Abstract
Introduction
Modulation of Factor XIa (FXIa) may provide a novel mechanism for systemic anticoagulation with the potential to improve the risk-benefit profile observed with existing anticoagulants through greater efficacy or a safer bleeding profile. This study assessed the effects of co-administration with strong and moderate CYP3A inhibitors itraconazole and diltiazem, respectively, on the pharmacokinetic and pharmacodynamic properties of milvexian, a Factor XIa inhibitor.
Methods
This was an open-label, non-randomized, two-period crossover study in healthy participants. In period 1, participants received a single oral dose of milvexian (30 mg) on day 1, followed by a washout on days 2 and 3. In period 2, participants received multiple oral doses of itraconazole (200 mg) or diltiazem (240 mg) with a single dose of milvexian.
Results
A total of 28 participants entered the treatment period. Following itraconazole co-administration, milvexian exposure was increased; AUC(0–T), AUC(INF), and C24 were 2.5-, 2.5-, and 3.8-fold higher, while mean Cmax was 28% higher versus milvexian alone. Diltiazem co-administration also increased milvexian exposure; AUC(0–T), AUC(INF), and C24 were 38, 38, and 64% higher, and mean Cmax was 9.6% higher versus milvexian alone. Prolongation of activated partial thromboplastin time was observed with milvexian in a concentration-dependent fashion irrespective of co-administration with itraconazole or diltiazem. Administration of a single dose of milvexian, alone or in combination with itraconazole or diltiazem, was generally safe and well tolerated; there were no deaths or serious adverse events.
Conclusions
A moderate increase in milvexian exposure was observed following co-administration of itraconazole while a minimal increase was seen with diltiazem, consistent with the involvement of CYP3A metabolism and P-glycoprotein in drug absorption/elimination. Milvexian was generally safe and well tolerated in healthy participants.
Trial Registration
The study was registered with ClinicalTrials.gov (NCT02807909; submitted June 17, 2016).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Modulation of Factor XIa (FXIa) may provide a novel mechanism for systemic anticoagulation with an improved risk–benefit profile for bleeding episodes compared with current anticoagulants. |
This study assessed the effects of co-administration with strong and moderate CYP3A inhibitors itraconazole and diltiazem, respectively, on the pharmacokinetic and pharmacodynamic properties of milvexian, a Factor XIa inhibitor. |
What was learned from the study? |
A moderate increase in milvexian exposure was observed following co-administration of itraconazole while a minimal increase was seen with diltiazem, consistent with the involvement of CYP3A metabolism and P-glycoprotein in drug absorption/elimination; concentration-dependent prolongation of activated partial thromboplastin time was observed with milvexian irrespective of co-administration with itraconazole or diltiazem. |
Prolongation of activated partial thromboplastin time was observed with milvexian in a concentration-dependent fashion irrespective of co-administration with itraconazole or diltiazem. |
Milvexian was generally safe and well tolerated in healthy participants. |
Introduction
Antithrombotic therapies are routinely used for the prevention of thrombosis in patients with cardiovascular disease and are increasingly used as a prophylaxis following orthopedic surgeries for the prevention of deep-vein thrombosis and pulmonary embolism [1,2,3,4,5]. Despite a well-demonstrated effectiveness, there are challenges with the use of current therapies, such as residual risk of ischemic events and the risk of bleeding episodes [6,7,8,9]. As such, the development of a novel anticoagulant with an improved risk–benefit profile for bleeding episodes compared with current agents would fulfill an unmet medical need.
The coagulation cascade involves the coordinated activation of plasma proteases, their co-factors, and platelets, through two distinct coagulation pathways, which in total balance clot formation and dissolution [10]. The zymogen factor XI (FXI) is a component of the intrinsic contact pathway and, when activated by thrombin to the protease FXIa, enhances the formation and the stability of clots. FXIa also amplifies thrombin generation when coagulation is initiated by either tissue factor or thrombin, forming a positive feedback loop for coagulation [11, 12]. Notably, epidemiologic data suggest that FXIa plays a greater role in thrombosis than in hemostasis, suggesting that inhibition of FXI or FXIa would be beneficial for thrombosis prevention, without increasing the risk of bleeding in a variety of conditions that predispose individuals to a high risk of thrombotic events [13, 14]. In both clinical and preclinical studies, FXIa inhibitors have been shown to reduce thrombus formation [15,16,17,18].
Milvexian (BMS-986177/JNJ-70033093) is a potent, orally bioavailable small molecule that inhibits FXIa with high affinity and selectivity [19]. In preclinical models of arterial and venous thrombosis, milvexian demonstrated antithrombotic activity while preserving homeostasis [20, 21]. In subsequent clinical studies, milvexian was generally safe and well tolerated in healthy participants and in those with hepatic and renal impairment [22,23,24].
Elimination of milvexian occurs across multiple pathways, including cytochrome P450 (CYP)–mediated metabolism. Preclinical results indicate that milvexian is a substrate of CYP3A4/5 and is also a substrate for P-glycoprotein (P-gp; unpublished data). CYP3A4/5 is involved in the metabolism of a wide range of pharmacological therapies [25]. Therapies that are metabolized by CYP3A4/5 can be impacted by concomitant drugs that are inducers or inhibitors of CYP3A4/5, creating clinically relevant pharmacokinetic (PK) effects [26]. Similarly, P-gp is an ATP-binding cassette transporter that plays a role in drug absorption and disposition [27]. Understanding the effects of CYP3A and/or P-gp inhibition on the PK and pharmacodynamic (PD) properties of milvexian will help to characterize the human metabolic profile and inform dosing strategies in patients taking co-medications that are CYP3A and/or P-gp inhibitors.
This study assessed the effects of strong and moderate CYP3A inhibition with itraconazole and diltiazem, respectively, on the PK and PD properties of milvexian. Itraconazole is considered a strong index inhibitor of CYP3A4/5 [28] and can cause ≥ 10-fold increase in the area under the curve (AUC) of sensitive substrates. Itraconazole is also an inhibitor for P-gp and has demonstrated a > 1.25-fold increase in the AUC of digoxin [28]. Investigation of drug–drug interaction (DDI) of itraconazole with milvexian will model a maximum effect of both CYP3A and P-gp inhibition. The bioavailability of itraconazole (oral solution) is greater under fasted conditions and provides a higher systemic exposure with less variability. As such, participants receiving itraconazole in the current study fasted overnight on the day of co-administration of itraconazole and milvexian. A dosing regimen of 200 mg of itraconazole with a 3-day run-in before co-administration with the substrate was chosen for the sequence, as the lead-in allows for accumulation, greater itraconazole exposure, and a potentially greater degree of CYP3A inhibition [29]. Diltiazem is considered a moderate inhibitor of CYP3A4 and has increased the AUC of certain sensitive CYP3A substrates more than fivefold [28]. To investigate the potential for DDI between moderate CYP3A inhibitors and milvexian, diltiazem was co-administered with milvexian. Diltiazem is well absorbed from the gastrointestinal tract and is subject to an extensive first-pass effect, giving an absolute oral bioavailability (compared to intravenous administration) of about 40% [30]. To evaluate the potential interaction, a 240-mg daily dose of diltiazem was selected for the current study, as this dose is commonly used in clinical practice and has been used in previous studies [30, 31]. Based on preclinical in vitro studies, the potential of milvexian to cause clinically relevant DDIs with substrates of CYP enzymes or P-gp transport at the dose investigated was considered to be low. Therefore, the effect of itraconazole and diltiazem on milvexian, but not the effect of milvexian on itraconazole and diltiazem exposure, was investigated in this study.
Methods
Ethics
The study was conducted in accordance with Good Clinical Practice, as defined by the International Council for Harmonisation, and in accordance with the ethical principles underlying European Union Directive 2001/20/EC and the United States Code of Federal Regulations Title 21, Part 50 (21CFR50) and was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. The protocol, amendments, and participant informed consent received appropriate approval by the Independent Ethics Committee and Institutional Review Board of IntegReview (now Advarra; Columbia, MD, USA) prior to the initiation of the study at the site. Prior to beginning the study, all participants provided written informed consent, including consent for any screening procedures conducted to establish participant eligibility for the study. The study was registered with ClinicalTrials.gov (NCT02807909).
Study Design
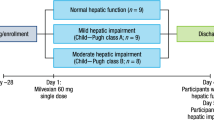
This was an open-label, non-randomized, two-period crossover study performed in two single sequences (itraconazole and diltiazem) in healthy participants (Fig. 1). As the study was non-randomized, enrolled participants, including those not dosed, were assigned sequential subject numbers. The study was conducted at one clinical research center in the United States between July 20, 2016, and September 20, 2016. Participants underwent screening evaluations to determine eligibility within 21 days before study drug administration. Participants received study treatment from authorized study site personnel. In period 1, all participants received a single oral dose of milvexian 30 mg on day 1, followed by a washout on days 2 and 3. In period 2, participants entered either the itraconazole or diltiazem sequence and received either itraconazole 200 mg on days 4 to 6, followed by milvexian 30 mg and itraconazole 200 mg on day 7, and itraconazole 200 mg on days 8 to 11, or diltiazem extended-release (ER) 240 mg on days 4 to 10, milvexian 30 mg and diltiazem ER 240 mg on day 11, and diltiazem ER 240 mg on days 12 to 14. Participants in the itraconazole sequence fasted for at least 8 h prior to dosing on day 7, and milvexian was administered approximately 1 h after itraconazole; participants remained fasted until 4 h after dosing of milvexian. Participants in the diltiazem sequence fasted for at least 8 h prior to dosing on day 11, with no delay in dosing of milvexian; participants remained fasted until 4 h after dosing of milvexian.
Participants
The study included healthy male and female participants as determined by medical and surgical history, physical examination, vital sign measurements, electrocardiogram (ECG) findings, and clinical laboratory evaluations. Participants were aged 18–55 years with a body mass index of 18.0–30.0 kg/m2. Women of childbearing potential or who were breastfeeding were excluded. Other exclusion criteria included, but were not limited to, significant acute or chronic medical illness, or any condition listed as a contraindication in the itraconazole or diltiazem package inserts, as well as evidence of coagulopathy or a history of bleeding. Participants with current or recent (within 3 months of study drug administration) gastrointestinal disease, those with a history of chronic constipation, or those with any major surgery within 12 weeks of study drug administration were also excluded.
Study participants were prohibited from taking corticosteroids, non-steroidal anti-inflammatory compounds, aspirin, or other antiplatelet agents or anticoagulants within 2 weeks of study drug administration. Participants were also prohibited from consuming specific types of cruciferous vegetables and fruits known to interact with CYP450 enzymes (e.g., broccoli, grapefruit juice) within 3 days prior to the first dose of study drug until study discharge and could not consume more than 350 mg of vitamin C.
Safety Assessments
Safety assessments were based on medical review of adverse event (AE) reports and the results of vital sign measurements, ECG measurements, physical examinations, clinical laboratory tests, and fecal occult blood tests. Assessments of clinically significant and non-clinically significant bleeding included, but were not limited to, AE reporting, whole-blood hemoglobin and hematocrit levels, template bleeding times, and/or presence of occult or gross hematuria.
Pharmacokinetic and Pharmacodynamic Assessments
PK analyses were performed to assess the effect of co-administration of itraconazole or diltiazem on the PK of milvexian. PK parameters were derived from the respective plasma concentration versus time data using non-compartmental methods; assessments included maximum observed concentration (Cmax), time of maximum observed concentration (Tmax), area under the plasma concentration–time curve from time 0 to time of last quantifiable concentration (AUC[0–T]), area under the concentration–time curve from time 0 extrapolated to infinite time (AUC[INF]), concentration observed at 24 h postdose (C24), and terminal plasma half-life (T1/2). Activated partial thromboplastin time (aPTT) was assessed as a PD biomarker.
Bioanalytical Assays
During all periods, blood samples were collected for PK and PD analyses (Supplementary Material, Tables S1–S3). Plasma samples were analyzed for milvexian by a validated liquid chromatography tandem mass spectrometry (LC–MS/MS) assay using appropriate calibration curves and quality-control samples that were conducted in compliance with applicable standard procedures. Calibration curves were generated using a weighted linear 1/x2 least-squares regression. The lower limit of quantification for milvexian was 1.00 ng/ml and the upper limit of quantification was 1000 ng/ml. Of the 796 total samples analyzed, 80 were reanalyzed for incurred sample reanalysis (ISR). The ISRs passed the pre-defined acceptance criterion, with 100% of milvexian values having results within 20% of their mean values. Overall precision for the quality control samples, as measured by percent coefficient of variation, was ≤ 3.96% for milvexian. The overall accuracy (% deviation from nominal) as measured by percent relative error, ranged from – 6.63 to 2.67% for milvexian. aPTT was measured with a validated Actin FS assay at Labcorp Colorado Coagulation (Englewood, CO, USA).
Statistical Analyses
The treated population, which included all participants who received at least one dose of study medication, was used for the safety analyses. The evaluable PK population (all subjects in the PK population with adequate PK profiles for accurate estimation of PK parameters) was used for summary statistics and statistical analyses of PK variables. The PD population included all subjects who received at least one dose of study medication and had any available PD biomarker data.
Sample size determination was based on consideration of the precision of the estimate of the geometric mean ratios (GMRs) of Cmax, AUC(0–T), and AUC(INF) of milvexian with and without co-administration of itraconazole or diltiazem.
All plasma milvexian PK data were summarized by treatment sequence using descriptive statistics. A linear mixed model with treatment as a fixed effect and participant as repeated measures was fitted to the log-transformed PK parameters (Cmax, AUC[0–T], AUC[INF], C24) for use in estimation of effects and construction of confidence intervals (CI).
All statistical analyses and calculations were performed using SAS® software (SAS Institute, Inc., Cary, NC, USA; Version 9.2).
Results
Demographics
Of the 95 participants enrolled in the study, 28 entered the treatment period, with 14 participants entering each arm of the study. A total of 26 out of 28 participants (92.9%) completed the study (13 participants in the itraconazole arm and 13 participants in the diltiazem arm). One participant each from the itraconazole and diltiazem sequences was withdrawn from the study during period 2 due to an AE. Table 1 outlines the baseline characteristics of the participants who entered the treatment period.
Safety
Administration of a single dose of milvexian alone and in combination with itraconazole or diltiazem was generally safe and well tolerated, and there were no deaths or serious AEs during the study. Most AEs that occurred in the study were considered likely related to itraconazole or diltiazem treatment, with two participants in each sequence experiencing mild or moderate AEs that were considered to be related to milvexian. In the itraconazole sequence, five of 14 participants (35.7%) reported at least one AE; all were considered mild in intensity and resolved by the end of the study (Table 2). One participant was withdrawn from the study by the investigator after receiving the day 5 dose of itraconazole due to a related AE of drug eruption. Two participants in the itraconazole sequence had a treatment-emergent clinical laboratory test result that met the predefined criteria for a marked abnormality, but none of these were reported as an AE and all were resolved by the end of the study. In the diltiazem sequence, five of 14 participants (35.7%) reported at least one AE during the study; most were considered mild in intensity and resolved by the end of the study (Table 3). One participant (7.1%) experienced a moderate AE of syncope after receiving the day 10 dose of diltiazem and was withdrawn from the study by the investigator. There were no notable clinical laboratory tests, ECGs, vital signs, or physical examination results.
Pharmacokinetics
Figure 2 shows an increase in milvexian exposure during co-administration with itraconazole or diltiazem. With co-administration of itraconazole, AUC(0–T), AUC(INF), and C24 were 2.5-, 2.5-, and 3.8-fold higher, respectively, and mean Cmax was 28% higher compared with milvexian alone (Fig. 3). Similarly, when diltiazem was co-administered with milvexian, there was an increase in milvexian exposure, with AUC(0–T), AUC(INF), and C24 38, 38, and 64% higher, respectively, and mean Cmax 9.6% higher compared with milvexian alone. When milvexian was co-administered with itraconazole or diltiazem, the adjusted GMRs for AUC(0–T), AUC(INF), and C24 were higher compared with administration of milvexian alone. Compared with milvexian alone, mean T1/2 values were approximately 1.5- and 1.1-fold longer with itraconazole and diltiazem co-administration, respectively, while median Tmax values were similar in the two treatment arms. For both treatment sequences, mean milvexian concentrations declined with multi-exponential elimination. Table 4 describes the summary statistics for milvexian PK parameters for both the itraconazole and diltiazem sequences.
Forest plot to assess the effect of itraconazole and diltiazem on milvexian PK parameters. PK pharmacokinetic, GMR geometric mean ratio, CI confidence interval, Cmax maximum observed concentration, AUC(0–T) area under the plasma concentration–time curve from time 0 to time of last quantifiable concentration, AUC(INF) area under the concentration–time curve from time 0 extrapolated to infinite time, C24 concentration observed at 24 h postdose
Pharmacodynamics
Across all post-dose samples, aPTT was prolonged by milvexian administration either alone or when co-administered with itraconazole or diltiazem, with maximal mean aPTT prolongation occurring near Cmax (Fig. 4); the magnitude of aPTT prolongation decreased with declining milvexian concentration. The relationship between aPTT and milvexian concentrations was similar for milvexian alone or in the presence of itraconazole or diltiazem (Supplementary Material, Fig. S1).
Discussion
The aim of the current study was to characterize PK parameters of a single dose of milvexian alone and in combination with either itraconazole or diltiazem in healthy participants, with secondary assessments in measurements of aPTT, safety, and tolerability.
Overall, results from this study were consistent with those of prior preclinical studies that showed that milvexian is a substrate for CYP3A and P-gp. Mean Cmax, AUC(0–T), AUC(INF), and C24 were increased when milvexian was co-administered with a strong (itraconazole) or moderate (diltiazem) CYP3A inhibitor. The impact of a strong CYP3A inhibitor was confirmed to be < 5-fold by the observed increases in milvexian exposure, and the impact of a moderate CYP3A inhibitor was confirmed to be less than 2.5-fold by the increases in milvexian exposure, which suggests that milvexian would not be considered a sensitive CYP3A substrate (i.e., AUC ≥ 5-fold) [28]. The median Tmax of milvexian was not altered by co-administration of itraconazole or diltiazem, but the mean T1/2 was longer with co-administration of itraconazole, which suggests reduced clearance. The slight increase in Cmax (approximately 28%; Fig. 3) was consistent with a modest effect of itraconazole on P-gp or first-pass metabolism. Increases in milvexian exposure after co-administration with itraconazole or diltiazem may not be substantial enough to require dose changes with inhibitors of CYP3A/P-gp; further data from ongoing phase 2 clinical trials are needed to help determine whether milvexian dose adjustments will be required for patients taking concomitant inhibitors of CYP3A and/or P-gp.
The mean aPTT was prolonged after dosing of milvexian in both the itraconazole and diltiazem sequences. In general, higher values of aPTT were associated with higher concentrations of milvexian. Moreover, the apparent relationship between aPTT and milvexian concentrations was similar for milvexian alone or in the presence of itraconazole or diltiazem; this observation was consistent with expectations that itraconazole or diltiazem alone would not have an effect on aPTT.
The results from this study indicate that milvexian has a similar CYP3A and/or P-gp inhibition profile as several of the Factor Xa inhibitors, namely rivaroxaban and apixaban [32]. However, given the potentially improved therapeutic window of milvexian, the same restrictions on co-medications and dose adjustment needed for factor Xa inhibitors may not apply. Further studies, including the radiolabeled mass-balance to characterize the absorption, distribution, metabolism, and excretion (ADME) profile of milvexian, and patient studies to characterize the risk-benefit profile, will help with the comparison of milvexian to factor Xa inhibitors.
The study was somewhat limited by the sample sizes in each panel; however, the CIs around the GMR indicate that a meaningful conclusion can be drawn from these results. Further characterization of the impact of co-medications with CYP3A and/or P-gp inhibition will be generated through development of population PK models and exposure–response analysis from broader patient studies. Of note, both a moderate and a strong CYP inhibitor were selected for investigation in the current study. Future patients may be exposed to both strong and moderate CYP inhibitors, thus necessitating the investigation of the effects of CYP inhibition on the PK of milvexian. In addition, these results will contribute to future modeling efforts. Overall, findings from the current study suggest that a dose adjustment of milvexian may not be necessary for patients receiving concomitant CYP3A and/or P-gp inhibitors.
Conclusion
In conclusion, PK assessments demonstrated an increase in milvexian exposure as a function of co-administration with moderate and strong CYP3A inhibitors, indicating that milvexian is a substrate for CYP3A. Milvexian administration also resulted in concentration-related prolongation of aPTT, with higher aPTT values observed at higher milvexian concentrations. Administration of a single dose of milvexian alone and in combination with itraconazole or diltiazem was generally safe and well tolerated by the healthy participants in this study.
References
Flevas DA, Megaloikonomos PD, Dimopoulos L, Mitsiokapa E, Koulouvaris P, Mavrogenis AF. Thromboembolism prophylaxis in orthopaedics: an update. EFORT Open Rev. 2018;3:136–48.
Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–236.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130:e344-426.
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2016;152:1243–75.
Anderson DR, Morgano GP, Bennett C, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019;3:3898–944.
Bracey A, Shatila W, Wilson J. Bleeding in patients receiving non-vitamin K oral anticoagulants: clinical trial evidence. Ther Adv Cardiovasc Dis. 2018;12:361–80.
Mega JL, Braunwald E, Wiviott SD, et al. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med. 2012;366:9–19.
Eikelboom JW, Connolly SJ, Bosch J, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017;377:1319–30.
Naqvi IA, Kamal AK, Rehman H. Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack. Cochrane Database Syst Rev. 2020;8:CD009716.
ten Cate H, Hackeng TM, Garcia de Frutos P. Coagulation factor and protease pathways in thrombosis and cardiovascular disease. Thromb Haemost. 2017;117:1265–71.
Lowenberg EC, Meijers JC, Monia BP, Levi M. Coagulation factor XI as a novel target for antithrombotic treatment. J Thromb Haemost. 2010;8:2349–57.
Emsley J, McEwan PA, Gailani D. Structure and function of factor XI. Blood. 2010;115:2569–77.
Puy C, Rigg RA, McCarty OJ. The hemostatic role of factor XI. Thromb Res. 2016;141(Suppl 2):S8–11.
Bane CE Jr, Gailani D. Factor XI as a target for antithrombotic therapy. Drug Discov Today. 2014;19:1454–8.
Pollack CV Jr, Kurz MA, Hayward NJ. EP-7041, a Factor XIa inhibitor as a potential antithrombotic strategy in extracorporeal membrane oxygenation: a brief report. Crit Care Explor. 2020;2: e0196.
Sakimoto S, Hagio T, Yonetomi Y, et al. ONO-8610539, an injectable small-molecule inhibitor of blood coagulation Factor XIa, improves cerebral ischemic injuries associated with photothrombotic occlusion of rabbit middle cerebral artery. Presented at the International Stroke Conference; February 21–24, 2017; Houston, Texas.
Thomas D, Kanefendt FS, Schwers S, Unger S, Yassen A, Boxnick S. First evaluation of the safety, pharmacokinetics and pharmacodynamics of BAY 2433334 a small molecule targeting coagulation Factor XIa in healthy young male participants. Presented at the International Society on Thrombosis and Haemostasis (ISTH) Congress; July 12–14, 2020. Virtual.
Weitz JI, Bauersachs R, Becker B, et al. Effect of osocimab in preventing venous thromboembolism among patients undergoing knee arthroplasty: the FOXTROT randomized clinical trial. JAMA. 2020;323:130–9.
Dilger AK, Pabbisetty KB, Corte JR, et al. Discovery of milvexian, a high-affinity, orally bioavailable inhibitor of factor XIa in clinical studies for antithrombotic therapy. J Med Chem. 2022;65:1770–85.
Wang X, Qiu L, Du F, Shukla N, Nawrocki A, Chintala M. Antithrombotic effects of a novel small molecule FXIa inhibitor BMS-986177/JNJ-70033093 in a rabbit AV-shunt model of thrombosis. Poster PB0179. Presented at the International Society on Thrombosis and Haemostasis (ISTH) virtual congress; July 12–14, 2020.
Wong PC, Crain EJ, Bozarth JM, et al. Milvexian, an orally bioavailable, small-molecule, reversible, direct inhibitor of factor XIa: in vitro studies and in vivo evaluation in experimental thrombosis in rabbits. J Thromb Haemost. 2022;20:1030.
Perera V, Abelian G, Li D, et al. Single-dose pharmacokinetics of milvexian in participants with mild or moderate hepatic impairment compared with healthy participants. Clin Pharmacokinet. 2022. https://doi.org/10.1007/s40262-022-01110-9.
Perera V, Wang Z, Luettgen J, et al. First-in-human study of milvexian, an oral, direct, small molecule factor XIa inhibitor. Clin Transl Sci. 2022;15:330–42.
Perera V, Abelian G, Li D, et al. Single-dose pharmacokinetics of milvexian (BMS-986177/JNJ-70033093) in participants with normal renal function and participants with moderate or severe renal impairment. Presented at the American College of Cardiology (ACC) virtual 70th annual session & expo; May 15–17, 2021.
Nebert DW, Russell DW. Clinical importance of the cytochromes P450. Lancet. 2002;360:1155–62.
Frost CE, Byon W, Song Y, et al. Effect of ketoconazole and diltiazem on the pharmacokinetics of apixaban, an oral direct factor Xa inhibitor. Br J Clin Pharmacol. 2015;79:838–46.
Lin JH, Yamazaki M. Role of P-glycoprotein in pharmacokinetics: clinical implications. Clin Pharmacokinet. 2003;42:59–98.
US Food and Drug Administration. Drug development and drug interactions: table of substrates, inhibitors and inducers. Available at: https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers. Accessed 1 Apr 2021.
Liu L, Bello A, Dresser MJ, et al. Best practices for the use of itraconazole as a replacement for ketoconazole in drug–drug interaction studies. J Clin Pharmacol. 2016;56:143–51.
CARDIZEM® LA (diltiazem hydrochloride) Extended-Release Tablets [package insert]. Mississauga, ON, Canada: Biovail Corporation; 2010.
Yeung PK, Hung OR, Pollak PT, Klassen GA. Pharmacokinetics and hemodynamic effects of diltiazem in healthy volunteers: comparing resting with the effect of exercise. Int J Clin Pharmacol Ther. 1999;37:413–6.
Foerster KI, Hermann S, Mikus G, Haefeli WE. Drug–drug interactions with direct oral anticoagulants. Clin Pharmacokinet. 2020;59:967–80.
Acknowledgements
Funding
This study was sponsored by Bristol Myers Squibb. Bristol Myers Squibb and Janssen Global Services, LLC, funded the journal’s Rapid Service Fee.
Medical Writing Assistance
Medical writing support was provided by Alana Simorellis, PhD, of Cello Health Communications/MedErgy, and was funded by Bristol Myers Squibb and Janssen Global Services, LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Vidya Perera, Zhaoqing Wang, Susan Lubin, Lisa J. Christopher, Wei Chen, Sophia Xu, Dietmar Seiffert, Mary DeSouza, and Bindu Murthy contributed to the study design and concept, data analysis and review, or data interpretation; critically reviewed the manuscript for intellectual content; and approved the final manuscript for publication.
Disclosures
Vidya Perera, Zhaoqing Wang, Susan Lubin, Lisa J. Christopher, Wei Chen, Dietmar Seiffert, and Bindu Murthy are full-time employees and may be stockholders of Bristol Myers Squibb. Sophia Xu and Mary DeSouza were full-time employees of Bristol Myers Squibb when the study was conducted.
Compliance with Ethics Guidelines
The study was conducted in accordance with Good Clinical Practice, as defined by the International Council for Harmonisation, and in accordance with the ethical principles underlying European Union Directive 2001/20/EC and the United States Code of Federal Regulations Title 21, Part 50 (21CFR50) and was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. The protocol, amendments, and participant informed consent received appropriate approval by the Independent Ethics Committee and Institutional Review Board of IntegReview (now Advarra; Columbia, MD, USA) prior to the initiation of the study at the site. Prior to beginning the study, all participants provided written informed consent, including consent for any screening procedures conducted to establish participant eligibility for the study. The study was registered with ClinicalTrials.gov (NCT02807909).
Data Availability
The data that support the findings of this study are not publicly available due to privacy or ethical restrictions. Please contact the corresponding author, Vidya Perera, for additional information.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Perera, V., Wang, Z., Lubin, S. et al. Effects of Itraconazole and Diltiazem on the Pharmacokinetics and Pharmacodynamics of Milvexian, A Factor XIa Inhibitor. Cardiol Ther 11, 407–419 (2022). https://doi.org/10.1007/s40119-022-00266-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-022-00266-6