Abstract
Background
Revision THA and TKA are growing and important clinical and economic challenges. Healthcare systems tend to combine revision joint replacement procedures into a single service line, and differences between revision THA and revision TKA remain incompletely characterized. These differences carry implications for guiding care and resource allocation. We therefore evaluated epidemiologic trends associated with revision THAs and TKAs.
Questions/purposes
We sought to determine differences in (1) the number of patients undergoing revision TKA and THA and respective demographic trends; (2) differences in the indications for and types of revision TKA and THA; (3) differences in patient severity of illness scoring between THA and TKA; and (4) differences in resource utilization (including cost and length of stay [LOS]) between revision THA and TKA.
Methods
The Nationwide Inpatient Sample (NIS) was used to evaluate 235,857 revision THAs and 301,718 revision TKAs between October 1, 2005 and December 31, 2010. Patient characteristics, procedure information, and resource utilization were compared across revision THAs and TKAs. A revision burden (ratio of number of revisions to total number of revision and primary surgeries) was calculated for hip and knee procedures. Severity of illness scoring and cost calculations were derived from the NIS. As our study was principally descriptive, statistical analyses generally were not performed; however, owing to the large sample size available to us through this NIS analysis, even small observed differences presented are likely to be highly statistically significant.
Results
Revision TKAs increased by 39% (revision burden, 9.1%–9.6%) and THAs increased by 23% (revision burden, 15.4%–14.6%). Revision THAs were performed more often in older patients compared with revision TKAs. Periprosthetic joint infection (25%) and mechanical loosening (19%) were the most common reasons for revision TKA compared with dislocation (22%) and mechanical loosening (20%) for revision THA. Full (all-component) revision was more common in revision THAs (43%) than in TKAs (37%). Patients who underwent revision THA generally were sicker (> 50% major severity of illness score) than patients who underwent revision TKA (65% moderate severity of illness score). Mean LOS was longer for revision THAs than for TKAs. Mean hospitalization costs were slightly higher for revision THA (USD 24,697 +/− USD 40,489 [SD]) than revision TKA (USD 23,130 +/− USD 36,643 [SD]). Periprosthetic joint infection and periprosthetic fracture were associated with the greatest LOS and costs for revision THAs and TKAs.
Conclusions
These data could prove important for healthcare systems to appropriately allocate resources to hip and knee procedures: the revision burden for THA is 52% greater than for TKA, but revision TKAs are increasing at a faster rate. Likewise, the treating clinician should understand that while both revision THAs and TKAs bear significant clinical and economic costs, patients undergoing revision THA tend to be older, sicker, and have greater costs of care.
Similar content being viewed by others
Introduction
Primary THA and TKA remain cost-effective interventions [12, 31, 32]. However, despite the clinical success of THAs and TKAs, the number of revision THAs [4, 38] and TKAs [4, 21, 34, 35] performed in the United States has increased with time. The revision THA and TKA caseload per orthopaedic surgeon also has increased [28]. The etiology of the increase in the number of revision procedures is multifactorial. The increasing absolute number of primary arthroplasties [21, 44, 53, 58], expansion of the indications to include younger and more active individuals [11, 18, 19, 23, 29, 30, 34, 42, 44, 46, 49], and certain patient factors such as obesity [55, 60], all likely contribute to overall revision rates. Projections based on population studies point to continued increases in the prevalence of revision procedures [22].
Healthcare systems tend to combine joint replacement procedures into one service line, and differences between primary total joint arthroplasties and revision THAs and TKAs remain incompletely characterized. These differences carry implications for guiding care and resource allocation. New approaches to capturing the diagnoses and procedures that physicians and hospitals code as part of the billing process, such as the those used by the Nationwide Inpatients Sample (NIS), allow for larger-scale evaluations of the epidemiology of revision total joint arthroplasties than previously could be performed [13, 14, 17, 37, 51, 56]. Prior studies [7, 8] have been done that investigated the revised coding scheme in a national sample [1] to more clearly identify the indications for revision, procedure frequencies, and degree of adoption of the new diagnosis and procedure codes. While subset analyses were performed regarding payer status, patient demographics, and cost metrics, previous studies presented only the early experience during the first 15 months after revised ICD-9-CM coding changes [5, 6] were introduced. Since then, an additional 4 years of data have been made available with the more granular ICD-9-CM codes, which can now be used to provide better understanding of the epidemiology of revision THAs and TKAs.
The purpose of our study was to evaluate the causes and epidemiology of revision THAs and TKAs with respect to patient, hospital, geographic, and payer characteristics. We sought to determine differences in (1) the number of patients undergoing revision TKAs and THAs and respective demographic trends; (2) differences in the indications for and types of revision TKAs and THAs; (3) differences in patient severity of illness scoring between THA and TKA; and (4) differences in resource utilization (including cost and length of stay [LOS]) between revision THA and TKA. As epidemiology is a dynamic process, we sought to define the changing patterns and to understand the mechanisms of failure in revision joint arthroplasties during a 5-year period.
Patients and Methods
The NIS [1] was used to evaluate 235,857 revision THAs and 301,718 revision TKAs between October 1, 2005 and December 31, 2010. The NIS dataset is widely used to examine the prevalence and epidemiology of various diseases and surgical procedures [1]. It is the largest nationally representative inpatient dataset in the United States [1]. In the latest year of data used for our study (2010), the NIS contained discharge data from 1051 hospitals in 45 states, including approximately 8,000,000 discharge records. For 2010, the 45 states in the database comprised more than 96% of the US population. Community hospitals sampled by the NIS are stratified, using five hospital characteristics: ownership/control, bed size, teaching status, urban/rural location, and US region. Stratified probability samples of hospitals, with sampling probabilities proportional to the number of US community hospitals in each stratum, are used to approximate a 20% sample of all hospital discharges in the United Stated, regardless of patient demographics or payer. Statistical weights are provided to calculate national estimates, extrapolating from the 20% sample. The NIS is administered by the Healthcare Cost and Utilization Project (HCUP) through the Agency for Healthcare Research and Quality [1].
Inpatient stay records in the NIS include clinical and resource-use information typically available from discharge abstracts. Each record includes details regarding patient demographics, diagnosis, and procedure performed at the hospital based on ICD-9-CM codes, diagnosis-related group (DRG) information, payer information, and various risk-stratification metrics (including All Patient Refined-DRG severity of illness). Severity of illness scores are based on the number and severity of patient comorbid conditions and are stratified as minor, moderate, major, or extreme.
Based on ICD-9-CM codes for revision THA (00.70–00.73, 80.05, 81.53) and revision TKA (00.80–00.84, 80.06, 81.55), we extracted all records pertaining to revision THAs and TKAs. The data were analyzed based on the specific type of procedure and diagnosis associated with the revision surgery. Revision burden was determined by the ratio of the number of revision procedures to total number of revision and primary procedures. Patient characteristics and procedure information were compared across revision THAs and TKAs.
Other resource utilization data included in the NIS are hospital charges, LOS, and various hospital characteristics. Hospitalization costs were calculated by converting the charges using charge-to-cost ratios provided in the NIS dataset. As our study principally was descriptive, statistical analyses generally were not performed; however, owing to the large sample size available through this NIS analysis, even small observed differences are likely to be highly statistically significant.
The NIS contains hospital charge data, which represents the amount that hospitals billed for services but does not reflect how much hospital services actually cost or the specific amounts that hospitals received in payment. The HCUP uses cost information obtained from the hospital accounting reports collected by the Centers for Medicare & Medicaid Services to provide hospital-specific cost-to-charge ratios, to allow researchers to convert the hospital charges to costs.
Results
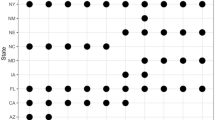
Analysis of the number of patients undergoing revision TKAs and THAs highlights important differences and demographic trends between the two procedures. Revision TKAs increased by 39%, from 48,260 in 2006 to 67,534 in 2010 (revision burden, 9.1%–9.6%); revision THAs increased by 23%, from 40,555 in 2006 to 49,857 in 2010 (revision burden, 15.4%–14.6%) (Table 1). The peak frequency of revision THAs occurred in older patients (75–84 years old) compared with revision TKAs (65–74 years old). The highest percentage of revision THAs and TKAs were performed in white women who were Medicare patients in large, urban hospitals in the South and Midwest United States (Table 2). Women accounted for 78% of revision TKAs and 65% of revision THAs associated with periprosthetic fractures. Similarly, women accounted for 65% of revision TKAs and 65% of revision THAs associated with instability/dislocation (Table 3).
Differences were found in the indications for and types of revision TKA and THA. Periprosthetic joint infections accounted for 25% of the TKA revisions, and mechanical loosening (19%) were the most common reasons for revision TKAs, while dislocation (22%) and mechanical loosening (20%) were the most common reasons for revision THAs (Table 4). Among the various reasons for revision, periprosthetic fracture (996.44) and dislocation (996.42) were much more prevalent among women compared with men. All-component revision was greater in revision THAs (43%) than in revision TKAs (37%) (Table 5).
In general, patients who underwent revision THA had more medical comorbidities than did patients undergoing revision TKA. Patients who had revision THAs were more likely to have a major severity of revision score (53%) compared with patients who had revision TKAs (15%).
Resource utilization was greater for patients who had revision THAs than TKAs with respect to LOS and hospitalization costs. The mean LOS was longer for patients who had revision THA (mean ± SD, 5.8 days ± 14.0 days) than for patients who had TKA (mean ± SD, 4.8 days ± 10.5 days). The mean hospitalization costs were greater for revision THA (mean ± SD, USD 24,697 ± USD 40,489) than revision TKA (mean ± SD, USD 23,130 ± USD 36,643 (Table 6). Periprosthetic joint infection and periprosthetic fracture were associated with the greatest LOS and costs for revision THAs and TKAs.
Discussion
Rates of revision THAs and TKAs continue to increase [21, 39] despite changes in implant design and surgical technique. Therefore, it is important to understand and define the epidemiology of failure of these procedures. Using administrative data, referencing more clinically descriptive ICD-9-CM diagnosis and procedure codes introduced in October 2005, we can better discern trends in causes and types of reverse joint arthroplasties. Healthcare systems tend to combine joint replacement procedures in one service line, and differences between primary and revision THAs and TKAs are often incompletely characterized. These differences carry implications for guiding care and resource allocation. We therefore sought to determine differences in (1) the number of patients undergoing revision TKAs and THAs and respective demographic trends; (2) differences in the indications for and types of revision TKAs and THAs; (3) differences in severity of illness scoring for patients between THAs and TKAs; and (4) differences in resource utilization (including cost and LOS) between revision THAs and TKAs.
Limitations exist with the use of administratively coded data. The value of administrative codes in determining how total joint arthroplasties fail, and the procedures used to revise failing implants, depend largely on the adoption of diagnosis and procedure codes, and their definitions and use. Accuracy of revision total joint arthroplasty procedure codes may depend on interpretation of clinical documentation by coding staff, and completeness of diagnosis descriptions may be surgeon-dependent. Confounding factors, when comparing revision THA with revision TKA, include changing design factors and particular implant failures (eg, early failure of certain designs like metal-on-metal implants for THA). Although administrative datasets and improved ICD-9-CM diagnosis and procedure coding are not a substitute for a formal national arthroplasty registry [34, 57], a large, nationally representative, and generalizable study population provides increased external validity, and administrative datasets are used by public reporting and governmental agencies. While the NIS contains hospital charge data (ie, how much the hospitals billed for particular services), the cost data in our study derived from the NIS does not reflect how much hospital services actually cost or the specific amounts that hospitals received in payment. In addition, as this study principally was descriptive, statistical analyses were not performed. However, owing to the large sample size in the NIS dataset, even small observed differences are likely to be highly statistically significant and unlikely to be a consequence of chance. Therefore, one should focus on the effect size in terms of absolute differences in the changes.
Our analysis of the demographic trends associated with revision TKAs and THAs showed important differences among patients who undergo the respective procedures.
Although a 23% increase in the number of hospitalizations was seen for patients having revision THAs from 2006 to 2010, a nearly 40% increase in the number of hospitalizations for patients having revision TKAs was observed. Revision TKAs are increasing at a faster rate than revision THAs, likely attributable in part to the higher underlying rates of primary TKA [21]. This trend is mirrored in worldwide rates of revision TKAs [26] using international registry data [40].
The revision TKAs were mostly attributable to mechanical loosening and periprosthetic joint infection in younger patients (younger than 75 years), which may represent an emerging age shift, given that an increasing proportion of primary TKAs are being performed in younger patients [18, 58]. The similar patient age trends in revision THA also may represent an emerging age shift in the burden of revision, given that an increasing proportion of primary THAs are being performed in younger patients [11, 19, 23, 42, 44]. It is estimated that by 2030, patients younger than 65 years will comprise 52% of primary THAs being performed [23]. Nevertheless, the largest difference across age subgroups for revision THA was for periprosthetic fracture, for which more than 30% of total revisions were in patients 75 to 84 years old. Future data will show if age-related trends prove to be important for revision THAs and TKAs.
As reported in previous studies [7, 8], the majority of revision THAs and TKAs were performed in women. Only periprosthetic osteolysis was a more common revision diagnosis for men. The greatest sex differences in diagnoses for revision surgery were for periprosthetic fracture. The disparity in patient sex may be compared with other revision TKA diagnoses, such as periprosthetic osteolysis and periprosthetic joint infection, which had a nearly even sex distribution. For revision THAs and TKAs, white patients accounted for more than 80% of all revisions performed in each year. Black and Hispanic patients were the second highest patient groups, but accounted for less than 15% of patients undergoing total revisions.
When comparing the indications and types of procedures associated with revision TKA and revision THA, several differences were found. Our findings of indications for revision echo previous epidemiologic studies of revision total joint arthroplasties [7, 8]; however, our findings for revision THAs differ from prior observational cohort studies [3, 54] and international registry reports [33, 43] that identified aseptic loosening, bearing surface wear, and osteolysis as primary causes of TKA failure. Likewise, our revision TKA findings differ from those of prior reports implicating aseptic etiologies, including polyethylene wear, prosthetic loosening, and instability as the primary mechanisms for failed TKA [16, 36, 37, 41, 51, 52]. Other studies have reported that periprosthetic joint infection is a primary indication for revision TKA [14, 56]. Population and other regional differences might exist that may explain differing results in international registry data. Some of the variation in reasons reported for revision total joint arthroplasties may be based on differences in coding between administrative and clinical databases. For example, there are several categories of “mechanical problems” in ICD-9-CM coding that may be included under different titles (eg, aseptic loosening) in clinical databases.
The increasing trend for the use of the “mechanical loosening” code (ICD-9-CM 996.41) may be partly explained by a relative increase in mechanical loosening as a dominant mode of total joint replacement failure. The second most common reason for revision TKA, mechanical loosening (16.1%), may have been surpassed owing to the coalescing of other codes for mechanical complications. All-component revision ranks as the most common type of revision procedure and has remained fairly constant [7, 8]. With a periprosthetic joint infection, “arthrotomy or removal” accounted for more than 45% of procedures for revision THAs and TKAs, and all-component revision was the next most common reason.
Patient comorbidities and severity of illness proved to be important factors in treating patients who undergo revision arthroplasty. Analysis of severity of illness in our patient populations found differences with respect to revision THAs and TKAs. The revision THA diagnoses most often associated with a major severity of illness score were implant-related problems, followed by periprosthetic joint infection. For a periprosthetic joint infection, the minimum severity of illness score for patients was moderate (ie, no patients received a minor score), which points to the potential for comorbidities and poor overall health often associated with a periprosthetic joint infection. Revision TKAs for periprosthetic joint infections and fracture are the two diagnoses most frequently seen in patients in urban, nonteaching settings, and these diagnoses were most often associated with a major (and/or extreme) severity of illness score. Comorbidities have been reported to be associated with increased risk of periprosthetic joint infection in patients who have undergone TKA [25]. The diagnoses most often associated with a moderate severity of illness score were periprosthetic osteolysis, then implant-related problems. The proportion of patients with older age (≥ 65 years) undergoing revision THA affects the underlying frequencies of population comorbidities. Revision THAs tend to be performed in sicker patients, and comorbidities particularly influence the rate of revision after primary THA [38], including the rate of early revision in the elderly [9]. Risk-assessment tools may offer physicians the opportunity to counsel elderly patients regarding the specific risks of infection after THA [10]. Bearing surface wear was the only diagnosis in which a moderate severity of illness score was more common than a major score; again, this may have been related to age or other patient-related factors that track with bearing surface failure mechanisms. It also may have been related to younger patients who had hip implants with conventional polyethylene during previous decades, who now more often are undergoing revision for bearing wear.
We noted important differences in resource utilization, including LOS and cost, between revision THAs and TKAs. The differences between LOS for revision THAs and TKAs may relate to severity of illness scoring and complexity of surgical procedures and rehabilitation issues. Periprosthetic joint infection and periprosthetic fracture were associated with the highest costs for revision THA and revision TKA. Hospitalization costs contribute to the overall economic burden of patients with an infected arthroplasty [24, 27]. Outcomes after revision TKAs for patients with periprosthetic joint infection are worse than for patients with aseptic knee revision [2, 15, 20, 50, 59].
The prevalence of revision THAs and TKAs is increasing. Our study highlights the comparative differences between revision THAs and TKAs. For both procedures, numerous epidemiologic changes, compared with prior reports [7, 8], have been identified, and variability continues to exist in patient characteristics, modes of failure, procedure types, and resource utilization across hospitals and different regions of the country. Identifying the mechanisms of failure in revision joint arthroplasties is critical to guiding efforts to improve clinical outcomes. Beyond clinical demands associated with revisions, the increasing economic burden of these procedures creates financial strains for surgeons, patients, and health systems [23, 47, 48]. These data may be important for healthcare systems to appropriately allocate resources in arthroplasty service lines: The revision burden for THA is greater than for TKA, but revision TKAs are increasing at a faster rate. Likewise, the treating clinician should understand that, while revision THAs and TKAs bear significant clinical and economic costs, patients undergoing revision THA tend to be older, sicker, and have greater costs of care. The results of our study should inform avenues for research, clinical care, and cost measurements [45]. Continued analyses will further characterize emerging trends in the provision of care to patients undergoing revision THAs and TKAs.
References
Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP). Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2007. Available at: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2007_INTRODUCTION.pdf. Accessed July 1, 2014.
Bengtson S, Knutson K. The infected knee arthroplasty: a 6-year follow-up of 357 cases. Acta Orthop Scand. 1991;62:301–311.
Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84:171–177.
Bourne RB, Maloney WJ, Wright JG. An AOA critical issue: the outcome of the outcomes movement. J Bone Joint Surg Am. 2004;86:633–640.
Bozic KJ. CMS changes IC9 and DRG codes for revision TJA. 2005. Available at: http://www2.aaos.org/bulletin/jun05/fline1.asp. Accessed September 1, 2014.
Bozic KJ, Katz P, Cisternas M, Ono L, Ries MD, Showstack J. Hospital resource utilization for primary and revision total hip arthroplasty. J Bone Joint Surg Am. 2005;87:570–576.
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51.
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133.
Bozic KJ, Lau E, Ong K, Chan V, Kurtz S, Vail TP, Rubash HE, Berry DJ. Risk factors for early revision after primary total hip arthroplasty in Medicare patients. Clin Orthop Relat Res. 2014;472:449–454.
Bozic KJ, Ong K, Lau E, Berry DJ, Vail TP, Kurtz SM, Rubash HE. Estimating risk in Medicare patients with THA: an electronic risk calculator for periprosthetic joint infection and mortality. Clin Orthop Relat Res. 2013;471:574–583.
Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PLoS One. 2010;5:e13520.
Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol. 2012;26:649–658.
Emmerson KP, Moran CG, Pinder IM. Survivorship analysis of the Kinematic Stabilizer total knee replacement: a 10- to 14-year follow-up. J Bone Joint Surg Br. 1996;78:441–445.
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318.
Goldman RT, Scuderi GR, Insall JN. 2-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res. 1996;331:118–124.
Gonzalez MH, Mekhail AO. The failed total knee arthroplasty: evaluation and etiology. J Am Acad Orthop Surg. 2004;12:436–446.
Huang CH, Liau JJ, Lung CY, Lan CT, Cheng CK. The incidence of revision of the metal component of total knee arthroplasties in different tibial-insert designs. Knee. 2002;9:331–334.
Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R, Katz JN. Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum. 2005;52: 3928–3933.
Katz JN, Wright EA, Wright J, Malchau H, Mahomed NN, Stedman M, Baron JA, Losina E. Twelve-year risk of revision after primary total hip replacement in the U.S. Medicare population. J Bone Joint Surg Am. 2012;94:1825–1832.
Kramhoft M, Bodtker S, Carlsen A. Outcome of infected total knee arthroplasty. J Arthroplasty. 1994;9:617–621.
Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785.
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467: 2606–2612.
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27(8 suppl):61–65.e1.
Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010;468:52–56.
Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gomez-Barrena E, de Pina Mde F, Manno V, Torre M, Walter WL, de Steiger R, Geesink RG, Peltola M, Roder C. International survey of primary and revision total knee replacement. Int Orthop. 2011;35:1783–1789.
Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, Karrholm J, Garellick G, Havelin LI, Furnes O, Malchau H, Lau E. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(suppl 3):144–151.
Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty. 2009;24:195–203.
Leskinen J, Eskelinen A, Huhtala H, Paavolainen P, Remes V. The incidence of knee arthroplasty for primary osteoarthritis grows rapidly among baby boomers: a population-based study in Finland. Arthritis Rheum. 2012;64:423–428.
Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207.
Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–1121; discussion 1121–1122.
Lyman S, Marx RG, Bach PB. Cost-effectiveness analysis of an established, effective procedure. Arch Intern Med. 2009;169:1102–1103.
Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84(suppl 2):2–20.
Maloney WJ. National Joint Replacement Registries: has the time come? J Bone Joint Surg Am. 2001;83:1582–1585.
Maloney WJ. An American implant registry: a clinical use trip wire. Orthopedics. 2002;25:923–924.
Mikulak SA, Mahoney OM, dela Rosa MA, Schmalzried TP. Loosening and osteolysis with the press-fit condylar posterior-cruciate-substituting total knee replacement. J Bone Joint Surg Am. 2001;83:398–403.
Mulhall KJ, Ghomrawi HM, Scully S, Callaghan JJ, Saleh KJ. Current etiologies and modes of failure in total knee arthroplasty revision. Clin Orthop Relat Res. 2006;446:45–50.
Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468:3070–3076.
Ong KL, Mowat FS, Chan N, Lau E, Halpern MT, Kurtz SM. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2006;446:22–28.
Peltola M, Malmivaara A, Paavola M. Learning curve for new technology?: a nationwide register-based study of 46,363 total knee arthroplasties. J Bone Joint Surg Am. 2013;95:2097–2103.
Peters PC Jr, Engh GA, Dwyer KA, Vinh TN. Osteolysis after total knee arthroplasty without cement. J Bone Joint Surg Am. 1992;74:864–876.
Prokopetz JJ, Losina E, Bliss RL, Wright J, Baron JA, Katz JN. Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC Musculoskelet Disord. 2012;13:251.
Puolakka TJ, Pajamaki KJ, Halonen PJ, Pulkkinen PO, Paavolainen P, Nevalainen JK. The Finnish Arthroplasty Register: report of the hip register. Acta Orthop Scand. 2001;72:433–441.
Ravi B, Croxford R, Reichmann WM, Losina E, Katz JN, Hawker GA. The changing demographics of total joint arthroplasty recipients in the United States and Ontario from 2001 to 2007. Best Pract Res Clin Rheumatol. 2012;26:637–647.
Rorabeck CH, Murray P. Cost effectiveness of revision total knee replacement. Instr Course Lect. 1997;46:237–240.
Saleh KJ, Santos ER, Ghomrawi HM, Parvizi J, Mulhall KJ. Socioeconomic issues and demographics of total knee arthroplasty revision. Clin Orthop Relat Res. 2006;446:15–21.
Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472:464–470.
Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital Rradmission after total knee arthroplasty? Clin Orthop Relat Res. 2014;472:181–187.
Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa’vae F, McKellop HA, McClung CD, Martell J, Moreland JR, Amstutz HC. The John Charnley Award: Wear is a function of use, not time. Clin Orthop Relat Res. 2000;381:36–46.
Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB. Infection after total knee arthroplasty: a retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999;81:1434–1445.
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper: Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13.
Sheng P, Lehto M, Kataja M, Halonen P, Moilanen T, Pajamaki J. Patient outcome following revision total knee arthroplasty: a meta-analysis. Int Orthop. 2004;28:78–81.
Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ 3rd, Kurland RL, Berry DJ. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969–2008. Mayo Clin Proc. 2010;85: 898–904.
Ulrich SD, Seyler TM, Bennett D, Delanois RE, Saleh KJ, Thongtrangan I, Kuskowski M, Cheng EY, Sharkey PF, Parvizi J, Stiehl JB, Mont MA. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008;32:597–604.
Vasarhelyi EM, MacDonald SJ. The influence of obesity on total joint arthroplasty. J Bone Joint Surg Br. 2012;94:100–102.
Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. The Chitranjan Ranawat Award: Long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006;452:28–34.
von Knoch F, Malchau H. Why do we need a national joint replacement registry in the United States? Am J Orthop (Belle Mead NJ). 2009;38:500–503.
Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am. 2013;95:385–392.
Wilde AH, Ruth JT. Two-stage reimplantation in infected total knee arthroplasty. Clin Orthop Relat Res. 1988;236:23–35.
Wright EA, Katz JN, Baron JA, Wright RJ, Malchau H, Mahomed N, Prokopetz JJ, Losina E. Risk factors for revision of primary total hip replacement: results from a national case-control study. Arthritis Care Res (Hoboken). 2012;64:1879–1885.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (SMK, KO, EL) are employees of Exponent, Inc, Menlo Park, CA, USA, and Philadelphia, PA, USA.
One of the authors certifies that he (DJB), or a member of his or her immediate family, has received or may receive payments or benefits, during the study period, an amount in excess of USD 100,001–USD 1,000,000, from DePuy Orthopaedics, Inc (Warsaw, IN, USA).
One of the authors (TPV) certifies that he has received or may receive payments or benefits, during the study period, an amount in excess of USD 10,001–USD 100,000 from DePuy Orthopaedics, Inc (Warsaw, IN, USA).
One of the authors (HER) certifies that he has received or may receive payments or benefits, during the study period, an amount in excess of USD 100,001–USD 1,000,000, from Zimmer, Inc (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that the institution where the work was performed approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
This work was performed at University of California, San Francisco and Exponent, Inc, Menlo Park, CA, USA.
About this article
Cite this article
Bozic, K.J., Kamath, A.F., Ong, K. et al. Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA. Clin Orthop Relat Res 473, 2131–2138 (2015). https://doi.org/10.1007/s11999-014-4078-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-4078-8