Abstract
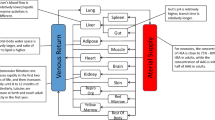
Physiologically based pharmacokinetic modeling and simulation is an important tool for predicting the pharmacokinetics, pharmacodynamics, and safety of drugs in pediatrics. Physiologically based pharmacokinetic modeling is applied in pediatric drug development for first-time-in-pediatric dose selection, simulation-based trial design, correlation with target organ toxicities, risk assessment by investigating possible drug–drug interactions, real-time assessment of pharmacokinetic–safety relationships, and assessment of non-systemic biodistribution targets. This review summarizes the details of a physiologically based pharmacokinetic modeling approach in pediatric drug research, emphasizing reports on pediatric physiologically based pharmacokinetic models of individual drugs. We also compare and contrast the strategies employed by various researchers in pediatric physiologically based pharmacokinetic modeling and provide a comprehensive overview of physiologically based pharmacokinetic modeling strategies and approaches in pediatrics. We discuss the impact of physiologically based pharmacokinetic models on regulatory reviews and product labels in the field of pediatric pharmacotherapy. Additionally, we examine in detail the current limitations and future directions of physiologically based pharmacokinetic modeling in pediatrics with regard to the ability to predict plasma concentrations and pharmacokinetic parameters. Despite the skepticism and concern in the pediatric community about the reliability of physiologically based pharmacokinetic models, there is substantial evidence that pediatric physiologically based pharmacokinetic models have been used successfully to predict differences in pharmacokinetics between adults and children for several drugs. It is obvious that the use of physiologically based pharmacokinetic modeling to support various stages of pediatric drug development is highly attractive and will rapidly increase, provided the robustness and reliability of these techniques are well established.



Similar content being viewed by others
References
Jones HM, Chen Y, Gibson C, Heimbach T, Parrott N, Peters SA, et al. Physiologically based pharmacokinetic modeling in drug discovery and development: a pharmaceutical industry perspective. Clin Pharmacol Ther. 2015;97(3):247–62.
Yoshida K, Budha N, Jin JY. Impact of physiologically based pharmacokinetic models on regulatory reviews and product labels: frequent utilization in the field of oncology. Clin Pharmacol Ther. 2017;101(5):597–602.
Wagner C, Zhao P, Pan Y, Hsu V, Grillo J, Huang SM, et al. Application of physiologically based pharmacokinetic (PBPK) modeling to support dose selection: report of an FDA Public Workshop on PBPK. CPT Pharmacomet Syst Pharmacol. 2015;4(4):226–30.
Maharaj AR, Edginton AN. Physiologically based pharmacokinetic modeling and simulation in pediatric drug development. CPT Pharmacomet Syst Pharmacol. 2014;3(11):1–13.
Grillo JA. Pediatric applications of PBPK modeling and simulation in drug regulatory service: where are we now?. San Diego: American Association of Pharmaceutical Sciences Annual Meeting, 2–6 November 2014.
Zhao P. Application of physiologically-based pharmacokinetic modeling to support dosing recommendations: the US Food and Drug Administration experience; 2016. http://www.ema.europa.eu/docs/en_GB/document_library/Presentation/2016/12/WC500217569.pdf. Accessed 7 May 2018.
Barrett JS, Della Casa Alberighi O, Laer S, Meibohm B. Physiologically based pharmacokinetic (PBPK) modeling in children. Clin Pharmacol Ther. 2012;92(1):40–9.
Della Casa Alberighi O, Barrett JS, Laer S, Meibohm B. Response to “Physiologically based pharmacokinetic modeling at the extremes of age”. Clin Pharmacol Ther. 2013;93(2):149.
Gentry PR, Covington TR, Clewell HJ 3rd. Evaluation of the potential impact of pharmacokinetic differences on tissue dosimetry in offspring during pregnancy and lactation. Regul Toxicol Pharmacol. 2003;38(1):1–16.
Pelekis M, Gephart LA, Lerman SE. Physiological-model-based derivation of the adult and child pharmacokinetic intraspecies uncertainty factors for volatile organic compounds. Regul Toxicol Pharmacol. 2001;33(1):12–20.
Price K, Haddad S, Krishnan K. Physiological modeling of age-specific changes in the pharmacokinetics of organic chemicals in children. J Toxicol Environ Health A. 2003;66(5):417–33.
Edginton AN. Knowledge-driven approaches for the guidance of first-in-children dosing. Paediatr Anaesth. 2011;21(3):206–13.
Mouksassi MS, Marier JF, Cyran J, Vinks AA. Clinical trial simulations in pediatric patients using realistic covariates: application to teduglutide, a glucagon-like peptide-2 analog in neonates and infants with short-bowel syndrome. Clin Pharmacol Ther. 2009;86(6):667–71.
Huang W, Nakano M, Sager J, Ragueneau-Majlessi I, Isoherranen N. Physiologically based pharmacokinetic model of the CYP2D6 probe atomoxetine: extrapolation to special populations and drug–drug interactions. Drug Metab Dispos. 2017;45(11):1156–65.
Jones H, Rowland-Yeo K. Basic concepts in physiologically based pharmacokinetic modeling in drug discovery and development. CPT Pharmacomet Syst Pharmacol. 2013;14(2):e63.
Maharaj AR, Barrett JS, Edginton AN. A workflow example of PBPK modeling to support pediatric research and development: case study with lorazepam. AAPS J. 2013;15(2):455–64.
ICRP. Basic anatomical and physiological data for use in radiological protection: reference values. ICRP Publication 89. Amsterdam: Elsevier Science; 2002.
Alcorn J, McNamara PJ. Ontogeny of hepatic and renal systemic clearance pathways in infants: part II. Clin Pharmacokinet. 2002;41(13):1077–94.
Khalil F, Laer S. Physiologically based pharmacokinetic modeling: methodology, applications, and limitations with a focus on its role in pediatric drug development. J Biomed Biotechnol. 2011;2011:907461.
Miyagi SJ, Long-Boyle JR. Predicting pediatric drug disposition: present and future directions of pediatric physiologically-based pharmacokinetics. Drug Metab Lett. 2015;9(2):80–7.
Leong R, Vieira ML, Zhao P, Mulugeta Y, Lee CS, Huang SM, et al. Regulatory experience with physiologically based pharmacokinetic modeling for pediatric drug trials. Clin Pharmacol Ther. 2012;91(5):926–31.
Henthorn TK, Avram MJ, Krejcie TC, Shanks CA, Asada A, Kaczynski DA. Minimal compartmental model of circulatory mixing of indocyanine green. Am J Physiol. 1992;262(3 Pt 2):H903–10.
Cao Y, Jusko WJ. Applications of minimal physiologically-based pharmacokinetic models. J Pharmacokinet Pharmacodyn. 2012;39(6):711–23.
Maharaj AR, Edginton AN. Examining small intestinal transit time as a function of age: is there evidence to support age-dependent differences among children? Drug Metab Dispos. 2016;44(7):1080–9.
Bonner JJ, Vajjah P, Abduljalil K, Jamei M, Rostami-Hodjegan A, Tucker GT, et al. Does age affect gastric emptying time? A model-based meta-analysis of data from premature neonates through to adults. Biopharm Drug Dispos. 2015;36(4):245–57.
Maharaj AR, Edginton AN, Fotaki N. Assessment of age-related changes in pediatric gastrointestinal solubility. Pharm Res. 2016;33(1):52–71.
Maharaj AR, Gonzalez D, Cohen-Wolkowiez M, Hornik CP, Edginton AN. Improving pediatric protein binding estimates: an evaluation of alpha1-acid glycoprotein maturation in healthy and infected subjects. Clin Pharmacokinet. 2018;57(5):577–89.
McNamara PJ, Alcorn J. Protein binding predictions in infants. AAPS Pharm Sci. 2002;4(1):E4.
Prasad B, Gaedigk A, Vrana M, Gaedigk R, Leeder JS, Salphati L, et al. Ontogeny of hepatic drug transporters as quantified by LC–MS/MS proteomics. Clin Pharmacol Ther. 2016;100(4):362–70.
Edginton AN, Shah B, Sevestre M, Momper JD. The integration of allometry and virtual populations to predict clearance and clearance variability in pediatric populations over the age of 6 years. Clin Pharmacokinet. 2013;52(8):693–703.
Rhodin MM, Anderson BJ, Peters AM, Coulthard MG, Wilkins B, Cole M, et al. Human renal function maturation: a quantitative description using weight and postmenstrual age. Pediatr Nephrol. 2009;24(1):67–76.
Edginton AN, Schmitt W, Voith B, Willmann S. A mechanistic approach for the scaling of clearance in children. Clin Pharmacokinet. 2006;45(7):683–704.
Hayton WL. Maturation and growth of renal function: dosing renally cleared drugs in children. AAPS Pharm Sci. 2000;2(1):E3.
Lu H, Rosenbaum S. Developmental pharmacokinetics in pediatric populations. J Pediatr Pharmacol Ther. 2014;19(4):262–76.
Krekels EH, Neely M, Panoilia E, Tibboel D, Capparelli E, Danhof M, et al. From pediatric covariate model to semiphysiological function for maturation: part I-extrapolation of a covariate model from morphine to zidovudine. CPT Pharmacomet Syst Pharmacol. 2012;3(1):e9.
European Medicines Agency. Guideline on the qualification and reporting of physiologically based pharmacokinetic (PBPK) modelling and simulation (draft). London: European Medicines Agency; 2016.
Strougo A, Eissing T, Yassen A, Willmann S, Danhof M, Freijer J. First dose in children: physiological insights into pharmacokinetic scaling approaches and their implications in paediatric drug development. J Pharmacokinet Pharmacodyn. 2012;39(2):195–203.
Vinks AA, Emoto C, Fukuda T. Modeling and simulation in pediatric drug therapy: application of pharmacometrics to define the right dose for children. Clin Pharmacol Ther. 2015;98(3):298–308.
Wagner C, Zhao P, Pan Y, Hsu V, Grillo J, Huang S, et al. Application of physiologically based pharmacokinetic (PBPK) modeling to support dose selection: report of an FDA Public Workshop on PBPK. CPT Pharmacomet Syst Pharmacol. 2015;4(4):226–30.
Allegaert K, van den Anker JN. Clinical pharmacology in neonates: small size, huge variability. Neonatology. 2014;105(4):344–9.
Ginsberg G, Hattis D, Russ A, Sonawane B. Physiologically based pharmacokinetic (PBPK) modeling of caffeine and theophylline in neonates and adults: implications for assessing children’s risks from environmental agents. J Toxicol Environ Health A. 2004;67(4):297–329.
Bjorkman S. Prediction of drug disposition in infants and children by means of physiologically based pharmacokinetic (PBPK) modelling: theophylline and midazolam as model drugs. Br J Clin Pharmacol. 2005;59(6):691–704.
Lukacova V, Goelzer P, Reddy M, Greig G, Reigner B, Parrott N. A physiologically based pharmacokinetic model for ganciclovir and its prodrug valganciclovir in adults and children. AAPS J. 2016;18(6):1453–63.
Parrott N, Davies B, Hoffmann G, Koerner A, Lave T, Prinssen E, et al. Development of a physiologically based model for oseltamivir and simulation of pharmacokinetics in neonates and infants. Clin Pharmacokinet. 2011;50(9):613–23.
Johnson TN, Rostami-Hodjegan A, Tucker GT. Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet. 2006;45(9):931–56.
Jiang XL, Zhao P, Barrett JS, Lesko LJ, Schmidt S. Application of physiologically based pharmacokinetic modeling to predict acetaminophen metabolism and pharmacokinetics in children. CPT Pharmacomet Syst Pharmacol. 2013;16(2):e80.
Boberg M, Vrana M, Mehrotra A, Pearce RE, Gaedigk A, Bhatt DK, et al. Age-dependent absolute abundance of hepatic carboxylesterases (CES1 and CES2) by LC–MS/MS proteomics: application to PBPK modeling of oseltamivir in vivo pharmacokinetics in infants. Drug Metab Dispos. 2017;45(2):216–23.
Emoto C, Fukuda T, Johnson TN, Adams DM, Vinks AA. Development of a pediatric physiologically based pharmacokinetic model for sirolimus: applying principles of growth and maturation in neonates and infants. CPT Pharmacomet Syst Pharmacol. 2015;4(2):e17.
Mahmood I. Dosing in children: a critical review of the pharmacokinetic allometric scaling and modelling approaches in paediatric drug development and clinical settings. Clin Pharmacokinet. 2014;53(4):327–46.
Jorga K, Chavanne C, Frey N, Lave T, Lukacova V, Parrott N, et al. Bottom-up meets top-down: complementary physiologically based pharmacokinetic and population pharmacokinetic modeling for regulatory approval of a dosing algorithm of valganciclovir in very young children. Clin Pharmacol Ther. 2016;100(6):761–9.
Emoto C, Fukuda T, Johnson TN, Neuhoff S, Sadhasivam S, Vinks AA. Characterization of contributing factors to variability in morphine clearance through PBPK modeling implemented with OCT1 transporter. CPT Pharmacomet Syst Pharmacol. 2017;6(2):110–9.
Edginton AN, Schmitt W, Willmann S. Development and evaluation of a generic physiologically based pharmacokinetic model for children. Clin Pharmacokinet. 2006;45(10):1013–34.
Herigon JC, Hersh AL, Gerber JS, Zaoutis TE, Newland JG. Antibiotic management of Staphylococcus aureus infections in US children’s hospitals, 1999–2008. Pediatrics. 2010;125(6):e1294–300.
Hornik CP, Wu H, Edginton AN, Watt K, Cohen-Wolkowiez M, Gonzalez D. Development of a pediatric physiologically-based pharmacokinetic model of clindamycin using opportunistic pharmacokinetic data. Clin Pharmacokinet. 2017;56(11):1343–53.
Laughon MM, Benjamin DK Jr. Mechanisms to provide safe and effective drugs for children. Pediatrics. 2014;134(2):e562–3.
Gonzalez D, Melloni C, Yogev R, Poindexter BB, Mendley SR, Delmore P, et al. Use of opportunistic clinical data and a population pharmacokinetic model to support dosing of clindamycin for premature infants to adolescents. Clin Pharmacol Ther. 2014;96(4):429–37.
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52(3):285–92.
Reeves DS, Holt HA, Phillips I, King A, Miles RS, Paton R, et al. Activity of clindamycin against Staphylococcus aureus and Staphylococcus epidermidis from four UK centres. J Antimicrob Chemother. 1991;27(4):469–74.
Online L-C. Pediatric and neonatal. Hudson (OH): Lexi-Comp, Inc.; 2012.
Register F, editor. List of drugs for which pediatric studies are needed. Bethesda, MD: National Institutes of Health; 2003. p. 2789–90.
Chamberlain JM, Capparelli EV, Brown KM, Vance CW, Lillis K, Mahajan P, et al. Pharmacokinetics of intravenous lorazepam in pediatric patients with and without status epilepticus. J Pediatr. 2012;160(4):667–672.e2.
MacDonald A, Scarola J, Burke JT, Zimmerman JJ. Clinical pharmacokinetics and therapeutic drug monitoring of sirolimus. Clin Ther. 2000;22 Suppl. B:B101–21.
Hammill AM, Wentzel M, Gupta A, Nelson S, Lucky A, Elluru R, et al. Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer. 2011;57(6):1018–24.
Michaels MG, Greenberg DP, Sabo DL, Wald ER. Treatment of children with congenital cytomegalovirus infection with ganciclovir. Pediatr Infect Dis J. 2003;22(6):504–9.
Schmidt GM, Horak DA, Niland JC, Duncan SR, Forman SJ, Zaia JA. A randomized, controlled trial of prophylactic ganciclovir for cytomegalovirus pulmonary infection in recipients of allogeneic bone marrow transplants; The City of Hope-Stanford-Syntex CMV Study Group. N Engl J Med. 1991;324(15):1005–11.
Treanor JJ, Hayden FG, Vrooman PS, Barbarash R, Bettis R, Riff D, et al. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: a randomized controlled trial: US Oral Neuraminidase Study Group. JAMA. 2000;283(8):1016–24.
Gabbay E, Fraser J, McNeil K. Review of bosentan in the management of pulmonary arterial hypertension. Vasc Health Risk Manag. 2007;3(6):887–900.
Rosenzweig EB, Ivy DD, Widlitz A, Doran A, Claussen LR, Yung D, et al. Effects of long-term bosentan in children with pulmonary arterial hypertension. J Am Coll Cardiol. 2005;46(4):697–704.
Zisowsky J, Géhin M, Kusic-Pajic A, Krause A, Beghetti M, Dingemanse J. Pediatric development of bosentan facilitated by modeling and simulation. Pediatr Drugs. 2017;19(2):121–30.
Donnelly M, Zametkin AJ, Rapoport JL, Ismond DR, Weingartner H, Lane E, et al. Treatment of childhood hyperactivity with desipramine: plasma drug concentration, cardiovascular effects, plasma and urinary catecholamine levels, and clinical response. Clin Pharmacol Ther. 1986;39(1):72–81.
Wilens TE, Biederman J, Prince J, Spencer TJ, Faraone SV, Warburton R, et al. Six-week, double-blind, placebo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry. 1996;153(9):1147–53.
Wenzel-Seifert K, Wittmann M, Haen E. QTc prolongation by psychotropic drugs and the risk of Torsade de Pointes. Dtsch Arztebl Int. 2011;108(41):687–93.
Riddle MA, Geller B, Ryan N. Another sudden death in a child treated with desipramine. J Am Acad Child Adolesc Psychiatry. 1993;32(4):792–7.
Samant TS, Lukacova V, Schmidt S. Development and qualification of physiologically based pharmacokinetic models for drugs with atypical distribution behavior: a desipramine case study. CPT Pharmacomet Syst Pharmacol. 2017;6(5):315–21.
Seroquel XR prescribing information. US Food and Drug Adminstration; 2017.
Johnson TN, Zhou D, Bui KH. Development of physiologically based pharmacokinetic model to evaluate the relative systemic exposure to quetiapine after administration of IR and XR formulations to adults, children and adolescents. Biopharm Drug Dispos. 2014;35(6):341–52.
Johnson TN, Rostami-Hodjegan A. Resurgence in the use of physiologically based pharmacokinetic models in pediatric clinical pharmacology: parallel shift in incorporating the knowledge of biological elements and increased applicability to drug development and clinical practice. Paediatr Anaesth. 2011;21(3):291–301.
Rioux N, Waters NJ. Physiologically based pharmacokinetic modeling in pediatric oncology drug development. Drug Metab Dispos. 2016;44(7):934–43.
Sager JE, Yu J, Ragueneau-Majlessi I, Isoherranen N. Physiologically based pharmacokinetic (PBPK) modeling and simulation approaches: a systematic review of published models, applications, and model verification. Drug Metab Dispos. 2015;43(11):1823–37.
Tylutki Z, Mendyk A, Polak S. Mechanistic physiologically based pharmacokinetic (PBPK) model of the heart accounting for inter-individual variability: development and performance verification. J Pharm Sci. 2018;107(4):1167–77.
Ke A, Barter Z, Rowland-Yeo K, Almond L. Towards a best practice approach in PBPK modeling: case example of developing a unified efavirenz model accounting for induction of CYPs 3A4 and 2B6. CPT Pharmacomet Syst Pharmacol. 2016;5(7):367–76.
Author information
Authors and Affiliations
Contributions
VY, JR, XL, JR, SK, and CS developed the review and wrote the initial draft of the manuscript. Additionally, all authors contributed substantively to the review and revision of the final versions.
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the preparation of this article.
Conflict of interest
Venkata Yellepeddi, Joseph Rower, Xiaoxi Liu, Shaun Kumar, Jahidur Rashid, and Catherine M. T. Sherwin have no conflicts of interest directly relevant to the content of this article.
Rights and permissions
About this article
Cite this article
Yellepeddi, V., Rower, J., Liu, X. et al. State-of-the-Art Review on Physiologically Based Pharmacokinetic Modeling in Pediatric Drug Development. Clin Pharmacokinet 58, 1–13 (2019). https://doi.org/10.1007/s40262-018-0677-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-018-0677-y