Abstract
Increasing evidence has confirmed that the nervous system shows innate and adaptive immunity, which also participates in nerve damage. This study aimed to explore the neuroimmune imbalance induced by arsenic and its possible mechanism. Mice were exposed to NaAsO2 (0, 5, 10, 25, and 50 mg/L) for 1 month by drinking water. Y-maze and Morris water maze tests revealed that arsenic impaired learning and memory. The optical density of Evans blue showed a marked dose-dependent increase in the brain, and the mRNA and protein levels of the BBB tight junctions (TJs), occludin at 25 and 50 mg/L arsenic, and claudin-5 at 50 mg/L arsenic, were markedly decreased in the cerebral cortex. Arsenic downregulated occludin and claudin-5 mRNA expression at 50 mg/L and protein expression at 25 and 50 mg/L in the hippocampus. Immunohistochemical staining showed that 50 mg/L arsenic increased corticocerebral and hippocampal CD3+ T, CD4+ T, and CD8+ T cells; CD4 and CD8 proteins were increased with 25 and 50 mg/L arsenic. Arsenic decreased the corticocerebral and hippocampal Th1, Th17, and regulatory Treg transcription factors T-bet, Rorγt, and Foxp3 and the cytokine IFN-γ, IL-17, and TGF-β mRNA levels and increased the Th2 transcription factor GATA3 and cytokine IL-4 mRNA levels. Moreover, arsenic enhanced the expression of nuclear factor E2-related factor (Nrf2) and its downstream enzymes heme oxygenase-1 (HO-1) and glutathione-S-transferase (GST). In conclusion, these results demonstrate that arsenic exposure induces BBB dysfunction and T lymphocyte infiltration and affects CD4+ T lymphocyte differentiation, which may be associated with Nrf2 activation.
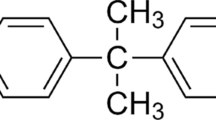
Graphical Abstract







Similar content being viewed by others
Data Availability
No data were used to support this study.
Abbreviations
- As:
-
Arsenic
- BBB:
-
Blood‒brain barrier
- CNS:
-
Central nervous system
- Foxp3:
-
Forkhead box p3
- GATA3:
-
GATA‒binding protein 3
- GCLM:
-
Glutamate‒cysteine ligase regulatory subunit
- GST:
-
Glutathione S‒transferase
- HO‒1:
-
Heme oxygenase-1
- IFN‒γ:
-
Interfern gamma
- IL-17:
-
Interleukin 17
- NQO1:
-
NAD(P)H:quinone oxidoreductase 1
- Nrf2:
-
Nuclear factor‒erythroid 2-related factor 2
- Rorγt:
-
Retinoic acid‒related orphan receptor
- T‒bet:
-
T-box transcription factor
- TGF‒β:
-
Transforming growth factor‒β
- Th1:
-
T helper 1
- TJs:
-
Tight junction proteins
- Treg cell:
-
Regulatory T cells
References
Chen QY, Costa M (2021) Arsenic: a global environmental challenge. Annu Rev Pharmacol Toxicol 61:47–63. https://doi.org/10.1146/annurev-pharmtox-030220-013418
LiLi S, Wei BK, Wang J, Dong G, Wang X (2019) Taurine supplementation ameliorates arsenic-induced hepatotoxicity and oxidative stress in mouse. Adv Exp Med Biol 1155:463–470. https://doi.org/10.1007/978-981-13-8023-5_43
Xu G, Gu Y, Yan N, Li Y, Sun L, Li B (2021) Curcumin functions as an anti-inflammatory and antioxidant agent on arsenic-induced hepatic and kidney injury by inhibiting MAPKs/NF-κB and activating Nrf2 pathways. Environ Toxicol 36:2161–2173. https://doi.org/10.1002/tox.23330
Kushwaha R, Mishra J, Tripathi S, Raza W, Mandrah K, Roy SK, Bandyopadhyay S (2018) Arsenic attenuates heparin-binding EGF-like growth factor/EGFR signaling that promotes matrix metalloprotease 9-dependent astrocyte damage in the developing rat brain. Toxicol Sci 162:406–428. https://doi.org/10.1093/toxsci/kfx264
Virk D, Kumar A, Jaggi AS, Singh N (2021) Ameliorative role of rolipram, PDE-4 inhibitor, against sodium arsenite-induced vascular dementia in rats. Environ Sci Pollut Res Int 28:63250–63262. https://doi.org/10.1007/s11356-021-15189-3
Wang X, Huang X, Zhou L, Chen J, Zhang X, Xu K, Huang Z, He M, Shen M, Chen X, Tang B, Shen L, Zhou Y (2021) Association of arsenic exposure and cognitive impairment: a population-based cross-sectional study in China. Neurotoxicology 82:100–107. https://doi.org/10.1016/j.neuro.2020.11.009
He Q, Chen B, Chen S, Zhang M, Duan L, Feng X, Chen J, Zhou L, Chen L, Duan Y (2021) MBP-activated autoimmunity plays a role in arsenic-induced peripheral neuropathy and the potential protective effect of mecobalamin. Environ Toxicol 36:1243–1253. https://doi.org/10.1002/tox.23122
Moore CL, Flanigan TJ, Law CD, Loukotková L, Woodling KA, da Costa GG, Fitzpatrick SC, Ferguson SA (2019) Developmental neurotoxicity of inorganic arsenic exposure in Sprague-Dawley rats. Neurotoxicol Teratol 72:49–57. https://doi.org/10.1016/j.ntt.2019.01.007
Rodríguez-Barranco M, Gil F, Hernández AF, Alguacil J, Lorca A, Mendoza R, Gómez I, Molina-Villalba I, González-Alzaga B, Aguilar-Garduño C, Rohlman DS, Lacasaña M (2016) Postnatal arsenic exposure and attention impairment in school children. Cortex 74:370–382. https://doi.org/10.1016/j.cortex.2014.12.018
Ikegami A, Wake H (2021) Microglial regulation of blood brain barrier, the neuro-immunological interface. Brain and nerve 73:913–919. https://doi.org/10.11477/mf.1416201861
Pan J, Ma N, Zhong J, Yu B, Wan J, Zhang W (2021) Age-associated changes in microglia and astrocytes ameliorate blood-brain barrier dysfunction. Mol Ther Nucleic Acids 26:970–986. https://doi.org/10.1016/j.omtn.2021.08.030
Sweeney MD, Kisler K, Montagne A, Toga AW, Zlokovic BV (2018) The role of brain vasculature in neurodegenerative disorders. Nat Neurosci 21:1318–1331. https://doi.org/10.1038/s41593-018-0234-x
Huang Y, Chen S, Luo Y, Han Z (2020) Crosstalk between inflammation and the BBB in stroke. Curr Neuropharmacol 18:1227–1236. https://doi.org/10.2174/1570159X18666200620230321
Zuniga EI, Macal M, Lewis GM, Harker JA (2015) Innate and adaptive immune regulation during chronic viral infections. Annu Rev Virol 2:573–597. https://doi.org/10.1146/annurev-virology-100114-055226
Yin X, Chen S, Eisenbarth SC (2021) Dendritic cell regulation of T helper cells. Annu Rev Immunol 39:759–790. https://doi.org/10.1146/annurev-immunol-101819-025146
Yan J, Yang X, Han D, Feng J (2016) Tanshinone IIA attenuates experimental autoimmune encephalomyelitis in rats. Mol Med Rep 14:1601–1609. https://doi.org/10.3892/mmr.2016.5431
Guo P, Chen S, Li D, Zhang J, Luo J, Zhang A, Yu D, Bloom MS, Chen L, Chen W (2020) SFPQ is involved in regulating arsenic-induced oxidative stress by interacting with the miRNA-induced silencing complexes. Environ Pollut 261:114160. https://doi.org/10.1016/j.envpol.2020.114160
Song C, Heping H, Shen Y, Jin S, Li D, Zhang A, Ren X, Wang K, Zhang L, Wang J, Shi D (2020) AMPK/p38/Nrf2 activation as a protective feedback to restrain oxidative stress and inflammation in microglia stimulated with sodium fluoride. Chemosphere 244:125495. https://doi.org/10.1016/j.chemosphere.2019.125495
Lin G, Sun Y, Long J, Sui X, Yang J, Wang Q, Wang S, He H, Luo Y, Qiu Z, Wang Y (2020) Involvement of the Nrf2-Keap1 signaling pathway in protection against thallium-induced oxidative stress and mitochondrial dysfunction in primary hippocampal neurons. Toxicol Lett 319:66–73. https://doi.org/10.1016/j.toxlet.2019.11.008
Lin X, Tawch S, Wong HT, Roy S, Gaudino S, Castillo P, Elsegeiny W, Wakabayashi N, Oury TD, Pociask D, Chen K, McLinskey N, Melville P, Syritsyna O, Coyle P, Good M, Awasthi A, Kolls JK, Kumar P (2021) Nrf2 through aryl hydrocarbon receptor regulates IL-22 response in CD4+ T cells. J Immunol 206:1540–1548. https://doi.org/10.4049/jimmunol.1900656
Zhang Y, Duan X, Li J, Zhao S, Li W, Zhao L, Li W, Nie H, Sun G, Li B (2016) Inorganic arsenic induces NRF2-regulated antioxidant defenses in both cerebral cortex and hippocampus in vivo. Neurochem Res 41:2119–2128. https://doi.org/10.1007/s11064-016-1927-8
Calabrese V, Sultana R, Scapagnini G, Guagliano E, Sapienza M, Bella R, Kanski J, Pennisi G, Mancuso C, Stella AM, Butterfield DA (2006) Nitrosative stress, cellular stress response, and thiol homeostasis in patients with Alzheimer’s disease. Antioxid Redox Sign 8:1975–1986. https://doi.org/10.1089/ars.2006.8.1975
Wang Y, Yang X, Yu H, Wang H, Qi Y, Geng M (2020) Effects of arsenic exposure on D-serine metabolism in the hippocampus of offspring mice at different developmental stages. Arch Toxicol 94:77–87. https://doi.org/10.1007/s00204-019-02616-1
Li J, Guo Y, Duan X, Li B (2020) Tissue- and region-specific accumulation of arsenic species, especially in the brain of mice, after long-term arsenite exposure in drinking water. Biol Trace Elem Res 198:168–176. https://doi.org/10.1007/s12011-020-02033-x
Gudapati K, Singh A, Clarkson-Townsend D, Phillips SQ, Douglass A, Feola AJ, Allen RS (2020). Behavioral assessment of visual function via optomotor response and cognitive function via Y-maze in diabetic rats Jove-J Vis Exp. https://doi.org/10.3791/61806.10.3791/61806
Buckinx A, Van Schuerbeek A, Bossuyt J, Allaoui W, Van Den Herrewegen Y, Smolders I, De Bundel D (2021) Exploring refinement strategies for single housing of male C57BL/6JRj mice: effect of cage divider on stress-related behavior and hypothalamic-pituitary-adrenal-axis activity. Front Behav Neurosci 15:743959. https://doi.org/10.3389/fnbeh.2021.743959
Niikura M, Komatsuya K, Inoue SI, Matsuda R, Asahi H, Inaoka DK, Kita K, Kobayashi F (2017) Suppression of experimental cerebral malaria by disruption of malate:quinone oxidoreductase. Malar J 16:247. https://doi.org/10.1186/s12936-017-1898-5
Rom S, Heldt NA, Gajghate S, Seliga A, Reichenbach NL, Persidsky Y (2020) Hyperglycemia and advanced glycation end products disrupt BBB and promote occludin and claudin-5 protein secretion on extracellular microvesicles. Sci Rep 10:7274. https://doi.org/10.1038/s41598-020-64349-x
Mónaco NM, Bartos M, Dominguez S, Gallegos C, Bras C, Esandi MDC, Bouzat C, Giannuzzi L, Minetti A, Gumilar F (2018) Low arsenic concentrations impair memory in rat offpring exposed during pregnancy and lactation: role of α7 nicotinic receptor, glutamate and oxidative stress. Neurotoxicology 67:37–45. https://doi.org/10.1016/j.neuro.2018.04.011
Jou YC, Wang SC, Dai YC, Chen SY, Shen CH, Lee YR, Chen LC, Liu YW (2019) Gene expression and DNA methylation regulation of arsenic in mouse bladder tissues and in human urothelial cells. Oncol Rep 42:1005–1016. https://doi.org/10.3892/or.2019.7235
Hu Y, Yu C, Yao M, Wang L, Liang B, Zhang B, Huang X, Zhang A (2018) The PKCδ-Nrf2-ARE signalling pathway may be involved in oxidative stress in arsenic-induced liver damage in rats. Environ Toxicol Pharmacol 62:79–87. https://doi.org/10.1016/j.etap.2018.05.012
Dixit S, Mehra RD, Dhar P (2020) Effect of α-lipoic acid on spatial memory and structural integrity of developing hippocampal neurons in rats subjected to sodium arsenite exposure. Environ Toxicol Pharmacol 75:103323. https://doi.org/10.1016/j.etap.2020.103323
Singh V, Kushwaha S, Gera R, Ansari JA, Mishra J, Dewangan J, Patnaik S, Ghosh D (2019) Sneaky entry of IFNγ through arsenic-induced leaky blood-brain barrier reduces CD200 expression by microglial pro-inflammatory cytokine. Mol Neurobiol 56:1488–1499. https://doi.org/10.1007/s12035-018-1155-0
Yu Y, Wang C, Zhang X, Zhu J, Wang L, Ji M, Zhang Z, Ji XM, Wang SL (2020) Perfluorooctane sulfonate disrupts the blood brain barrier through the crosstalk between endothelial cells and astrocytes in mice. Environ Pollut 256:113429. https://doi.org/10.1016/j.envpol.2019.113429
Li Y, Du X, Zhao Y, Wang J, Wang J (2021) Fluoride can damage the spleen of mice by perturbing Th1/Th2 cell balance. Biol Trace Elem Res 199:1493–1500. https://doi.org/10.1007/s12011-020-02264-y
Chang L, Hu L, Wei C, Zhang H, Liu S (2020) Chinese medicine Tongxinluo capsule protects against blood-brain barrier disruption after ischemic stroke by inhibiting the low-density lipoprotein receptor-related protein 1 pathway in mice. J Stroke Cerebrovasc Dis 29:105071. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105071
Manthari RK, Tikka C, Ommati MM, Niu R, Sun Z, Wang J, Zhang J, Wang J (2018) Arsenic induces autophagy in developmental mouse cerebral cortex and hippocampus by inhibiting PI3K/Akt/mTOR signaling pathway: involvement of blood-brain barrier’s tight junction proteins. Arch Toxicol 92:3255–3275. https://doi.org/10.1007/s00204-018-2304-y
Wang Y, Zhao H, Liu Y, Guo M, Tian Y, Huang P, Xing M (2021) Arsenite induce neurotoxicity of common carp: involvement of blood brain barrier, apoptosis and autophagy, and subsequently relieved by zinc (II) supplementation. Aquat Toxicol 232:105765. https://doi.org/10.1016/j.aquatox.2021.105765
DiSano KD, Linzey MR, Welsh NC, Meier JS, Pachner AR, Gilli F (2020) Isolating central nervous system tissues and associated meninges for the downstream analysis of immune cells. Jove-J Vis Exp. https://doi.org/10.3791/61166.10.3791/61166
Lye SH, Chtarbanova S (2018) Drosophila as a model to study brain innate immunity in health and disease. Int J Mol Sci 19:3922. https://doi.org/10.3390/ijms19123922
Katz Sand I (2015) Classification, diagnosis, and differential diagnosis of multiple sclerosis. Curr Opin Neurol 28:193–205. https://doi.org/10.1097/WCO.0000000000000206
DiStasio MM, Nagakura I, Nadler MJ, Anderson MP (2019) T lymphocytes and cytotoxic astrocyte blebs correlate across autism brains. Ann Neurol 86:885–898. https://doi.org/10.1002/ana.25610
Zhang X, Liu W, Yuan J, Zhu H, Yang Y, Wen Z, Chen Y, Li L, Lin J, Feng H (2017) T lymphocytes infiltration promotes blood-brain barrier injury after experimental intracerebral hemorrhage. Brain Res 1670:96–105. https://doi.org/10.1016/j.brainres.2017.06.019
Park ES, Uchida K, Nakayama H (2013) Th1-, Th2-, and Th17-related cytokine and chemokine receptor mRNA and protein expression in the brain tissues, T cells, and macrophages of dogs with necrotizing and granulomatous meningoencephalitis. Vet Pathol 50:1127–1134. https://doi.org/10.1177/0300985813488957
Cañete JD, Martínez SE, Farrés J, Sanmartí R, Blay M, Gómez A, Salvador G, Muñoz-Gómez J (2000) Differential Th1/Th2 cytokine patterns in chronic arthritis: interferon gamma is highly expressed in synovium of rheumatoid arthritis compared with seronegative spondyloarthropathies. Ann Rheum Dis 59:263–268. https://doi.org/10.1136/ard.59.4.263
Li L, Cheng SQ, Guo W, Cai ZY, Sun YQ, Huang XX, Yang J, Ji J, Chen YY, Dong YF, Cheng H, Sun XL (2021) Oridonin prevents oxidative stress-induced endothelial injury via promoting Nrf-2 pathway in ischaemic stroke. J Cell Mol Med 25:9753–9766. https://doi.org/10.1111/jcmm.16923
Yin L, Ouyang D, Lin L, Xin X, Ji Y (2019) Salidroside regulates imbalance of Th17/Treg and promotes ischemic tolerance by targeting STAT-3 in cerebral ischemia-reperfusion injury. Arch Med Sci 17:523–534. https://doi.org/10.5114/aoms.2019.85349
Zhang Y, Liu M, Sun H, Yin K (2015) Matrine improves cognitive impairment and modulates the balance of Th17/Treg cytokines in a rat model of Aβ1-42-induced Alzheimer’s disease. Cent Eur J Immunol 40:411–419. https://doi.org/10.5114/ceji.2015.56961
Saha S, Buttari B, Panieri E, Profumo E, Saso L (2020) An overview of Nrf2 signaling pathway and its role in inflammation. Molecules 25:5474. https://doi.org/10.3390/molecules25225474
Bi Z, Zhang Q, Fu Y, Wadgaonkar P, Zhang W, Almutairy B, Xu L, Rice M, Qiu Y, Thakur C, Chen F (2020) Nrf2 and HIF1α converge to arsenic-induced metabolic reprogramming and the formation of the cancer stem-like cells. Theranostics 10:4134–4149. https://doi.org/10.7150/thno.42903
Kansanen E, Kuosmanen SM, Leinonen H, Levonen AL (2013) The Keap1-Nrf2 pathway: mechanisms of activation and dysregulation in cancer. Redox Biol 1:45–49. https://doi.org/10.1016/j.redox.2012.10.001
Zagorski JW, Turley AE, Freeborn RA, VanDenBerg KR, Dover HE, Kardell BR, Liby KT, Rockwell CE (2018) Differential effects of the Nrf2 activators tBHQ and CDDO-Im on the early events of T cell activation. Biochem Pharmacol 147:67–76. https://doi.org/10.1016/j.bcp.2017.11.005
Funding
This study was supported by grants from the National Natural Science Foundation of China (NSFC) (no. 81803180 and 81803200), the Basic Research Project of Liaoning Provincial Department of Education Youth Project (no. LJKQZ2021173), the Shenyang Middleyounger Scientific and Technological Innovation Support Plan (no. RC190479 and RC200238), the Liaoning Province Key Research and Development Program Guidance (no. 2019JH8/10300047), the Shenyang Science and Technology Plan Project Social Governance Science and Technology Special Project (no. 21-108-9-11), and the Science and Technology Innovation Fund of Shenyang Medical College (no. Y20210513).
Author information
Authors and Affiliations
Contributions
N.Y. and H.J. designed the study; J.W. and Z.L. performed the study; K.J.X., Q.W., J.W.Z., and L.S. analyzed the data; X.K.C. and X.X.D. wrote and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
Animal use was approved by Animal Use and Care Committee at Shenyang Medical College (protocol number: SYYXY2020082801), and all experiments were performed in accordance with the approved guidelines and regulations.
Consent for Publication
All authors of the manuscript have read and agreed to its content.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, N., Jing, H., Wang, J. et al. Arsenic Induces Blood‒Brain Barrier Disruption and Regulates T Lymphocyte Subpopulation Differentiation in the Cerebral Cortex and Hippocampus Associated with the Nrf2 Pathway In Vivo. Biol Trace Elem Res 201, 3981–3993 (2023). https://doi.org/10.1007/s12011-022-03500-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03500-3