Abstract
Background
Elderly patients with achalasia are more frequently being referred for minimally invasive Heller myotomy (MIM). The associated morbidity and mortality of MIM in the elderly are not well defined. The objective of this study was to review our experience with MIM in the elderly.
Methods
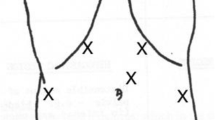
We identified a total of 57 patients (32 men, 25 women) 70 years or older (mean age 78 years, range 70 to 96 years) who underwent MIM [55 laparoscopically (LAP), 2 videothoracoscopically (VATS)] for achalasia at our institution. Clinical outcomes were analyzed including postoperative surgical interventions (redo myotomy, esophagectomy), and dysphagia scores (range: 1, no dysphagia to 5, dysphagia to saliva).
Results
Thirty-seven (59.6%) patients had prior endoscopic therapy. There was no perioperative mortality and median hospital stay was 3 days. There were three (5.3%) conversions to open due to adhesions and concern regarding the viability of the myotomy following repair of a small perforation. A total of 11 (19.3%) patients had complications, including three (5.3%) intraoperative esophageal perforations, three pleural effusions, one (1.8%) pneumonia, one intraoperative gastric perforation, one C. difficile infection, one ileus, and one postoperative intubation. Mean follow-up was 23.5 months. Mean dysphagia score improved from 3.38 preoperatively to 1.36 following MIM (p < 0.0001), with 55 (96.5%) patients experiencing an improvement. Reoperation for recurrent dysphagia was required in four (7.0%) of the patients.
Conclusions
MIM can be performed safely in elderly patients with achalasia in centers with significant experience in laparoscopic foregut surgery. MIM affords similar symptomatic improvement in the elderly as compared to younger patients. MIM should be seriously considered as a therapeutic strategy in elderly achalasia patients.
Similar content being viewed by others
References
St. Peter SD, Swain JM (2003) Achalasia: A comprehensive review. Surg Lap Endosc Perc Tech 13:227–240
Heller E (1913) Extramukose Cardioplastic beim chronishen Cardiospasmus mit Dilatation des Oesophagus. Mitt Grenzeg Med Chir 27:141
Zaaijer JH (1923) Cardiospasm in the aged. Ann Surg 77:615–617
Dor J, Humbert P, Dor V, Figarella J (1962) L’interet de la technique de Nissen modifiee dans la prevention de reflux apres cardiomyotomie extramuqueuse de Heller. Mem Acad Chir 88:877–883
Toupet A (1963) Tehnique d’oesophago-gastroplastie avec phrenicogastropexie appliquee dan la cure radicale des hernias hiatales et comme complement de l’operation d’Heller dans les cardiospasmes. Mem Acad Chir 89:394–399
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, Sharp KW (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia. A prospective, randomized, double-blind clinical trial. Ann Surg 240:405–415
Csendes A, Braghetto I, Henriquez A, Cortes C (1989) Late results of a prospective randomized study comparing forceful dilatation and oesophagomyotomy in patients with achalasia. Gut 30:299–304
Shimi S, Nathanson LK, Cuschieri A (1991) Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb 36:152–154
Pellegrini C, Wetter LA, Patti M, Leichter R, Mussan G, Mori T, Bernstein G, Way L (1992) Thoracoscopic esophagomyotomy. Initial experience with a new approach for the treatment of achalasia. Ann Surg 216:291–296
Luketich JD, Fernando HC, Christie NA, Buenaventura PO, Keenan RJ, Ikramuddin S, Schauer PR (2001) Outcomes after minimally invasive esophagomyotomy. Ann Thorac Surg 72:1909–1912
Sharp KW, Khaitan L, Scholz S, Holzman MD, Richards WO (2002) 100 consecutive minimally invasive Heller myotomies: Lessons learned. Ann Surg 235:631–638
Rosemurgy A, Villadolid D, Thometz D, Kalipersad C, Rakita S, Albrink M, Johnson M, Boyce W (2005) Laparoscopic Heller myotomy provides durable relief from achalasia and salvages failures after botox or dilation. Ann Surg 241:725–733
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanstrom LL (2005) Laparoscopic Heller myotomy with Toupet fundoplication: Outcomes predictors in 121 consecutive patients. Arch Surg 140:827–833
Deb S, Deschamps C, Allen MS, Nichols FC 3rd, Cassivi SD, Crownhart BS, Pairolero PC (2005) Laparoscopic esophageal myotomy for achalasia: factors affecting functional results. Ann Thorac Surg 80:1191–1194
Torquati A, Richards WO, Holzman MD, Sharp KW (2006) Laparoscopic myotomy for achalasia: predictors of successful outcome after 200 cases. Ann Surg 243:587–591
Patti MG, Fisichella PM, Perretta S, Galvani C, Gorodner MV, Robinson T, Way LW (2003) Impact of minimally invasive surgery on the treatment of esophageal achalasia: a decade of change. J Am Coll Surg 196:698–703
Castell DO (1990) Esophageal disorders in the elderly. Gastroenterol Clin North Am 19:235–254
Rakita S, Bloomston M, Villadolid D, Thometz D, Boe B, Rosemurgy A (2005) Age affects presenting symptoms of achalasia and outcomes after myotomy. Am Surg 71:424–429
Eckardt VF, Stauf B, Bernhard G (1999) Chest pain in achalasia: patient characteristics and clinical course. Gastroenterology 116:1300–1304
Bondi JL, Godwin DH, Garrett JM (1972) “Vigorous” achalasia. Its clinical interpretation and significance. Am J Gastroenterol 58:145–155
Adams CW, Brain RH, Ellis FG, Kauntze R, Trounce JR (1961) Achalasia of the cardia. Guy’s Hosp Rep 110:191–236
Goldblum JR, Rice TW, Richter JL (1996) Histopathologic features in esophagomyotomy specimens from patients with achalasia. Gastroenterology 111:648–654
Lasch H, Castell DO, Castell JA (1992) Evidence for diminished visceral pain with aging: Studies using graded intraesophageal balloon distension. Am J Physiol 272:G1–3
Grade A, Pulliam G, Johnson C, Garewal H, Sampliner RE, Fass R (1997) Reduced chemoreceptor sensitivity in patients with Barrett’s esophagus may be related to age and not to the presence of Barrett’s epithelium. Am J Gastroenterol 92:2040–2043
Neubrand M, Scheurlen C, Schepke M, Sauerbruch T (2002) Long-term results and prognostic factors in the treatment of achalasia with botulinum toxin. Endoscopy 34:519–523
Farhoomand K, Connor JT, Richter JE, Achkar E, Vaezi MF (2004) Predictors of outcome of pneumatic dilation in achalasia. Clin Gastroenterol Hepatol 2:389–394
Pasricha PJ, Rai R, Ravich WJ, Hendrix TR, Kalloo AN (1996) Botulinum toxin for achalasia: long-term outcome and predictors of response. Gastroenterology 110:1410–1415
Kolbasnik J, Waterfall WE, Fachnie B, Chen Y, Tougas G (1999) Long-term efficacy of Botulinum toxin in classical achalasia: a prospective study. Am J Gastroenterol 94:3434–3439
Torbey CF, Achkar E, Rice TW, Baker M, Richter JE (1999) Long-term outcome of achalasia treatment: the need for closer follow-up. J Clin Gastroenterol 28:125–130
Karamanolis G, Sgouros S, Karatzias G, Papadopoulou E, Vasiliadis K, Stefanidis G, Mantides A (2005) Long-term outcome of pneumatic dilation in the treatment of achalasia. Am J Gastroenterol 100:270–274
Torquati A, Richards WO, Holzman MD, Sharp KW (2006) Laparoscopic myotomy for achalasia: predictors of successful outcome after 200 cases. Ann Surg 243:587–591
Smith CD, Stival A, Howell DL, Swafford V (2006) Endoscopic therapy for achalasia before Heller myotomy results in worse outcomes than Heller myotomy alone. Ann Surg 243:579–584
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanstrom LL (2005) Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg 140:827–833
Katsinelos P, Kountouras J, Paroutoglou G, Beltsis A, Zavos C, Papaziogas B, Mimidis K (2005) Long-term results of pneumatic dilation for achalasia: a 15 years’ experience. World J Gastroenterol 11:5701–5705
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a poster at the 2007 SAGES Annual Meeting.
Rights and permissions
About this article
Cite this article
Kilic, A., Schuchert, M.J., Pennathur, A. et al. Minimally invasive myotomy for achalasia in the elderly. Surg Endosc 22, 862–865 (2008). https://doi.org/10.1007/s00464-007-9657-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9657-2