Abstract
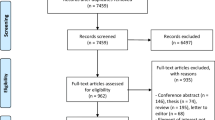
The homeostasis of trace elements is essential to regulate different aspects of the immune system and might play important roles in systemic lupus erythematosus (SLE). However, epidemiological evidences that compared the level of essential trace elements in SLE patients and healthy controls (HCs) did not reach a consensus. This was the first meta-analysis to comprehensively assess the level of zinc (Zn), copper (Cu), iron (Fe), and selenium (Se) in SLE and HCs. PubMed, Embase, and Web of Science were systematically searched until April 2022 to find relevant literatures. The PRISMA statement 2020 was followed to make sure the quality of reporting a meta-analysis. The outcomes were assessed by pooled standardized mean difference (SMD) and 95% confidence intervals (CIs). Finally, eleven articles with 1262 subjects were included in the meta-analysis. Significantly lower levels of Zn (SMD = −0.709; 95% CI: −1.173, −0.245; P = 0.003) and Fe (SMD = −1.783; 95% CI: −2.756, −0.809; P = 0.000) were found in SLE compared with HCs. Higher levels of Cu (SMD = 0.808; 95% CI: 0.234, 1.382; P = 0.006) were found in SLE patients. In addition, compared with HCs, Fe and Zn were lower in SLE patients in Asia and Cu was higher in SLE patients in Europe. However, no significant difference was observed in the level of Se (SMD = −0.251; 95% CI: −1.087, 0.586; P = 0.557). Above all, SLE patients exhibited lower Zn and Fe and increased Cu concentrations compared with HCs. Further studies are warranted to investigate the mechanism of Zn, Cu, and Fe in SLE patients.




Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this published article.
References
Pan HF, Leng RX, Wu GC, Ye DQ (2018) Advance in epidemiologic studies on major autoimmune diseases. Chin J Dis Control Prev 22(11):1093–1095. https://doi.org/10.16462/j.cnki.zhjbkz.2018.11.001
Kiriakidou M, Ching CL (2020) Systemic lupus erythematosus. Ann Intern Med 172(11):ITC81–ITC96. https://doi.org/10.7326/AITC202006020
Stojan G, Petri M (2018) Epidemiology of systemic lupus erythematosus: an update. Curr Opin Rheumatol 30(2):144–150. https://doi.org/10.1097/BOR.0000000000000480
González F, Sia CL, Shepard MK, Rote NS, Minium J (2012) Inflammation in response to glucose ingestion is independent of excess abdominal adiposity in normal-weight women with polycystic ovary syndrome. J Clin Endocrinol Metab 97(11):4071–4079. https://doi.org/10.1210/jc.2012-2131
Byrne C, Divekar SD, Storchan GB, Parodi DA, Martin MB (2013) Metals and breast cancer. J Mammary Gland Biol Neoplasia 18(1):63–73. https://doi.org/10.1007/s10911-013-9273-9
Meramat A, Rajab NF, Shahar S, Sharif R (2015) Cognitive impairment, genomic instability and trace elements. J Nutr Health Aging 19(1):48–57. https://doi.org/10.1007/s12603-014-0489-1
Cannas D, Loi E, Serra M, Firinu D, Valera P, Zavattari P (2020) Relevance of essential trace elements in nutrition and drinking water for human health and autoimmune disease risk. Nutrients 12(7):2074. https://doi.org/10.3390/nu12072074
Mattei J, Tamez M, Bigornia SJ, Noel SE, Xiao RS, Ríos-Bedoya CF, Rodríguez-Orengo JF, Tucker KL (2019) Dietary intake and its determinants among adults living in the metropolitan area of Puerto Rico. Nutrients 11(7):1598. https://doi.org/10.3390/nu11071598
World Health Organization. Accessed 3 July 2017; Available online: http://www.who.int/whr/2002
Tchounwou PB, Yedjou CG, Patlolla AK, Sutton DJ (2012) Heavy metal toxicity and the environment. Exp Suppl 101:133–164. https://doi.org/10.1007/978-3-7643-8340-4_6
Sanna A, Firinu D, Zavattari P, Valera P (2018) Zinc status and autoimmunity: a systematic review and meta-analysis. Nutrients 10(1):68. https://doi.org/10.3390/nu10010068
Prabhu KS, Lei XG (2016) Selenium. Adv Nutr (Bethesda, Md) 7(2):415–417. https://doi.org/10.3945/an.115.010785
Li S, Zhao H, Wang Y, Shao Y, Li J, Liu J, Xing M (2017) The inflammatory responses in Cu-mediated elemental imbalance is associated with mitochondrial fission and intrinsic apoptosis in Gallus gallus heart. Chemosphere 189:489–497. https://doi.org/10.1016/j.chemosphere.2017.09.099
Hien L, Trang P, Phuong PC, Tam PT, Xuan NT (2019) Effects of nano-copper on maize yield and inflammatory response in mice. Iran J Basic Med Sci 22(7):781–788. https://doi.org/10.22038/ijbms.2019.35787.8526
Gao X, Song Y, Lu S, Hu L, Zheng M, Jia S, Zhao M (2022) Insufficient iron improves pristane-induced lupus by promoting Treg cell expansion. Front Immunol 13:799331. https://doi.org/10.3389/fimmu.2022.799331
Katsiari CG, Liossis SN, Sfikakis PP (2010) The pathophysiologic role of monocytes and macrophages in systemic lupus erythematosus: a reappraisal. Semin Arthritis Rheum 39(6):491–503. https://doi.org/10.1016/j.semarthrit.2008.11.002
Lourdudoss C, Elkan AC, Hafström I, Jogestrand T, Gustafsson T, van Vollenhoven R, Frostegård J (2016) Dietary micronutrient intake and atherosclerosis in systemic lupus erythematosus. Lupus 25(14):1602–1609. https://doi.org/10.1177/0961203316655211
Brown AC (2000) Lupus erythematosus and nutrition: a review of the literature. J Ren Nutr 10(4):170–183. https://doi.org/10.1053/jren.2000.16323
Chang R, Chu KA, Lin MC, Chu YH, Hung YM, Wei JC (2020) Newly diagnosed iron deficiency anemia and subsequent autoimmune disease: a matched cohort study in Taiwan. Curr Med Res Opin 36(6):985–992. https://doi.org/10.1080/03007995.2020.1748585
Tóth CN, Baranyai E, Csípő I, Tarr T, Zeher M, Posta J, Fábián I (2017) Elemental analysis of whole and protein separated blood serum of patients with systemic lupus erythematosus and Sjögren’s syndrome. Biol Trace Elem Res 179(1):14–22. https://doi.org/10.1007/s12011-017-0945-y
Jahan I, Das DC, Hussain MS, Hossain MM, Chowdhury MAZ, Fardous Z, Rahman MM, Kabir AKMH, Deb SR, Siddique MAB, Das A (2021) Alterations of serum trace elements and other biochemical parameters are correlated with the pathogenesis of systemic lupus erythematosus: a preliminary study on Bangladeshi population. J Trace Elem Med Biol 68:126861. https://doi.org/10.1016/j.jtemb.2021.126861
Sahebari M, Abrishami-Moghaddam M, Moezzi A, Ghayour-Mobarhan M, Mirfeizi Z, Esmaily H, Ferns G (2014) Association between serum trace element concentrations and the disease activity of systemic lupus erythematosus. Lupus 23(8):793–801. https://doi.org/10.1177/0961203314530792
Yilmaz A, Sari RA, Gundogdu M, Kose N, Dag E (2005) Trace elements and some extracellular antioxidant proteins levels in serum of patients with systemic lupus erythematosus. Clin Rheumatol 24(4):331–335. https://doi.org/10.1007/s10067-004-1028-y
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Saghazadeh A, Mahmoudi M, Shahrokhi S, Mojarrad M, Dastmardi M, Mirbeyk M, Rezaei N (2020) Trace elements in schizophrenia: a systematic review and meta-analysis of 39 studies (N=5151 participants). Nutr Rev 78(4):278–303. https://doi.org/10.1093/nutrit/nuz059
Singh TP, Moxon JV, Gasser TC, Golledge J (2021) Systematic review and meta-analysis of peak wall stress and peak wall rupture index in ruptured and asymptomatic intact abdominal aortic aneurysms. J Am Heart Assoc 10(8):e019772. https://doi.org/10.1161/JAHA.120.019772
González S, Gutie Rrez-Díaz I, Lo Pez P, Suárez A, Fernández-Navarro T, Sánchez B, Margolles A (2017) Microbiota and oxidant-antioxidant balance in systemic lupus erythematosus. Nutr Hosp 34(‘): 934–941. doi: https://doi.org/10.20960/nh.546
Pedro EM, da Rosa Franchi Santos LF, Scavuzzi BM, Iriyoda TMV, Peixe TS, Lozovoy MAB, Reiche EMV, Dichi I, Simão ANC, Santos MJ (2018) Trace elements associated with systemic lupus erythematosus and insulin resistance. Biol Trace Elem Res 191(1):34–44. https://doi.org/10.1007/s12011-018-1592-7
Ray D, Strickland FM, Richardson BC (2018) Oxidative stress and dietary micronutrient deficiencies contribute to overexpression of epigenetically regulated genes by lupus T cells. Clin Immunol 196:97–102. https://doi.org/10.1016/j.clim.2018.04.003
Koca SS, Isik A, Ustundag B, Metin K, Aksoy K (2008) Serum pro-hepcidin levels in rheumatoid arthritis and systemic lupus erythematosus. Inflammation 31(3):146–153. https://doi.org/10.1007/s10753-008-9060-8
Gamal NM, Khedr TM, Ismail NM, He R, Badawy ER (2020) Is it useful to measure serum ferritin level in systemic lupus erythematosus patients? Egypt Rheumatol 42(11):17–21. https://doi.org/10.1016/j.ejr.2019.04.007
Lozovoy MA, Simão AN, Oliveira SR, Iryioda TM, Panis C, Cecchini R, Dichi I (2013) Relationship between iron metabolism, oxidative stress, and insulin resistance in patients with systemic lupus erythematosus. Scand J Rheumatol 42(4):303–310. https://doi.org/10.3109/03009742.2012.754942
Gonzalez JT, Fuchs CJ, Betts JA, van Loon LJ (2017) Glucose plus fructose ingestion for post-exercise recovery-greater than the sum of its parts? Nutrients 9(4):344. https://doi.org/10.3390/nu9040344
Song CH, Kim YH, Jung KI (2012) Associations of zinc and copper levels in serum and hair with sleep duration in adult women. Biol Trace Elem Res 149(1):16–21. https://doi.org/10.1007/s12011-012-9398-5
Kurien BT, Scofield RH (2008) Autoimmunity and oxidatively modified autoantigens. Autoimmun Rev 7(7):567–573. https://doi.org/10.1016/j.autrev.2008.04.019
Vural H, Uzun K, Uz E, Koçyigit A, Cigli A, Akyol O (2000) Concentrations of copper, zinc and various elements in serum of patients with bronchial asthma. J Trace Elem Med Biol 14(2):88–91. https://doi.org/10.1016/S0946-672X(00)80036-X
Prasad AS (2007) Zinc: mechanisms of host defense. J Nutr 137(5):1345–1349. https://doi.org/10.1093/jn/137.5.1345
Kurien BT, Scofield RH (2003) Free radical mediated peroxidative damage in systemic lupus erythematosus. Life Sci 73(13):1655–1666. https://doi.org/10.1016/s0024-3205(03)00475-2
Pereira TC, Campos MM, Bogo MR (2016) Copper toxicology, oxidative stress and inflammation using zebrafish as experimental model. J Appl Toxicol 36(7):876–885. https://doi.org/10.1002/jat.3303
Wei H, Zhang WJ, Leboeuf R, Frei B (2014) Copper induces--and copper chelation by tetrathiomolybdate inhibits--endothelial activation in vitro. Redox Rep 19(1):40–48. https://doi.org/10.1179/1351000213Y.0000000070
Cornelissen A, Guo L, Sakamoto A, Virmani R, Finn AV (2019) New insights into the role of iron in inflammation and atherosclerosis. EBioMedicine 47:598–606. https://doi.org/10.1016/j.ebiom.2019.08.014
Bates J, McClain CJ (1981) The effect of severe zinc deficiency on serum levels of albumin, transferrin, and prealbumin in man. Am J Clin Nutr 34(9):1655–1660. https://doi.org/10.1093/ajcn/34.9.1655
Fayyaz A, Igoe A, Kurien BT, Danda D, James JA, Stafford HA, Scofield RH (2015) Haematological manifestations of lupus. Lupus Sci Med 2(1):e000078. https://doi.org/10.1136/lupus-2014-000078
Voulgarelis M, Kokori SI, Ioannidis JP, Tzioufas AG, Kyriaki D, Moutsopoulos HM (2000) Anaemia in systemic lupus erythematosus: aetiological profile and the role of erythropoietin. Ann Rheum Dis 59(3):217–222. https://doi.org/10.1136/ard.59.3.21
Velo-García A, Castro SG, Isenberg DA (2016) The diagnosis and management of the haematologic manifestations of lupus. J Autoimmun 74:139–160. https://doi.org/10.1016/j.jaut.2016.07.001
Funding
This study was supported by the National Natural Science Foundation of China [81803310], Research Fund of Anhui Institute of translational medicine [2021zhyx-C21], Undergraduate Innovation and Entrepreneurship Training Program in Anhui Province [S201910366064], the Grants for Scientific Research of BSKY from Anhui Medical University [XJ201619], and Peak Discipline of Public Health and Preventive Medicine, Anhui Medical University.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Article retrieval, data extraction, and the first draft of the manuscript were performed by Hua Wang, Xian-Bao Li, and Rong-Gui Huang. Data sorting, inspection, and analysis were performed by Nv-Wei Cao, Hong Wu, Kai-Di Li, and Yi-Yu Wang. Bao-Zhu Li contributed to the project administration and funding acquisition. All authors commented on previous versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Ethics Approval
Not applicable (This article does not contain any studies with human participants or animals performed by any of the authors).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Wang, H., Li, XB., Huang, RG. et al. Essential Trace Element Status in Systemic Lupus Erythematosus: a Meta-analysis Based on Case-Control Studies. Biol Trace Elem Res 201, 2170–2182 (2023). https://doi.org/10.1007/s12011-022-03335-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-022-03335-y