Abstract
Technologies for minimally-invasive cardiac output measurement in patients during surgery remain little used in routine practice. We tested a redeveloped system based on CO2 elimination (VCO2) by the lungs for use in ventilated patients, which can be seamlessly integrated into a modern anesthesia/monitoring platform, and provides automated, continuous breath-by-breath cardiac output monitoring. A prototype measurement system was constructed to measure VCO2 and end-tidal CO2 concentration with each breath. A baseline measurement of non-shunt cardiac output was made during a brief oscillating change in ventilator rate, according to the differential CO2 Fick approach and repeated at 5–10 min intervals. Continuous breath-by-breath monitoring of cardiac output was performed between these intervals from measurement of VCO2, using a derivation of the Fick equation applied to pulmonary CO2 elimination and cardiac output displayed in real time. Measurements were compared with simultaneous measurements by thermodilution in 50 patients undergoing cardiac surgery or liver transplantation. Overall mean bias [sd] for agreement in cardiac output measurement was − 0.3 [1.1] L/min, percentage error ± 38.7%, intraclass correlation coefficient = 0.91. Concordance in measurement of changes of at least 15% in cardiac output was 81.4%, with a mean angular bias of − 1.7°, and radial limits of agreement of ± 76.2° on polar plot analysis. The accuracy and precision compared favourably to other clinical techniques. The method is relatively seamless and automated and has potential for continuous, cardiac output monitoring in ventilated patients during anesthesia and critical care.
Similar content being viewed by others
1 Introduction
There is a growing body of evidence suggesting that advanced haemodynamic monitoring and “goal directed” fluid and haemodynamic management strategies may improve patient outcomes in major surgery [1, 2]. However, despite a variety of available technologies, this has not achieved widespread use in clinical practice [3]. Reasons for this may include the cost and complexity of these technologies, which generally require additional stand alone monitors and peripherals such as transducers and connectors, and can be labour intensive to the operator, as well as concerns about the reliability of measurement provided [4, 5].
Available technologies for minimally invasive cardiac output measurement include techniques based on measured carbon dioxide (CO2) elimination and the differential Fick principle, where a step change in alveolar ventilation rate is made. This is the principle of the partial CO2 rebreathing technique, commercialized in the form of the Novametrix/Respironics NICO and CO2SMO+, and now the Philips NM3 (Philips Corp, USA), which use a rebreathing loop with automated opening valve place near the Y-piece of the patient’s breathing system to produce the change.
We have previously published results of Phase 2 clinical studies of a prototype system termed capnotracking which delivers fully automated, continuous cardiac output monitoring from measured CO2 elimination in ventilated patients [6, 7]. The system involves an automated “calibration” ventilatory manoeuvre similar to that first described by Gedeon et al. [8] where alveolar ventilation rate is changed by altering respiratory rate and inspiratory to expiratory (I:E) ratio to obtain a baseline measurement of effective, non-shunt pulmonary capillary blood flow, followed by continuous tracking of changes in pulmonary blood flow from measured CO2 elimination rate and end-tidal partial pressure. The advantages of the method is that it does not require a rebreathing loop or additional attachments or hardware, utilizing components already integrated in standard modern anaesthesia machines, and is therefore relatively seamless, which would allow it to be readily made a routine function in anaesthesia delivery. The system provided accuracy and precision of agreement with right heart thermodilution similar to other more invasive or cumbersome technologies [4, 6, 7].
We developed an algorithm intended to improve the cardiac output measurement precision of the capnotracking method. These changes included more frequent and prolonged “calibration” ventilatory manoeuvres with concurrent measurement of estimated effective lung volume from CO2 washin and washout, to obtain more precise calibration cardiac outputs, and incorporation of a previously described, non-invasive approach to estimation of unmeasured pulmonary shunt fraction [9]. The accuracy and precision of this system was tested under clinical conditions in patients undergoing major surgery by comparison of cardiac output measurements with those obtained from thermodilution. Given the potential limitations of a method based on lung gas exchange, we also sought evidence that its reliability was affected by patients’ preoperative lung function.
2 Materials and methods
With local institutional ethics approval (HREC 03432, 2009), adult patients were recruited to the current series, who were scheduled to undergo either elective cardiac surgery or orthotopic liver transplantation (OLTx). Exclusion criteria were the presence of clinical contraindications to insertion of a pulmonary artery catheter (PAC) or its use for thermodilution cardiac output measurement (severe tricuspid regurgitation, known intracardiac shunt, history of severe or recurrent ventricular arrhythmias). Routine anesthetic management and monitoring for these surgeries was undertaken including insertion of an arterial line and continuous “CCO Combo” pulmonary artery catheter (Edwards Lifesciences, Irvine, CA, USA), with floatation and correct position in the pulmonary artery performed using real-time pressure monitoring, with further confirmation using trans-oesophageal echocardiography in cardiac surgery patients where required. After relaxant general anesthesia was induced and following endotracheal intubation, anesthesia was maintained by either or both of intravenous propofol or inspired volatile anaesthetic agent, titrated according to clinical indication and bi-spectral index, and a neuromuscular blocker. The patient was ventilated with oxygen/air, with tidal volumes of 7–10 mL/kg and 4 mmHg positive end-expiratory pressure, at a minute ventilation adjusted to achieve an end-tidal CO2 partial pressure of 25–35 mmHg. After several minutes, when the patient’s induction had been completed and ventilation commenced, the gas exchange measurement system (pneumotachograph and gas sampling port) was attached to breathing system just proximal to the breathing filter, and the measurement process was started.
Data was collected for a minimum of 30 min or until run onto cardio-pulmonary bypass (CPB) in patients undergoing on-pump cardiac surgery. In this group, where logistic and time constraints permitted, the measurement process was recommenced after separation from CPB and re-establishment of circulation and ventilation of the lungs. Data was again collected for a minimum of 30 min or until separation from the ventilator for transfer to the intensive care unit.
2.1 Measurement system
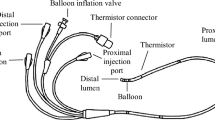
The measurement system consisted of a CO2SMO+ inline infrared capnograph transducer and differential pressure pneumotachograph (Novametrix/Respironics USA), placed just proximal to the breathing circuit filter, interfaced via an RS232 serial cable to a notebook computer (MacBook Pro, Apple Corp. Cupertino, CA, USA). Ventilation was provided by an Ohmeda 7800 patient ventilator (Datex-Ohmeda, Helsinki, Finland) modified to run under real time computer controlled manipulation of tidal volume, breath rate, and I:E ratio, by replacing the existing analog potentiometer inputs with digitally controllable potentiometers (MCP42010, Microchip Technology Inc. Arizona USA). The MCP42010 was controlled by an ATMEGA8535 microcontroller (Atmel Corporation, San Jose, CA, USA) which relayed user parameters communicated over a USB connector from the computer [6]. Data interfacing, download and processing described below was done using LabVIEW 2011 software (National Instruments, TX, USA). A schematic diagram is shown in Fig. 1.
CO2 elimination rate (L/min) (\({\dot {V}_{C{O_2}}}\)) and alveolar (end-tidal) partial pressure (\(P{A_{C{O_2}}}\)) were measured with each breath in real time. \(P{A_{C{O_2}}}\) was taken from an interval on the same early part of the phase 3 plateau of the capnogram both before and during the ventilatory change (to avoid differences in the end-tidal partial pressure with different breath durations that would be expected where the end-tidal plateau was not perfectly flat). \({\dot {V}_{C{O_2}}}\) for each breath was measured by multiplication and integration of inspired and expired flow and CO2 concentration waveforms with respect to time, with appropriate correction to body temperature and pressure, saturated (BTPS).
The accuracy of the system in measurement of expired \({\dot {V}_{C{O_2}}}\) was verified by comparison against a volumetrically measured flow of pure CO2 gas fed into a tidally ventilated gas exchange simulator (TTL type 1600 hinged bellows test lung, Michigan Instruments, Grand Rapids, MI, USA). The coefficient of variation of measured \({\dot {V}_{C{O_2}}}\) from this simulator was found to be 3% of the target value within the range of ventilator rate settings employed, and that of the \(P{A_{C{O_2}}}\) was 0.25%.
2.2 Measurement algorithm
2.2.1 Baseline “calibration” cardiac output measurement
Baseline cardiac output measurement was obtained as follows. The change in alveolar ventilation for baseline cardiac output measurement was made when the standard error of the measured baseline \({\dot {V}_{C{O_2}}}\) (\({\dot {V}_{C{O_2}i}}\)) was < 1.5% of the average value and that of the baseline \(P{A_{C{O_2}}}\) (\(P{A_{C{O_2}i}}\)) was < 0.1 mmHg for a minimum of 5 consecutive breaths. This was achieved within a median of 6.1 (interquartile range 5.2–8.2) minutes after commencement of the measurement process. For a patient with a typical baseline respiratory rate setting of 12 breaths/min, the ventilatory change involved an oscillating change in respiratory rate between 8 and 16 breaths/min for four 30 s periods to a total of 2 min. This change was accompanied by a change in I:E ratio from 1:2 to 1:6 so that duration of inspiration, passive expiration and inspiratory pressures remained largely unchanged, in effect only the duration of the end-expiratory pause being altered throughout the process. This oscillating pattern of change in respiratory rate was assumed to produce no significant change in mixed venous CO2 content, obeying a fundamental prerequisite of the differential Fick method.
Baseline non-shunt pulmonary capillary blood flow (\(\dot {Q}{c_i}\)) was then calculated, as follows. For any combination of two breaths i and j during the period of the calbration manoeuvre
where is the barometric pressure and \({S_{C{O_2}}}\) was the solubility coefficient of CO2 in blood. The derivation of Eq. (1) is outlined in our previous paper [10]. \({S_{C{O_2}}}\) was obtained from the slope of the CO2 dissociation curve using the equations of Kelman and a previously published algorithm employing a measured hemoglobin, body temperature, arterial oxygen saturation and base excess obtained from an arterial blood gas sample at the time of measurement, processed on a Radiometer ABL 625 blood gas analyser (Radiometer, Odense, Denmark) [11,12,13]. The numerator represents alveolar-capillary \({\dot {V}_{C{O_2}}}\) for breaths i and j required for pulmonary blood flow calculation, which is measured expired \({\dot {V}_{C{O_2}}}\) adjusted for washin and washout of CO2 from the alveolar compartment and lung tissues that occurs with the changes induced in alveolar ventilation rate. \(Vef{f_{C{O_2}}}\), the effective volume of distribution of carbon dioxide in the lung, was obtained using regression of the terms in the numerator against the denominator to find the value with maximal regression coefficient.
\(\dot {Q}{c_i}\) was then corrected using a non-invasive estimate of pulmonary shunt fraction \({{\dot {Q}s} \mathord{\left/ {\vphantom {{\dot {Q}s} {\dot {Q}t}}} \right. \kern-0pt} {\dot {Q}t}}\) obtained from a pulse oximetry saturation measurement (SpO2) according to the method previously described by us [9]
\(C{c^{\prime}_{{O_2}}}\) was calculated from the O2 dissociation curve and the ideal alveolar air equation, and \({\dot {V}_{{O_2}}}\) was estimated from \({\dot {V}_{C{O_2}}}\) and an assumed respiratory quotient of 0.8.
Finally, to obtain baseline total pulmonary blood flow (cardiac output) \(\dot {Q}{t_i}\):
2.2.2 Ongoing breath-by-breath cardiac output monitoring
Continuous ongoing breath-by-breath measurement of \(\dot {Q}t\) at any subsequent breath k was then made using the continuity equation, derivation of which is outlined in our previous paper [7].
Because changes in alveolar ventilation will alter \({\dot {V}_{C{O_2}k}}\) irrespective of the cardiac output, where the minute ventilation was altered by the anesthesiologist the measured value of \({\dot {V}_{C{O_2}k}}\) was simply scaled according to the change in alveolar minute ventilation (calculated using an estimate of anatomical deadspace based on height and weight) relative to the baseline value until a further recalibration measurement was made.
Because pulmonary \({\dot {V}_{C{O_2}}}\) is ultimately dictated by metabolic CO2 production, which is buffered in the short term by substantial body CO2 stores, \({\dot {V}_{C{O_2}k}}\) following a sustained change in cardiac output will normalise toward baseline. Therefore this calibration manoeuvre was recommenced (“recalibration”) in fully automated fashion 5 min after achievement of the last calibration measurement.
A ten breath moving average was used to smooth the resulting value for \(\dot {Q}{t_k}\). At intervals of approximately 10 min where arterial blood pressure was stable (< 20% variation) for at least 3 min, a measurement was simultaneously made by bolus thermodilution (\({\dot {Q}_{Td}}\)) using an average of 3 boluses with room temperature saline, excluding outliers more than two standard deviations from the mean of the other two and repeating the excluded measurement (to deal with occasional artefactual measurements). The boluses were not timed with respiration, and in patients undergoing liver transplantation, where continuous thermodilution cardiac output was being measured at > 12 L/min, the continuous thermodilution measurement, generated from a 3 min average, was used instead of room temperature bolus thermodilution, due to concerns regarding the accuracy of the very small amplitude thermal bolus signal obtained in such patients. This measurement was compared with the simultaneous 2 min average of \(\dot {Q}{t_k}\) measurements (\(\dot {Q}_{cap}\)).
An arbitrary sample size of 50 patients was nominated for the current series. Agreement between \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\) was assessed using the method of Bland and Altman with adjustment for uneven replicate measurements [14, 15], measuring the difference between pairs of \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\), and calculating the mean difference (bias), standard deviation of the difference (precision) and percentage error (1.96 sd/mean) [5]. Correlation was calculated using intraclass correlation coefficient [16]. Agreement in measurement of change in cardiac output was assessed using a 4-quadrant plot and by the polar plot method described by Critchley, using a central exclusion zone where cardiac output measurement by both methods change by < 15% [17, 18]. The relationship of bias and precision of agreement to available spirometric indices of preoperative respiratory function was also examined using regression modeling and r. Statistical analysis was done using STATA 12 (STATA Corp, TX, USA) and LabVIEW.
3 Results
Fifty-two patients (35 male and 17 female) were consented for this study between February and August 2017, of whom 37 underwent cardiac surgery and 15 underwent OLTx. One cardiac surgical patient was excluded due to a faulty pulmonary artery catheter and one OLTx patient was excluded due to a breathing system gas leak. The mean ± standard deviation (range) for age of the remaining 50 patients was 62.9 ± 10.6 (41.0–83.0) years, weight 85.0 ± 18.7 (48.0–121.3) kg and height 167.9 ± 9.6 (146.5–186.5). 7 cardiac surgery patients had moderate or severe impairment of left ventricular systolic function. All cardiac surgery patients received vasopressor support in the form of metaraminol boluses pre-and post-cardiopulmonary bypass. All OLTx patients received a background noradrenaline infusion up to 4 mcg/min which was increased according to clinical indication (mean arterial blood pressure < 70 mmHg).
A total of 293 bolus thermodilution measurements were made with a median of 6 [interquartile range (IQR) 5–7] measurements per patient (both pre- and post-bypass/liver re-perfusion). The mean \({\dot {Q}_{Td}}\) was 5.71 L/min (median 4.74 L/min and range 1.7–15.3 L/min).
The median duration for data collection was 37.0 min (IQR 30.3–48.2 min). The median time to first calibration cardiac output measurement was 6.1 min (IQR 5.2–8.2 min) following commencement of the measurement process.
Figure 2 shows a Bland–Altman plot of agreement displaying the difference between \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\) measurements against the average of the two. Normality of the distribution of differences was confirmed with the skewness and kurtosis test (p = 0.22 on the sktest, STATA 12). The mean bias between capnotracking and thermodilution (\(\dot {Q}_{cap} - {\dot {Q}_{Td}}\)) was 0.32 L/min with a standard deviation of the difference between them (precision) of 1.10 L/min, giving limits of agreement of + 2.51 L/min and − 1.87 L/min. the percentage error in agreement between \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\) (1.96 sd/mean) was 38.4, and 38.7% after adjustment for uneven replicate measurements.
In a post hoc analysis, comparison with 452 sets of paired measurements in 77 patients made using the earlier version of the capnotracking system and bolus thermodilution (mean bias − 0.1 L/min, precision 1.2, percentage error 44.2%) showed better precision of agreement in the current series (p = 0.024, using sdtest STATA 12) but a larger mean bias (p = 0.11 on the t-test STATA 12) [7].
Figure 3 shows the correlation between simultaneous measurements of \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\). The intraclass correlation coefficient was 0.91. The line of best fit followed the relationship of \(\dot {Q}_{cap}\) = 0.89\({\dot {Q}_{Td}}\) + 0.32 L/min, with the coefficient of determination r2 = 0.84.
Figure 4a shows a four-quadrant plot and Fig. 4b depicts a polar plot of the relative changes from the previous measurement in \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\) (d\(\dot {Q}_{cap}\) and d\({\dot {Q}_{Td}}\)). There were 197 consecutive changes recorded, however only 27 were changes of > 15%. Concordance in d\(\dot {Q}_{cap}\)and d\({\dot {Q}_{Td}}\) assessed by the four-quadrant method was 81.5%. The polar plot analysis yielded a mean angular bias of − 1.7°, with radial limits of agreement of ± 76.2°.
a Four-quadrant plot and b polar plot of relative changes from the previous measurement in cardiac output, measured by capnotracking (d\(\dot {Q}_{cap}\)) and thermodilution (d\({\dot {Q}_{Td}}\)). Both exclude changes of < 15%, n = 27. a Showing line of identity: y = x. b Showing 30° radial sector lines
Preoperative spirometry data was available for 27 patients. Figure 5 displays the relationship between the percentage (%) error of agreement between \(\dot {Q}_{cap}\) and \({\dot {Q}_{Td}}\) and the percentage of predicted Forced Expired Volume-one second (FEV1), Forced Vital Capacity (FVC) and Transfer factor for Carbon Monoxide (TLCO). No relationship with FEV1, FVC or TLCO was evident (FEV1: r2 = 0.02, FVC: r2 = 0.02, TLCO: r2 = 0.002). Similarly, no relationship with mean bias of agreement was found (FEV1: r2 = 0.09, FVC: r2 = 0.003, TLCO: r2 = 0.02).
Regression plot of percentage error against lung function. Percentage error is the error between capnotracking and thermodilution for each individual patient. Lung function is the patient’s percentage of predicted FEV1 (Forced Expired Volume-one second), FVC (Forced Vital Capacity) and TLCO (Transfer factor for Carbon Monoxide). n = 27
4 Discussion
A second generation prototype capnotracking system achieved precision of agreement with thermodilution in measurement of cardiac output which compared favourably to that found in a meta-analysis of the accuracy and precision of four existing generic technologies for minimally invasive cardiac measurement in the intraoperative environment (pulse pressure waveform analysis, oesophageal Doppler, partial CO2 rebreathing and transthoracic bioimpedance). Percentage error for these methods varied between 41.3 and 44.5% [4]. The precision of agreement with thermodilution was also better than that of our previous capnotracking system version in a similar patient population. The mean bias was slightly greater, but not to a clinically significant degree (3.5% of the mean cardiac output in this series) [7].
However, the system still failed to achieve the arbitrary threshold of acceptability for percentage error in agreement with thermodilution suggested by Critchley and Critchley of 30% [5]. This criterion assumed a percentage error of agreement with the true cardiac output for both test method and thermodilution of 20%, a desired level of precision shown subsequently to be unrealistic under unstable clinical conditions by studies using an invasive gold standard for reference [19,20,21].
The better precision of the current system compared to our previous version was likely due largely to the fact that the calibration manoeuvre was considerably more prolonged, incorporating data from around 50 breaths, in contrast to the previous version where data from fewer than 10 breaths was accessible for each calibration. This was due to the oscillating pattern of variation in respiratory rate around the set mean, rather than a unidirectional change, which allowed a prolonged manoeuvre without disturbing the stability of mixed venous CO2 partial pressures. This also allowed more frequent recalibration manoeuvres which may also have further improved agreement with thermodilution.
Assumption of stability of mixed venous CO2 partial pressures during the induced change in alveolar ventilation is central to the differential CO2 Fick principle, and has been shown to be a key theoretical limitation to the accuracy of methods based on it, such as partial CO2 rebreathing [22, 23]. An oscillating pattern of variation in alveolar ventilation with a short enough periodicity obviates this limitation because recirculation of blood from various tissues and organ beds with different blood flow rates occurs in a staggered fashion that effectively smoothes the resulting changes in mixed venous blood gas content and delivers reliable breath by breath measurements of pulmonary blood flow. This has been shown to be the case by us [10] and more recently by Hallsjo-Sander et al. in a series of preclinical studies using a similar approach in a porcine model of unstable haemodynamics [24,25,26]. They also demonstrated relatively well preserved accuracy and precision in the presence of acutely impaired lung gas exchange in their model [27]. We could find no evidence of reduced reliability of measurements in patients with poorer baseline lung function in our series.
The current system used an in-line CO2 sensor, while the previous system used sidestream gas sampling, which is more adaptable to incorporation in existing anaesthetic monitoring platforms. However this is unlikely to explain the improvement in precision, since both systems synchronized gas concentration and flow waveforms in software rather than hardware, before being multiplied together to obtain CO2 flow.
The patient population in this and our previous series are a challenging group for any method, but represent a near ideal study population for a number of reasons. Both cardiac surgical and OLTx patients are monitored routinely with a pulmonary artery catheter in our institution. Patients presenting for OLTx for liver failure usually exhibit a hyperdynamic vasodilated circulatory state with high cardiac output measurements, in contrast to patients with advanced heart disease presenting for cardiac surgery. The wide range of haemodynamic states captured across these two patient groups provides a robust test of the linearity of the method being tested, a feature not commonly seen in most studies in the field which are restricted to cardiac surgery only.
The system tested here retains all the potential advantages of our previous prototype system, being fully automated and hands-free, using components for monitoring of physiological variables, including capnography and circuit gas flow, which are now standard on modern anaesthesia machines. While the relatively short duration of measurement in the current series, and the absence of acute instability at these times, such as was captured in our previous study [7], limited the opportunity to measure the response of the system to fluctuations in cardiac output, the response time of the system to sudden changes in pulmonary blood flow, which was readily followed during run onto cardiopulmonary bypass, remained under 30 s. A limitation of the method is that it has only been validated in controlled ventilation in clinical studies to date [6, 7]. Adaptation of the measurement system to spontaneous breathing patterns or ventilator weaning environments, for example, remains a potential future direction for investigation and development.
The capnotracking method thus delivers continuous cardiac output monitoring without added complexity or encroachment on the anaesthetist’s workspace. While research should continue to try to improve the reliability of minimally invasive measurement of cardiac output by available methods under clinical conditions, our study showed comparable precision to existing, more cumbersome or expensive technologies. It would therefore seem a practical and attractive option for improving the penetration of non-invasive advanced haemodynamic monitoring and management into the routine care of patients undergoing major surgery [28].
References
Funk DJ, Moretti EW, Gan TJ. Minimally invasive cardiac output monitoring in the perioperative setting. Anesth Analg. 2009;108:887–97.
Pearse RM, Harrison DA, MacDonald N, Gillies MA, Blunt M, Ackland G, Grocott MP, Ahern A, Griggs K, Scott R, Hinds C, Rowan K. OPTIMISE Study Group. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery: a randomized clinical trial and systematic review. JAMA. 2014;311(21):2181–90.
Miller TE, Roche AM, Gan TJ. Poor adoption of hemodynamic optimization during major surgery: are we practicing substandard care? Anesth Analg. 2011;112(6):1274–6.
Peyton P, Chong S. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology. 2010;113(5):1220–35.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91.
Peyton P, Thompson D, Junor P. Non-invasive automated measurement of cardiac output during stable cardiac surgery using a fully integrated differential CO2 Fick method. J Clin Monit Comput. 2008;22(4):285 – 92.
Peyton P. Continuous minimally invasive peri-operative monitoring of cardiac output by pulmonary capnotracking: comparison with thermodilution and transesophageal echocardiography. J Clin Monit Comput. 2012;26(2):121 – 32.
Gedeon A, Forslund L, Hedenstierna G, Romano E. A new method for noninvasive bedside determination of pulmonary blood flow. Med Biol Eng Comput. 1980;18:411–8.
Peyton P, Robinson G, McCall P, Thompson B. Non-invasive measurement of intrapulmonary shunting. J Cardiothorac Vasc Anesth. 2004;18(1):47–52.
Peyton P, Venkatesan Y, Hood S, Junor P, May C. Non-invasive, automated and continuous cardiac output monitoring by pulmonary capnodynamics: breath by breath comparison with ultrasonic flow probe. Anesthesiology. 2006;105:72–80.
Kelman GR. Digital computer subroutine for the conversion of oxygen tension into saturation. J Appl Physiol. 1966;21(4):1375–6.
Kelman GR. Digital computer procedure for the conversion of PCO2 into blood CO2 content. Respir Physiol. 1967;3:111–5.
Peyton P, Robinson G, Thompson B. The effect of ventilation-perfusion inhomogeneity and nitrous oxide on oxygenation in anesthesia: physiological modeling of gas exchange. J Appl Physiol. 2001;91:17–25.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;327:307–10.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–82.
Streiner DL, Norman GR. Health measurement scales. A practical guide to their development and use. 2nd ed. Oxford Medical Publications. 1995. Ch 8, pp 104–26.
Perrino AC Jr, Harris SN, Luther MA. Intraoperative determination of cardiac output using multiplane transesophageal echocardiography: a comparison to thermodilution. Anesthesiology. 1998;89:350–7.
Critchley LA, Lee A, Ho AM-H. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Botero M, Kirby D, Lobato E, Staples E, Gravenstein N. Measurement of cardiac output before and after cardiopulmonary bypass: comparison among aortic transit-time ultrasound, thermodilution, and noninvasive partial CO2 rebreathing. J Cardiothorac Vasc Anesth. 2004;18(5):563 – 72.
Bajorat J, Hofmockel R, Vagts DA, Janda M, Pohl B, Beck C, Noeldge-Schomburg G. Comparison of invasive and less-invasive techniques of cardiac output measurement under different haemodynamic conditions in a pig model. Eur J Anaesthesiol. 2006;23(1):23–30.
Critchley L. Bias and precision statistics: should we still adhere to the 30% benchmark for cardiac output monitor validation studies? Anesthesiology. 2011;114:1245–6.
Capek JM, Roy RJ. Encyclopedia of medical devices and instrumentation. In: Webster JG, editor. New York: Wiley; 1988. pp. 1309–10.
Yem JS, Tang Y, Turner MJ, Baker AB. Sources of error in noninvasive pulmonary blood flow measurements by partial rebreathing: a computer model study. Anesthesiology. 2003 Apr;98(4):881–7.
Hällsjö Sander C, Hallbäck M, Wallin M, Emtell P, Oldner A, Björne H. Novel continuous capnodynamic method for cardiac output assessment during mechanical ventilation. Br J Anaesth. 2014;112(5):824–31.
Hällsjö Sander C, Lönnqvist PA, Hallbäck M, Sipmann FS, Wallin M, Oldner A, Björne H. Capnodynamic assessment of effective lung volume during cardiac output manipulations in a porcine model. J Clin Monit Comput. 2016;30(6):761–9.
Sigmundsson TS, Öhman T, Hallbäck M, Redondo E, Sipmann FS, Wallin M, Oldner A, Hällsjö Sander C, Björne H. Performance of a capnodynamic method estimating effective pulmonary blood flow during transient and sustained hypercapnia. J Clin Monit Comput. 2017. https://doi.org/10.1007/s10877-017-0021-3.
Hällsjö Sander C, Hallbäck M, Suarez Sipmann F, Wallin M, Oldner A, Björne H. A novel continuous capnodynamic method for cardiac output assessment in a porcine model of lung lavage. Acta Anaesthesiol Scand. 2015;59(8):1022–31.
Peyton P. Editorial: minimally-invasive monitoring of cardiac output and lung gas exchange: taking it mainstream. J Clin Monit Comput. 2016;30(6):749–51.
Funding
Support was kindly provided from a Project Grant from the Australian and New Zealand College of Anaesthetists.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Philip Peyton is Inventor on two patents on this and related technology. Peyton P, Austin Health. A system and method for monitoring cardiac output. US Patent No. 8,613,707. Peyton P, Austin Health. System and method for monitoring cardiac output with substantially improved accuracy and precision. US Patent No. 9,259,187 issued February 16, 2016.
Rights and permissions
About this article
Cite this article
Peyton, P.J., Kozub, M. Performance of a second generation pulmonary capnotracking system for continuous monitoring of cardiac output. J Clin Monit Comput 32, 1057–1064 (2018). https://doi.org/10.1007/s10877-018-0110-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0110-y