Abstract
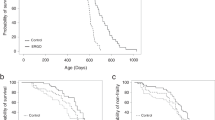
Understanding of the underlying mechanism of epilepsy is desired since some patients fail to control their seizures. The carnitine/organic cation transporter OCTN1/SLC22A4 is expressed in brain neurons and transports food-derived antioxidant ergothioneine (ERGO), l-carnitine, and spermine, all of which may be associated with epilepsy. This study aimed to clarify the possible association of this transporter with epileptic seizures. In both pentylenetetrazole (PTZ)-induced acute seizure and kindling models, ocnt1 gene knockout mice (octn1−/−) showed lower seizure scores compared with wild-type mice. Up-regulation of the epilepsy-related genes, c-fos and Arc, and the neurotrophic factor BDNF following PTZ administration was observed in the hippocampus of wild-type, but not octn1−/− mice. To find the OCTN1 substrate associated with the seizure, untargeted metabolomics analysis using liquid chromatography–quadrupole time-of-flight mass spectrometry was conducted on extracts from the hippocampus, frontal cortex, and plasma of both strains, leading to the identification of a plant alkaloid homostachydrine as a compound present in a lower concentration in octn1−/− mice. OCTN1-mediated uptake of deuterium-labeled homostachydrine was confirmed in OCTN1-transfected HEK293 cells, suggesting that this compound is a substrate of OCTN1. Homostachydrine administration increased PTZ-induced acute seizure scores and the expression of Arc in the hippocampus and that of Arc, Egr1, and BDNF in the frontal cortex. Conversely, administration of the OCTN1 substrate/inhibitor ERGO inhibited PTZ-induced kindling and reduced the plasma homostachydrine concentration. Thus, these results suggest that OCTN1 is at least partially associated with PTZ-induced seizures, which is potentially deteriorated by treatment with homostachydrine, a newly identified food-derived OCTN1 substrate.







Similar content being viewed by others
Data Availability
The datasets used or analyzed during this study are available from the corresponding author upon reasonable request.
References
Wang J, Lin Z-J, Liu L et al (2017) Epilepsy-associated genes. Seizure 44:11–20. https://doi.org/10.1016/j.seizure.2016.11.030
Mattison KA, Butler KM, Inglis GAS et al (2018) SLC6A1 variants identified in epilepsy patients reduce γ-aminobutyric acid transport. Epilepsia 59:e135–e141. https://doi.org/10.1111/epi.14531
Koch H, Weber YG (2019) The glucose transporter type 1 (Glut1) syndromes. Epilepsy Behav 91:90–93. https://doi.org/10.1016/j.yebeh.2018.06.010
Tian N, Boring M, Kobau R et al (2018) Active epilepsy and seizure control in adults—United States, 2013 and 2015. Morb Mortal Wkly Rep 67:437–442. https://doi.org/10.15585/mmwr.mm6715a1
Gründemann D, Harlfinger S, Golz S et al (2005) Discovery of the ergothioneine transporter. Proc Natl Acad Sci USA 102:5256–5261. https://doi.org/10.1073/pnas.0408624102
Tamai I, Ohashi R, Nezu JI et al (2000) Molecular and functional characterization of organic cation/carnitine transporter family in mice. J Biol Chem 275:40064–40072. https://doi.org/10.1074/jbc.M005340200
Bacher P, Giersiefer S, Bach M et al (2009) Substrate discrimination by ergothioneine transporter SLC22A4 and carnitine transporter SLC22A5: gain-of-function by interchange of selected amino acids. Biochim Biophys Acta 1788:2594–2602. https://doi.org/10.1016/j.bbamem.2009.09.019
Masuo Y, Ohba Y, Yamada K et al (2018) Combination metabolomics approach for identifying endogenous substrates of carnitine/organic cation transporter OCTN1. Pharm Res 35:224. https://doi.org/10.1007/s11095-018-2507-1
Pochini L, Scalise M, Galluccio M et al (2012) The human OCTN1 (SLC22A4) reconstituted in liposomes catalyzes acetylcholine transport which is defective in the mutant L503F associated to the Crohn’s disease. Biochim Biophys Acta - Biomembr 1818:559–565. https://doi.org/10.1016/j.bbamem.2011.12.014
Kato Y, Kubo Y, Iwata D et al (2010) Gene knockout and metabolome analysis of carnitine/organic cation transporter OCTN1. Pharm Res 27:832–840. https://doi.org/10.1007/s11095-010-0076-z
Ishimoto T, Nakamichi N, Hosotani H et al (2014) Organic cation transporter-mediated ergothioneine uptake in mouse neural progenitor cells suppresses proliferation and promotes differentiation into neurons. PLoS ONE 9:e89434. https://doi.org/10.1371/journal.pone.0089434
Ishimoto T, Nakamichi N, Nishijima H et al (2018) Carnitine/organic cation transporter OCTN1 negatively regulates activation in murine cultured microglial cells. Neurochem Res 43:107–119. https://doi.org/10.1007/s11064-017-2350-5
Nakamichi N, Nakao S, Nishiyama M et al (2020) Oral administration of the food derived hydrophilic antioxidant ergothioneine enhances object recognition memory in mice. Curr Mol Pharmacol 13:1121–1132. https://doi.org/10.2174/1874467213666200212102710
Pearson-Smith J, Patel M (2017) Metabolic dysfunction and oxidative stress in epilepsy. Int J Mol Sci 18:2365. https://doi.org/10.3390/ijms18112365
Mehvari J, Motlagh F, Najafi M et al (2016) Effects of Vitamin E on seizure frequency, electroencephalogram findings, and oxidative stress status of refractory epileptic patients. Adv Biomed Res 5:36. https://doi.org/10.4103/2277-9175.178780
Banach M, Gurdziel E, Jędrych M, Borowicz KK (2011) Melatonin in experimental seizures and epilepsy. Pharmacol Rep 63:1–11. https://doi.org/10.1016/S1734-1140(11)70393-0
Halliwell B, Cheah IK, Tang RMY (2018) Ergothioneine – a diet-derived antioxidant with therapeutic potential. FEBS Lett 592:3357–3366
Kumar M, Kumar P (2017) Protective effect of spermine against pentylenetetrazole kindling epilepsy induced comorbidities in mice. Neurosci Res 120:8–17. https://doi.org/10.1016/j.neures.2017.02.003
Hussein A, Adel M, El-Mesery M et al (2018) l-carnitine modulates epileptic seizures in pentylenetetrazole-kindled rats via suppression of apoptosis and autophagy and upregulation of Hsp70. Brain Sci 8:45. https://doi.org/10.3390/brainsci8030045
Becchetti A, Aracri P, Meneghini S et al (2015) The role of nicotinic acetylcholine receptors in autosomal dominant nocturnal frontal lobe epilepsy. Front Physiol 6:22. https://doi.org/10.3389/fphys.2015.00022
Servillo L, Giovane A, Balestrieri ML et al (2012) Occurrence of pipecolic acid and pipecolic acid betaine (Homostachydrine) in citrus genus plants. J Agric Food Chem 60:315–321. https://doi.org/10.1021/jf204286r
Claycomb RJ, Hewett SJ, Hewett JA (2011) Prophylactic, prandial rofecoxib treatment lacks efficacy against acute PTZ-induced seizure generation and kindling acquisition. Epilepsia 52:273–283. https://doi.org/10.1111/j.1528-1167.2010.02889.x
Binder DK, Croll SD, Gall CM, Scharfman HE (2001) BDNF and epilepsy: too much of a good thing? Trends Neurosci 24:47–53. https://doi.org/10.1016/S0166-2236(00)01682-9
Morimoto K, Fahnestock M, Racine RJ (2004) Kindling and status epilepticus models of epilepsy: rewiring the brain. Prog Neurobiol 73:1–60. https://doi.org/10.1016/j.pneurobio.2004.03.009
Servillo L, D’Onofrio N, Giovane A et al (2018) The betaine profile of cereal flours unveils new and uncommon betaines. Food Chem 239:234–241. https://doi.org/10.1016/j.foodchem.2017.06.111
Wood KV, Stringham KJ, Smith DL et al (1991) Betaines of alfalfa: characterization by fast atom bombardment and desorption chemical ionization mass spectrometry. Plant Physiol 96:892–897. https://doi.org/10.1104/pp.96.3.892
Essery JM, McCaldint DJ, Marion L (1962) The biogenesis of stachydrine. Phytochemistry 1:209–213. https://doi.org/10.1016/S0031-9422(00)82824-1
Yang J, Yan B, Zhao B et al (2020) Assessing the causal effects of human serum metabolites on 5 major psychiatric disorders. Schizophr Bull 46:804–813. https://doi.org/10.1093/schbul/sbz138
Mangalam A, Poisson L, Nemutlu E et al (2013) Profile of circulatory metabolites in a relapsing-remitting animal model of multiple sclerosis using global metabolomics. J Clin Cell Immunol 4:1000150. https://doi.org/10.4172/2155-9899.1000150
Plecko B, Stöckler-Ipsiroglu S, Paschke E et al (2000) Pipecolic acid elevation in plasma and cerebrospinal fluid of two patients with pyridoxine-dependent epilepsy. Ann Neurol 48:121–125. https://doi.org/10.1002/1531-8249(200007)48:1<121:AID-ANA20>3.0.CO;2-V
Chang Y-F, Hargest V, Chen J-S (1988) Modulation of benzodiazepine by lysine and pipecolic acid on pentylenetetrazol-induced seizures. Life Sci 43:1177–1188. https://doi.org/10.1016/0024-3205(88)90207-X
Gutiérrez MC, Delgado-Coello BA (1989) Influence of pipecolic acid on the release and uptake of [3H]GABA from brain slices of mouse cerebral cortex. Neurochem Res 14:405–408. https://doi.org/10.1007/BF00964852
Tuomainen M, Kärkkäinen O, Leppänen J et al (2019) Quantitative assessment of betainized compounds and associations with dietary and metabolic biomarkers in the randomized study of the healthy Nordic diet (SYSDIET). Am J Clin Nutr 110:1108–1118. https://doi.org/10.1093/ajcn/nqz179
Kärkkäinen O, Lankinen MA, Vitale M et al (2018) Diets rich in whole grains increase betainized compounds associated with glucose metabolism. Am J Clin Nutr 108:971–979. https://doi.org/10.1093/ajcn/nqy169
Derkach A, Sampson J, Joseph J et al (2017) Effects of dietary sodium on metabolites: the Dietary Approaches to Stop Hypertension (DASH)–Sodium Feeding Study. Am J Clin Nutr 106:1131–1141. https://doi.org/10.3945/ajcn.116.150136
Tunón H, Thorsell W, Bohlin L (1994) Mosquito repelling activity of compounds occurring in Achillea millefolium L. (asteraceae). Econ Bot 48:111–120. https://doi.org/10.1007/BF02908196
Urban TJ, Yang C, Lagpacan LL et al (2007) Functional effects of protein sequence polymorphisms in the organic cation/ergothioneine transporter OCTN1 (SLC22A4). Pharmacogenet Genomics 17:773–782. https://doi.org/10.1097/FPC.0b013e3281c6d08e
Futatsugi A, Masuo Y, Kawabata S et al (2016) L503F variant of carnitine/organic cation transporter 1 efficiently transports metformin and other biguanides. J Pharm Pharmacol 68:1160–1169. https://doi.org/10.1111/jphp.12574
Peltekova VD, Wintle RF, Rubin LA et al (2004) Functional variants of OCTN cation transporter genes are associated with Crohn disease. Nat Genet 36:471–475. https://doi.org/10.1038/ng1339
Genghof DS (1970) Biosynthesis of ergothioneine and hercynine by fungi and actinomycetales. J Bacteriol 103:475–478. https://doi.org/10.1128/JB.103.2.475-478.1970
Song T-Y, Chen C-L, Liao J-W et al (2010) Ergothioneine protects against neuronal injury induced by cisplatin both in vitro and in vivo. Food Chem Toxicol 48:3492–3499. https://doi.org/10.1016/j.fct.2010.09.030
Yang N-C, Lin H-C, Wu J-H et al (2012) Ergothioneine protects against neuronal injury induced by β-amyloid in mice. Food Chem Toxicol 50:3902–3911. https://doi.org/10.1016/j.fct.2012.08.021
Boeve BF, Silber MH, Ferman TJ (2003) Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: results in 14 patients. Sleep Med 4:281–284. https://doi.org/10.1016/S1389-9457(03)00072-8
Cheah IK, Tang RMY, Yew TSZ et al (2017) Administration of pure ergothioneine to healthy human subjects: uptake, metabolism, and effects on biomarkers of oxidative damage and inflammation. Antioxid Redox Signal 26:193–206. https://doi.org/10.1089/ars.2016.6778
Harpsøe NG, Andersen LPH, Gögenur I, Rosenberg J (2015) Clinical pharmacokinetics of melatonin: a systematic review. Eur J Clin Pharmacol 71:901–909. https://doi.org/10.1007/s00228-015-1873-4
Funding
Grants-in-Aid for Scientific Research to Noritaka Nakamichi (No. 19K07126) and Yukio Kato (No. 15H04664) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, and grant by the Hoansha Foundation (Osaka, Japan) to Yukio Kato.
Author information
Authors and Affiliations
Contributions
Conceptualization: MN, NN, YK. Methodology: NN, TY, YM, YK. Analysis and investigation: MN, TY, TK, YM. Writing—original draft preparation: MN, TK, TY. Writing, review, and editing: NN, TI, YK. Funding acquisition: NN, YK. Resources: YK. Supervision: NN, JM, YK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical Approval
Experiments were performed according to the Guidelines for the Care and Use of Laboratory Animals at Kanazawa University. All protocols were approved by the Institutional Animal Care and Use Committee of Kanazawa University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nishiyama, M., Nakamichi, N., Yoshimura, T. et al. Homostachydrine is a Xenobiotic Substrate of OCTN1/SLC22A4 and Potentially Sensitizes Pentylenetetrazole-Induced Seizures in Mice. Neurochem Res 45, 2664–2678 (2020). https://doi.org/10.1007/s11064-020-03118-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-020-03118-8