Abstract
Older adults have a higher prevalence of chronic obstructive pulmonary disease (COPD), which will likely increase substantially in the coming decades owing to aging populations and increased long-term exposure to risk factors for this disease. COPD in older adults is characterized by low-grade chronic systemic inflammation, known as inflamm-aging. It contributes substantially to age-associated pulmonary changes that are clinically expressed by reduced lung function, poor health status, and limitations in activities of daily living. In addition, inflamm-aging has been associated with the onset of many comorbidities commonly encountered in COPD. Furthermore, physiologic changes that are often seen with aging can influence the optimal treatment of older patients with COPD. Therefore, variables such as pharmacokinetics, pharmacodynamics, polypharmacy, comorbidities, adverse drug responses, drug interactions, method of administration, and social and economic issues that impact nutrition and adherence to therapy must be carefully evaluated when prescribing medication to these patients because each of them alone or together may affect the outcome of treatment. Current COPD medications focus mainly on alleviating COPD-related symptoms, so alternative treatment approaches that target the disease progression are being investigated. Considering the importance of inflamm-aging, new anti-inflammatory molecules are being evaluated, focusing on inhibiting the recruitment and activation of inflammatory cells, blocking mediators of inflammation thought to be important in the recruitment or activation of these inflammatory cells or released by these cells. Potential therapies that may slow the aging processes by acting on cellular senescence, blocking the processes that cause it (senostatics), eliminating senescent cells (senolytics), or targeting the ongoing oxidative stress seen with aging need to be evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic obstructive pulmonary disease is a disease of premature aging of the lung but it is more prevalent in older individuals and is often associated with other comorbidities. |
Managing chronic obstructive pulmonary disease in older adults is challenging because of the anatomical, physiological, and psychological changes peculiar to aging and the ongoing systemic inflammation. |
Changes in cognitive function and motor skills as well as underlying comorbid conditions impact the choice and response to the different medications available for chronic obstructive pulmonary disease. |
Evaluation of novel pharmacological agents capable of controlling inflamm-aging and slowing cellular senescence in this population is needed. |
1 Introduction
In healthy people, lung maturation and function peak at the age of 25 years, then stabilize and exhibit minimal variance until the age of 35 years, when it begins to decline [1]. Even in the absence of disease, older age can decrease pulmonary physiological performance. With aging, there are significant changes in lung cellular composition, with substantial anatomical, physiological, and psychological changes [2]. Lungs experience a reduction in their function [3] and poor regeneration of their tissue [4]. There is an increase in average alveolus size and a decrease in alveolus flexibility, which reduces air exchange efficiency and susceptibility to alveolar damage during infections [1].
There is a growing understanding of the intricate molecular mechanisms involved in aging and how this process is accelerated in chronic disorders [5]. Genomic instability, telomere shortening, diminished proteostasis (autophagy), mitochondrial dysfunction, faulty nutrition sensing, epigenetic alterations, stem cell depletion, and cellular senescence are all markers of aging [6]. Cellular senescence is a cell-cycle arrest condition in which cells experience phenotypical alterations that result in the pathology of many age-related disorders.
Senescent cells secrete numerous cytokines, chemokines, growth factors, and proteases collectively known as the senescence-associated secretory phenotype (SASP), which act as signaling molecules [7]. Persistent cellular senescence and an excessive SASP when combined with a dysfunctional immune system induce disruption of normal tissue microenvironments, and chronic low-grade inflammation, known as inflamm-aging and caused by an imbalance of inflammatory and anti-inflammatory networks, emerges [8].
Inflammation is a critical factor in the etiology of chronic obstructive pulmonary disease (COPD) and is linked to disease progression [4]. Early senescence of lung resident cells has been reported to affect the pathogenesis of COPD, which is now considered a disease of early aging [9]. However, the role of age-related changes in accelerating COPD pathogenesis remains unknown, while there is no doubt that older adults have a higher prevalence of the disease [10].
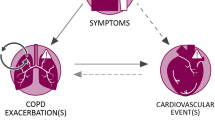
It is unclear whether age-associated lung changes predispose to COPD development [11]. However, they do contribute to poor health status and limitations in activities of daily living [12]. Furthermore, age-associated lung changes are associated with the onset of many comorbidities, such as cardiovascular, neurological, psychiatric, and gastrointestinal diseases and/or muscle wasting and osteoporosis, which are very common in COPD [13], probably linked by a common mechanism related to inflamm-aging [14]. When compared with those without COPD, older individuals with COPD showed a higher probability of coexisting geriatric syndromes, which could also be multiple [15]. Functional impairment, urine incontinence, malnutrition, cognitive impairment, and frailty were shown to be more prevalent in patients with COPD [15]. They worsen health status and increase morbidity and medication nonadherence and also the risk of admission to acute care units and mortality in older adults with COPD [16, 17]. Furthermore, tissue microenvironments and chronic low-grade inflammation may increase susceptibility to respiratory infection mainly in elderly patients [18].
Understanding why age increases the risk of COPD is still somewhat lacking [17]. It is widely accepted, however, that the older the patient, the more therapeutic aspects that need to be addressed to treat him/her most effectively [19]. Over the past two decades, as the population ages worldwide, the issue of more appropriately treating elderly patients with COPD has become an increasingly perceived need. Although reliable data to elaborate specific recommendations are still lacking, the accumulating evidence is leading to better therapeutic management of these patients.
The aim of this narrative review is to describe the challenges to be faced when pharmacologically treating older adults with COPD, but also the new opportunities that are gradually emerging even though many are not yet approved for the treatment of these patients.
2 The Pharmacological Treatment of COPD in Older Adults
The pharmacological treatment of COPD in older adults is a hot issue [19]. Unfortunately, no guidelines or strategies for treating COPD report age-specific recommendations for this population. Therefore, the same treatment algorithms indicated for patients with COPD also apply to elderly patients. However, there are some general considerations related to aging and its influence on the performance of medications traditionally used to treat COPD that should be considered when prescribing for older patients (Table 1). It is indeed possible that older patients’ responses to COPD medications do not fully reflect those seen in adult populations.
The significant anatomical, physiological, and psychological changes peculiar to aging can influence the optimal treatment of patients with COPD [19]. Because of diminished metabolism despite therapeutic levels [20] and an overall decline in defensive organ functioning [21], older patients with COPD may be more susceptible to drug-induced adverse events. In addition, they are often at an increased risk of drug–drug interactions [22] because they are often taking multiple medications for comorbid conditions.
Therefore, pharmacokinetics, pharmacodynamics, polypharmacy, comorbidities, adverse drug responses, drug interactions, the delivery method, and social and economic issues that impact nutrition and adherence to therapy must all be carefully assessed when prescribing for elderly patients [19]. The results may be influenced by any one of these variables.
2.1 Pharmacokinetics
Bronchodilators and inhaled corticosteroids (ICSs) are the mainstay therapy for COPD [23]. However, the evidence on which guidelines and strategies are determined is mainly based on the results of well-designed randomized controlled trials “in the population for which the recommendation is made without any important limitations” [23].
However, evidence on key therapeutic aspects in older patients with COPD is still lacking because pivotal randomized controlled trials have important limitations related to selection criteria [24]. In general, older patients are less likely to be enrolled in clinical trials because their comorbidities are usually among the most frequent exclusion criteria. Furthermore, only a few studies have specifically examined how aging affects the pharmacokinetics and pharmacodynamics of inhaled bronchodilators [24]. Regrettably, there are no studies on age-related changes in the pharmacokinetics of ICSs [25].
The pharmacokinetics of drugs, including inhaled drugs, may be changed in aged people because of renal and hepatic insufficiency, weight loss, increased body fat, decreased body water, and the impact of aging on absorption [26]. In addition, aging affects the pharmacokinetics of inhaled drugs because of the ongoing decline in respiratory function [26]. An example of the importance of the pharmacokinetics of bronchodilators in elderly patients is the demonstration that when the effect of aging was investigated on the pharmacokinetics of tiotropium bromide administered routinely via HandiHaler®, the area under the concentration–time curve in older patients was 43% higher than that in young patients [24]. Renal clearance values in young and old patients were 326 and 163 mL/min, respectively. The area under the concentration–time curve was likely higher in older patients because of reduced renal function. Another example of the importance of the pharmacokinetics of bronchodilators in older adults comes from theophylline, which, although no longer recommended as a bronchodilator in algorithms for treating COPD, is still used in low-income countries. Compared with young individuals, theophylline metabolic clearance decreases by 15–30% in old nonsmokers and 16–20% in old smokers. These decreases are most likely related to a decrease in cytochrome P450 (CYP) activity, namely CYP1A2 [27].
2.2 Pharmacodynamics
It has been proposed that aging-related changes in lung mechanics, receptor populations, and nervous system regulation may be responsible for differences in bronchodilator effectiveness in older patients versus younger people [28] (Table 2). Various animal model studies showed no change or a decline in response to β-adrenoceptor (AR) stimulation with aging [29]. There is substantial evidence linking aging to a decrease in β2-AR affinity (or a lower fraction of high-affinity receptors), presumably because of receptor internalization in membrane-bound vesicles [30]. Abnormal post-receptor events may also cause impaired β-adrenergic action in elderly patients. A senescent rat lung displays lower β-AR agonist affinity and adenylate cyclase activity [31]. It is unclear if older people are less responsive to the bronchodilating effects of β2-AR agonists. In older participants, the response to a β2-AR agonist following methacholine-induced bronchoconstriction has been investigated, with inconsistent findings [32, 33]. However, and unexpectedly, it has been shown that indacaterol, which is a once-daily β2-AR agonist, is effective in improving forced expiratory volume in 1 second (FEV1) across all age groups (< 65, ≥ 65, and ≥ 75 years of age). In contrast, formoterol, which is a twice-daily β2-AR agonist, is more effective in patients with COPD younger than 65 years of age [34].
The response to muscarinic acetylcholine receptor (mAChR) antagonists following methacholine-induced bronchoconstriction does not appear to change with age [35]. However, smaller improvements in lung function were observed in patients with COPD aged 80 years and older receiving tiotropium [36]. Nevertheless, the higher odds of FEV1 response to umeclidinium compared with placebo, with its improvement from clinically significant baseline values (≥ 100 mL) observed in a subgroup of patients with COPD aged ≥ 65 years compared with the subgroup aged < 65 years, suggest that older patients may be more responsive to mAChR antagonist monotherapy than younger patients [37].
It has been suggested that the number and functional responsiveness of lung M2 mAChRs diminish during the aging process in humans [38]. Still, nothing is known regarding possible age-dependent modifications in human mAChRs. M2 mAChRs usually inhibit the release of acetylcholine from parasympathetic neurons. As a result, the depletion of M2 mAChRs leads to enhanced acetylcholine release, followed by an increase in vagal tone [38]. It has been proposed that elderly patients (aged > 60 years) respond better to mAChR antagonists than younger patients, who benefit more from β2-AR agonists [39]. If this is true, older patients may require higher dosages of β2-AR agonists than mAChR antagonists to achieve a maximum bronchodilator response.
However, dual bronchodilation with a long-acting β2-AR agonist (LABA) and a long-acting mAChR antagonist (LAMA), which is now recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy as the initial treatment in the dyspneic patient [19] and by the American Thoracic Society for treating patients with COPD who complain of dyspnea or exercise intolerance [40], is effective across all age groups (< 65, ≥ 65, and ≥ 75 years) [41]. The bronchodilator effect is most pronounced in subjects aged 40 to < 65 years, while it is smaller, with largely overlapping 95% confidence intervals, in subjects aged ≥ 75 years [42]. The difference in FEV1 response between dual bronchodilation and a LAMA is generally less pronounced in subjects aged ≥ 75 years [41], and the proportion of patients responding with improved trough FEV1 ≥ 100 mL compared with LAMAs seems to be lower in older patients (≥ 75 years of age) [41].
Current recommendations for treating COPD include adding an ICS to dual bronchodilation if the patient has frequent exacerbations or complains of dyspnea or exercise intolerance despite dual bronchodilation with LABAs/LAMAs [23, 40]. Experimental studies have suggested that the response to corticosteroids generally declines towards older age. For example, changes in the responsiveness of dog leukocytes to corticosteroids occur during the aging process [43]. Furthermore, changes in glucocorticoid receptor activation have been found in aging rats [44]. In humans, the sensitivity of peripheral blood mononuclear cells to dexamethasone declines with age [45], although the precise mechanism underlying changes in corticosteroid sensitivity throughout aging has yet to be determined. This decreased sensitivity could lead to increasing the dose of corticosteroids in elderly patients. However, corticosteroid doses that appear safe in younger people may place older patients at risk of infection [46]. When using corticosteroids to treat older individuals, cell-mediated immunity factors, including a decrease in the fractional population of naïve T cells and a reduction in the chemotactic response of polymorphonuclear neutrophil leukocytes and monocytes, are of concern [46].
According to an old study, ICS treatment can increase survival and minimize hospitalization in older patients with moderate-to-severe COPD beyond what standard pharmacological therapy can achieve [47]. There is documentation that long-term triple therapy with LABAs/LAMAs/ICSs significantly improves FEV1 from baseline compared with dual bronchodilation or LABAs/ICSs. This effect is linked with a lower rate of exacerbation of COPD when compared with LABA/LAMA therapy, regardless of age [48]. On the contrary, compared with ICS/LABA therapy, triple therapy is related to a lower risk of moderate/severe exacerbations, particularly in patients aged 65 years or more. Unsurprisingly, therefore, older adults are more likely to be prescribed triple therapy than other patients [49]. However, a large, retrospective, longitudinal, population analysis of people aged 66 years and older with physician-diagnosed COPD found that ICSs had no effect on the absolute or relative risk of hospitalization for COPD [50]. Patients above the age of 75 years and those who were weak and taking ICS were at a greater risk of hospitalization.
Concerning the other drugs recommended in the treatment of COPD [23], there is documentation that roflumilast, a phosphodiesterase 4 inhibitor to be used in patients with chronic bronchitis, severe to very severe COPD, and a history of exacerbations [19], reduces the frequency of exacerbations and improves lung function in patients aged 65 years or less and in those aged older than 65 years [51]. However, adverse events were found to occur more frequently in patients aged > 65 years. It must be mentioned that much preclinical evidence points to the function of phosphodiesterase 4 inhibitors in the restoration of aging-related changes generated in animal models by various pharmacological agents and in the overexpression of mutant versions of human amyloid precursor proteins and aging [52]. It has even been suggested that phosphodiesterase 4-related molecular pathways might be involved in both the biology of lung aging and the pathogenesis of COPD [53]. Azithromycin, a macrolide recommended to reduce the risk of COPD exacerbation, appears to be most effective in older patients (aged > 65 years), with a significant interaction between age and treatment effect on the risk of exacerbation [54]. However, no evidence exists that the pharmacodynamic response to azithromycin is modified by age.
2.3 Comorbidities
It has been reported that many patients with COPD have at least one comorbidity [13, 55]. In addition, with aging, patients with COPD comorbid conditions increase [56]. However, clinical practice guidelines for a specific disease do not usually address comorbidities in their recommendation. In its last version, the GOLD strategy recommends that comorbidities should be actively sought for and treated appropriately, which means that they should be managed per specific guidelines, irrespective of COPD [23]. Nevertheless, comorbidities can significantly influence the overall treatment of people with COPD. Drugs used to treat COPD may have a negative or, sometimes, even favorable impact on comorbidity, and vice versa, those used to treat comorbidity may aggravate COPD or influence it positively [57].
Long-acting β2-AR agonists induce an increase in heart rate and a worsening of arrhythmia, mainly in patients with COPD experiencing pre-existing cardiac arrhythmias and hypoxemia [58] and could increase the risk of heart failure (HF) [59]. An observational population-based study of 191,005 older adults with COPD aged 66 years or older in Canada comparing the cardiovascular risk associated with LAMA and LABA use discovered increased risks of hospitalization and emergency department visits for cardiovascular disease in new users of both medications [60]. Specifically, LABA use was associated with a 31% increase in cardiovascular events among older patients. However, in patients aged 50–85 years, β2-AR agonists reduced lung hyperinflation, with improvements in right cardiac chamber compliance indices and contractility [61]. Furthermore, a small prospective study conducted in patients with COPD aged ≥ 80 years showed that a LABA/LAMA combination had an acceptable cardiac profile and did not increase the short-term proarrhythmic risk in older individuals [62].
An increased risk of acute urinary retention with mAChR antagonists should be considered when treating older patients with evidence of benign prostatic hyperplasia [63]. Long-term treatment with ICS at daily doses greater than 1000 μg of beclomethasone equivalent for more than 4 years was correlated with a modest but substantial increase in the risk of hip and upper extremity fractures in a large population-based cohort of 191,622 elderly subjects (mean age 81 years) treated for chronic respiratory disease [64]. Nonetheless, the relationship between ICS use and bone fracture incidence in patients with stable COPD remains unclear [65]. For example, adding an ICS to dual bronchodilation conferred no increased risk of osteoporosis and fractures, even in those aged 75 years or older [37, 48].
β-Blockers, statins, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II type 1 receptor blockers, and anti-platelet agents are the drugs that are usually used to treat the different cardiovascular diseases, regardless of whether the patient also has COPD [57].
β-Blockers are a valuable alternative for patients with COPD with ischemic heart disease, hypertension, and/or particularly HF [57]. Despite the clinical and pharmacological rationale suggesting the use of β-blockers in most patients with HF, it was reported that in hospitalized older patients (median age 82.8 years) affected by HF and COPD, only 36.9% were receiving a β-blocker on admission. This percentage became 38.0% at discharge, and there were no other β-blocker users after discharge [66]. These percentages were significantly lower than those observed in patients affected by HF alone (51.3 and 51.7%, respectively). However, studies that have enrolled patients with COPD with concomitant cardiovascular disease and an average age of at least 65 years have shown that although non-cardioselective-selective β-blockers and high doses of cardio-selective β-blockers might lead to a diminished response to inhaled β2-AR agonists [67, 68], there is no risk when a β-blocker is added to a LAMA [69] or a dual bronchodilator [70].
A study, which used population-based administrative data and identified a cohort of patients with COPD and a mean age of 71.0 years, suggested that statins are associated with a significant reduction in all-cause and lung-related mortality among patients with COPD [71]. However, the STATUETTE cohort study found no association between statin use and the risk of COPD exacerbation or all-cause mortality, regardless of patient age [72].
An extensive retrospective analysis of older individuals (mean age was 74.0 years) hospitalized for a COPD exacerbation evaluated the potential mortality benefit of ACE inhibition [73]. When demographics, co-morbidities, and other medications were considered, the study found that ACE inhibitor or angiotensin II type 1 receptor blocker usage was substantially related to a reduced 90-day mortality after their COPD hospital presentation.
Platelet activation increases in patients with stable and COPD exacerbation [54]. In older male patients with COPD, the mean platelet volume was negatively correlated with the level of FEV1 and left-ventricular ejection fraction [74]. Thus, preventing the formation of platelet–monocyte aggregates may be a valuable strategy for reducing the development of a cardiovascular disease in patients with COPD [74]. The SPIROMICS study showed that aspirin users were significantly older than non-users, and daily aspirin use at baseline was associated with a lower incidence rate of COPD exacerbation, as well as less severe respiratory symptoms and a better quality of life at baseline [75].
In older patients with COPD with concomitant diabetes mellitus, larger corticosteroid doses are associated with an increased risk of diabetic complications [76]. Surprisingly, in a sample of aged (mean age 72 years) outpatients with COPD attending a university hospital, there was a slight association between ICS use and type 2 diabetes. Still, the combination of an ICS and a β2-AR agonist seemingly attenuated this association [77]. It has been observed that insulin therapy was a factor related to COPD and a reduced FEV1/FVC ratio in elderly individuals [78]. However, a comparison of a large group of patients with diabetes with an average age of about 70 years and treated with insulin, metformin, or sulfonylureas and a control group without diabetes and with an average age of about 48 years showed that the use of these drugs was not associated with incident COPD [79]. Recently, it has been suggested to use glucagon-like peptide-1 receptor agonists, such as liraglutide, dulaglutide, and exenatide, when there is a need to treat diabetes in an aged subject with COPD because they may modulate pulmonary function [80] and also induce anti-inflammatory actions and reduce the secretion of surfactants, which decreases the risk of exacerbations [81].
2.4 Polypharmacy and Drug Interactions
Polypharmacy is often required when treating COPD and comorbidities at the same time. However, clinicians should be cautious about polypharmacy for several reasons [82]. Because of aging-related metabolic changes and decreased drug clearance, older adults are at a higher risk of experiencing harmful drug responses [83]. Adverse drug responses can arise either through a direct effect on the lungs or the organ affected by the comorbidity or through a drug–drug interaction that increases the toxicity and decreases the therapeutic efficacy of the prescribed treatment for COPD or comorbidity [83]. This risk worsens because older adults take numerous medications and are particularly vulnerable to drug–drug interactions because of gradual physiological changes affecting the pharmacokinetics and pharmacodynamics [83].
Bronchodilators and corticosteroids have great potential for systemic drug interactions [84]. β-Agonists can interact with β-blockers, diuretics, and digitalis frequently used by elderly patients. Furthermore, salmeterol, a substrate of CYP3A4, should not be used with potent CYP3A4 inhibitors such as azithromycin because concurrent administration can lead to an increased risk of adverse cardiovascular effects. Muscarinic acetylcholine receptor antagonists may have additive anticholinergic effects when concurrently used with anticholinergic-containing medications, such as antidepressants (amitriptyline, paroxetine), agents for overactive bladder (darifenacin, fesoterodine, oxybutynin, solifenacin, tolterodine, trospium), anti-Parkinson agents (benztropine, trihexyphenidyl), antipsychotics (olanzapine, quetiapine, haloperidol), and cardiovascular agents (disopyramide), all of which are of wide use in old age, and this could be a concern for patients with narrow-angle glaucoma, prostatic hyperplasia, or bladder neck obstruction [84].
In any case, it was shown that using a LABA/LAMA combination, the rates of adverse events, including drug-related adverse events, were similar at all ages (< 65 years, ≥ 65 years, and ≥ 75 years) [41]. Additionally, ICSs are substrates of CYP3A4, and when used with potent CYP3A4 inhibitors, their metabolism is inhibited, and consequently, their systemic exposure increases [84].
2.5 The Choice of Inhaled Delivery Device
The subject’s age is critical for the rational choice of inhaler devices [85]. Numerous older adults have trouble using inhalers because of physical and cognitive changes, the prevalence of arthritis or joint discomfort, as well as neuromuscular diseases such as Parkinson’s disease or issues following a stroke [86]. Furthermore, older age, female sex, and short stature have been associated with reductions in peak inspiratory flow (PIF) regardless of COPD [87]. Weak respiratory muscles and/or the existence of intrinsic positive end-expiratory pressure, which prevents patients from achieving an appropriate PIF, are proposed as mechanisms to account for this limitation [87]. Therefore, the capacity of older adults to generate sufficient PIF across a dry powder inhaler (DPI) is impaired [86]. A significant negative correlation between age and PIF is independent of the degree of the disease. In any case, approximately one-third of patients with COPD, generally older and more likely female, have a low PIF at hospital discharge following a COPD exacerbation [88]. Furthermore, there is a real possibility that even a patient with mild COPD may fail to generate an adequate PIF when he/she exacerbates and is treated at home [89]. This is further complicated by the fact that some patients can generate sufficient PIF, but this is accompanied by such exertion and dyspnea that they cannot hold their breath for 5–10 s, which compromises adequate lung deposition.
There are also many elderly people who, because of limited dexterity or grip strength, may have difficulty activating a pressurized metered-dose inhaler (pMDI) device. Actually, up to 43% of DPI users and 75% of pMDI users among older patients used the wrong inhaler technique [90]. For this reason, spacers are often prescribed for elderly patients with dexterity and coordination problems [91].
In any case, older patients believe that the breath-actuated metered-dose inhaler is easier to use than the pMDI or DPI. Alternatively, they could consider nebulized medication, mainly if they are male individuals aged over 65 years [86]. Nebulizer distribution of the whole dosage across several breaths may be more efficient in elderly patients than DPI or pMDI delivery of the dose during a single breath, especially in those with severe COPD and debilitating dyspnea [92]. Furthermore, nebulizer treatment is not limited by the need to produce sufficient PIF, which prevents DPI from being used effectively in older patients with severe COPD [92]. No particular inhaling technique or hand strength is needed. As many nebulizers have facemasks, older adults and those who experience consciousness changes common in COPD can utilize them [93].
Therefore, when selecting a device for an older patient, it is vital to consider a variety of factors, including the drug formulation, the clinical setting, their ability to generate enough inspirational flow, their ability to handle the device appropriately, and, most importantly, how well the inhaler’s actuation is coordinated with their inspiratory effort [93]. Furthermore, consistent repeated instruction considerably and gradually reduces mistakes with all devices. Therefore, patients who are aged older than 70 years should get ongoing repeated instruction to minimize breathing errors such as inhalation speed and gargling mistakes [94].
2.6 Adherence to Therapy
Patients with COPD are poorly adherent to prescribed therapy because of the chronicity of the disease, multiple medications, and the time it takes to achieve symptom relief [95]. Poor adherence is prevalent in male individuals and in those aged older than 70 years [96]. It is also influenced by the number of comorbidities and using two or more inhalers [96]. Cognitive impairment, depression, cultural barriers (foreign caregiver, low education), the timing of therapy, and fear of adverse drug reactions are other risk factors for nonadherence in older patients [97].
Patients often do not realize that skipping doses worsens the disease [98]. They are also unsure about inhalation techniques, mainly when more than one inhaler has been prescribed. Another important aspect of nonadherence to therapy is forgetfulness [98]. This seems especially true for second doses in the middle of the day. Therapy costs are crucial for primary nonadherence, underdosing, increased dosages, and other problematic patterns. There are patients who, when doctors order them to discontinue one inhaler and prescribe another, continue to use both because they do not want to “waste” expensive drugs [98]. Others take smaller doses of medication than prescribed to reduce the cost of therapy.
Although further research is needed on the most effective approaches to optimize medication adherence in elderly patients with COPD, practical opportunities exist to intervene to support adherence to prescribed therapy. It is necessary to develop interventions that address adherence barriers specific to older patients (such as cognition, polypharmacy, and immobility), identify strategies for continuous inhaler technique support outside of the professional healthcare setting, and assess the impact of prescribing multiple types of inhalers on medication adherence, and that of elective inhaler use in older adults with COPD [99]. Smart inhalers connected to smartphones or tablets can offer accurate real-world data regarding a patient’s patterns of adherence and inhaler technique during routine use [93].
The involvement of a caregiver or family members can help to provide support to help ensure the delivery of effective care in older adults [100, 101]. Patients with a caregiver or someone to assist them in remembering, preparing, and purchasing medicine had positive adherence behavior in a study on the patient-related determinants of adherence to inhaled COPD treatments [102]. Adherence measures such as compensation and technology-mediated solutions have been shown to assist older adults in remembering to take their prescriptions [103]. To maintain or improve their medication adherence, older adults employ a variety of compensatory strategies, including daily routines, memories, associations, simplification, location, taking medication, if necessary, external help tools, visibility, printed medication lists, specific times, visual of compartments, mental awareness, repeating the instructions, education, and physical pain. Technology-based approaches that help the elderly manage their prescription adherence, such as electronic pillboxes, text message reminders, tablet/smartphone applications, and electronic reminders, are also beneficial.
3 Prospects for COPD Treatment in Older Adults
Alternative therapeutic approaches are required to assess the underlying processes that cause COPD and its progression, especially in older adults, as current COPD medications mainly focus on COPD-related symptoms.
3.1 Novel Anti-inflammatory Drugs
There are numerous attempts to develop medications that block the activation and recruitment of inflammatory cells in the lungs of patients with COPD, such as macrophages, neutrophils, and T lymphocytes, or that specifically target the inflammatory mediators that play a role in these processes or are released by these cells [104]. Developing new anti-inflammatory drugs is also crucial for controlling systemic inflammation, which could allow a better therapeutic impact on the progression of COPD comorbidities. Several new potential targets have recently been identified, and novel agents have been developed for these targets [104, 105]. Table 3 reports information on new classes of anti-inflammatory drugs that have already been tested in humans and are possible treatments for patients with COPD because their development has likely not been discontinued. In any case, there is no specific information about effects on elderly populations.
It is worth noting, however, that the risk of infection, prevalent in patients with COPD, makes the clinical development of new drugs that directly block the biological components of inflammation extremely difficult and slow. This risk is greater in older adults, in which advancing age is associated with a decline in the integrity of physical barriers and protection against pathogens, and age-related changes in the immune system are associated with increased susceptibility to infection [106]. Growing evidence is suggesting that dysfunction of the cystic fibrosis transmembrane conductance regulator (CFTR), an ion transporter that regulates the hydration and viscosity of mucous secretions in the airway, is related to the impaired bacterial phagocytosis and favors recurrent bacterial infections and airway inflammation [107]. Furthermore, an experimental study in mice has documented that reduced expression of CFTR contributes to airspace enlargement because of aging and in response to cigarette smoke [108]. Therefore, CFTR potentiation may lead to an overall improvement in lung health in patients with COPD. Ivacaftor, a potentiator of CFTR chloride channel function, augmented measures of CFTR function and clinical symptoms in patients with COPD and chronic bronchitis [109]. Icenticaftor, another CFTR potentiator, significantly increased FEV1 and reduced systemic inflammation, with a trend towards reduced sputum bacterial colonization in patients with moderate-to-severe COPD [110]. Furthermore, experimental research has shown that following acute treatment, roflumilast potentiated CFTR channels in cell culture, human tracheal sections, and animals, as well as restored smoke-induced CFTR dysfunction following acute and chronic administration [111, 112]. There is yet no information on a specific response to CFTR potentiators in elderly patients. However, the experimental documentation that CFTR-deficient mice develop emphysema-like alveolar remodeling with aging makes it interesting to test the role of these molecules in older patients with COPD.
In any case, although the outcomes of the novel medicines have been disappointing so far, significant evidence is starting to emerge that recommends using these molecules in particular subgroups of patients with COPD not necessarily related to old age [104, 105]. A strategy based on the use of an oral fixed-dose combination or polypill, which includes essential medications for COPD and its comorbidities, i.e., also anti-inflammatory molecules, has the potential to target both diseases by simplifying healthcare delivery, increasing cost effectiveness, increasing medication adherence, and supporting comprehensive prescribing of evidence-based therapies [113]. This is because COPD and its comorbidities must always be considered in an integrated manner. However, at present, there seems to be no interest in developing the polypill approach to COPD, despite its apparent usefulness in older adults.
3.2 Senostatics and Senolytics
Attempts are also being made to find opportunities to slow down the aging process. According to experimental studies, senescent cell removal might prolong life and prevent or postpone age-related functional decline [114]. Moreover, senescent cell eradication offers a possible therapeutic alternative for managing several chronic disorders, including COPD [115]. Reactive oxygen species inhibit phosphatase tensin homolog, resulting in activation of phosphoinositide-3-kinase and then mechanistic target of rapamycin, which is inhibited by adenosine monophosphate-activated kinase [116, 117]. Cellular senescence and mitochondrial malfunction come from mechanistic target of rapamycin activation, which activates ribosomal p70 S6 kinase and microRNA-34a and microRNA-570, which block sirtuin-1. This causes the production of mitochondrial reactive oxygen species. The senescence-associated secretory phenotype, which is produced by senescent cells, releases inflammatory proteins (SASP).
Many medications that may address cellular senescence are being developed considering this pathway [115,116,117]. N-acetylcysteine is an effective antioxidant candidate to reduce reactive oxygen species-induced senescence [118]. A recent randomized controlled trial has shown that supplementing glycine and n-acetylcysteine in older adults improves several aging-related symptoms, including glutathione deficiency, oxidative stress, mitochondrial impairment, mitophagy, inflammation, insulin resistance, endothelial dysfunction, physical function and strength, exercise capacity, waist circumference, systolic blood pressure, and multiple genomic alterations associated with aging and reduces stem-cell exhaustion and cellular senescence [119].
It is becoming possible to target cellular senescence by blocking the processes that cause it (senostatics) or by eliminating senescent cells (senolytics) [116, 117] (Table 4). Among potential senostatic molecules, there are mechanistic target of rapamycin inhibitors (rapamycin and everolimus), adenosine monophosphate-activated kinase activators (metformin) antagomirs of specific micro-RNAs, and sirtuin-activating compounds (resveratrol). Among potential senolytics, dasatinib, quercetin, and navitoclax, tyrosine kinase inhibitors with markedly high affinity for BCR/ABL kinase, appear promising molecules in models of aging. However, no appropriate clinical studies have been reported to date, a part of a first-in-human, open-label pilot study in patients with idiopathic pulmonary fibrosis in whom the impact of orally administered dasatinib and quercetin on circulating SASP factors were inconclusive, but correlations were observed between changes in function and changes in SASP-related matrix-remodeling proteins, microRNAs, and pro-inflammatory cytokines [120]. Interestingly, the administration of this combination was acceptable and feasible in the older participants in the study.
4 Conclusions
Chronic obstructive pulmonary disease is one of the most common chronic diseases in the world, which often has a progressive course that worsens with age. Pharmacotherapeutic decisions must be combined with careful assessment of age-related pharmacokinetic and pharmacodynamic changes, and polypharmacy to maximize treatment benefits and minimize adverse events and drug–drug or drug–disease interactions. It is also essential to pay attention to a proper inhalation technique, which is often inadequate in older adults. Monitoring the myriad of comorbidities that may complicate management is crucial as well. The involvement of caregivers or family members can help provide additional support to promote good care and adherence to treatment. Apart from the proper use of the currently approved treatments for COPD and its comorbidities, there is interest in developing therapies that can reduce oxidative stress during aging and slow down the aging process by acting on cellular senescence, blocking the processes that cause it (senostatics) or eliminating senescent cells (senolytics).
References
Bowdish DME. The aging lung: is lung health good health for older adults. Chest. 2019;155(2):391–400. https://doi.org/10.1016/j.chest.2018.09.003.
Xie C, Ya Likun MM, Luo QL, Dong JC. Role of cellular senescence in inflammatory lung diseases. Cytokine Growth Factor Rev. 2023;S1359–6101(23):00010–2. https://doi.org/10.1016/j.cytogfr.2023.02.001.
Mannino DM, Davis KJ. Lung function decline and outcomes in an elderly population. Thorax. 2006;61(6):472–7. https://doi.org/10.1136/thx.2005.052449.
Ito K, Barnes PJ. COPD as a disease of accelerated lung aging. Chest. 2009;135(1):173–80. https://doi.org/10.1378/chest.08-1419.
Barnes PJ, Baker J, Donnelly LE. Cellular senescence as a mechanism and target in chronic lung diseases. Am J Respir Crit Care Med. 2019;200(5):556–64. https://doi.org/10.1164/rccm.201810-1975TR.
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153(6):1194–217. https://doi.org/10.1016/j.cell.2013.05.039.
Campisi J. Cellular senescence and lung function during aging. Yin and Yang Ann Am Thorac Soc. 2016;13(Suppl 5):S402–6. https://doi.org/10.1513/AnnalsATS.201609-703AW.
Andina N, de Meuron L, Schnegg-Kaufmann AS, et al. Increased inflammasome activation is associated with aging and chronic myelomonocytic leukemia disease severity. J Immunol. 2023;210(5):580–9. https://doi.org/10.4049/jimmunol.2200412.
Divo MJ, Celli BR, Poblador-Plou B, et al. Chronic obstructive pulmonary disease (COPD) as a disease of early aging: evidence from the EpiChron Cohort. PLoS ONE. 2018;13(2): e0193143. https://doi.org/10.1371/journal.pone.0193143.
Safiri S, Carson-Chahhoud K, Noori M, et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990–2019: results from the Global Burden of Disease Study 2019. BMJ. 2022;378: e069679. https://doi.org/10.1136/bmj-2021-069679.
Bellia M, Benfante A, Menozzii M, et al. Validation of lung densitometry threshold at CT for the distinction between senile lung and emphysema in elderly subjects. Monaldi Arch Chest Dis. 2011;75(3):162–6. https://doi.org/10.4081/monaldi.2011.216.
Janson C, Marks G, Buist S, et al. The impact of COPD on health status: findings from the BOLD study. Eur Respir J. 2013;42(6):1472–83. https://doi.org/10.1183/09031936.00153712.
Cazzola M, Bettoncelli G, Sessa E, Cricelli C, Biscione G. Prevalence of comorbidities in patients with chronic obstructive pulmonary disease. Respiration. 2010;80(2):112–9. https://doi.org/10.1159/000281880.
Barnes PJ. Senescence in COPD and its comorbidities. Annu Rev Physiol. 2017;79:517–39. https://doi.org/10.1146/annurev-physiol-022516-034314.
Soni N, Banerjee J, Gunasekaran V, et al. Association of geriatric syndromes in older adults with chronic obstructive pulmonary disease. Aging Med (Milton). 2022;5(2):106–12. https://doi.org/10.1002/agm2.12208.
Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–57. https://doi.org/10.1183/09031936.00133805.
Budinger GRS, Kohanski RA, Gan W, et al. The intersection of aging biology and the pathobiology of lung diseases: a joint NHLBI/NIA workshop. J Gerontol A Biol Sci Med Sci. 2017;72(11):1492–500. https://doi.org/10.1093/gerona/glx090.
Yanagi S, Tsubouchi H, Miura A, Matsuo A, Matsumoto N, Nakazato M. The impacts of cellular senescence in elderly pneumonia and in age-related lung diseases that increase the risk of respiratory infections. Int J Mol Sci. 2017;18(3):503. https://doi.org/10.3390/ijms18030503.
Valente S, Pasciuto G, Bernabei R, Corbo GM. Do we need different treatments for very elderly COPD patients? Respiration. 2010;80(5):357–68. https://doi.org/10.1159/000320221.
Antonelli Incalzi R, Scarlata S, Pennazza G, Santonico M, Pedone C. Chronic obstructive pulmonary disease in the elderly. Eur J Intern Med. 2014;25(4):320–8. https://doi.org/10.1016/j.ejim.2013.10.001.
Li Y, Wang C, Peng M. Aging immune system and its correlation with liability to severe lung complications. Front Public Health. 2021;9: 735151. https://doi.org/10.3389/fpubh.2021.735151.
Hanania NA, Sharma G, Sharafkhaneh A. COPD in the elderly patient. Semin Respir Crit Care Med. 2010;31(5):596–606. https://doi.org/10.1055/s-0030-1265900.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2023 report. Available from: https://goldcopd.org/wp-content/uploads/2022/11/GOLD-2023-ver-1.0-14Nov2022_WMV.pdf. Accessed 26 Jan 2023.
Matera MG, Rinaldi B, Page C, Rogliani P, Cazzola M. Pharmacokinetic considerations concerning the use of bronchodilators in the treatment of chronic obstructive pulmonary disease. Expert Opin Drug Metab Toxicol. 2018;14(10):1101–11. https://doi.org/10.1080/17425255.2018.1530215.
Matera MG, Rinaldi B, Calzetta L, Rogliani P, Cazzola M. Pharmacokinetics and pharmacodynamics of inhaled corticosteroids for asthma treatment. Pulm Pharmacol Ther. 2019;58: 101828. https://doi.org/10.1016/j.pupt.2019.101828.
Wallin M, Tagami T, Chen L, Yang M, Chan HK. Pulmonary drug delivery to older people. Adv Drug Deliv Rev. 2018;135:50–61. https://doi.org/10.1016/j.addr.2017.11.010.
Ohnishi A, Kato M, Kojima J, Ushiama H, Yoneko M, Kawai H. Differential pharmacokinetics of theophylline in elderly patients. Drugs Aging. 2003;20(1):71–84. https://doi.org/10.2165/00002512-200320010-00005.
Bellia V, Battaglia S, Matera MG, Cazzola M. The use of bronchodilators in the treatment of airway obstruction in elderly patients. Pulm Pharmacol Ther. 2006;19(5):311–9. https://doi.org/10.1016/j.pupt.2005.08.004.
Santulli G, Iaccarino G. Pinpointing beta adrenergic receptor in ageing pathophysiology: victim or executioner? Evidence from crime scenes. Immun Ageing. 2013;10(1):10. https://doi.org/10.1186/1742-4933-10-10.
Scarpace PJ, Tumer N, Mader SL. Beta-adrenergic function in aging. Basic mechanisms and clinical implications. Drugs Aging. 1991;1(2):116–29. https://doi.org/10.2165/00002512-199101020-00004.
Scarpace PJ, Abrass IB. Decreased beta-adrenergic agonist affinity and adenylate cyclase activity in senescent rat lung. J Gerontol. 1983;38(2):143–7. https://doi.org/10.1093/geronj/38.2.143.
Parker AL. Aging does not affect beta-agonist responsiveness after methacholine-induced bronchoconstriction. J Am Geriatr Soc. 2004;52(3):388–92. https://doi.org/10.1111/j.1532-5415.2004.52110.x.
Connolly MJ, Crowley JJ, Charan NB, Nielson CP, Vestal RE. Impaired bronchodilator response to albuterol in healthy elderly men and women. Chest. 1995;108(2):401–6. https://doi.org/10.1378/chest.108.2.401.
Girodet PO, Jasnot JY, Le Gros V, Decuypère L, Cao W, Devouassoux G. Efficacy and safety of indacaterol in patients with chronic obstructive pulmonary disease aged over 65 years: a pooled analysis. Respir Med. 2017;128:92–101. https://doi.org/10.1016/j.rmed.2017.05.010.
Ullah MI, Newman GB, Saunders KB. Influence of age on response to ipratropium and salbutamol in asthma. Thorax. 1981;36(7):523–9. https://doi.org/10.1136/thx.36.7.523.
Satoh H, Kagohashi K, Ohara G, et al. Use of tiotropium in patients with COPD aged 80 years and older. Exp Ther Med. 2013;5(4):997–1000. https://doi.org/10.3892/etm.2013.956.
Hanania NA, Caveney S, Soule T, et al. Effect of age on efficacy and safety of fluticasone furoate/vilanterol (FF/VI), umeclidinium (UMEC), and UMEC + FF/VI in patients with chronic obstructive pulmonary disease: analyses of five randomized clinical trials. Int J Chron Obstruct Pulmon Dis. 2021;16:1925–38. https://doi.org/10.2147/COPD.S302864.
Cazzola M, Page CP, Calzetta L, Matera MG. Pharmacology and therapeutics of bronchodilators. Pharmacol Rev. 2012;64(3):450–4. https://doi.org/10.1124/pr.111.004580.
van Schayck CP, Folgering H, Harbers H, Maas KL, van Weel C. Effects of allergy and age on responses to salbutamol and ipratropium bromide in moderate asthma and chronic bronchitis. Thorax. 1991;46(5):355–9. https://doi.org/10.1136/thx.46.5.355.
Nici L, Mammen MJ, Charbek E, et al. Pharmacologic management of chronic obstructive pulmonary disease: an official American Thoracic Society clinical practice guideline. Am J Respir Crit Care Med. 2020;201(9):e56-69. https://doi.org/10.1164/rccm.202003-0625ST.
Ray R, Tombs L, Naya I, Compton C, Lipson DA, Boucot I. Efficacy and safety of the dual bronchodilator combination umeclidinium/vilanterol in COPD by age and airflow limitation severity: a pooled post hoc analysis of seven clinical trials. Pulm Pharmacol Ther. 2019;57: 101802. https://doi.org/10.1016/j.pupt.2019.101802.
Ferguson GT, Karpel JP, Clerisme-Beaty E, Grönke L, Voß F, Buhl R. Efficacy and safety of tiotropium + olodaterol maintenance treatment in patients with COPD in the TONADO® and OTEMTO® studies: a subgroup analysis by age. Int J Chron Obstruct Pulmon Dis. 2016;11:2701–10. https://doi.org/10.2147/COPD.S108758.
Pereira MB, Traverse MC, Barros DM, Bianchini A, Martínez PE. The effects of aging on leukocyte glucocorticoid receptor concentration and response to dexamethasone in dogs. Exp Gerontol. 2003;38(9):989–95. https://doi.org/10.1016/s0531-5565(03)00163-3.
Djordjevic-Markovic R, Radic O, Jelic V, et al. Glucocorticoid receptors in ageing rats. Exp Gerontol. 1999;34(8):971–82. https://doi.org/10.1016/s0531-5565(99)00067-4.
Bauer ME. Stress, glucocorticoids and ageing of the immune system. Stress. 2005;8(1):69–83. https://doi.org/10.1080/10253890500100240.
Bowie MW, Slattum PW. Pharmacodynamics in older adults: a review. Am J Geriatr Pharmacother. 2007;5(3):263–303. https://doi.org/10.1016/j.amjopharm.2007.10.001.
Sin DD, Tu JV. Inhaled corticosteroids and the risk of mortality and readmission in elderly patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164(4):580–4. https://doi.org/10.1164/ajrccm.164.4.2009033.
Hanania NA, Mannino DM, Criner GJ, et al. Effect of age on the efficacy and safety of once-daily single-inhaler triple-therapy fluticasone furoate/umeclidinium/vilanterol in patients with COPD: a post hoc analysis of the Informing the Pathway of COPD Treatment Trial. Chest. 2021;159(3):985–95. https://doi.org/10.1016/j.chest.2020.09.253.
Di Marco F, Santus P, Terraneo S, et al. Characteristics of newly diagnosed COPD patients treated with triple inhaled therapy by general practitioners: a real world Italian study. NPJ Prim Care Respir Med. 2017;27(1):51. https://doi.org/10.1038/s41533-017-0051-9.
Kendzerska T, Aaron SD, To T, et al. Effectiveness and safety of inhaled corticosteroids in older individuals with chronic obstructive pulmonary disease and/or asthma: a population study. Ann Am Thorac Soc. 2019;16(10):1252–62. https://doi.org/10.1513/AnnalsATS.201902-126OC.
Hanania NA, Dransfield MT, Goehring UM, Lakkis H, Rowe P. Efficacy of roflumilast in elderly patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2011;183:A3087. https://doi.org/10.1164/ajrccm-conference.2011.183.1_MeetingAbstracts.A3087.
Sugin LJS, Murugesan A, Bindu M, Sunil KN. Roflumilast: a potential drug for the treatment of cognitive impairment? Neurosci Lett. 2020;736: 135281. https://doi.org/10.1016/j.neulet.2020.135281.
Kang MJ. Recent advances in molecular basis of lung aging and its associated diseases. Tuberc Respir Dis (Seoul). 2020;83(2):107–15. https://doi.org/10.4046/trd.2020.0003.
Han MK, Tayob N, Murray S, et al. Predictors of chronic obstructive pulmonary disease exacerbation reduction in response to daily azithromycin therapy. Am J Respir Crit Care Med. 2014;189(12):1503–8. https://doi.org/10.1164/rccm.201402-0207OC.
Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099–107. https://doi.org/10.1378/chest.128.4.2099.
Ioakeim-Skoufa I, Clerencia-Sierra M, Moreno-Juste A, et al. Multimorbidity clusters in the oldest old: results from the EpiChron cohort. Int J Environ Res Public Health. 2022;19(16):10180. https://doi.org/10.3390/ijerph191610180.
Cazzola M, Calzetta L, Rinaldi B, et al. Management of chronic obstructive pulmonary disease in patients with cardiovascular diseases. Drugs. 2017;77(7):721–32. https://doi.org/10.1007/s40265-017-0731-3.
Cazzola M, Imperatore F, Salzillo A, et al. Cardiac effects of formoterol and salmeterol in patients suffering from COPD with preexisting cardiac arrhythmias and hypoxemia. Chest. 1998;114(2):411–5. https://doi.org/10.1378/chest.114.2.411.
Matera MG, Calzetta L, Cazzola M. β-Adrenoceptor modulation in chronic obstructive pulmonary disease: present and future perspectives. Drugs. 2013;73(15):1653–63. https://doi.org/10.1007/s40265-013-0120-5.
Gershon A, Croxford R, Calzavara A, et al. Cardiovascular safety of inhaled long-acting bronchodilators in individuals with chronic obstructive pulmonary disease. JAMA Intern Med. 2013;173(13):1175–85. https://doi.org/10.1001/jamainternmed.2013.1016.
Santus P, Radovanovic D, Di Marco S, et al. Effect of indacaterol on lung deflation improves cardiac performance in hyperinflated COPD patients: an interventional, randomized, double-blind clinical trial. Int J Chron Obstruct Pulmon Dis. 2015;10:1917–23. https://doi.org/10.2147/COPD.S91684.
Spannella F, Giulietti F, Cesari V, et al. Combination therapy of inhaled indacaterol/glycopyrronium for chronic obstructive pulmonary disease in the very elderly: is it safe? An electrocardiographic evaluation. Respiration. 2018;95(Suppl 1):22–9. https://doi.org/10.1159/000487182.
Stephenson A, Seitz D, Bell CM, et al. Inhaled anticholinergic drug therapy and the risk of acute urinary retention in chronic obstructive pulmonary disease: a population-based study. Arch Intern Med. 2011;171(10):914–20. https://doi.org/10.1001/archinternmed.2011.170.
Suissa S, Baltzan M, Kremer R, Ernst P. Inhaled and nasal corticosteroid use and the risk of fracture. Am J Respir Crit Care Med. 2004;169(1):83–8. https://doi.org/10.1164/rccm.200305-640OC.
Caramori G, Ruggeri P, Arpinelli F, Salvi L, Girbino G. Long-term use of inhaled glucocorticoids in patients with stable chronic obstructive pulmonary disease and risk of bone fractures: a narrative review of the literature. Int J Chron Obstruct Pulmon Dis. 2019;14:1085–97. https://doi.org/10.2147/COPD.S190215.
Arcoraci V, Squadrito F, Rottura M, et al. Beta-blocker use in older hospitalized patients affected by heart failure and chronic obstructive pulmonary disease: an Italian survey from the REPOSI register. Front Cardiovasc Med. 2022;9: 876693. https://doi.org/10.3389/fcvm.2022.876693.
Cazzola M, Matera MG, Ruggeri P, et al. Comparative effects of a two-week treatment with nebivolol and nifedipine in hypertensive patients suffering from COPD. Respiration. 2004;71(2):159–64. https://doi.org/10.1159/000076677.
Chang CL, Mills GD, McLachlan JD, Karalus NC, Hancox RJ. Cardio-selective and non-selective beta-blockers in chronic obstructive pulmonary disease: effects on bronchodilator response and exercise. Intern Med J. 2010;40(3):193–200. https://doi.org/10.1111/j.1445-5994.2009.01943.x.
Chapman KR, Wise RA, Scirica BM, et al. Long-acting antimuscarinic therapy in patients with chronic obstructive pulmonary disease receiving beta-blockers. Respir Res. 2021;22(1):272. https://doi.org/10.1186/s12931-021-01861-2.
Maltais F, Buhl R, Koch A, et al. β-Blockers in COPD: a cohort study from the TONADO research program. Chest. 2018;153(6):1315–25. https://doi.org/10.1016/j.chest.2018.01.008.
Raymakers AJN, Sadatsafavi M, Sin DD, De Vera MA, Lynd LD. The impact of statin drug use on all-cause mortality in patients with COPD: a population-based cohort study. Chest. 2017;152(3):486–93. https://doi.org/10.1016/j.chest.2017.02.002.
Damkjær M, Håkansson K, Kallemose T, Ulrik CS, Godtfredsen N. Statins in high-risk chronic obstructive pulmonary disease outpatients: no impact on time to first exacerbation and all-cause mortality: the STATUETTE cohort study. Int J Chron Obstruct Pulmon Dis. 2021;16:579–89. https://doi.org/10.2147/COPD.S296472.
Mortensen EM, Copeland LA, Pugh MJ, et al. Impact of statins and ACE inhibitors on mortality after COPD exacerbations. Respir Res. 2009;10(1):45. https://doi.org/10.1186/1465-9921-10-45.
Maclay JD, McAllister DA, Johnston S, et al. Increased platelet activation in patients with stable and acute exacerbation of COPD. Thorax. 2011;66(9):769–74. https://doi.org/10.1136/thx.2010.157529.
Fawzy A, Putcha N, Aaron CP, et al. Aspirin use and respiratory morbidity in COPD: a propensity score-matched analysis in subpopulations and intermediate outcome measures in COPD study. Chest. 2019;155(3):519–27. https://doi.org/10.1016/j.chest.2018.11.028.
Caughey GE, Preiss AK, Vitry AI, Gilbert AL, Roughead EE. Comorbid diabetes and COPD: impact of corticosteroid use on diabetes complications. Diabetes Care. 2013;36(10):3009–14. https://doi.org/10.2337/dc12-2197.
Rogliani P, Calzetta L, Segreti A, Barrile A, Cazzola M. Diabetes mellitus among outpatients with COPD attending a university hospital. Acta Diabetol. 2014;51:933–40. https://doi.org/10.1007/s00592-014-0584-0.
Ishii M, Yamaguchi Y, Hamaya H, Ogawa S, Imura M, Akishita M. Characteristics of factors for decreased lung function in elderly patients with type 2 diabetes. Sci Rep. 2019;9(1):20206. https://doi.org/10.1038/s41598-019-56759-3.
Rayner LH, McGovern AP, Sherlock J, et al. Type 2 diabetes: a protective factor for COPD? Prim Care Diabetes. 2018;12(5):438–44. https://doi.org/10.1016/j.pcd.2018.05.002.
Rogliani P, Matera MG, Calzetta L, et al. Long-term observational study on the impact of GLP-1R agonists on lung function in diabetic patients. Respir Med. 2019;154:86–92. https://doi.org/10.1016/j.rmed.2019.06.015.
Figat M, Kardas G, Kuna P, Panek MG. Beneficial influence of exendin-4 on specific organs and mechanisms favourable for the elderly with concomitant obstructive lung diseases. Brain Sci. 2022;12(8):1090. https://doi.org/10.3390/brainsci12081090.
Dagli RJ, Sharma A. Polypharmacy: a global risk factor for elderly people. J Int Oral Health. 2014;6(6):i–ii.
Zerah L, Henrard S, Wilting I, et al. Prevalence of drug–drug interactions in older people before and after hospital admission: analysis from the OPERAM trial. BMC Geriatr. 2021;21(1):571. https://doi.org/10.1186/s12877-021-02532-z.
Ajimura CM, Jagan N, Morrow LE, Malesker MA. Drug interactions with oral inhaled medications. J Pharm Technol. 2018;34(6):273–80. https://doi.org/10.1177/8755122518788809.
Barrons R, Pegram A, Borries A. Inhaler device selection: special considerations in elderly patients with chronic obstructive pulmonary disease. Am J Health Syst Pharm. 2011;68(13):1221–32. https://doi.org/10.2146/ajhp100452.
Cazzola M, Rogliani P. Inhaled medication: which device for which patient? ERS Monogr. 2015;69:213–23.
Duarte AG, Tung L, Zhang W, Hsu ES, Kuo YF, Sharma G. Spirometry measurement of peak inspiratory flow identifies suboptimal use of dry powder inhalers in ambulatory patients with COPD. Chronic Obstr Pulm Dis. 2019;6(3):246–55. https://doi.org/10.15326/jcopdf.6.3.2018.0163.
Sharma G, Mahler DA, Mayorga VM, Deering KL, Harshaw O, Ganapathy V. Prevalence of low peak inspiratory flow rate at discharge in patients hospitalized for COPD exacerbation. Chronic Obstr Pulm Dis. 2017;4(3):217–24. https://doi.org/10.15326/jcopdf.4.3.2017.0183.
Jarvis S, Ind PW, Shiner RJ. Inhaled therapy in elderly COPD patients; time for re-evaluation? Age Ageing. 2007;36(2):213–8. https://doi.org/10.1093/ageing/afl174.
Khassawneh BY, Al-Ali MK, Alzoubi KH, et al. Handling of inhaler devices in actual pulmonary practice: metered-dose inhaler versus dry powder inhalers. Respir Care. 2008;53(3):324–8.
Rogliani P, Calzetta L, Coppola A, et al. Optimizing drug delivery in COPD: the role of inhaler devices. Respir Med. 2017;124:6–14. https://doi.org/10.1016/j.rmed.2017.01.006.
Dhand R, Dolovich M, Chipps B, Myers TR, Restrepo R, Farrar JR. The role of nebulized therapy in the management of COPD: evidence and recommendations. COPD. 2012;9(1):58–72. https://doi.org/10.3109/15412555.2011.630047.
Cazzola M, Cavalli F, Usmani OS, Rogliani P. Advances in pulmonary drug delivery devices for the treatment of chronic obstructive pulmonary disease. Expert Opin Drug Deliv. 2020;17(5):635–46. https://doi.org/10.1080/17425247.2020.1739021.
Usami O. Improved inhaler handling after repeated inhalation guidance for elderly patients with bronchial asthma and chronic obstructive pulmonary disease. Medicine (Baltimore). 2022;101(35): e30238. https://doi.org/10.1097/MD.0000000000030238.
Toy EL, Beaulieu NU, McHale JM, et al. Treatment of COPD: relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med. 2011;105(3):435–41. https://doi.org/10.1016/j.rmed.2010.09.006.
Suh HS, Chang MS, Yu I, et al. Adherence to long-acting inhaler use for initial treatment and acute exacerbation of chronic obstructive pulmonary disease: a retrospective cohort study. J Pers Med. 2022;12(12):2073. https://doi.org/10.3390/jpm12122073.
Corsonello A, Scarlata S, Pedone C, et al. Treating COPD in older and oldest old patients. Curr Pharm Des. 2015;21(13):1672–89. https://doi.org/10.2174/1381612821666150130121229.
O’Toole J, Krishnan M, Riekert K, Eakin MN. Understanding barriers to and strategies for medication adherence in COPD: a qualitative study. BMC Pulm Med. 2022;22(1):98. https://doi.org/10.1186/s12890-022-01892-5.
Rogliani P, Ora J, Puxeddu E, Matera MG, Cazzola M. Adherence to COPD treatment: myth and reality. Respir Med. 2017;129:117–23. https://doi.org/10.1016/j.rmed.2017.06.007.
Nazir SA, Erbland ML. Chronic obstructive pulmonary disease: an update on diagnosis and management issues in older adults. Drugs Aging. 2009;26(10):813–31. https://doi.org/10.2165/11316760-000000000-00000.
Trivedi RB, Bryson CL, Udris E, Au DH. The influence of informal caregivers on adherence in COPD patients. Ann Behav Med. 2012;44(1):66–72. https://doi.org/10.1007/s12160-012-9355-8.
Duarte-de-Araújo A, Teixeira P, Hespanhol V, Correia-de-Sousa J. COPD: understanding patients’ adherence to inhaled medications. Int J Chron Obstruct Pulmon Dis. 2018;13:2767–73. https://doi.org/10.2147/COPD.S160982.
Pratiwi H, Kristina SA, Widayanti AW, Prabandari YS, Kusuma IY. A systematic review of compensation and technology-mediated strategies to maintain older adults’ medication adherence. Int J Environ Res Public Health. 2023;20(1):803. https://doi.org/10.3390/ijerph20010803.
Matera MG, Cazzola M, Page C. Prospects for COPD treatment. Curr Opin Pharmacol. 2021;56:74–84. https://doi.org/10.1016/j.coph.2020.11.003.
Matera MG, Calzetta L, Annibale R, Russo F, Cazzola M. Classes of drugs that target the cellular components of inflammation under clinical development for COPD. Expert Rev Clin Pharmacol. 2021;14(8):1015–27. https://doi.org/10.1080/17512433.2021.1925537.
Meiners S, Eickelberg O, Königshoff M. Hallmarks of the ageing lung. Eur Respir J. 2015;45(3):807–27. https://doi.org/10.1183/09031936.00186914.
Mall MA, Criner GJ, Miravitlles M, et al. Cystic fibrosis transmembrane conductance regulator in COPD: a role in respiratory epithelium and beyond. Eur Respir J. 2023;61(4):2201307. https://doi.org/10.1183/13993003.01307-2022.
Wellmerling JH, Chang SW, Kim E, et al. Reduced expression of the Ion channel CFTR contributes to airspace enlargement as a consequence of aging and in response to cigarette smoke in mice. Respir Res. 2019;20(1):200. https://doi.org/10.1186/s12931-019-1170-3.
Solomon GM, Hathorne H, Liu B, et al. Pilot evaluation of ivacaftor for chronic bronchitis. Lancet Respir Med. 2016;4(6):e32–3. https://doi.org/10.1016/S2213-2600(16)30047-9.
Rowe SM, Jones I, Dransfield MT, et al. Efficacy and safety of the CFTR potentiator Icenticaftor (QBW251) in COPD: results from a phase 2 randomized trial. Int J Chron Obstruct Pulmon Dis. 2020;15:2399–409.
Lambert JA, Raju SV, Tang LP, et al. Cystic fibrosis transmembrane conductance regulator activation by roflumilast contributes to therapeutic benefit in chronic bronchitis. Am J Respir Cell Mol Biol. 2014;50(3):549–58.
Raju SV, Rasmussen L, Sloane PA, Tang LP, Libby EF, Rowe SM. Roflumilast reverses CFTR-mediated ion transport dysfunction in cigarette smoke-exposed mice. Respir Res. 2017;18(1):173.
Castellano JM, Sanz G, Fernandez Ortiz A, Garrido E, Bansilal S, Fuster V. A polypill strategy to improve global secondary cardiovascular prevention: from concept to reality. J Am Coll Cardiol. 2014;64(6):613–21. https://doi.org/10.1016/j.jacc.2014.06.009.
Kirkland JL, Tchkonia T. Clinical strategies and animal models for developing senolytic agents. Exp Gerontol. 2015;68:19–25. https://doi.org/10.1016/j.exger.2014.10.012.
Cazzola M, Matera MG, Rogliani P, Calzetta L. Senolytic drugs in respiratory medicine: is it an appropriate therapeutic approach? Expert Opin Investig Drugs. 2018;27(7):573–81. https://doi.org/10.1080/13543784.2018.1492548.
Barnes PJ. Targeting cellular senescence as a new approach to chronic obstructive pulmonary disease therapy. Curr Opin Pharmacol. 2021;56:68–73. https://doi.org/10.1016/j.coph.2020.11.004.
Baker JR, Donnelly LE, Barnes PJ. Senotherapy: a new horizon for COPD therapy. Chest. 2020;158(2):562–70. https://doi.org/10.1016/j.chest.2020.01.027.
Al-Azab M, Safi M, Idiiatullina E, Al-Shaebi F, Zaky MY. Aging of mesenchymal stem cell: machinery, markers, and strategies of fighting. Cell Mol Biol Lett. 2022;27(1):69. https://doi.org/10.1186/s11658-022-00366-0.
Kumar P, Liu C, Suliburk J, et al. Supplementing glycine and N-acetylcysteine (GlyNAC) in older adults improves glutathione deficiency, oxidative stress, mitochondrial dysfunction, inflammation, physical function, and aging hallmarks: a randomized clinical trial. J Gerontol A Biol Sci Med Sci. 2023;78(1):75–89. https://doi.org/10.1093/gerona/glac135.
Justice JN, Nambiar AM, Tchkonia T, et al. Senolytics in idiopathic pulmonary fibrosis: results from a first-in-human, open-label, pilot study. EBioMedicine. 2019;40:554–63. https://doi.org/10.1016/j.ebiom.2018.12.052.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi di Roma Tor Vergata within the CRUI-CARE Agreement.
Conflict of interest
Mario Cazzola, Nicola A. Hanania, Mauro Maniscalco, and Maria Gabriella Matera have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
MC: Conceptualization, methodology, writing (original draft preparation). NAH: Conceptualization, writing (reviewing and editing). MM: Writing (reviewing and editing). MGM: conceptualization, methodology, writing (original draft preparation).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Matera, M.G., Hanania, N.A., Maniscalco, M. et al. Pharmacotherapies in Older Adults with COPD: Challenges and Opportunities. Drugs Aging 40, 605–619 (2023). https://doi.org/10.1007/s40266-023-01038-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01038-0