Abstract
Background
We investigated the effect of a 5-day low-dose ritonavir therapy, as it is used in the treatment of COVID-19 with nirmatrelvir/ritonavir, on the pharmacokinetics of three factor Xa inhibitors (FXaI). Concurrently, the time course of the activities of the cytochromes P450 (CYP) 3A4, 2C19, and 2D6 was assessed.
Methods
In an open-label, fixed sequence clinical trial, the effect and duration of a 5-day oral ritonavir (100 mg twice daily) treatment on the pharmacokinetics of three oral microdosed FXaI (rivaroxaban 25 µg, apixaban 25 µg, and edoxaban 50 µg) and microdosed probe drugs (midazolam 25 µg, yohimbine 50 µg, and omeprazole 100 µg) was evaluated in eight healthy volunteers. The plasma concentrations of all drugs were quantified using validated liquid chromatography–tandem mass spectrometry (LC-MS/MS) methods and pharmacokinetics were analysed using non-compartmental analyses.
Results
Ritonavir increased the exposure of apixaban, edoxaban, and rivaroxaban, but to a different extent the observed area under the plasma concentration–time curve (geometric mean ratio 1.29, 1.46, and 1.87, respectively). A strong CYP3A4 inhibition (geometric mean ratio > 10), a moderate CYP2C19 induction 2 days after ritonavir (0.64), and no alteration of CYP2D6 were observed. A CYP3A4 recovery half-life of 2.3 days was determined.
Conclusion
This trial with three microdosed FXaI suggests that at most the rivaroxaban dose should be reduced during short-term ritonavir, and only in patients receiving high maintenance doses. Thorough time series analyses demonstrated differential effects on three different drug-metabolising enzymes over time with immediate profound inhibition of CYP3A4 and only slow recovery after discontinuation.
Clinical Trial Registration
EudraCT number: 2021-006643-39.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The effect of short-term low-dose ritonavir on the pharmacokinetics of factor Xa inhibitors (FXaI) is not well studied and the time course of interaction with major cytochrome P450 (CYP) pathways has not been described in detail. |
We simultaneously quantified the effect of 5 days of ritonavir 100 mg twice daily on three microdosed oral FXaI and concurrently assessed the time course of CYP3A4, CYP2C19, and CYP2D6 activity during ritonavir and for 4 days after discontinuation. |
Of the three FXaI, only rivaroxaban exposure increased relevantly during ritonavir treatment while apixaban and edoxaban exposures were only mildly increased. |
Ritonavir inhibited CYP3A4 rapidly and profoundly and the recovery of its activity was delayed. CYP2C19 was mildly and transiently induced at the end of treatment, while CYP2D6 activity was unchanged throughout the observation period. |
1 Introduction
The COVID-19 pandemic affects people worldwide and can lead to hospitalization and death. Nirmatrelvir-ritonavir (Paxlovid®) has been available through an Emergency Use Authorization (EUA) since early 2022 and was approved by the US Food and Drug Administration (FDA) in May 2023 for the treatment of mild to moderate COVID-19 in adults at high risk for progression to severe COVID-19 and within 5 days of symptom onset. This therapy consists of a low dose (100 mg) of ritonavir taken orally every 12 h for 5 days, which inhibits the metabolism of nirmatrelvir, reducing its clearance (CL) and increasing its bioavailability [1]. This short-term use for only 5 days is new for ritonavir, as ritonavir-boosted treatments for HIV patients are chronic and therefore drug–drug interaction (DDI) studies usually examine the effects of long-term use. Ritonavir is a potent mechanism-based inhibitor of cytochrome P450 (CYP) 3A with inhibitory and time-dependent inductive effects on numerous other CYPs and drug transporters such as p-glycoprotein (P-gp), breast cancer resistance protein (BCRP), and organic anion-transporting polypeptides (OATP) [2,3,4,5,6,7]. Using a 300-mg twice-daily (bid) schedule, potent CYP3A inhibition of ritonavir over time was already demonstrated during 9 days of treatment [8].
Nirmatrelvir/ritonavir therapy is indicated for patients at high-risk for severe COVID-19 courses, who frequently take other drugs such as factor Xa inhibitors (FXaI). Infection with SARS-CoV-2 seems additionally associated with an increased risk of thrombotic events [9]. All three available FXaI are substrates of P-gp and BCRP but their clearance pathways differ, with edoxaban being mostly excreted unchanged [10], apixaban being metabolized mainly by CYP3A with a minor contribution from other CYP isozymes [11], and rivaroxaban being metabolized mainly by CYP2J2 and CYP3A [12,13,14]. Therefore, DDIs are known and expected for strong CYP3A and P-gp inhibitors and are associated with increased haemorrhagic risk [15, 16]. However, there are limited data on coadministration with ritonavir showing a 2.5-fold exposure increase in rivaroxaban in healthy volunteers after 6 days of high-dose (600 mg bid) ritonavir therapy [17], as well as case reports of increased plasma concentrations and/or bleeding risk of FXaI with concomitant ritonavir-boosted therapy [18,19,20,21,22,23]. The manufacturer does not recommend the use of nirmatrelvir/ritonavir with rivaroxaban, while there is no statement for apixaban and edoxaban [24].
Therefore, we aimed to assess the influence of shorter and much lower standard boosting doses of ritonavir, as recommended for COVID-19 treatment (100 mg ritonavir bid for 5 days), on the pharmacokinetics of FXaI to quantify the magnitude of these DDI. We administered FXaI microdoses, which are predictive of their therapeutic doses [25, 26], and evaluated all three FXaI simultaneously.
In the absence of mechanistic studies on the time course of the interaction of short-term ritonavir with other major CYPs, we also examined the effects on CYP2D6 and CYP2C19 activities over time. Therefore, the pharmacokinetics of the established microdosed CYP probe drugs midazolam [8], yohimbine [27], and omeprazole [28] were studied daily during ritonavir intake and for another 4 days after stopping ritonavir.
2 Methods
2.1 Trial Design
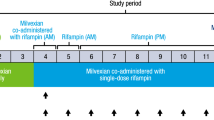
This phase I trial was conducted as a single-centre, open-label, fixed sequence clinical trial. Ritonavir was administered orally as 100-mg tablets (Norvir® 100-mg film-coated tablets, Abbvie, Ludwigshafen, Germany) bid for 5 days. Before ritonavir administration (baseline day) and on the last day of ritonavir intake, the participants received a microdosed cocktail of FXaI (Fig. 1) consisting of apixaban 25 µg (Eliquis®, Bristol-Myers Squibb, Munich, Germany), edoxaban 50 µg (Lixiana®, Daiichi Sankyo Europe, Munich, Germany), and rivaroxaban 25 µg (Xarelto®, Bayer, Leverkusen, Germany) [25]. The oral stock solutions of edoxaban (30 µg/mL), rivaroxaban (25 µg/mL), and apixaban (25 µg/mL) were prepared by the Pharmacy of Heidelberg University Hospital in compliance with GMP guidelines according to the pharmaceutical development protocols approved by the competent authority (BfArM, Bonn, Germany).
Eight healthy volunteers received oral ritonavir 100 mg (blue boxes) twice daily from day 1 to 5. At baseline and on day 5, a microdosed cocktail consisting of apixaban 25 µg, edoxaban 50 µg, and rivaroxaban 25 µg was administered (µFXaI, orange boxes). Additionally, at each visit, a cocktail of CYP probe drugs (green boxes) consisting of midazolam 10 µg (at baseline 30 µg), yohimbine 50 µg, and omeprazole 100 µg together with sodium hydrogen carbonate (50 mL 10 min before and 100 mL simultaneously) was administered. Blood samples (red arrows) for the analyses of FXaI concentration were taken before and 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 23, and 24 h after drug administration at baseline and on day 5. On other study visits, blood samplings were taken over a period of 4 h (before, 0.5, 1, 1.5, 2, 2.5, 3, and 4 h post dose). Urine was collected for 24 h at baseline and on day 5. CYP cytochrome P450, FXaI factor Xa inhibitor
To monitor the different CYP isozyme activities, midazolam (Dormicum®; 5 mg/5 mL solutions for infusion; Roche, Grenzach-Wyhlen, Germany; 30 µg at baseline and 10 µg at all other administration times), yohimbine 50 µg (Yohimbinum hydrochloricum D4® tablets, DHU-Arzneimittel GmbH, Karlsruhe, Germany), and omeprazole 100 µg (OMEP® 40 mg power for solution for infusion; Hexal, Holzkirchen, Germany) were administered as oral solutions together with the FXaI cocktail before ritonavir was initiated, every day with the intake of ritonavir, and 2 and 4 days after stopping ritonavir. To buffer gastric acid and prevent degradation of the uncoated omeprazole, sodium hydrogen carbonate (4.2% w/v) was administered 10 min before (50 mL equivalent to 25 mmol) and simultaneously (100 mL equivalent to 50 mmol) with the 100-µg uncoated omeprazole dose as used previously [28]. Microdoses were always prepared immediately before administration and were administered with ritonavir always in the same sequence (first the FXaI, followed by yohimbine, midazolam, and omeprazole) within 1 min.
2.2 Trial Population
We enrolled volunteers who were in good physical and mental health and had no clinically relevant findings in medical history, physical examination, electrocardiogram, and routine laboratory analyses including renal and liver function. Not enrolled were pregnant or lactating women, participants with known intolerance or contraindication to any component of the trial medication, a history of anaphylactic shock, or participants of an interventional clinical trial within 30 days before inclusion. The use of medicines (except iodine and levothyroxine), cannabis, or citrus fruits (including grapefruit) was not allowed during the trial, and enrolment in the study was allowed at the earliest 5 half-lives (for inhibitors) or 2 weeks (for inductors) after discontinuation of the previously taken medicines. Alcohol and smoking were not allowed on study days. All participants used highly effective contraceptive methods (intrauterine devices, intrauterine hormone-releasing systems, vasectomized partner, or sexual abstinence for female volunteers and condom or sexual abstinence for men) during the trial and for a further 2 weeks after the last medication intake.
2.3 Trial Conduct
The trial was conducted at the Clinical Research Centre of the Department of Clinical Pharmacology and Pharmacoepidemiology (KliPS), Heidelberg University Hospital, which is certified according to DIN EN ISO 9001:2015. Participants arrived fasting (for at least 8 h) and remained fasting for a further 4 h after taking all microdoses simultaneously. Blood samples for the analyses of FXaI concentration were drawn before and 0.5, 1, 1.5, 2, 2.5, 3, 4, 6, 8, 23, and 24 h after drug administration on the first day (baseline) and at the fifth day of ritonavir intake (Fig. 1). On days with FXaI intake, the entire 24-h urine was collected. Blood samples for analyses of yohimbine, omeprazole, and ritonavir were taken before and 0.5, 1, 1.5, 2, 2.5, 3, and 4 h on every day of ritonavir intake and on days 2 and 4 after discontinuation of ritonavir. Additional ritonavir plasma samples were taken 6, 8, 23, and 24 h after dosing on baseline and on day 5. Midazolam plasma samples were taken before and 2, 2.5, 3, and 4 h after drug administration on each study day.
All samples were collected in lithium-heparin tubes and centrifuged for 10 min at 20 °C and 2500g within 30 min. Urine aliquots and separated plasma aliquots were stored at − 20 °C until analysis.
2.4 Quantification of Factor Xa Inhibitors and Probe Drugs
The concentrations of FXaI, midazolam, yohimbine, and omeprazole with 5’-hydroxy omeprazole were quantified by ultra-performance liquid chromatography coupled to tandem mass spectrometry (UPLC–MS/MS) according to published assays [29,30,31,32] with a lower limit of quantification (LLOQ) of 1 pg/mL for midazolam and yohimbine and 5 pg/mL for omeprazole, 5′-hydroxy omeprazole, and the FXaI. Ritonavir plasma concentrations were quantified by high-performance LC–MS/MS with a LLOQ of 10 ng/mL [2]. Urine samples were diluted 1:10 with blank human plasma for analyses of FXaI concentrations [33]. Accuracy and precision values were always ≤ ± 15% and all assays complied with the relevant guidelines for the validation of bioanalytical methods of the European Medicines Agency and the US Food and Drug Administration [34, 35].
2.5 Calculations and Statistical Analysis
The sample size was determined using the interaction data from a previous trial (EudraCT 2017-004453) [36] investigating the effect of ketoconazole on FXaI, which was assumed to be comparable to ritonavir. A sample size of 3 (apixaban and rivaroxaban) and 5 (edoxaban) was calculated to detect the observed area under the plasma concentration–time curve (AUC) extrapolated to infinity (AUCinf) ratio of 1.68 ± 0.36 for apixaban, 2.28 ± 1.10 for edoxaban, and 2.37 ± 0.53 for rivaroxaban with a power of 0.8 and an α error of 5%. Using these data, a two-sided paired t-test with a sample size of N = 8 (log-transformed AUCinf) would allow to detect a 20% change of exposure (i.e., an AUCinf ratio of 1.20) for apixaban, rivaroxaban, and edoxaban with a power of 80% and an α error of 5%.
The standard non-compartmental pharmacokinetic parameters of each FXaI were calculated using Phoenix™ WinNonlin Software 8.3.5 (Certara, Princeton, NJ, USA). The calculated parameters included maximum plasma concentration (Cmax), time to Cmax (tmax), AUCinf, AUC from 0 to 24 h (AUC0–24), 0 to 4 h (AUC0–4, omeprazole, yohimbine), and 2 to 4 h (AUC2–4, midazolam), apparent volume of distribution at steady-state (Vz/F), apparent oral clearance (CL/F), terminal elimination half-life (t½), renal clearance (CLrenal), expressed as the amount excreted unchanged in urine over 24 h divided by AUC0–24, and non-renal clearance (CLnonrenal) as the difference between CL/F and renal clearance. The AUC was calculated using a mixed log-linear trapezoidal model.
To determine the effect of ritonavir on CYP3A activity, the estimated midazolam partial metabolic clearance (eCLmet) was calculated using the data of a limited sampling methodology [8, 37, 38]. Due to the prolonged midazolam elimination half-life with coadministration of ritonavir, midazolam concentrations above the LLOQ were observed in predose samples from the second day of ritonavir intake until 4 days after ritonavir discontinuation, which was taken into account as follows: the residual AUC was calculated using the predose concentration and the current half-life in the interval 2–4 h of the individual visit and then subtracted accordingly. The CYP3A4 recovery half-life was calculated as described previously [39].
The effect of ritonavir on CYP2C19 and CYP2D6 activity was determined using AUC0–4 and Cmax of yohimbine and omeprazole. The exposure of ritonavir was determined using AUC0–4 after dose 1, 3, 5, 7, and 9, and after discontinuation.
Data are reported as geometric means with 95% confidence intervals (CIs) except tmax, which is reported as median with range. To test for differences of each FXaI separately between baseline and ritonavir, the geometric mean ratios (GMRs) and their 90% CIs were calculated. The default no-effect boundary of point estimates is 0.8–1.25 and when 90% CIs for systemic exposure (AUC) ratios are entirely within the equivalence range of 0.85–1.25, according to the standard practice of the FDA, it is concluded that no clinically relevant interaction is present. For other FXaI PK parameters, a ratio paired t-test (two-tailed) was performed to compare day 5 of ritonavir intake with baseline.
To account for the multiple occasions of assessing midazolam, yohimbine, and omeprazole exposure, repeated-measure one-way ANOVA of logarithmic transformed data with correction for multiple testing (Dunnett’s multiple comparisons test) was performed to test for differences to baseline.
All statistics were performed with Prism 9.0.0 (GraphPad Software, La Jolla, CA, USA). A p value <0.05 was considered significant.
3 Results
Nine healthy volunteers were included in the study. One participant dropped out on the last day of ritonavir intake due to an unrelated COVID-19 infection. Therefore, eight participants (7 females) with a median age of 25.5 years (range 21–58) and a body mass index of 24.2 kg/m2 (range 18.0–28.1) completed the study.
3.1 Factor Xa Inhibitors
Over the observation period, all plasma concentrations were above the LLOQ, except for the 23- and 24-h edoxaban concentrations in two and the 24-h edoxaban concentration in three participants. The 24-h urine collection from one participant was excluded from analyses due to suspected incomplete urine collection on day 5.
Coadministration of ritonavir 100 mg bid for 5 days increased plasma concentrations of all three FXaI (Fig. 2; Tables 1 and 2). The individual increase in AUC0–24 for apixaban and edoxaban was heterogeneous: three participants had an AUC0–24 ratio of 0.8–1.2 versus two and three participants, respectively, with AUC0–24 increases of 2–2.3 (Fig. 3). The largest and consistent change was observed for rivaroxaban. A slightly but significantly prolonged t½ (from 5.14 h to 6.57 h) and a significantly reduced CLrenal (from 49.4 to 34.8 mL/min) were observed for rivaroxaban but not for the other two FXaI. The volume of distribution was significantly reduced for edoxaban and rivaroxaban but not for apixaban.
Individual AUC0–24 changes of apixaban, edoxaban, and rivaroxaban and geometric population mean (with 95% confidence interval) of 8 healthy volunteers after oral administration of apixaban 25 µg, edoxaban 50 µg, and rivaroxaban 25 µg alone and during low-dose ritonavir for 5 days. AUC0–24 area under the plasma concentration–time curve from 0 to 24 h
3.2 CYP Probe Drugs
3.2.1 Midazolam
Ritonavir profoundly reduced the CLmet of midazolam (Table 3) and already after the first intake of ritonavir 100 mg, midazolam AUC2–4 increased 5.1-fold. From day 2 to day 5 of ritonavir treatment, the AUC2–4 of midazolam continued to increase to 11.1–15.5 times baseline values and recovered only slowly after ritonavir discontinuation, with AUC2–4 values still 10.2-fold and 2.9-fold higher 2 and 4 days after ritonavir discontinuation, respectively (Fig. 4). The estimated CYP3A4 recovery half-life was 2.30 ± 0.89 days.
Time course of the estimated geometric mean metabolic clearance (CLmet, with 95% confidence interval) of midazolam in 8 healthy volunteers before (baseline) and during ritonavir therapy (100 mg twice daily, days 1–5; light blue box) as well as 2 and 4 days after ritonavir discontinuation (day 7 and 9, respectively)
3.2.2 Omeprazole and Yohimbine
The baseline pharmacokinetics of yohimbine and omeprazole are shown in Table 3. During ritonavir, omeprazole pharmacokinetics were unchanged but after ritonavir discontinuation, the AUC0–4 was decreased by approximately 35% and the AUC0–4 ratio also decreased (Fig. 5). The molar AUC0–4 ratio of omeprazole and 5-OH-omeprazole decreased from baseline during ritonavir treatment and was significantly reduced on days 4 and 5 (32%), and remained significantly reduced afterwards (Table 3).
Geometric means of the omeprazole AUC0–4 and 5-OH-omeprazole AUC0–4 of a 100-µg omeprazole dose (with 95% confidence intervals) before (baseline) and during ritonavir (100 mg bid) for 5 days (light blue box), as well as 2 and 4 days after ritonavir discontinuation (day 7 and 9, respectively). ns: p > 0.05. AUC0–4 area under the concentration–time curve from 0 to 4 h, bid twice daily
Ritonavir gradually, but not significantly, increased yohimbine AUC0–4 to a GMR of approximately 1.5; this effect was short-lived and 2 days after ritonavir discontinuation, CYP2D6 activity had returned to baseline activity (Table 3; Fig. 6).
Geometric means of AUC0–4 of a 50-µg yohimbine dose (with 95% confidence intervals) before (baseline) and during ritonavir (100 mg bid) for 5 days (light blue box), as well as 2 and 4 days after ritonavir discontinuation (day 7 and 9, respectively). ns: p > 0.05. AUC0–4 area under the concentration–time curve from 0 to 4 h, bid twice daily
3.3 Ritonavir
The AUC0–4 of ritonavir was 906 ng/mL⋅h (95% CI 543–1512) and Cmax was 373 ng/mL (95% CI 244–572) after intake of the first dose. Exposure and Cmax were similar on the remaining 4 days, ranging between 4593–5331 ng/mL⋅h and 1776–2107 ng/mL, respectively (Fig. 7). Two days after the last ritonavir dose, concentrations were close to or below the LLOQ.
3.4 Safety Data
Overall, the study medication was well tolerated. Twenty adverse events (5 considered related to study drug) were observed in six participants with most adverse events occurring on baseline day, that is, before ritonavir administration (Supplementary Table S1, see electronic supplementary material [ESM]), and all were transient. One adverse event (presyncope) was moderate and one (syncope) was severe and both occurred as an immediate consequence of unsuccessful venepunctures; all other adverse events were mild. The most common adverse event was headache on the first study day without ritonavir therapy (5 out of 8 participants affected). A relationship was considered unlikely, as only microdosed substances were administered on this day and headaches only occurred in one participant after repeated administration on the fifth day of ritonavir intake.
4 Discussion
4.1 Interaction of Low-Dose Ritonavir With Factor Xa Inhibitors
Treatment with ritonavir 100 mg bid for 5 days increased the AUC0–24 of all currently marketed FXaI but with different magnitude and likely little clinical relevance in the absence of other clearance impairment (e.g., renal dysfunction) [40,41,42]. The largest increase was observed with rivaroxaban but this change was below the order of magnitude that usually prompts dose reductions (factor 2). Unless very high doses are administered, as required in the initial treatment of major embolic events [43], dose reductions should be individually planned and it should also be considered that COVID-19 can trigger a prothrombotic state and at least prophylactic anticoagulation is generally recommended [44].
The differences in the magnitude of interaction between the different FXaI are not fully elucidated. They are certainly influenced by the different effects of ritonavir on the diverse clearance mechanisms involved, and similar differences have also been observed in a series of patients receiving these FXaI together with protease inhibitors boosted with ritonavir 100 mg bid [18,19,20,21,22,23]. In these earlier case series and in our study, the interaction was most pronounced with rivaroxaban, the FXaI with the largest bioavailability (and complete bioavailability at low doses [45]), indicating that the exposure change was not caused by a change in bioavailability but rather a reduction of systemic drug clearance, which is also reflected in a prolongation of the elimination t½. Other than with other FXaI, these clearance changes were partly due to reduced renal excretion, likely reflecting combined inhibition of efflux transporters (P-gp and BCRP) and of the organic anion transporter 3 (OAT3, SLC22A8), which plays a major role in the renal elimination of rivaroxaban [46, 47]. In our study with low ritonavir doses, the effect was smaller than the interaction observed with very high doses of ritonavir (600 mg bid), where a 2.5-fold increase in AUC and an even more extensive reduction of CLrenal were observed [17, 25, 36]. These data therefore suggest that boosting doses of ritonavir do not completely inhibit renal efflux transporters while they are likely high enough to inhibit CYP3A4 (and possibly CYP2J2 [7, 17, 48]) as efficiently as higher doses [2].
In contrast, there was only a minor DDI with apixaban, which is in agreement with the minimal interaction with potent CYP3A inhibitors such as voriconazole [25, 36] and the limited suspected contribution of efflux transporters [49] or OAT3 [47].
Ritonavir also increased edoxaban exposure but, in contrast to rivaroxaban, CLrenal and t½ were not altered, suggesting an increase in bioavailability as a result of intestinal inhibition of efflux transporters. This is consistent with other DDI studies and physiology-based pharmacokinetic modelling, which suggested a role of intestinal P-gp (and possibly BCRP) in edoxaban bioavailability [50,51,52]. It also agrees well with the effect size observed with the P-gp substrate dabigatran etexilate when it was administered with the same dose of ritonavir [53]. In addition, ritonavir also inhibits carboxylesterase 1 (CES1) in vitro [54], suggesting that concurrent inhibition of this minor pathway [10] could additionally be involved. The different influence of ritonavir on the urinary excretion of FXaI could be due to the fact that edoxaban and apixaban are not substrates of OAT3 and therefore the activity of the downstream renal P-gp is less important for their urinary excretion [47, 51].
4.2 CYP Probe Drugs
Our trial generated activity data of relevant drug metabolising CYPs over the time course of ritonavir treatment (5 days) and after its discontinuation. As expected [2], already after the first ritonavir dose, the CYP3A4 clearance profoundly decreased, indicating strong inhibition. This is in line with the dose–CYP3A4 inhibition relationship established in vivo, which estimated that the ritonavir dose inhibiting CYP3A4 by 50% (ED50) was very low (3.4 mg) [2]. After ritonavir discontinuation, the CYP3A activity recovered slowly with a half-life of 2.3 days. On day 4 after ritonavir discontinuation, CYP3A activity was still reduced while no ritonavir was detectable in plasma, which suggests prolonged mechanism-based inactivation of CYP3A4. Based on these data, the full recovery of CYP3A4 activity is estimated to take 10–12 days after a 5-day treatment course with ritonavir 100 mg bid.
Regarding the effect of ritonavir on CYP2D6 activity, no significant changes of the probe drug yohimbine were observed. In contrast, using desipramine as an index substrate for CYP2D6, ritonavir (100 mg bid) caused a modest inhibitory effect on CYP2D6 activity in extensive metabolizers [55]. However, the dextromethorphan/dextrorphan metabolic ratio as another indicator for CYP2D6 activity was not altered. Thus, these findings with microdosed yohimbine as a sensitive CYP2D6 probe drug [27] confirm that no clinically relevant alteration of CYP2D6 enzyme activity during the course of a 5-day treatment with ritonavir 100 mg bid occurs.
Ritonavir had a small induction effect on CYP2C19 activity leading to slightly decreased omeprazole exposure on day 5 of ritonavir treatment, which was also reflected in corresponding changes in the molar AUC ratio of omeprazole and 5-hydroxy omeprazole. This inducing effect is time-dependent as it is more pronounced after a 10-day ritonavir (100 mg bid) treatment [56]. CYP2C19 induction is also dose-dependent as reported with other CYP2C19 substrates; as an example, after 20 days of ritonavir (100 mg bid) treatment, voriconazole exposure was decreased by 33% [57] or 39% [58], which is only a small effect, probably attenuated by the autoinhibition of voriconazole [59, 60]. However, higher doses of ritonavir 400 mg bid for 20 days decreased voriconazole AUC by 83% [58]. Although short-term ritonavir treatment with low doses induces CYP2C19 activity, this effect is short lasting and likely does not require any dose adaptation of CYP2C19 substrates.
4.3 Limitations
The following limitations merit discussion. First, we only assessed the effect on the last day of the 5-day ritonavir treatment, which was expected to be the day with the maximum possible change in short-course low-dose therapies with ritonavir. Due to its short duration, this trial was not suitable to assess the potential inducing properties of ritonavir and its results should only be extrapolated to longer treatment regimens with caution. In addition, no transporter probe drugs were tested, so the time course of transporter inhibition is still not well characterized. Second, patients may differ from healthy volunteers in many ways. In patients, comorbidities such as renal impairment can potentiate apparently minor DDI [41, 42] and it will always be critical to consider all relevant clearance pathways when determining appropriate individualized treatment plans for FXaI. Third, coadministration of the probe drugs with sodium hydrogen carbonate to buffer gastric acid could potentially influence their pharmacokinetics. However, the baseline pharmacokinetics agree well with prior studies using microdosed FXaI [25, 36], suggesting that buffering did not alter the pharmacokinetics of the three microdosed FXaI. This is in line with the absence of clinically relevant DDI of therapeutic FXaI doses with acid lowering drugs such as famotidine, ranitidine, or omeprazole [61,62,63,64]. In addition, the clearance values and relative contribution of renal excretion compare well with those reported for regular doses of FXaI in healthy volunteers [17, 18, 65], suggesting that microdoses adequately reflect the pharmacokinetics of regular doses and are therefore suitable for DDI studies.
5 Conclusion
We have successfully evaluated the effect of a 5-day treatment regimen with low doses of ritonavir (100 mg bid) on the pharmacokinetics of three FXaI in healthy volunteers (Fig. 8) and found that the clearance of all FXaI decreased with potential clinical relevance only for rivaroxaban, where a dose reduction by a factor of 0.5 might be considered if therapeutic rivaroxaban doses are administered. Concurrently, we also monitored the daily activity changes of three important CYPs over the 5-day treatment and 2 days and 4 days after discontinuation of ritonavir and found that CYP2D6 activity was not significantly altered, while CYP2C19 was mildly induced and CYP3A was profoundly inhibited.
Radar chart of oral clearance changes induced by 5 days of low-dose ritonavir therapy (100 mg twice daily) in 8 healthy volunteers. The percentage clearance compared with baseline, which is set at 100%, is shown for the different study days. The area of bioequivalence is highlighted in green, the risk area where dose adjustments may be required is highlighted in red
References
Lamb YN. Nirmatrelvir plus ritonavir: first approval. Drugs. 2022;82(5):585–91. https://doi.org/10.1007/s40265-022-01692-5.
Eichbaum C, Cortese M, Blank A, Burhenne J, Mikus G. Concentration effect relationship of CYP3A inhibition by ritonavir in humans. Eur J Clin Pharmacol. 2013;69(10):1795–800. https://doi.org/10.1007/s00228-013-1530-8.
Zeldin RK, Petruschke RA. Pharmacological and therapeutic properties of ritonavir-boosted protease inhibitor therapy in HIV-infected patients. J Antimicrob Chemother. 2004;53(1):4–9. https://doi.org/10.1093/jac/dkh029.
Foisy MM, Yakiwchuk EM, Hughes CA. Induction effects of ritonavir: implications for drug interactions. Ann Pharmacother. 2008;42(7):1048–59. https://doi.org/10.1345/aph.1K615.
Kis O, Robillard K, Chan GN, Bendayan R. The complexities of antiretroviral drug-drug interactions: role of ABC and SLC transporters. Trends Pharmacol Sci. 2010;31(1):22–35. https://doi.org/10.1016/j.tips.2009.10.001.
Vermeer LM, Isringhausen CD, Ogilvie BW, Buckley DB. Evaluation of ketoconazole and its alternative clinical CYP3A4/5 inhibitors as inhibitors of drug transporters: the in vitro effects of ketoconazole, ritonavir, clarithromycin, and itraconazole on 13 clinically-relevant drug transporters. Drug Metab Dispos. 2016;44(3):453–9. https://doi.org/10.1124/dmd.115.067744.
Loos NHC, Beijnen JH, Schinkel AH. The mechanism-based inactivation of CYP3A4 by ritonavir: what mechanism? Int J Mol Sci. 2022;23(17):9866. https://doi.org/10.3390/ijms23179866.
Katzenmaier S, Markert C, Riedel KD, Burhenne J, Haefeli WE, Mikus G. Determining the time course of CYP3A inhibition by potent reversible and irreversible CYP3A inhibitors using a limited sampling strategy. Clin Pharmacol Ther. 2011;90(5):666–73. https://doi.org/10.1038/clpt.2011.164.
Ali MAM, Spinler SA. COVID-19 and thrombosis: from bench to bedside. Trends Cardiovasc Med. 2021;31(3):143–60. https://doi.org/10.1016/j.tcm.2020.12.004.
Bathala MS, Masumoto H, Oguma T, He L, Lowrie C, Mendell J. Pharmacokinetics, biotransformation, and mass balance of edoxaban, a selective, direct factor Xa inhibitor, in humans. Drug Metab Dispos. 2012;40(12):2250–5. https://doi.org/10.1124/dmd.112.046888.
Wang L, Zhang D, Raghavan N, Yao M, Ma L, Frost CE, et al. In vitro assessment of metabolic drug-drug interaction potential of apixaban through cytochrome P450 phenotyping, inhibition, and induction studies. Drug Metab Dispos. 2010;38(3):448–58. https://doi.org/10.1124/dmd.109.029694.
Weinz C, Schwarz T, Kubitza D, Mueck W, Lang D. Metabolism and excretion of rivaroxaban, an oral, direct factor Xa inhibitor, in rats, dogs, and humans. Drug Metab Dispos. 2009;37(5):1056–64. https://doi.org/10.1124/dmd.108.025569.
Mueck W, Schwers S, Stampfuss J. Rivaroxaban and other novel oral anticoagulants: pharmacokinetics in healthy subjects, specific patient populations and relevance of coagulation monitoring. Thromb J. 2013;11(1):10. https://doi.org/10.1186/1477-9560-11-10.
Zhao T, Chen Y, Wang D, Wang L, Dong P, Zhao S, et al. Identifying the dominant contribution of human cytochrome P450 2J2 to the metabolism of rivaroxaban, an oral anticoagulant. Cardiovasc Drugs Ther. 2022;36(1):121–9. https://doi.org/10.1007/s10557-020-07129-z.
Ruff CT, Giugliano RP, Braunwald E, Morrow DA, Murphy SA, Kuder JF, et al. Association between edoxaban dose, concentration, anti-factor Xa activity, and outcomes: an analysis of data from the randomised, double-blind ENGAGE AF-TIMI 48 trial. Lancet. 2015;385(9984):2288–95. https://doi.org/10.1016/s0140-6736(14)61943-7.
Herink MC, Zhuo YF, Williams CD, DeLoughery TG. Clinical management of pharmacokinetic drug interactions with direct oral anticoagulants (DOACs). Drugs. 2019;79(15):1625–34. https://doi.org/10.1007/s40265-019-01183-0.
Mueck W, Kubitza D, Becka M. Co-administration of rivaroxaban with drugs that share its elimination pathways: pharmacokinetic effects in healthy subjects. Br J Clin Pharmacol. 2013;76(3):455–66. https://doi.org/10.1111/bcp.12075.
Testa S, Prandoni P, Paoletti O, Morandini R, Tala M, Dellanoce C, et al. Direct oral anticoagulant plasma levels’ striking increase in severe COVID-19 respiratory syndrome patients treated with antiviral agents: the Cremona experience. J Thromb Haemost. 2020;18(6):1320–3. https://doi.org/10.1111/jth.14871.
Lomakina V, Sozio SJ, Tekle J. Use of apixaban in atrial fibrillation with ritonavir-boosted antiretroviral therapy: a case report. J Pharm Pract. 2022;36(3):728–32. https://doi.org/10.1177/08971900221074938.
Nisly SA, Stevens BN. Ritonavir- or cobicistat-boosted antiretroviral therapy and direct oral anticoagulants: a case for apixaban. Int J STD AIDS. 2019;30(7):718–22. https://doi.org/10.1177/0956462419832099.
Corallo CE, Grannell L, Tran H. Postoperative bleeding after administration of a single dose of rivaroxaban to a patient receiving antiretroviral therapy. Drug Saf Case Rep. 2015;2(1):11. https://doi.org/10.1007/s40800-015-0014-4.
George JM, Kuriakose SS, Monroe A, Hou Q, Byrne M, Pau AK, et al. Utilization of direct oral anticoagulants in people living with human immunodeficiency virus: observational data from the District of Columbia cohort. Clin Infect Dis. 2020;71(10):e604–13. https://doi.org/10.1093/cid/ciaa284.
Lakatos B, Stoeckle M, Elzi L, Battegay M, Marzolini C. Gastrointestinal bleeding associated with rivaroxaban administration in a treated patient infected with human immunodeficiency virus. Swiss Med Wkly. 2014;22(144): w13906. https://doi.org/10.4414/smw.2014.13906.
European Medicines Agency. Summary of product characteristics Paxlovid. 2022. https://www.ema.europa.eu/en/documents/product-information/paxlovid-epar-product-information_en.pdf. Accessed 18 Sept 2023.
Mikus G, Foerster KI, Schaumaeker M, Lehmann ML, Burhenne J, Haefeli WE. Application of a microdosed cocktail of 3 oral factor Xa inhibitors to study drug-drug interactions with different perpetrator drugs. Br J Clin Pharmacol. 2020;86(8):1632–41. https://doi.org/10.1111/bcp.14277.
Lenard A, Hermann SA, Stoll F, Burhenne J, Foerster KI, Mikus G, et al. Effect of clarithromycin, a strong CYP3A and P-glycoprotein inhibitor, on the pharmacokinetics of edoxaban in healthy volunteers and the evaluation of the drug interaction with other oral factor Xa inhibitors by a microdose cocktail approach. Cardiovasc Drugs Ther. 2023. https://doi.org/10.1007/s10557-023-07443-2.
Vay M, Meyer MJ, Blank A, Skopp G, Rose P, Tzvetkov MV, et al. Oral yohimbine as a new probe drug to predict CYP2D6 activity: results of a fixed-sequence phase I trial. Clin Pharmacokinet. 2020;59(7):927–39. https://doi.org/10.1007/s40262-020-00862-6.
Elbe A, Foerster KI, Blank A, Rose P, Burhenne J, Haefeli WE, et al. Evaluation of CYP2C19 activity using microdosed oral omeprazole in humans. Eur J Clin Pharmacol. 2022;78(6):975–87. https://doi.org/10.1007/s00228-022-03304-3.
Foerster KI, Huppertz A, Muller OJ, Rizos T, Tilemann L, Haefeli WE, et al. Simultaneous quantification of direct oral anticoagulants currently used in anticoagulation therapy. J Pharm Biomed Anal. 2018;30(148):238–44. https://doi.org/10.1016/j.jpba.2017.10.011.
Burhenne J, Halama B, Maurer M, Riedel KD, Hohmann N, Mikus G, et al. Quantification of femtomolar concentrations of the CYP3A substrate midazolam and its main metabolite 1’-hydroxymidazolam in human plasma using ultra performance liquid chromatography coupled to tandem mass spectrometry. Anal Bioanal Chem. 2012;402(7):2439–50. https://doi.org/10.1007/s00216-011-5675-y.
Vay M, Sauter M, Mikus G, Burhenne J. Quantification of microdosed oral yohimbine and its major metabolite in human plasma in the picogram range. Bioanalysis. 2019;11(16):1459–67. https://doi.org/10.4155/bio-2019-0129.
Mahmoudi M, Foerster KI, Burhenne J, Weiss J, Mikus G, Haefeli WE. Application of microdosed intravenous omeprazole to determine hepatic CYP2C19 activity. J Clin Pharmacol. 2021;61(6):789–98. https://doi.org/10.1002/jcph.1789.
Mikus G, Foerster KI, Schaumaeker M, Lehmann M-L, Burhenne J, Haefeli WE. Microdosed cocktail of three oral factor Xa inhibitors to evaluate drug-drug interactions with potential perpetrator drugs. Clin Pharmacokinet. 2019;58(9):1155–63. https://doi.org/10.1007/s40262-019-00749-1.
Food and Drug Administration. Bioanalytical method validation guidance for industry. 2018. https://www.fda.gov/files/drugs/published/Bioanalytical-Method-Validation-Guidance-for-Industry.pdf. Accessed 18 Sept 2023.
European Medical Agency. Guideline on bioanalytical method validation. 2012. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-bioanalytical-method-validation_en.pdf. Accessed 18 Sept 2023.
Rohr BS, Foerster KI, Blank A, Burhenne J, Mahmoudi M, Haefeli WE, et al. Perpetrator characteristics of azole antifungal drugs on three oral factor Xa inhibitors administered as a microdosed cocktail. Clin Pharmacokinet. 2022;61(1):97–109. https://doi.org/10.1007/s40262-021-01051-9.
Katzenmaier S, Markert C, Mikus G. Proposal of a new limited sampling strategy to predict CYP3A activity using a partial AUC of midazolam. Eur J Clin Pharmacol. 2010;66(11):1137–41. https://doi.org/10.1007/s00228-010-0878-2.
Halama B, Hohmann N, Burhenne J, Weiss J, Mikus G, Haefeli WE. A nanogram dose of the CYP3A probe substrate midazolam to evaluate drug interactions. Clin Pharmacol Ther. 2013;93(6):564–71. https://doi.org/10.1038/clpt.2013.27.
Breithaupt MH, Krohmer E, Taylor L, Körner E, Hoppe-Tichy T, Burhenne J, et al. Time course of CYP3A activity during and after metamizole (dipyrone) in healthy volunteers. Br J Clin Pharmacol. 2023;89(8):2458–64. https://doi.org/10.1111/bcp.15720.
Wang Z, Chan ECY. Physiologically-based pharmacokinetic modeling-guided dose management of oral anticoagulants when initiating nirmatrelvir/ritonavir (Paxlovid) for COVID-19 treatment. Clin Pharmacol Ther. 2022;112(4):803–7. https://doi.org/10.1002/cpt.2687.
Willmann S, Coboeken K, Kapsa S, Thelen K, Mundhenke M, Fischer K, et al. Applications of physiologically based pharmacokinetic modeling of rivaroxaban-renal and hepatic impairment and drug–drug interaction potential. J Clin Pharmacol. 2021;61(5):656–65. https://doi.org/10.1002/jcph.1784.
Hanigan S, Park JM. Evaluating pharmacokinetic drug-drug interactions of direct oral anticoagulants in patients with renal dysfunction. Expert Opin Drug Metab Toxicol. 2022;18(3):189–202. https://doi.org/10.1080/17425255.2022.2074397.
European Medicines Agency. Summary of product characteristics Xarelto®. 2018. https://www.ema.europa.eu/en/medicines/human/EPAR/xarelto. Accessed 18 Sept 2023.
Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, et al. Scientific and standardization committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1859–65. https://doi.org/10.1111/jth.14929.
Stampfuss J, Kubitza D, Becka M, Mueck W. The effect of food on the absorption and pharmacokinetics of rivaroxaban. Int J Clin Pharmacol Ther. 2013;51(7):549–61. https://doi.org/10.5414/cp201812.
Cheong EJY, Teo DWX, Chua DXY, Chan ECY. Systematic development and verification of a physiologically based pharmacokinetic model of rivaroxaban. Drug Metab Dispos. 2019;47(11):1291–306. https://doi.org/10.1124/dmd.119.086918.
Tsuruya Y, Nakanishi T, Komori H, Wang X, Ishiguro N, Kito T, et al. Different involvement of OAT in renal disposition of oral anticoagulants rivaroxaban, dabigatran, and apixaban. J Pharm Sci. 2017;106(9):2524–34. https://doi.org/10.1016/j.xphs.2017.04.044.
Kaspera R, Kirby BJ, Sahele T, Collier AC, Kharasch ED, Unadkat JD, et al. Investigating the contribution of CYP2J2 to ritonavir metabolism in vitro and in vivo. Biochem Pharmacol. 2014;91(1):109–18. https://doi.org/10.1016/j.bcp.2014.06.020.
Sodhi JK, Liu S, Benet LZ. Intestinal efflux transporters P-gp and BCRP are not clinically relevant in apixaban disposition. Pharm Res. 2020;37(10):208. https://doi.org/10.1007/s11095-020-02927-4.
Parasrampuria DA, Truitt KE. Pharmacokinetics and pharmacodynamics of edoxaban, a non-vitamin K antagonist oral anticoagulant that inhibits clotting factor Xa. Clin Pharmacokinet. 2016;55(6):641–55. https://doi.org/10.1007/s40262-015-0342-7.
Mikkaichi T, Yoshigae Y, Masumoto H, Imaoka T, Rozehnal V, Fischer T, et al. Edoxaban transport via P-glycoprotein is a key factor for the drug’s disposition. Drug Metab Dispos. 2014;42(4):520–8. https://doi.org/10.1124/dmd.113.054866.
Kato T, Mikkaichi T, Yoshigae Y, Okudaira N, Shimizu T, Izumi T, et al. Quantitative analysis of an impact of P-glycoprotein on edoxaban’s disposition using a human physiologically based pharmacokinetic (PBPK) model. Int J Pharm. 2021;15(597): 120349. https://doi.org/10.1016/j.ijpharm.2021.120349.
Cox DS, Rehman M, Khan T, Ginman K, Salageanu J, LaBadie RR, et al. Effects of nirmatrelvir/ritonavir on midazolam and dabigatran pharmacokinetics in healthy participants. Br J Clin Pharmacol. 2023;89(11):3352–63. https://doi.org/10.1111/bcp.15835.
Rhoades JA, Peterson YK, Zhu HJ, Appel DI, Peloquin CA, Markowitz JS. Prediction and in vitro evaluation of selected protease inhibitor antiviral drugs as inhibitors of carboxylesterase 1: a potential source of drug-drug interactions. Pharm Res. 2012;29(4):972–82. https://doi.org/10.1007/s11095-011-0637-9.
Aarnoutse RE, Kleinnijenhuis J, Koopmans PP, Touw DJ, Wieling J, Hekster YA, et al. Effect of low-dose ritonavir (100 mg twice daily) on the activity of cytochrome P450 2D6 in healthy volunteers. Clin Pharmacol Ther. 2005;78(6):664–74. https://doi.org/10.1016/j.clpt.2005.09.001.
Yeh RF, Gaver VE, Patterson KB, Rezk NL, Baxter-Meheux F, Blake MJ, et al. Lopinavir/ritonavir induces the hepatic activity of cytochrome P450 enzymes CYP2C9, CYP2C19, and CYP1A2 but inhibits the hepatic and intestinal activity of CYP3A as measured by a phenotyping drug cocktail in healthy volunteers. J Acquir Immune Defic Syndr. 2006;42(1):52–60. https://doi.org/10.1097/01.qai.0000219774.20174.64.
Zhu L, Bruggemann RJ, Uy J, Colbers A, Hruska MW, Chung E, et al. CYP2C19 genotype-dependent pharmacokinetic drug interaction between voriconazole and ritonavir-boosted atazanavir in healthy subjects. J Clin Pharmacol. 2017;57(2):235–46. https://doi.org/10.1002/jcph.798.
Liu P, Foster G, Gandelman K, LaBadie RR, Allison MJ, Gutierrez MJ, et al. Steady-state pharmacokinetic and safety profiles of voriconazole and ritonavir in healthy male subjects. Antimicrob Agents Chemother. 2007;51(10):3617–26. https://doi.org/10.1128/aac.00526-07.
Hohmann N, Kocheise F, Carls A, Burhenne J, Weiss J, Haefeli WE, et al. Dose-dependent bioavailability and CYP3A inhibition contribute to non-linear pharmacokinetics of voriconazole. Clin Pharmacokinet. 2016;55(12):1535–45. https://doi.org/10.1007/s40262-016-0416-1.
Hohmann N, Kreuter R, Blank A, Weiss J, Burhenne J, Haefeli WE, et al. Autoinhibitory properties of the parent but not of the N-oxide metabolite contribute to infusion rate-dependent voriconazole pharmacokinetics. Br J Clin Pharmacol. 2017;83(9):1954–65. https://doi.org/10.1111/bcp.13297.
Upreti VV, Song Y, Wang J, Byon W, Boyd RA, Pursley JM, et al. Effect of famotidine on the pharmacokinetics of apixaban, an oral direct factor Xa inhibitor. Clin Pharmacol. 2013;5:59–66. https://doi.org/10.2147/cpaa.S41999.
Kubitza D, Becka M, Zuehlsdorf M, Mueck W. Effect of food, an antacid, and the H2 antagonist ranitidine on the absorption of BAY 59–7939 (rivaroxaban), an oral, direct factor Xa inhibitor, in healthy subjects. J Clin Pharmacol. 2006;46(5):549–58. https://doi.org/10.1177/0091270006286904.
Moore KT, Plotnikov AN, Thyssen A, Vaccaro N, Ariyawansa J, Burton PB. Effect of multiple doses of omeprazole on the pharmacokinetics, pharmacodynamics, and safety of a single dose of rivaroxaban. J Cardiovasc Pharmacol. 2011;58(6):581–8. https://doi.org/10.1097/FJC.0b013e31822f6c2b.
Mendell J, Lasseter K, Shi M. Effect of esomeprazole on edoxaban pharmacokinetics and pharmacodynamics when administered orally as tablet and as solution. Europace. 2011;13(Suppl 3). (Abstract P1052).
Mendell J, Noveck RJ, Shi M. Pharmacokinetics of the direct factor Xa inhibitor edoxaban and digoxin administered alone and in combination. J Cardiovasc Pharmacol. 2012;60(4):335–41. https://doi.org/10.1097/FJC.0b013e31826265b6.
Rohr BS, Krohmer E, Mikus G, Foerster KI, Burhenne J, Schulz M, Blank A, Haefeli WE. Factor Xa inhibitors exposure increases by five-day, low-dose ritonavir therapy. Br J Pharmacol. 2023;180(Suppl 1):214. https://doi.org/10.1111/bph.16106. (Abstract OC108).
Acknowledgements
The authors would like to thank Marina Weißenborn and Theresa Terstegen for monitoring the study, all lab technicians for their support in the sample analyses, and the clinical team of the trial centre for their contribution to the trial conduct.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. This trial was funded by the Department’s internal resources. No medical writing support was used.
Conflict of interest
Walter E. Haefeli received grants for clinical trials, travel support, and lecture fees from Daiichi Sankyo, the manufacturer of edoxaban, not related to this work. All other authors have no conflicts of interest to declare.
Availability of data and material
The collected and analysed data can be made available upon reasonable request. Part of the data was presented at the 19th World Congress of Clinical Pharmacology, Glasgow, and therefore published as an abstract [66].
Ethical approval and informed consent
The trial protocol (EudraCT 2021-006634-39) was approved by the competent authority (BfArM, Bonn, Germany) and the responsible Ethics Committee of the Medical Faculty of Heidelberg University. All procedures performed in studies involving human participants were in accordance with Good Clinical Practice (ICH-GCP) guidelines, all pertinent German laws, and the ethical standards specified in the applicable version of the declaration of Helsinki. All volunteers gave their written informed consent prior to any study procedures.
Trial registration
The trial was registered at the European Union Drug Regulating Authorities for Clinical Trials (EudraCT-No. 2021-006643-39) and at German Clinical Trial Register with ID DRKS00027838.
Author contributions
WEH and GM proposed the research topic. BSR, AB, EK, WEH, and GM developed the trial protocol. BSR was the responsible study physician and executed the trial. KIF and JB analysed the samples. BSR and GM performed the trial analysis and the statistics. BSR wrote the first draft of the manuscript. All authors discussed and interpreted the results and contributed to the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rohr, B.S., Krohmer, E., Foerster, K.I. et al. Time Course of the Interaction Between Oral Short-Term Ritonavir Therapy with Three Factor Xa Inhibitors and the Activity of CYP2D6, CYP2C19, and CYP3A4 in Healthy Volunteers. Clin Pharmacokinet 63, 469–481 (2024). https://doi.org/10.1007/s40262-024-01350-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-024-01350-x