Abstract
Background
This study evaluated early and medium-term changes in bone turnover markers, and their associations with weight loss, total bone mineral density (BMD), and hormonal changes after biliopancreatic diversion (BPD).
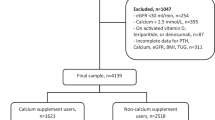
Methods
Ancillary study from a one-year prospective cohort of 16 individuals assessed before, 3 days, 3 and 12 months after BPD. Bone turnover markers (C-terminal telopeptide (CTX), intact osteocalcin (OC), sclerostin, and osteoprotegerin (OPG)) and several hormones were measured at each visit. Total BMD by DXA was assessed at baseline, 3 and 12 months after BPD. Three participants were lost to follow-up.
Results
CTX increased significantly at 3 days (+ 66%), 3 months (+ 219%), and 12 months (+ 295%). OC decreased at 3 days (− 19%) then increased at 3 months (+ 69%) and 12 months (+ 164%). Change in sclerostin was only significant between 3 days and 3 months (+ 13%), while change in OPG was significant between baseline and 3 days (+ 48%) and baseline and 12 months (+ 45%). CTX increase correlated negatively with weight loss at 3 (r = − 0.63, p = 0.009) and 12 months (r = − 0.58, p = 0.039), and total BMD decrease (r = − 0.67, p = 0.033) at 12 months. Change in insulin and adiponectin correlated with changes in bone turnover markers independently of weight loss.
Conclusion
BPD causes an earlier and greater increase in bone resorption over bone formation markers and a decrease in total BMD. Sclerostin did not increase as expected following extensive weight loss. Changes in insulin and adiponectin seem to play a role in the activation of bone remodeling after BPD.

Similar content being viewed by others
References
Ozsoy Z, Demir E. Which bariatric procedure is the most popular in the world? A bibliometric comparison. Obes Surg. 2018.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Claudia G, Schafer AL. Bone health after bariatric surgery. JBMR Plus. 2018;2(3):121–33.
Lu CW, Chang YK, Chang HH, et al. Fracture risk after bariatric surgery: a 12-year nationwide cohort study. Medicine (Baltimore). 2015;94(48):e2087.
Yu EW, Bouxsein ML, Putman MS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100(4):1452–9.
Rousseau C, Jean S, Gamache P, et al. Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. BMJ. 2016;354:i3794.
Nakamura KM, Haglind EG, Clowes JA, et al. Fracture risk following bariatric surgery: a population-based study. Osteoporos Int. 2014;25(1):151–8.
Yu EW. Bone metabolism after bariatric surgery. J Bone Miner Res. 2014;29(7):1507–18.
Yu EW, Wewalka M, Ding SA, et al. Effects of gastric bypass and gastric banding on bone remodeling in obese patients with type 2 diabetes. J Clin Endocrinol Metab. 2016;101(2):714–22.
Muschitz C, Kocijan R, Marterer C, et al. Sclerostin levels and changes in bone metabolism after bariatric surgery. J Clin Endocrinol Metab. 2015;100(3):891–901.
Hosseinzadeh-Attar MJ, Golpaie A, Janani L, et al. Effect of weight reduction following bariatric surgery on serum visfatin and adiponectin levels in morbidly obese subjects. Obes Facts. 2013;6(2):193–202.
Bruno C, Fulford AD, Potts JR, et al. Serum markers of bone turnover are increased at six and 18 months after Roux-en-Y bariatric surgery: correlation with the reduction in leptin. J Clin Endocrinol Metab. 2010;95(1):159–66.
Kotidis EV, Koliakos GG, Baltzopoulos VG, et al. Serum ghrelin, leptin and adiponectin levels before and after weight loss: comparison of three methods of treatment—a prospective study. Obes Surg. 2006;16(11):1425–32.
Grenier-Larouche T, Carreau AM, Geloen A, et al. Fatty acid metabolic remodeling during type 2 diabetes remission after bariatric surgery. Diabetes. 2017;66(11):2743–55.
Plourde CE, Grenier-Larouche T, Caron-Dorval D, et al. Biliopancreatic diversion with duodenal switch improves insulin sensitivity and secretion through caloric restriction. Obesity (Silver Spring). 2014;22(8):1838–46.
Tsiftsis DD, Mylonas P, Mead N, et al. Bone mass decreases in morbidly obese women after long limb-biliopancreatic diversion and marked weight loss without secondary hyperparathyroidism. A physiological adaptation to weight loss? Obes Surg. 2009;19(11):1497–503.
Sinha N, Shieh A, Stein EM, et al. Increased PTH and 1.25(OH)(2)D levels associated with increased markers of bone turnover following bariatric surgery. Obesity (Silver Spring). 2011;19(12):2388–93.
Balsa JA, Botella-Carretero JI, Peromingo R, et al. Chronic increase of bone turnover markers after biliopancreatic diversion is related to secondary hyperparathyroidism and weight loss. Relation with bone mineral density. Obes Surg. 2010;20(4):468–73.
Granado-Lorencio F, Simal-Anton A, Salazar-Mosteiro J, et al. Time-course changes in bone turnover markers and fat-soluble vitamins after obesity surgery. Obes Surg. 2010;20(11):1524–9.
Marceau P, Biron S, Lebel S, et al. Does bone change after biliopancreatic diversion? J Gastrointest Surg. 2002;6(5):690–8.
Ivaska KK, Heliovaara MK, Ebeling P, et al. The effects of acute hyperinsulinemia on bone metabolism. Endocr Connect. 2015;4(3):155–62.
Biagioni MFG, Mendes AL, Nogueira CR, et al. Bariatric Roux-En-Y gastric bypass surgery: adipocyte proteins involved in increased bone remodeling in humans. Obes Surg. 2017;27(7):1789–96.
Hofso D, Bollerslev J, Sandbu R, et al. Bone resorption following weight loss surgery is associated with treatment procedure and changes in secreted Wnt antagonists. Endocrine. 2016;53(1):313–21.
Stein EM, Carrelli A, Young P, et al. Bariatric surgery results in cortical bone loss. J Clin Endocrinol Metab. 2013;98(2):541–9.
Sims NA, Martin TJ. Coupling the activities of bone formation and resorption: a multitude of signals within the basic multicellular unit. Bonekey Rep. 2014;3:481.
Villareal DT, Fontana L, Das SK, et al. Effect of two-year caloric restriction on bone metabolism and bone mineral density in non-obese younger adults: a randomized clinical trial. J Bone Miner Res. 2016;31(1):40–51.
Devlin MJ, Cloutier AM, Thomas NA, et al. Caloric restriction leads to high marrow adiposity and low bone mass in growing mice. J Bone Miner Res. 2010;25(9):2078–88.
Ahn H, Seo DH, Kim HS, et al. Calorie restriction aggravated cortical and trabecular bone architecture in ovariectomy-induced estrogen-deficient rats. Nutr Res. 2014;34(8):707–13.
Murri M, Garcia-Fuentes E, Garcia-Almeida JM, et al. Changes in oxidative stress and insulin resistance in morbidly obese patients after bariatric surgery. Obes Surg. 2010;20(3):363–8.
Wauquier F, Leotoing L, Coxam V, et al. Oxidative stress in bone remodelling and disease. Trends Mol Med. 2009;15(10):468–77.
O'Flaherty EJ. Modeling normal aging bone loss, with consideration of bone loss in osteoporosis. Toxicol Sci. 2000;55(1):171–88.
Rodriguez-Carmona Y, Lopez-Alavez FJ, Gonzalez-Garay AG, et al. Bone mineral density after bariatric surgery. A systematic review. Int J Surg. 2014;12(9):976–82.
Armamento-Villareal R, Sadler C, Napoli N, et al. Weight loss in obese older adults increases serum sclerostin and impairs hip geometry but both are prevented by exercise training. J Bone Miner Res. 2012;27(5):1215–21.
Stein EM, Silverberg SJ. Bone loss after bariatric surgery: causes, consequences, and management. Lancet Diabetes Endocrinol. 2014;2(2):165–74.
Piec I, Washbourne C, Tang J, et al. How accurate is your sclerostin measurement? Comparison between three commercially available sclerostin ELISA kits. Calcif Tissue Int. 2016;98(6):546–55.
Topart P, Becouarn G, Ritz P. Weight loss is more sustained after biliopancreatic diversion with duodenal switch than Roux-en-Y gastric bypass in superobese patients. Surg Obes Relat Dis. 2013;9(4):526–30.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:Cd003641.
Neumann E, Muller-Ladner U, Frommer KW. Inflammation and bone metabolism. Z Rheumatol. 2014;73(4):342–8.
Canalis E, Delany AM. Mechanisms of glucocorticoid action in bone. Ann N Y Acad Sci. 2002;966:73–81.
Meek CL, Lewis HB, Reimann F, et al. The effect of bariatric surgery on gastrointestinal and pancreatic peptide hormones. Peptides. 2016;77:28–37.
Valderas JP, Padilla O, Solari S, et al. Feeding and bone turnover in gastric bypass. J Clin Endocrinol Metab. 2014;99(2):491–7.
Tonks KT, White CP, Center JR, et al. Bone turnover is suppressed in insulin resistance, independent of adiposity. J Clin Endocrinol Metab. 2017;102(4):1112–21.
Frost M, Balkau B, Hatunic M, et al. The relationship between bone turnover and insulin sensitivity and secretion: cross-sectional and prospective data from the RISC cohort study. Bone. 2018;108:98–105.
Wei J, Ferron M, Clarke CJ, et al. Bone-specific insulin resistance disrupts whole-body glucose homeostasis via decreased osteocalcin activation. J Clin Invest. 2014;124(4):1–13.
Fulzele K, Riddle RC, DiGirolamo DJ, et al. Insulin receptor signaling in osteoblasts regulates postnatal bone acquisition and body composition. Cell. 2010;142(2):309–19.
Clemens TL, Karsenty G. The osteoblast: an insulin target cell controlling glucose homeostasis. J Bone Miner Res. 2011;26(4):677–80.
Ferron M, Wei J, Yoshizawa T, et al. Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell. 2010;142(2):296–308.
Yu OH, Richards B, Berger C, et al. The association between sclerostin and incident type 2 diabetes risk: a cohort study. Clin Endocrinol. 2017;86(4):520–5.
Kang J, Boonanantanasarn K, Baek K, et al. Hyperglycemia increases the expression levels of sclerostin in a reactive oxygen species- and tumor necrosis factor-alpha-dependent manner. J Periodontal Implant Sci. 2015;45(3):101–10.
Luo XH, Guo LJ, Yuan LQ, et al. Adiponectin stimulates human osteoblasts proliferation and differentiation via the MAPK signaling pathway. Exp Cell Res. 2005;309(1):99–109.
Kanazawa I, Yamaguchi T, Yano S, et al. Adiponectin and AMP kinase activator stimulate proliferation, differentiation, and mineralization of osteoblastic MC3T3-E1 cells. BMC Cell Biol. 2007;8:51.
Ye R, Scherer PE. Adiponectin, driver or passenger on the road to insulin sensitivity? Mol Metab. 2013;2(3):133–41.
Lee B, Shao J. Adiponectin and energy homeostasis. Rev Endocr Metab Disord. 2014;15(2):149–56.
Hamrick MW, Ferrari SL. Leptin and the sympathetic connection of fat to bone. Osteoporos Int. 2008;19(7):905–12.
Luo XH, Guo LJ, Xie H, et al. Adiponectin stimulates RANKL and inhibits OPG expression in human osteoblasts through the MAPK signaling pathway. J Bone Miner Res. 2006;21(10):1648–56.
Nissen A, Christensen M, Knop FK, et al. Glucose-dependent insulinotropic polypeptide inhibits bone resorption in humans. J Clin Endocrinol Metab. 2014;99(11):E2325–9.
Zhao C, Liang J, Yang Y, et al. The impact of glucagon-like Peptide-1 on bone metabolism and its possible mechanisms. Front Endocrinol (Lausanne). 2017;8:98.
Funding
The Canadian Institutes of Health Research (MOP 97947), Diabetes Canada and CHU de Québec Foundation provided funding for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
AMC is the recipient of Fonds de recherche du Québec-Santé (FRQ-S) and Diabetes Canada scholarships. ACC is the recipient of the GSK Chair in Diabetes of Université de Sherbrooke. LM reports non-financial support from Roche Diagnostics Canada, personal fees from Amgen, personal fees from Eli Lilly, personal fees from Abbvie, personal fees from Bristol-Myers Squibb, personal fees from Novartis, outside the submitted work. AT and LB receive funding from Johnson Johnson Medical Companies and Medtronic for research studies on bariatric surgery. CG is a clinical research scholar of the FRQ-S and the recipient of a Diabetes Canada New Investigator Award. She received research funding from Technologies Khlôros, and speaker honoraria from Amgen, Eli Lilly, and Janssen. All other authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Turcotte, AF., Grenier-Larouche, T., Ung, RV. et al. Effects of Biliopancreatic Diversion on Bone Turnover Markers and Association with Hormonal Factors in Patients with Severe Obesity. OBES SURG 29, 990–998 (2019). https://doi.org/10.1007/s11695-018-3617-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3617-x