe OA pain had considerably higher HCRU and incurred almost double the annual direct costs of patients without OA. HCRU and costs were generally greater in the subgroup of patients with severe OA pain. Our findings demonstrate the significant burden of chronic OA pain on the local healthcare system in Salford, UK.
The population of patients with OA pain in Salford was typical for the UK and internationally—predominantly female, a mean age of ~ 65 years, more likely to be overweight, and with a higher level of comorbidity than patients in the general population [17]. Patients in both control cohorts were matched by propensity scoring on age, sex, and CCI to balance these features. Despite matching on CCI, on average, patients with chronic OA pain had significantly higher prevalences of several pre-specified comorbidities than their matched controls. Of these, depression was the comorbidity with the largest magnitude of difference. There is a complex interplay between OA and depression, and findings of a higher depression prevalence among patients with OA is expected; however, our results must be interpreted with caution, as patients with depression were considered to be those with an antidepressant prescription at any time in their recorded medical history [37, 38].
Patients with moderate to severe and severe OA pain had a significantly higher mean number of GP encounters (practice appointments and telephone consultations), inpatient admissions (overall, day, and elective admissions), outpatient visits (overall, gastroenterology, orthopaedic, physiotherapy, rheumatology, and pain management clinics), and A&E attendances as compared with matched controls. Mean HCRU of all types was generally highest in the cohort of patients with severe OA pain.
Due to the specific nature of our cohort definitions and the data held in the SIR, it is challenging to compare the incidence of HCRU with previously published studies. However, several studies support our findings of increasing HCRU with increasing OA pain severity in other populations [12, 13, 15, 27, 39]. A recent study using CPRD data from across the UK used almost identical inclusion criteria to ours for patients with moderate to severe OA pain and control cohorts [27]. This analysis included 28% of patients from the North of the UK, which would include Salford. Findings of higher HCRU in patients with moderate to severe OA pain were reported, but the mean number of GP encounters over the 12 months post-index was twice as high as in our analysis (12.88 vs 5.33 in our study), whereas the number of outpatient visits was lower (7.37 vs 11.19). The reasons for these minor divergences are not clear but likely represent differences in coding practices between the CPRD and the SIR. There may also be specific differences in the healthcare pathways employed in Salford that are not well reflected in pooled national data.
More than double the proportion of patients in the moderate to severe OA pain (43%) and severe OA pain cohorts (53%) had at least one inpatient admission of any type than in the respective control cohorts (both 21%). Among these patients, the mean length of stay was significantly shorter in the OA pain cohorts. Our analyses showed elective admissions to have particularly high standardised mean differences vs control cohorts. Along with our brief analysis of OA-related surgical interventions, this may suggest that some of these excess admissions are for orthopaedic surgery, for which the stay is generally short. Our analysis of surgical interventions was limited by our short follow-up window, but we noted around 800 post-index OA-related procedures in each of the OA pain cohorts. Consistent with treatment guidelines in the UK, this suggests that OA-related surgery is generally reserved for patients in severe chronic pain that is refractory to other treatments [40]. This is reflected in our findings, where a higher proportion of patients with severe OA pain had each type of surgical intervention over the 24 months post-index than in the moderate to severe OA pain cohort. In general, hospitals are encouraged to have short patient stays through the UK reimbursement system. Length of stay for joint replacement surgeries has been declining and was around 5 days for a primary total knee replacement in 2014 [41, 42]. Treatment for patients with OA might also emphasise physical movement, which would also encourage brief inpatient stays. Despite surgical interventions being a likely cause of the shorter stay for patients with OA pain than for matched controls, our findings also showed other types of inpatient stay (non-elective and day cases) to have shorter mean lengths. Interestingly, the recent CPRD study (mentioned above) found a longer average inpatient stay for patients with moderate to severe OA compared with controls [27]. Therefore, additional factors specific to the dataset or clinical practice in Salford are likely to be driving these findings.
As expected, we found patients with moderate to severe or severe OA pain to have a higher utilisation of prescription analgesic drugs than patients without OA. They also used a broader range of analgesics; the most commonly prescribed were paracetamol and strong opioids. The UK guidelines for the pharmacological treatment of OA at the time of this study recommended first-line use of paracetamol or topical NSAIDs. Other analgesics, including opioids, should only be considered if one or both drugs offer insufficient pain relief [40]. This is also consistent with international guidelines for OA treatment at the time of the study, which recommended that the use of opioids (particularly strong opioids) is reserved for the management of severe OA pain that has not responded sufficiently to other analgesics [43,44,45]. Our data include prescription analgesics only, and it is interesting to see that paracetamol (40% and 50% of the OA pain cohorts had at least one prescription) and oral NSAIDs (30% and 31%) were so widely prescribed for moderate to severe OA pain and severe OA pain, given that they are so easily and cheaply obtained over the counter. The National Health Service is looking to reduce the prescription of over-the-counter medicines in order to reduce costs [46]. Our findings on analgesic use are broadly consistent with those reported in the UK and internationally, with several studies showing trends over time for increasing paracetamol and opioid use and decreasing NSAID use in patients with OA [16, 25, 38, 47]. This perhaps occurs as they continue to search for an effective treatment.
Our study showed £2519 of direct healthcare costs for the year post-index in patients with moderate to severe OA pain, and £3389 for patients with severe OA pain. This was significantly higher than for patients in the control cohorts and consistent with our findings for higher HCRU and analgesic use. Many other studies have demonstrated the high cost of OA to healthcare systems, particularly for the management of patients with moderate to severe or severe pain [13, 15,16,17, 19, 22, 24, 27, 39, 48]. Our multivariable analysis showed that older age at index or the presence of gout, osteoporosis, type 2 diabetes, or coronary artery disease was associated with an increased cost of healthcare in all cohorts, but with generally higher proportional contributions in control cohorts than the OA pain cohorts. Overall, our analyses suggest that much of the additional cost of moderate to severe or severe OA pain might be related to inpatient stays, most likely for surgical interventions.
Limitations of this analysis include those common to the use of retrospective data. The SIR is limited to patients treated in Salford, UK, but it provides a rich source of healthcare data for this population. Although the representativeness of SIR data with respect to other regions of the UK is unproven, it is likely to be at least broadly representative of other urban populations in the North West. Limitations for the SIR include that it is missing sexual and mental health data and out-of-area hospital data (mainly cardiac surgery). Specific to our analysis, the lack of OA pain scoring made defining cohorts of patients with chronic OA pain more complex. The definitions used were clinically realistic but complex, and HCRU cannot be definitively linked to chronic pain caused by OA. Surgeries are an important cost for patients with OA, and our 2-year follow-up limited the ability to evaluate the impact of OA-related surgical procedures.
Conclusions
Patients from the population of Salford, UK, with moderate to severe OA pain had significantly higher HCRU of almost all types and incurred almost double the annual direct healthcare costs compared with matched controls without OA. In general, HCRU and costs were even higher in the subset of patients with severe chronic OA pain. Although HCRU and costs are only two facets of the personal and social implications of OA pain, these findings demonstrate the significant local burden of moderate to severe and severe OA pain in Salford, UK, which may also be indicative of its burden in the wider UK. A better understanding of the burden of OA pain at both local and national levels could help healthcare systems to better meet the specific needs of patients.
References
Fayaz A, Croft P, Langford RM, Donaldson LJ, Jones GT. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. 2016;6(6):e010364. https://doi.org/10.1136/bmjopen-2015-010364.
The Economist Intelligence Unit, Sayburn S. The unrecognised burden of osteoarthritis: unmet needs in Europe. 2021. https://cdn.vev.design/private/BCwBc9ZFZyVz8yQQKr9VeLxSnjf1/d6Jx2OYBUF_Unmet%20needs%20in%20Europe_EIU%20Briefing%20Paper_Pfizer.pdf.pdf. Accessed 18 Oct 2021.
Belsey J. Primary care workload in the management of chronic pain. A retrospective cohort study using a GP database to identify resource implications for UK primary care. J Med Econ. 2002;5(1–4):39–50. https://doi.org/10.3111/200205039050.
Public Health England. Musculoskeletal health: 5 year prevention strategic framework. A statement of PHE, NHS England and Versus Arthritis' commitments to promote musculoskeletal health and to prevent musculoskeletal conditions. 2019 (last update 20 Jun 2019). https://www.gov.uk/government/publications/musculoskeletal-health-5-year-prevention-strategic-framework. Accessed 18 Oct 2021.
Public Health England. Chronic pain in adults 2017. An analysis of self-reported chronic pain from 2017 Health Survey for England data. 2020 (last update 4 Jun 2021). https://www.gov.uk/government/publications/chronic-pain-in-adults-2017. Accessed 18 Oct 2021.
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99. https://doi.org/10.1093/bmb/lds038.
Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil. 2013;21(9):1145–53. https://doi.org/10.1016/j.joca.2013.03.018.
Elliott AM, Smith BH, Penny KI, Cairns Smith W, Alastair CW. The epidemiology of chronic pain in the community. Lancet. 1999;354(9186):1248–52. https://doi.org/10.1016/S0140-6736(99)03057-3.
Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–59. https://doi.org/10.1016/S0140-6736(17)32154-2.
Department of Health. The Musculoskeletal Services Framework. A joint responsibility: doing it differently. 2006 (last update 6 Jul 2006). https://webarchive.nationalarchives.gov.uk/20130124073659/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4138412.pdf. Accessed 18 Oct 2021.
Sadosky AB, Bushmakin AG, Cappelleri JC, Lionberger DR. Relationship between patient-reported disease severity in osteoarthritis and self-reported pain, function and work productivity. Arthritis Res Ther. 2010;12(4):R162. https://doi.org/10.1186/ar3121.
Dibonaventura MD, Gupta S, McDonald M, Sadosky A, Pettitt D, Silverman S. Impact of self-rated osteoarthritis severity in an employed population: cross-sectional analysis of data from the National Health and Wellness Survey. Health Qual Life Outcomes. 2012;10:30. https://doi.org/10.1186/1477-7525-10-30.
Wei W, Gandhi K, Blauer-Peterson C, Johnson J. Impact of pain severity and opioid use on health care resource utilization and costs among patients with knee and hip osteoarthritis. J Manag Care Spec Pharm. 2019;25(9):957–65. https://doi.org/10.18553/jmcp.2019.25.9.957.
Jackson J, Iyer R, Mellor J, Wei W. The burden of pain associated with osteoarthritis in the hip or knee from the patient’s perspective: a multinational cross-sectional study. Adv Ther. 2020;37(9):3985–99. https://doi.org/10.1007/s12325-020-01445-4.
Nalamachu S, Robinson RL, Viktrup L, et al. Pain severity and healthcare resource utilization in patients with osteoarthritis in the United States. Postgrad Med. 2021;133(1):10–9. https://doi.org/10.1080/00325481.2020.1841988.
Nalamachu SR, Robinson RL, Viktrup L, et al. Multimodal treatment patterns for osteoarthritis and their relationship to patient-reported pain severity: a cross-sectional survey in the United States. J Pain Res. 2020;13:3415–25. https://doi.org/10.2147/jpr.S285124.
Conaghan PG, Doane MJ, Jaffe DH, et al. Are pain severity and current pharmacotherapies associated with quality of life, work productivity, and healthcare utilisation for people with osteoarthritis in five large European countries? Clin Exp Rheumatol. 2021;39(4):819–28.
Colombo GL, Heiman F, Peduto I. Utilization of healthcare resources in osteoarthritis: a cost of illness analysis based on real-world data in Italy. Ther Clin Risk Manag. 2021;17:345–56. https://doi.org/10.2147/tcrm.S301005.
Schild M, Müller U, von Schenck U, Prieur S, Miller R. The burden of chronic pain for patients with osteoarthritis in Germany: a retrospective cohort study of claims data. BMC Musculoskelet Disord. 2021;22(1):317. https://doi.org/10.1186/s12891-021-04180-1.
Sicras-Mainar A, Tornero-Tornero C, Vargas-Negrín F, Lizarraga I, Rejas-Gutierrez J. Health outcomes and costs in patients with osteoarthritis and chronic pain treated with opioids in Spain: the OPIOIDS real-world study. Ther Adv Musculoskelet Dis. 2020;12:1759720x20942000. https://doi.org/10.1177/1759720x20942000.
Zhao X, Shah D, Gandhi K, et al. The association of pain interference and opioid use with healthcare utilization and costs, and wage loss among adults with osteoarthritis in the United States. J Med Econ. 2019;22(11):1192–201. https://doi.org/10.1080/13696998.2019.1658590.
Sicras-Mainar A, Rejas-Gutierrez J, Vargas-Negrín F, Tornero-Tornero JC, Sicras-Navarro A, Lizarraga I. Disease burden and costs in moderate-to-severe chronic osteoarthritis pain refractory to standard of care: ancillary analysis of the OPIOIDS real-world study. Rheumatol Ther. 2021;8(1):303–26. https://doi.org/10.1007/s40744-020-00271-y.
Silverman S, Rice JB, White AG, et al. Clinical and economic burden of prescribing tramadol and other opioids for patients with osteoarthritis in a commercially-insured population in the United States. Pain. 2021. https://doi.org/10.1097/j.pain.0000000000002300.
Chen A, Gupte C, Akhtar K, Smith P, Cobb J. The global economic cost of osteoarthritis: how the UK compares. Arthritis. 2012;2012:698709. https://doi.org/10.1155/2012/698709.
Kingsbury SR, Gross HJ, Isherwood G, Conaghan PG. Osteoarthritis in Europe: impact on health status, work productivity and use of pharmacotherapies in five European countries. Rheumatology (Oxford). 2014;53(5):937–47. https://doi.org/10.1093/rheumatology/ket463.
Oxford Economics. The economic costs of arthritis for the UK economy. 2010 (last update Mar 2010). https://www.oxfordeconomics.com/my-oxford/projects/128882. Accessed 18 Oct 2021.
Lohan C, Stevenson H, Coates G, et al. Quantifying healthcare resource utilisation for the management of moderate-to-severe chronic pain among patients with osteoarthritis in England: a retrospective analysis of linked primary and secondary care data. Osteoarthr Cartil. 2021;29:S383. https://doi.org/10.1016/j.joca.2021.02.498.
Public Health England. Musculoskeletal conditions. 2020. https://fingertips.phe.org.uk/profile/msk/data. Accessed 18 Oct 2021.
Steel N, Ford JA, Newton JN, et al. Changes in health in the countries of the UK and 150 English Local Authority areas 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10158):1647–61. https://doi.org/10.1016/S0140-6736(18)32207-4.
Yu D, Jordan KP, Bedson J, et al. Population trends in the incidence and initial management of osteoarthritis: age-period-cohort analysis of the Clinical Practice Research Datalink, 1992–2013. Rheumatology (Oxford). 2017;56(11):1902–17. https://doi.org/10.1093/rheumatology/kex270.
Elkhenini HF, Davis KJ, Stein ND, et al. Using an electronic medical record (EMR) to conduct clinical trials: Salford Lung Study feasibility. BMC Med Inform Decis Mak. 2015;15(1):8. https://doi.org/10.1186/s12911-015-0132-z.
New JP, Leather D, Bakerly ND, McCrae J, Gibson JM. Putting patients in control of data from electronic health records. BMJ. 2018;360: j5554. https://doi.org/10.1136/bmj.j5554.
NHS Salford Clinical Commissioning Group. Salford Integrated Record: sharing patient information locally. 2017. https://www.arc-gm.nihr.ac.uk/media/wpweb/Salford-Integrated-Record-Booklet.pdf. Accessed 18 Oct 2021.
Ministry of Housing Communities and Local Government. National Statistics. English indices of deprivation 2019. 2019. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019. Accessed 18 Oct 2021.
Williams R, Jenkins DA, Ashcroft DM, et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. Lancet Public Health. 2020;5(10):e543–50. https://doi.org/10.1016/S2468-2667(20)30201-2.
Akbarov A, Kontopantelis E, Sperrin M, et al. Primary care medication safety surveillance with integrated primary and secondary care electronic health records: a cross-sectional study. Drug Saf. 2015;38(7):671–82. https://doi.org/10.1007/s40264-015-0304-x.
Tan V, Jinks C, Chew-Graham C, Healey EL, Mallen C. The triple whammy anxiety depression and osteoarthritis in long-term conditions. BMC Fam Pract. 2015;16(1):163. https://doi.org/10.1186/s12875-015-0346-2.
Zheng S, Tu L, Cicuttini F, et al. Depression in patients with knee osteoarthritis: risk factors and associations with joint symptoms. BMC Musculoskelet Disord. 2021;22(1):40. https://doi.org/10.1186/s12891-020-03875-1.
Conaghan PG, Abraham L, Graham-Clarke P, et al. FRI0397 The impact of osteoarthritis disease severity on healthcare resource use: analysis of real-world European data. Ann Rheum Dis. 2020;79(suppl 1):796–7. https://doi.org/10.1136/annrheumdis-2020-eular.5513.
National Institute for Health and Care Excellence. Osteoarthritis: care and management: clinical guideline [CG177]. 2014 (last update 11 Dec 2020). https://www.nice.org.uk/guidance/cg177. Accessed 18 Oct 2021.
Burn E, Edwards CJ, Murray DW, et al. Trends and determinants of length of stay and hospital reimbursement following knee and hip replacement: evidence from linked primary care and NHS hospital records from 1997 to 2014. BMJ Open. 2018;8(1): e019146. https://doi.org/10.1136/bmjopen-2017-019146.
National Institute for Health and Care Excellence. Joint replacement (primary): hip, knee and shoulder. NICE guideline [NG157]. 2020 (last update 4 Jun 2020). https://www.nice.org.uk/guidance/ng157. Accessed 18 Oct 2021.
Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008;16(2):137–62. https://doi.org/10.1016/j.joca.2007.12.013.
McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil. 2014;22(3):363–88. https://doi.org/10.1016/j.joca.2014.01.003.
Jordan KM, Arden NK, Doherty M, et al. EULAR recommendations 2003: an evidence based approach to the management of knee osteoarthritis. Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62(12):1145–55. https://doi.org/10.1136/ard.2003.011742.
National Health Service. Prescription curbs to free up hundreds of millions of pounds for frontline care. 2017 (last update 30 Nov 2017). https://www.england.nhs.uk/2017/11/prescription-curbs-to-free-up-hundreds-of-millions-of-pounds-for-frontline-care/. Accessed 18 Oct 2021.
Kingsbury SR, Hensor EM, Walsh CA, Hochberg MC, Conaghan PG. How do people with knee osteoarthritis use osteoarthritis pain medications and does this change over time? Data from the Osteoarthritis Initiative. Arthritis Res Ther. 2013;15(5):R106. https://doi.org/10.1186/ar4286.
Rejas-Gutierrez J, Llopart-Carles N, García-López S, Darbà J. Disease burden on health care by pain severity and usual analgesic treatment in patients with symptomatic osteoarthritis: a Spanish nationwide health survey. Expert Rev Pharmacoecon Outcomes Res. 2020. https://doi.org/10.1080/14737167.2020.1807943.
Acknowledgements
Funding
This study was sponsored by Pfizer and Eli Lilly and Company. Pfizer and Eli Lilly and Company contributed to the study design; Pfizer contributed to the management and collection of data. In their role as authors, employees of Pfizer were involved in the interpretation of data, the preparation, review, and approval of the manuscript, and the decision to submit for publication, along with their co-authors. The study sponsors approved the manuscript from an intellectual property perspective but had no right to veto the publication. Pfizer and Eli Lilly and Company funded the Rapid Service Fee associated with this publication.
Medical Writing Assistance
Medical writing was provided by Jennifer Bodkin of Engage Scientific Solutions and was funded by Pfizer and Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the design of the study and the analysis and interpretation of the data. Norman Stein and Bozydar Wrona extracted the data. All authors participated in drafting and critically revising the manuscript, provided final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Prior Presentation
A portion of these data was presented as a poster at the World Congress on Osteoporosis, Osteoarthritis and Musculoskeletal Diseases in London, 26–29 August 2021.
Disclosures
Lucy Abraham, Kate Halsby, Birol Emir, and Hannah Stevenson are employees of and shareholders in Pfizer. Norman Stein and Bozydar Wrona are employees of NorthWest EHealth who were paid contractors to Pfizer and Eli Lilly and Company in connection with this study.
Compliance with Ethics Guidelines
The study protocol was examined by the SIR Review Board as part of the data extract request application process. No separate ethics committee review process was required. The study was conducted in accordance with all legal and regulatory requirements, as well as with scientific purpose, value, and rigor. It followed generally accepted research practices described in the Guidelines for Good Pharmacoepidemiology Practices, Good Practices for Outcomes Research, and the Declaration of Helsinki.
Data Availability
The datasets generated during and/or analysed during the current study are not publicly available but can be requested from the SIR.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Abraham, L., Halsby, K., Stein, N. et al. An Observational Retrospective Matched Cohort Study of Healthcare Resource Utilisation and Costs in UK Patients with Moderate to Severe Osteoarthritis Pain. Rheumatol Ther 9, 851–874 (2022). https://doi.org/10.1007/s40744-022-00431-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00431-2