Abstract
Background
Magnetic resonance imaging (MRI) with Gadolinium 1,4,7,10-tetraazacyclododecane-N′,N″,N′′′,N″″-tetraacetic acid (Gd-DOTA) enables assessment of myocardial perfusion during first-pass of the contrast agent, while increased retention can signify areas of myocardial infarction (MI). We studied whether Gallium-68-labeled analog, 68Ga-DOTA, can be used to assess myocardial perfusion on positron emission tomography/computed tomography (PET/CT) in rats, comparing it with 11C-acetate.
Methods
Rats were studied with 11C-acetate and 68Ga-DOTA at 24 hours after permanent ligation of the left coronary artery or sham operation. One-tissue compartmental models were used to estimate myocardial perfusion in normal and infarcted myocardium. After the PET scan, hearts were sectioned for autoradiographic detection of 68Ga-DOTA distribution.
Results
11C-acetate PET showed perfusion defects and histology showed myocardial necrosis in all animals after coronary ligation. Kinetic modeling of 68Ga-DOTA showed significantly higher k1 values in normal myocardium than in infarcted areas. There was a significant correlation (r = 0.82, P = 0.001) between k1 values obtained with 68Ga-DOTA and 11C-acetate. After 10 minutes of tracer distribution, the 68Ga-DOTA concentration was significantly higher in the infarcted than normal myocardium on PET imaging and autoradiography.
Conclusions
Our results indicate that acute MI can be detected as reduced perfusion, as well as increased late retention of 68Ga-DOTA.
Similar content being viewed by others
Introduction
Gadolinium (Gd)-labeled chelates are widely used magnetic resonance imaging (MRI) contrast agents. Cardiac MRI with Gd chelates enables assessment of myocardial perfusion during the first-pass of the contrast agent and detection of myocardial infarction (MI) using the delayed-enhancement technique.1,2,3,4,5,–6 Delayed-enhancement imaging is based on the accumulation and retention of contrast agent in the infarcted myocardium due to the loss of cell membrane integrity, and hence reflects increased extracellular tissue volume.7
Positron emission tomography/computed tomography (PET/CT) perfusion imaging enables quantification of myocardial blood flow (MBF) and myocardial flow reserve (MFR). As it does not require an on-site cyclotron, rubidium-82 (82Rb) chloride is the most widely used tracer for assessment of myocardial perfusion with PET. Quantification of myocardial perfusion on PET with the cyclotron products nitrogen-13-labeled ammonia (13N-ammonia) and oxygen-15-labeled water (15O-water) has been well validated.8,9 Another validated tracer for myocardial perfusion imaging is the 11C-acetate used as a control in this study.10
Gallium-68-labeled 1,4,7,10-tetraazacyclododecane-N′,N″,N′′′,N″″-tetraacetic acid (68Ga-DOTA) chelate has similar kinetics to the Gd-DOTA used in MRI,11 and is feasible for imaging of blood flow.12,13 Our research group found evidence that imaging of increased accumulation of 68Ga-DOTA PET may be useful for detecting conditions associated with increased blood flow and vascular permeability, such as adenosine-induced increase in myocardial perfusion and inflammatory lesions.12 This novel approach to PET perfusion imaging is generator-based and provides an opportunity for imaging centers distant to a radiochemistry unit to detect and quantify blood flow. 68Ga is a positron-emitting radionuclide that is readily available from a 68Germanium (68Ge)/68Ga generator system possessing a 1 year life span (68Ge T1/2 = 270.8 days). In contrast to most positron-emitting radionuclides that require a cyclotron for production, the 68Ge/68Ga generator provides low-cost and easy access to a positron-emitting radionuclide. However, it is not known whether 68Ga-DOTA PET can be used to detect abnormal myocardial perfusion and cell necrosis associated with MI.
In this study, we aimed to validate 68Ga-DOTA PET imaging measurement of myocardial perfusion, comparing it with 11C-acetate, and comparing the kinetics of 68Ga-DOTA between normal and infarcted myocardium in rats. Translation to a clinical setting should be feasible for 68Ga-DOTA, as Gd-DOTA is already in clinical use (trade names Artirem®, Dotarem®).14
METHODS
Animal Model
The study protocol was approved by the national Animal Experiment Board in Finland and the Regional State Administrative Agency for Southern Finland, and carried out in compliance with the European Union directives relating to the conduct of animal experimentation. In total, 12 male Sprague-Dawley rats were used. MI was induced by permanent ligation of the left coronary artery (LCA), as previously described.15,16,17,–18 Briefly, 0.2 mg·kg−1 buprenorphine (Temgesic; Schering-Plough, Espoo, Finland) was administered intramuscularly for analgesia prior to operation. Anesthesia was induced by a combination of inhaled isoflurane and subcutaneous injection of 10 mg·kg−1 xylazine (Rompun; Orion Pharma, Espoo, Finland) and 90 mg·kg−1 ketamine (Ketaminol; Orion Pharma). Body temperature was maintained using a heating pad. The rats were intubated and connected to a rodent ventilator (TOPO dual mode ventilator; Kent Scientific, Torrington, CT, USA).19
The heart was exposed by a left lateral thoracotomy of the fourth intercostal space, the pericardium was opened, and the LCA was ligated near to its origin. Ligation was confirmed visually as a pale appearance of the myocardium at risk. The ribs, muscle layer, and skin were tightly sewn with a dissolving string. The anesthesia was reversed after the operation with an intramuscular injection of 1 mg·kg−1 atipamezole (Antisedan; Orion Pharma). The sham operation consisted of all the same procedures except that the suture was not tightened around the LCA. Operative mortality in both coronary ligation and sham groups was ~ 25%, as previously described.15
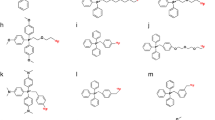
Radiochemistry
68Ga-DOTA synthesis was performed as previously described.12 Briefly, 68Ga was obtained from a 68Ge/68Ga generator (Eckert&Ziegler, Valencia, CA, USA) by elution with 0.1 M HCl. DOTA chelate (35 nmol in aqua; Macrocyclics, Dallas, TX, USA) was added, and the mixture was incubated at + 100°C for 15 minutes. Radiochemical purity of the final product was analyzed by high-performance liquid chromatography (HPLC) using μBondapak column and trifluoroacetic acid/acetonitrile/H3PO4 gradient. Retention time for 68Ga-DOTA was 3.9 ± 0.1 minutes and for unbound 68Ga 14.6 ± 0.2 minutes.
11C-Acetate was synthesized as previously described.20 For quality assessment, the final product was analyzed by HPLC.
PET/CT
The rats that survived surgery were imaged using small-animal PET/CT (Inveon Multimodality; Siemens Medical Solutions, Knoxville, TN, USA) at 24 ± 4 hours (n = 6) after coronary ligation or at 24 ± 4 hours (n = 6) after the sham operation. The rats were anesthetized using 1.5% isoflurane, and their body temperature was maintained with a heating pad throughout the imaging. First, a 10-minutes 11C-acetate PET (27 ± 12 MBq) was performed to evaluate myocardial perfusion and to localize the infarcted area. Then, after five half-lives of 11C, 68Ga-DOTA imaging was performed. To evaluate the myocardial kinetics of the tracer, the rats in the ligation group were injected with a bolus of 29 ± 3 MBq of 68Ga-DOTA and PET imaged for 30 minutes. Both 11C-acetate and 68Ga-DOTA PET acquisitions were started prior to injection to catch the first-pass peak of the imaging tracer. Images were collected according to the following time frames: 30 × 3 seconds, 9 × 10 seconds, 4 × 30 seconds, 5 × 60 seconds, and 4 × 300 seconds. Immediately after PET, 200 μL of intravascular iodinated eXIATM160XL contrast agent (Binitio Biomedical Inc, Ottawa, ON, Canada) was injected and high-resolution CT was acquired to delineate the myocardial borders. Sham-operated rats were injected with 14 ± 1 MBq of 68Ga-DOTA and PET/CT imaged as described above.
Alignment of PET and CT images was automatically performed and confirmed visually according to anatomical landmarks. Image analysis was performed using Carimas v.2.8 software (Turku PET Centre, Turku, Finland). Regions of interest (ROIs) were defined on the high-resolution CT image to delineate the infarcted myocardium (verified by 11C-acetate perfusion images) and remote myocardium. Results are reported as standardized uptake values (SUVs).
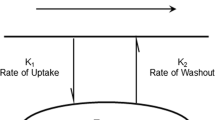
The kinetic parameters for both 68Ga-DOTA and 11C-acetate were determined using the Carimas 2.8 heart plugin modeling option. For 68Ga-DOTA, an input function was obtained from the left ventricle (LV), which was identified using high-resolution contrast-enhanced CT. The uptake rate (k1) was estimated assuming a one-tissue compartmental model (1TCM), as we previously validated.12 Modeling for 11C-acetate was performed using a tracer-specific mode readily available in the Carimas software.15 An 11C-acetate k1 polar map was used to determine specific segments in the normal areas in the septum and infarcted area in the anterior or anterolateral LV wall, with these same segments being used to compare the 68Ga-DOTA kinetics. In addition to perfusion, the myocardial infarct area was determined as the percent of non-viable tissue according to the k1 polar maps. The polar maps were normalized to the highest k1 value in the viable part of the myocardium, which was set as the 100% k1 value, and a cutoff of < 60% of the k1 value was used to determine the infarcted area.21
Autoradiography
A subgroup of MI rats (n = 3) were further analyzed to determine the microscopic distribution of the 68Ga-DOTA at 30 minutes post-injection of the tracer. The LV was frozen in cooled isopentane and sliced into serial transverse cryosections of 8 and 20 μm at 1 mm intervals (five to six intervals per heart) from apex to base. Distribution of 68Ga-DOTA in the infarcted and remote myocardium was analyzed by autoradiography of tissue sections. Air-dried sections were apposed to an imaging plate (BAS-TR2025; Fuji Photo Film Co. Tokyo, Japan), and after more than two radionuclide half-lives, the plates were scanned with a Fuji BAS-5000 analyzer (internal resolution of 25 μm). Tracer accumulation was measured as counts per area (photostimulated luminescence per square millimeter, PSL/mm2) with TINA software v.2.1 (Raytest Isotopenmessgeräte, GmbH, Straubenhardt, Germany).
After co-registration of autoradiography and histological images, ROIs were defined in the infarcted and remote areas of the LV. The background area count densities were subtracted from the image data. After autoradiography, the serial LV cryosections were stained with hematoxylin-eosin (HE) for histology.
Statistical Analysis
All results are expressed as mean ± standard deviation (SD). Correlation coefficients were computed using linear regression analysis. Student’s t-test was used for comparison between two groups. A P value less than 0.05 was considered statistically significant. All statistical analyses were conducted using Origin 7.5 software (Microcal Software, Inc., Northampton, MA, USA).
RESULTS
Radiochemistry
The radiochemical purity of 68Ga-DOTA was 99% ± 0.3% (n = 4), and the molar activity was 9.1 ± 3.5 MBq·nmol−1 (n = 4). The radiochemical purity of 11C-acetate was consistently > 99%.
Tracer Kinetics in the Infarcted vs. Normal Myocardium
68Ga-DOTA radioactivity concentration declined rapidly after initial peak in the remote and infarcted areas, but some remaining radioactivity was visible in the infarcted area 10 minutes after injection of the 68Ga-DOTA tracer. Infarct area was also visualized as a defect area with 11C-acetate in every MI animal (Fig. 1A). An example PET/CT image of the remaining radioactivity in the infarcted rat myocardium 30 minutes post-injection of 68Ga-DOTA is shown in Figure 1B.
Representative coronal PET/CT images of (A) 11C-acetate (sum image 30-90 seconds post-injection), (B) 68Ga-DOTA (sum image 20-30 minutes post-injection), and (C) combined 11C-acetate (blue) and 68Ga-DOTA (green) in a rat with coronary ligation. Note the high 11C-acetate uptake in the infero-posterior wall of the LV and defective uptake in the anterior wall subtended by the ligated coronary artery. 68Ga-DOTA is present in the defect area at this time point
A peak was detected in the myocardial uptake of 68Ga-DOTA within 20 seconds post-injection (Fig. 2B). At this time point, the peak in the MI rat group was higher in the remote myocardium (SUV: 8.8 ± 0.93) than in the infarcted area (SUV: 3.8 ± 0.67, P = 0.0014). At the end of the 30 minutes imaging study (25-30 minutes post-injection), the infarcted area (SUV: 1.13 ± 0.13) showed significantly higher uptake than the remote myocardium (SUV: 0.93 ± 0.087, P = 0.023; Fig. 2B). There was no difference between the anterior wall (SUV: 0.67 ± 0.13) and the septum (SUV: 0.72 ± 0.10) in the sham-operated animals (P = 0.11). The MI/remote ratio (1.2 ± 0.18) in the MI group was significantly higher than the anterior wall/septum ratio (0.93 ± 0.087) in the sham-operated control group (P = 0.0049).
(A) Radioactivity concentration as a function of time (time-activity curves) for myocardial 68Ga-DOTA uptake in rats with coronary ligation (mean, n = 6). Radioactivity peaks were higher in the remote myocardium than in the infarcted area in the initial distribution phase of the 68Ga-DOTA. (B) Tracer uptake in the heart at the end of the 30 minutes imaging study in MI and sham-operated animals demonstrates late phase contrast enhancement in the infarcted myocardium
Determination of MBF
68Ga-DOTA k1 values reflecting myocardial perfusion were calculated from the PET image data by application of a 1TCM. Polar maps demonstrated higher k1 values in the normal myocardium than infarcted myocardium using either 68Ga-DOTA or 11C-acetate (Fig 3A, 3B). Remote/MI ratios of k1 values were 4.7 ± 0.6 (P < 0.001) for 11C-acetate and 4.3 ± 1.0 (P < 0.001) for 68Ga-DOTA (Fig. 3D). Regression analysis showed that the 68Ga-DOTA values were closely comparable to the 11C-acetate values (y = 0.59x + 0.38, r = 0.82, P = 0.0010, Fig. 3D). The ratios of the remote to MI k1 values showed no significant differences between the 11C-acetate and 68Ga-DOTA k1. In the sham-operated animals, the ratio of k1 values for 68Ga-DOTA in the corresponding areas in the septum and anterior wall was 1.0 ± 0.06 (P = 0.8, Fig. 3d). When the threshold of 60% of maximum flow was used to define viable myocardium, the perfusion defect size was slightly overestimated with 68Ga-DOTA (64% ± 3.9%) in comparison with 11C-acetate (57% ± 1.8%), but this difference was not significant (P = 0.13).
Polar maps of k1 values obtained with (A) 11C-acetate and (B) 68Ga-DOTA in a rat with coronary ligation. (C) Representation of segments used in MBF quantification. Segments marked red were used for quantification of MBF on infarcted area whereas areas in green were used for quantification of remote area. Selected segment varied from animal to animal according localization of infarcted area. Same segment was used for both 11C-acetate and 68Ga-DOTA MBF quantification per animal. (D) Quantification of the remote/MI ratio of k1 values in MI rats imaged with 11C-acetate and 68Ga-DOTA, and a sham-operated animal imaged with 68Ga-DOTA, reveals comparable kinetics. (E) Correlation between 68Ga-DOTA and 11C-acetate k1 values is statistically significant. y = ax + b is the linear regression formula used to fit the k1 data of 11C-acetate and 68Ga-DOTA
Autoradiography
A representative autoradiograph of myocardial 68Ga-DOTA uptake at 30 minutes post-injection is shown in Figure 4. Infarcted area, which was confirmed by histology (Fig. 4A), demonstrated a necrotic core surrounded by granulated tissue that was seen in the anterior or anterolateral LV wall in all animals that underwent surgical coronary ligation. There was a local increase in 68Ga-DOTA tracer accumulation in the anterolateral wall of the LV, which was co-localized with the histologically infarcted area in the rats with coronary ligation. In the rats with coronary ligation, the average 68Ga-DOTA radioactivity concentration in the infarcted area was 4.4-fold higher than in the remote myocardium (28 ± 1.5 vs. 6.5 ± 0.7 PSL·mm2, P = 0.0015).
(A) Hematoxylin-eosin staining of the left ventricle shows defective myocardium that co-localizes with higher radioactivity concentration. (B) Autoradiography of the left ventricle myocardium 30 minutes post-injection of 68Ga-DOTA in a rat with myocardial infarction due to coronary ligation shows higher retention of 68Ga-DOTA than in remote myocardium. (C) Quantification of autoradiography analysis shows significantly higher radioactivity concentration in the ligated area in comparison with remote myocardium
DISCUSSION
Gd based MRI is safe, accurate, and practical for the imaging of patients with cardiac events.5,6,–7 Both first-pass perfusion imaging and delayed contrast enhancement have been utilized for this chelate in cardiac MRI. In the current study, our investigations provide evidence that 68Ga-DOTA has similar potential for the measurement of MBF, as well as showing a delayed washout in acutely infarcted myocardium. The 68Ga-DOTA works in this setting as a dual-function tracer. In the first-pass and early time frames it can be used to model blood perfusion in the remote myocardium. It is only at later time points when the tracer is accumulated in the defect area due to increased extracellular space. The PET perfusion imaging using tracer kinetic modeling allowed quantitative measurements of absolute MBF. This method is suitable for several applications in research and clinical diagnostics. In rat models, the 68Ga-DOTA chelate is comparable to two gold-standards of perfusion imaging, 15O-water, as we have previously shown,12 and now with 11C-acetate. This novel tool would offer the opportunity to in vivo image blood perfusion at imaging sites more distant from cyclotron facility.
Elevated radioactivity concentration was seen in the infarcted areas in the later time points of the 68Ga-DOTA imaging, with this probably reflecting the delayed washout kinetics of the tracer distributed in the increased extracellular space, i.e., delayed contrast enhancement. This finding is analogous to the late-enhancement imaging used in contrast-enhanced cardiac MRI, which allows visualization of the infarcted myocardium where cells have lost their membrane integrity or myocardium has been replaced by fibrosis. Higher radioactivity concentration in the infarcted areas was confirmed by autoradiography of the LV tissue sections.
We previously showed the feasibility of 68Ga-DOTA chelate for the detection of increased perfusion in inflammation foci,12 detecting higher 68Ga-DOTA signal at the site of inflamed skin/muscle in comparison with healthy muscle, thereby suggesting that inflammation-induced changes in blood flow and vascular permeability can be detected with 68Ga-DOTA. In addition, we were able to detect increased perfusion in healthy rat heart following induction of pharmacological hyperemia caused by intravenous infusion of adenosine. The MFR measured with 68Ga-DOTA was comparable to that measured with 15O-water, which is a tracer used for PET imaging of MBF.22,23,–24
The in vivo imaging of MBF is difficult in small animals due to the limited spatial and temporal resolution of PET scanners, partial-volume effects (PVEs), spill over, and the high positron energy of 68Ga. However, studies have indicated the possibility of imaging myocardial perfusion in rat heart with several different tracers.10,23,24,–25 Tracers that have been successfully used for the measurement of myocardial infarct size in small animals include 2-deoxy-2-18F-fluoro-D-glucose (18F-FDG), which is a marker of viable myocardium.25,26,–27 Here, we demonstrated that 68Ga-DOTA has potential for the measurement of myocardial perfusion in small animals. The results were validated using 11C-acetate, which is well established for the imaging of myocardial perfusion.10 The quantitative analysis method of 11C-acetate is based on fitting 1TCM parameters K1, k2, and Vb to the tissue curves covering the whole 10-minutes scan, with input function derived from the LV. The model parameter K1 represents perfusion, k2 represents rate of oxidative metabolism, and Vb is the fractional volume of blood in the tissue. The model is essentially the same as is applied for the analysis of 15O-water and 68Ga-DOTA. Usage of K1 from 11C-acetate for assessing myocardial perfusion (in addition to oxidative metabolism) has been previously validated against gold-standard 15O-water method in rats10 and in humans,28,29 and also against 13N-ammonia. In addition to 11C-acetate, it would have been possible to use 15O-water as a control. However, due to 2-minutes half-life of 15O, the transfer of 15O-water from the cyclotron/radiochemistry unit to the animal imaging facility was not feasible due to the long distance between sites. During this study 13N-ammonia was not available at our center.
In this study, we obtained the input function from the LV cavity on dynamic PET images. A direct comparison of the 68Ga-DOTA radioactivity concentration obtained from blood samples and PET images would be a valuable approach in a larger animal model (e.g., pigs), which would allow multiple blood samples to be taken from the same animal throughout the PET imaging. A dedicated small-animal PET/CT scanner was used to image the animals in this study, and even though it provided good resolution and we had the anatomical CT references to aid in ROI drawing, the structures being imaged were quite small (less than 10 mm in diameter). The in vivo imaging of small structures such as rat myocardium may therefore be affected by PVE, which might have influenced the in vivo quantitative PET data. When PVE is present, the apparent pixel values in PET images may be influenced by surrounding high pixel values. Other factors, such as the reconstruction algorithm and filter, scanner sensitivity, and scan duration, may also affect the accuracy of imaging data, and require evaluation.
CONCLUSION
Our results indicate that 68Ga-DOTA is a potential tracer for evaluating myocardial resting perfusion in small animals. Acute MI can be detected as both reduced perfusion and increased late retention of the tracer. The myocardial kinetics of 68Ga-DOTA assessed from the early distribution of the chelate reflected myocardial perfusion, while delayed contrast enhancement was demonstrated at later time points, showing delayed washout in the infarcted area with an increase in the extracellular space. This approach may provide an opportunity to conduct quantitative PET perfusion imaging studies in centers distant from the cyclotron unit. Further analyses will be needed to evaluate the potential of 68Ga-DOTA kinetic analysis for differentiating viable and non-viable myocardial areas in a clinical setting.
NEW KNOWLEDGE GAINED
This study demonstrates that 68Ga-DOTA PET has potential for in vivo quantification of MBF.
Abbreviations
- 68Ga-DOTA:
-
Gallium-68-labeled 1,4,7,10-tetraazacyclododecane-N′,N″,N′′′,N″″-tetraacetic acid
- LCA:
-
Left coronary artery
- LV:
-
Left ventricle
- MBF:
-
Myocardial blood flow
- MI:
-
Myocardial infarction
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- ROI:
-
Region of interest
- SUV:
-
Standardized uptake value
- 1TCM:
-
One-tissue compartmental model
References
Gibbons RJ, Valeti US, Araoz PA, Jaffe AS. The quantification of infarct size. J Am Coll Cardiol. 2004;19:1533–42.
Dilsizian V, Bonow RO. Current diagnostic techniques of assessing myocardial viability in patients with hibernating and stunned myocardium. Circulation. 1993;87:1–20.
Pereira RS, Prato FS, Wisenberg G, Sykes J, Yvorchuk KJ. The use of Gd-DTPA as a marker of myocardial viability in reperfused acute myocardial infarction. Int J Cardiovasc Imaging. 2001;17:395–404.
Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–53.
Saraste A, Nekolla S, Schwaiger M. Contrast-enhanced magnetic resonance imaging in the assessment of myocardial infarction and viability. J Nucl Cardiol. 2008;15:105–17.
Neilan TG, Farhad H, Mayrhofer T, Shah RV, Dodson JA, Abbasi SA, et al. Late Gadolinium enhancement among survivors of sudden cardiac arrest. J Am Coll Cardiol Img. 2015;8:414–23.
Saeed M, Van TA, Krug R, Hetts SW, Wilson MW. Cardiac MR imaging: current status and future direction. Cardiovasc Diagn Ther. 2015;4:290–310.
Saraste A, Kajander S, Han C, Nesterov SV, Knuuti J. PET: Is myocardial flow quantification a clinical reality? J Nucl Cardiol. 2012;19:1044–59.
Knuuti J, Bengel FM. Positron emission tomography and molecular imaging. Heart. 2008;94:360–7.
Croteau E, Gascon S, Bentourkia M, Langlois R, Rousseau JA, Lecomte R, et al. [11C]Acetate rest-stress protocol to assess myocardial perfusion and oxygen consumption reserve in a model of congestive heart failure in rats. Nucl Med Biol. 2012;39:287–94.
Bousquet JC, Saini S, Stark DD, Hahn PF, Nigam M, Wittenberg J, et al. Gd-DOTA: characterization of a new paramagnetic complex. Radiology. 1988;166:693–8.
Autio A, Saraste A, Kudomi N, Saanijoki T, Johansson J, Liljenbäck H, et al. Assessment of blood flow with 68Ga-DOTA PET in experimental inflammation: a validation study using 15O-water. Am J Nucl Med Mol Imaging. 2014;6:571–9.
Velasco C, Mateo J, Santos A, Mota-Cobian A, Herranz F, Pellico J, et al. Assessment of regional pulmonary blood flow using 68Ga-DOTA PET. EJNMMI Res. 2017;7:7.
Herborn CU, Honold E, Wolf M, Kemper J, Kinner S, Adam G, et al. Clinical safety and diagnostic value of the gadolinium chelate gadoterate meglumine (Gd-DOTA). Invest Radiol. 2007;42:58–62.
Kiugel M, Dijkgraaf I, Kytö V, Helin S, Liljenbäck H, Saanijoki T, et al. Dimeric [68Ga]DOTA-RGD peptide targeting αvβ 3 integrin reveals extracellular matrix alterations after myocardial infarction. Mol Imaging Biol. 2014;16:793–801.
Pfeffer MA, Pfeffer JM, Fishbein MC, Fletcher PJ, Spadaro J, Kloner RA, et al. Myocardial infarct size and ventricular function in rats. Circ Res. 1979;44:503–12.
Sherif HM, Saraste A, Weidl E, Weber AW, Higuchi T, Reder S, et al. Evaluation of a novel 18F-labeled positron-emission tomography perfusion tracer for the assessment of myocardial infarct size in rats. Circ Cardiovasc Imaging. 2009;2:77–84.
Palojoki E, Saraste A, Eriksson A, Pulkki K, Kallajoki M, Voipio-Pulkki LM, et al. Cardiomyocyte apoptosis and ventricular remodeling after myocardial infarction in rats. Am J Physiol Heart Circ Physiol. 2001;280:H2726–31.
Jou IM, Tsai YT, Tsai CL, Wu MH, Chang HY, Wang NS. Simplified rat intubation using a new oropharyngeal intubation wedge. J Appl Physiol. 2000;89:1766–70.
Seppälä J, Seppänen M, Arponen E, Lindholm P, Minn H. Carbon-11 acetate PET/CT based dose escalated IMRT in prostate cancer. Radiother Oncol. 2009;93:234–40.
Tarkia M, Stark C, Haavisto M, Kentala R, Vähäsilta T, Savunen T, et al. Cardiac remodeling in a new pig model of chronic heart failure: Assessment of left ventricular functional, metabolic, and structural changes using PET, CT, and echocardiography. J Nucl Cardiol. 2015;22:655–65.
Kajander SA, Joutsiniemi E, Saraste M, Pietilä M, Ukkonen H, Saraste A, et al. Clinical value of absolute quantification of myocardial perfusion with 15O-water in coronary artery disease. Circ Cardiovasc Imaging. 2011;4:678–84.
Croteau E, Bénard F, Bentourkia M, Rousseau J, Paquette M, Lecomte R. Quantitative myocardial perfusion and coronary reserve in rats with 13N-ammonia and small animal PET: impact of anesthesia and pharmacologic stress agents. J Nucl Med. 2004;45:1924–30.
Herrero P, Kim J, Sharp TL, Engelbach JA, Lewis JS, Gropler RJ, et al. Assessment of myocardial blood flow using 15O-water and 1-11C-acetate in rats with small-animal PET. J Nucl Med. 2006;47:477–85.
Stegger L, Hoffmeier AN, Schafers KP. Accurate noninvasive measurement of infarct size in mice with high-resolution PET. J Nucl Med. 2006;47:1837–44.
Higuchi T, Nekolla ST, Jankaukas A. Characterization of normal and infarcted rat myocardium using a combination of small-animal PET and clinical MRI. J Nucl Med. 2007;48:288–94.
Kudo T, Fukuchi K, Annala AJ. Noninvasive measurement of myocardial activity concentrations and perfusion defect sizes in rats with a new small-animal positron emission tomograph. Circulation. 2002;106:118–23.
Sciacca RR, Akinboboye O, Chou RL, Epstein S, Bergmann SR. Measurement of myocardial blood flow with PET using 1-11C-acetate. J Nucl Med. 2001;42:63–70.
Timmer SA, Lubberink M, Germans T, Götte MJ, ten Berg JM, ten Cate FJ, et al. Potential of [11C]acetate for measuring myocardial blood flow: Studies in normal subjects and patients with hypertrophic cardiomyopathy. J Nucl Cardiol. 2010;17:264–75.
Acknowledgments
Open access funding provided by University of Turku (UTU) including Turku University Central Hospital. The authors thank Erica Nyman for tissue sectioning and histological staining, Aake Honkaniemi for technical expertise in animal imaging studies, and Timo Kattelus for helping with figures.
Disclosure
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding The studies were conducted within the Finnish Centre of Excellence in Cardiovascular and Metabolic Diseases supported by the Academy of Finland, the University of Turku, the Turku University Hospital, and the Åbo Akademi University. In addition, this study was financially supported by the Sigrid Jusélius Foundation and Finnish Foundation for Cardiovascular Research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Autio, A., Uotila, S., Kiugel, M. et al. 68Ga-DOTA chelate, a novel imaging agent for assessment of myocardial perfusion and infarction detection in a rodent model. J. Nucl. Cardiol. 27, 891–898 (2020). https://doi.org/10.1007/s12350-019-01752-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-019-01752-6