Abstract
Most commonly occurring in elderly patients, the comminuted 4-part or Neer VI type proximal humerus fractures frequently necessitate complete shoulder replacement. Despite the recent advances in imaging technologies, there is still a need for more information about the degree of joint degeneration and changes of the collagen content of tendons to select the proper implant type. It is known that human long head biceps tendon subjected to synovial inflammation and mechanical wear could result in tear and structural damage. Differential scanning calorimetry has already been demonstrated to be a dependable in the assessment of collagen in degenerative tendon conditions. The purpose of the study was to determine whether variations in thermal parameters detected by DSC are related to the degenerative changes of LHBT samples. LHBT tendons were collected from patients who had reversed shoulder arthroplasty because of trauma. DSC was utilized to measure the thermodynamic changes. Macroscopical, radiological and histological assessment were also performed. Based on the thermal parameters and denaturation curves, LHBT samples collected of patients underwent reversed shoulder arthroplasty due to comminuted proximal humerus fracture have shown minimal or mild degenerative injuries. These data were supported by preoperative radiological examination and histological analysis. The authors suggest that DSC could be a useful investigative tool in the clinical evaluation of tendon injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The degenerative diseases of glenohumeral joints often lead to the need for total shoulder replacement [1]. Another indication for shoulder arthroplasty is displaced, comminuted fractures of the proximal humerus, mostly affecting the older population [2].
The degenerative process in the shoulder described by damage of cartilage and tendons, chronic rotator cuff tear, decreased quality of bone and impaired blood perfusion due to a generally aged biology [3]. The long head of the biceps tendon arises from the supraglenoid tubercle of the scapula and passes through the shoulder joint and the intertubercular groove of the humerus. Then, both heads of the biceps tendon unite distally to form a single muscle belly. Besides its functions as a supinator and flexor of the forearm, the biceps muscle plays a partial, usually a weak role in the forward flexion and abductions of the glenohumeral joint [4]. Because a biceps tendon subluxation or tear could result in rotator cuff damage, it is an indicator of the degenerative level of the glenohumeral joint as well [5, 6].
Collagens are abundant elements of tendons. Under pathologic conditions, the ratio of collagen type III to collagen type I increases [7]. Osteoarthritis accompanied with synovial inflammation may cause histomorphologic changes in the structure of the biceps tendon. Therefore, evaluation of collagen content of the long head of biceps tendon (LHBT) could provide relevant information on the degenerative changes of the tendon and the shoulder joint.
Recently, differential scanning calorimetry (DSC) has been applied to measure the thermoanalytical parameters of different type of tendons [8,9,10,11]. The changes of thermal characteristics have been proven as relevant indicators of conformational deterioration of collagen structure in different pathologic conditions.
The purpose of our investigation was to determine whether changes of thermal parameters detected with differential scanning calorimetry correlates with the degenerative alteration of human long head biceps samples, collected from patients underwent reversed shoulder arthroplasty with trauma indications.
Materials and methods
Sample collection
Patients undergoing reversed shoulder arthroplasty due to 4-part or Neer Type VI (AO/ASIF 11 C3.2–C3.3 proximal humerus factures were included to the study. The 5 × 5 × 10 mm part of the intra-articular portion of the biceps tendon was resected during reversed shoulder replacement. Detachment and tenodesis of this part of LHBT is a standard surgical procedure during shoulder replacements. Then the samples were preserved for further measurements as detailed elsewhere [11,12,13]. The control sample was taken from a macroscopically healthy segment of a biceps tendon, confirmed by histological examination.
All procedures followed were in accordance with the ethical standards of the relevant regional and institutional research ethics committees and with the 1975 Declaration of Helsinki as revised in 2008.
Clinical and radiological evaluation of rotator cuff damage
The biceps tendons were macroscopically examined during surgery to look for evidence of previous injury or degenerative changes. The Hamada classification [14] was used to assess rotator cuff tendon damage, while the Walch [15] and Outerbridge [16] classifications were used to assess primary arthropathies and cartilage damage, respectively. Radiological evaluation of conventional X-ray, CT and MRI images was performed using Siemens Syngo.via software (Siemens Healthineers Global).
Histological processing
The samples of biceps tendon were fixed in 4% formaldehyde for at least 2 days. Two representative sections from each sample were cut after fixation. Following standard histopathological processing, the tissues were dehydrated and embedded in paraffin before being cut into 4 μm thick sections using a microtome. Then hematoxylin–eosin was used to stain the slides.
DSC measurements
The stored samples were washed three times in normal saline and kept in sterile isotonic saline at 4 °C until the calorimetric tests began (max. half an hour). A SETARAM Micro DSC-II calorimeter was used to take measurements between 0 and 100 °C at a heating rate of 0.3 K min−1. The thermal denaturation was carried out in conventional closed Hastelloy batch vessels (V = 1 mL). In the case of traumatic patients, the sample masses ranged from 80 to 295 mg. The healthy control mass ranged from 200 to 220 mg. As a reference, normal saline was used. The calorimetric enthalpy was calculated from the area under the heat absorption curve using a two-point setting of the SETARAM peak integration, and then the other thermal parameters: denaturation or melting temperature (Tm), range of denaturation (ΔT), half width of transition (T1/2), and calorimetry enthalpy (ΔHcal) were compared.
Results
Patient demographics
The mean age of patients enrolled in the study was 71 ± 7 years (mean ± SEM) with a male to female ratio: 1/5. All patients suffered proximal humerus fractures due to low energy traumas, mostly domestic falls.
Macroscopic assessment
The macroscopic scoring was performed immediately after collection, based the evaluation criteria published by Szabó et al. [6]. In healthy tendons, the surfaces are smooth and the cross-sectional areas are oval. In the case of slight damage, the cross section is gently widened and flattened, and there were slight scabrous erosions on the surfaces. The severely damaged tendons showed more flattening and widening with hard scabrous erosions on the surface. The macroscopical evaluation of biceps samples, collected from the proximal intraarticular part of the tendons close to the bicipital groove, showed signs a minimal to a moderate level of damage. The average score was 2 ± 0.4 (mean ± SEM).
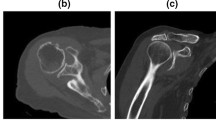
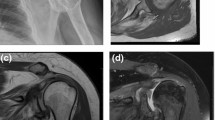
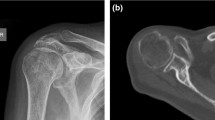
Radiological assessment
Based on osteoarthritis score, we have found only a minimal level of glenohumeral arthritis on the examined shoulders X-rays. Due to the comminuted fracture morphology, Walch and Hamada classifications could only have been used in a limited number of cases. However, these scores (B1, characterized by narrowing of the posterior articular space, subchondral sclerosis, and presence of osteophytes) indicated only a mild degree of glenohumeral osteoarthritis.
Histological analysis
The analyses of histological sections are shown in Table 1. The average histological score, based on the tissue damaged of harvested biceps tendon, was 1.15 ± 0.75 (mean ± SEM). Comparing to the radiological and macroscopic evaluation, the histological analysis demonstrated the highest grade of degenerative changes but it showed a relatively high level variability (see Fig. 1).
Calorimetric analysis
The average of the melting temperature of T1–T5 trauma samples (without T2) showed a minimal increase, compared to the Control sample (63.94 ± 0.57 °C vs. 63.55 °C, mean ± SEM). The difference between T2 and T1, ΔT was moderately lower in the trauma samples versus Control (14.05 ± 0.76 °C vs. 18.6 °C, see Table 2).
However, T1/2 (half width of denaturation) showed an increase in the trauma samples (2.19 ± 0.21 °C vs. 2.02 °C), similarly to the changes of the calorimetric enthalpy (5.12 ± 0.53 Jg−1 vs. 5.01 Jg−1). The increase in T1/2 and widening of gap between T2 and T1 generally indicates a less cooperative, therefore, less stable collagen formation. These relatively moderate changes in the T1/2 and Tm could be explained by the similarly small or moderate level of degeneration, detected by macroscopic, radiological and histological examinations. The mildly elevated calorimetric enthalpy may indicate a higher level of stability or an initial stage of degeneration and consequential start of scar formation (see Fig. 2).
In selected cases, an additional thermodynamic effect was observed in the higher temperature range during the control heating cycle (data are not shown). It can be caused by either the incomplete denaturation of the collagen, or, the samples were contaminated with another type of tissue.
Discussion
There is an increasing number of shoulder arthroplasties performed every year. The selection of the proper type of implant requires detailed knowledge about the degree of osteoarthritis and condition of the ROC and biceps tendon [17, 18]. For preoperative planning, CT, US and MRI examinations are available. However, there is still more information is needed about the stage of joint degeneration and changes of the collagen content of tendons.
Recently, differential scanning calorimetry has been introduced to evaluate the degenerative or inflammatory condition of different type of tendons. Wiegand et al. [19] have found that the thermal parameters of human carpal transverse ligament correlated with the degenerative changes, confirmed by histological examinations. Based on their results, the timing of surgery of carpal tunnel syndrome can be further optimized.
Furthermore, ruptured Achilles tendon, patellar ligament and quadriceps ligament samples were collected intraoperatively during reconstructive surgery. Their research supported our findings and showed distinct differences between the control and the torn tendons (control: Tm = 59.7 °C, T1/2 = 1.4 °C and ΔHcal = 8.54 J g−1; torn Achilles tendon: Tm = 62.75 °C, T1/2 = 2.6 °C and ΔHcal = 1.54 J g−1). Authors concluded that degenerative changes of collagen content led to enhanced thermal stability of the collagen components of the tendons [8].
It is known that the long head of the biceps tendon, a dense fibrosus connective tissue, contains cc. 80% type I collagen. Due to fraying, partial or complete tears and chronic inflammation, there will be a change in the collagen formation. Later on, the fibrosus form of collagen will turn into scar.
In our set of experiments, we have found a generally increased T1/2 and widening of gap between T2 and T1, compared to the control sample. These data suggest a less cooperative and more unstable collagen formation. Consistently, we could demonstrate mostly minimal or moderate degenerative tendon injuries with histomorphology. In addition, we have found a mildly elevated calorimetric enthalpy in partially damaged biceps tendons, indicating an initial stage of degeneration with start of scar formation. It is supporting our theory that trauma patient undergoing shoulder replacement because of comminuted humerus fracture exhibit less degenerative tendon damages, compared to orthopedic patients with rotator cuff tear arthropathy (RCA) or osteoarthritis (OA) [20, 21]. Notably, the acute trauma itself may not be responsible for significant damage in the protein structure of biceps tendon.
In a previous study, Szabó et al. [6] compared the thermal parameters of long biceps tendon specimens at various stages of injury. The thermal results were the mirror of macroscopic findings and histomorphologic changes. However, it is important to note that in our experiments, intraoperatively, in vivo collected samples were utilized. Meanwhile, Szabó et al. analyzed LHBT with cadaver origin and pathologic changes without signs of acute trauma. Contrary, in our study, LHBT samples were harvested of patients who suffered comminuted 4-part or Neer VI type proximal humerus fractures.
One of the limiting factors of the study is that we have processed a relatively small number of samples. However, our results clearly indicate the differences between the control and trauma groups. To keep the population homogeneous, patients undergoing hemiarthroplasty were excluded from our current study. The indication for shoulder hemiarthroplasty includes a relatively young age, an intact rotator cuff and no evidence of osteoarthritis [22,23,24]. Since we plan to process LHBT samples from orthopedic patients undergoing total shoulder replacement, the different nature of the surgical procedures would introduce another variable and a comparison of the hemiarthroplasty and reversed arthroplasty groups might not be feasible.
Another limitation is that MRI or CT evaluation have not been performed in all cases. Our preoperative planning protocol involves CT-scan in all trauma patients; but the classifications have mostly been developed to score orthopedic, and not trauma cases. Additionally, MRI scanning can be contraindicated due to older metal implants or claustrophobia. Nevertheless, histological examination was done to confirm our findings.
Conclusions
Based on changes of thermodynamic parameters, LHBT samples collected of patients underwent reversed shoulder arthroplasty due to comminuted proximal humerus fracture have shown minimal or mild degenerative injuries. These findings were supported by radiological and histological examinations. The authors suggest that DSC could be a useful investigative tool in the clinical evaluation of tendon injuries.
Data availability
There are no additional available data to upload.
References
Smith CD, Guyver P, Bunker TD. Indications for reverse shoulder replacement: a systematic review. J Bone Joint Surg Br Engl. 2012;94:577–83.
Yahuaca BI, Simon P, Christmas KN, Patel S, Gorman RA, Mighell MA, et al. Acute surgical management of proximal humerus fractures ORIF vs. hemiarthroplasty vs. reverse shoulder arthroplasty. J Shoulder Elb Surg USA. 2020;29:32–40.
Cavalier M, Jullion S, Kany J, Grimberg J, Lefebvre Y, Oudet D, et al. Management of massive rotator cuff tears: prospective study in 218 patients. Orthop Traumatol Surg Res France. 2018;104:S193–7.
Halder AM, Itoi E, An KN. Anatomy and biomechanics of the shoulder. Orthop Clin North Am US. 2000;31:159–76.
Gaskill TR, Braun S, Millett PJ. Multimedia article. The rotator interval: pathology and management. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc North Am Int Arthrosc Assoc US. 2011;27:556–67.
Szabó I, Bognár G, Kereskai L, Szász K, Lőrinczy D. Differentialscanning calorimetric and histological examinations of the long head of thebiceps in cadavers. J Therm Anal Calorim. 2007;88:343–9.
Thankam FG, Evan DK, Agrawal DK, Dilisio MF. Collagen type III content of the long head of the biceps tendon as an indicator of glenohumeral arthritis. Mol Cell Biochem Neth. 2019;454:25–31.
Wiegand N, Vámhidy L, Lőrinczy D. Differential scanning calorimetric examination of ruptured lower limb tendons in human. J Therm Anal Calorim. 2010;101:487–92.
Wiegand N, Naumov I, Vámhidy L, Kereskai L, Lőrinczy D, Nöt LG. Comparative calorimetric analysis of 13 different types of human healthy and pathologic collagen tissues. Thermochim Acta. 2013;568:171–4.
Nöt LG, Naumov I, Vámhidy L, Lőrinczy D, Wiegand N. Comparison of thermal characteristics of degenerated and inflamed human collagen structures with differential scanning calorimetry. J Therm Anal Calorim. 2013;113:273–9.
Nöt LG, Bata A, Szabó H, Cifra J, Lőrinczy D. DSC examination of rotator cuff damage in patients with total shoulder arthroplasty. J Therm Anal Calorim. 2021;146:165–70.
Bűcs G, Nőt LG, Dandé KL, Lőrinczy D. Calorimetric examination of hip pseudo-capsule after secondary hip surgeries. J Therm Anal Calorim. 2019;138:397–400.
Dandé Á, Kocsis B, Lőrinczy D. Thermal analysis of synovial fluids in different stages of osteoarthritis and after bacterial infections. J Therm Anal Calorim. 2020;142:797–808.
Brolin TJ, Updegrove GF, Horneff JG. Classifications in brief: hamada classification of massive rotator cuff tears. Clin Orthop Relat Res. 2017;475:2819–23.
Bercik MJ, Kruse K 2nd, Yalizis M, Gauci M-O, Chaoui J, Walch G. A modification to the Walch classification of the glenoid in primary glenohumeral osteoarthritis using three-dimensional imaging. J shoulder Elb Surg US. 2016;25:1601–6.
Slattery C, Kweon CY. Classifications in brief: outerbridge classification of chondral lesions. Clin Orthop Relat Res. 2018;476:2101–4.
Bata A, Nöt LG, Szabó H, Cifra J, Lőrinczy D. DSC examination of cartilage damage of patients undergoing shoulder replacement. J Therm Anal Calorim. 2022;147:1275–80.
Bata A, Nöt LG, Szabó H, Cifra J, Lőrinczy D. Thermogravimetric analysis of cancellous bone of humerus head in patients undergoing total shoulder arthroplasty. J Therm Anal Calorim. 2022;147:3107–15.
Wiegand N, Vámhidy L, Patczai B, Dömse E, Than P, Kereskai L, et al. Differential scanning calorimetric examination of transverse carpal ligament in carpal tunnel disease. J Therm Anal Calorim. 2009;95:793–6.
Lindbloom BJ, Christmas KN, Downes K, Simon P, McLendon PB, Hess AV 2nd, et al. Is there a relationship between preoperative diagnosis and clinical outcomes in reverse shoulder arthroplasty? An experience in 699 shoulders. J Shoulder Elb Surg US. 2019;28:S110–7.
Waterman BR, Dean RS, Naylor AJ, Otte RS, Sumner-Parilla SA, Romeo AA, et al. Comparative clinical outcomes of reverse total shoulder arthroplasty for primary cuff tear arthropathy versus severe glenohumeral osteoarthritis with intact rotator cuff: a matched-cohort analysis. J Am Acad Orthop Surg. 2020;28:e1042–8.
Schultz BJ, Lowe DT, Egol KA, Zuckerman JD. Shoulder hemiarthroplasty for proximal humerus fracture. J Orthop Trauma. 2021;35:S3-4.
Shukla DR, McAnany S, Kim J, Overley S, Parsons BO. Hemiarthroplasty versus reverse shoulder arthroplasty for treatment of proximal humeral fractures: a meta-analysis. J Shoulder Elb Surg. 2016;25:330–40.
Jonsson EÖ, Ekholm C, Salomonsson B, Demir Y, Olerud P. Reverse total shoulder arthroplasty provides better shoulder function than hemiarthroplasty for displaced 3- and 4-part proximal humeral fractures in patients aged 70 years or older: a multicenter randomized controlled trial. J Shoulder Elb Surg. 2021;30:994–1006.
Acknowledgements
This work was supported by CO-272 (OTKA) Grant (D.L.).
Funding
Open access funding provided by University of Pécs.
Author information
Authors and Affiliations
Contributions
Dr. L.G.N. contributed to operations, sample collection and handling, data analysis, manuscript writing. Dr. A.B. contributed to sample collection and handling, data analysis. Dr. Z.L. contributed to sample collection and handling, data analysis. Dr. H.S. contributed to radiological evaluation. Dr. J.C. contributed to histological examination. Prof. Dr. D.L., corresponding author, principle investigator, contributed to DSC experiments, data analysis, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Consent for publication
Copyright form has been uploaded with the manuscript.
Ethics approval
All procedures followed were approved and in accordance with the ethical standards of the responsible committee on animal experimentation (institutional and national) and with the revised Helsinki Declaration of 1975.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nöt, L.G., Bata, A., Lábas, Z. et al. Thermal analysis of the biceps tendon samples obtained from patients underwent reversed shoulder arthroplasty for comminuted proximal humerus fractures. J Therm Anal Calorim 147, 13389–13394 (2022). https://doi.org/10.1007/s10973-022-11595-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10973-022-11595-y