Abstract
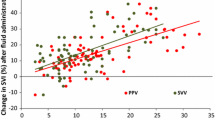
Animal studies suggest that dynamic predictors remain useful in patients with pneumoperitoneum, but human data is conflicting. Our aim was to determine predictive values of pulse pressure variation (PPV) and stroke volume variation (SVV) in patients with pneumoperitoneum using LiDCORapid™ haemodynamic monitor. Standardised fluid challenges of colloid were administered to patients undergoing laparoscopic procedures, one fluid challenge per patient. Intra-abdominal pressure was automatically held at 12 mmHg. Fluid responsiveness was defined as an increase in nominal stroke index (nSI) ≥ 10%. Linear regression was used to assess the ability of PPV and SVV to track the changes of nSI and logistic regression and area under the receiver operating curve (AUROC) to assess the predictive value of PPV and SVV for fluid responsiveness. Threshold values for PPV and SVV were obtained using the “gray zone” approach. A p < 0.05 was considered as statistically significant. 56 patients were included in analysis. 41 patients (73%) responded to fluids. Both PPV and SVV tracked changes in nSI (Spearman correlation coefficients 0.34 for PPV and 0.53 for SVV). Odds ratio for fluid responsiveness for PPV was 1.163 (95% CI 1.01–1.34) and for SVV 1.341 (95% CI 1.10–1.63). PPV achieved an AUROC of 0.674 (95% CI 0.518–0.830) and SVV 0.80 (95% CI 0.668–0.932). The gray zone of PPV ranged between 6.5 and 20.5% and that of SVV between 7.5 and 13%. During pneumoperitoneum, as measured by LiDCORapid™, PPV and SVV can predict fluid responsiveness, however their sensitivity is lower than the one reported in conditions without pneumoperitoneum. Trial registry number: (with the Australian New Zealand Clinical Trials Registry): ACTRN12612000456853.


Similar content being viewed by others
References
Schindler AW, Marx G. Evidence-based fluid management in the ICU. Curr Opin Anaesthesiol. 2016;29:158–65.
Sinclair S, James S, Singer M. Intraoperative volume optimisation and length of hospital stay after repair of proximal femoral fracture: randomised controlled trial. BMJ 1997;315:909–12.
Shoemaker WC, Appel PL, Kram HB. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest 1992;102:208–15.
Thacker JKM, Mountford WK, Ernst FR, Krukas MR, Mythen MM. Perioperative fluid utilization variability and association with outcomes. Ann Surg. 2016;263:502–10.
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445]. Crit Care. 2014;9:R687–93.
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg. 2011;112:1392–402.
Pearse RM, Harrison DA, MacDonald N, Gillies MA, Blunt M, Ackland G, et al. Effect of a perioperative, cardiac output-guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery. JAMA 2014;311:2181–90.
O’Neal JB, Shaw AD. Goal-directed therapy in the operating room: is there any benefit? Curr Opin Anaesthesiol. 2016;29:80–4.
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011;146:571.
Cecconi M, Corredor C, Arulkumaran N, Abuella G, Ball J, Grounds RM, et al. Clinical review: goal-directed therapy-what is the evidence in surgical patients? The effect on different risk groups. Crit Care. 2013;17:209.
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients*: a critical analysis of the evidence. Chest 2002;121:2000–8.
Michard F, Alaya S, Zarka V, Bahloul M, Richard C, Teboul JL. Global end-diastolic volume as an indicator of cardiac preload in patients with septic shock. Chest 2003;124:1900–8.
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 2008;134:172–8.
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–8.
Reuter DA, Kirchner A, Felbinger TW, Weis FC, Kilger E, Lamm P, et al. Usefulness of left ventricular stroke volume variation to assess fluid responsiveness in patients with reduced cardiac function. Crit Care Med. 2003;31:1399–404.
Kramer A, Zygun D, Hawes H, Easton P, Ferland A. Pulse pressure variation predicts fluid responsiveness following coronary artery bypass surgery. Chest 2004;126:1563–8.
Hofer CK, Müller SM, Furrer L, Klaghofer R, Genoni M, Zollinger A. Stroke volume and pulse pressure variation for prediction of fluid responsiveness in patients undergoing off-pump coronary artery bypass grafting. Chest 2005;128:848–54.
Novitsky YW, Litwin DEM, Callery MP. The net immunologic advantage of laparoscopic surgery. Surg Endosc Other Interv Tech. 2004;18:1411–9.
Høiseth L, Hoff IE, Myre K, Landsverk SA, Kirkebøen KA. Dynamic variables of fluid responsiveness during pneumoperitoneum and laparoscopic surgery. Acta Anaesthesiol Scand. 2012;56:777–86.
Renner J, Gruenewald M, Quaden R, Hanss R, Meybohm P, Steinfath M, et al. Influence of increased intra-abdominal pressure on fluid responsiveness predicted by pulse pressure variation and stroke volume variation in a porcine model. Crit Care Med. 2009;37:650–8.
Jacques D, Bendjelid K, Duperret S, Colling J, Piriou V, Viale J-P. Pulse pressure variation and stroke volume variation during increased intra-abdominal pressure: an experimental study. Crit Care. 2011;15:R33.
Guinot P-G, de Broca B, Bernard E, Arab OA, Lorne E, Dupont H. Respiratory stroke volume variation assessed by oesophageal Doppler monitoring predicts fluid responsiveness during laparoscopy. Br J Anaesth. 2014;112:660–4.
Bartha E, Arfwedson C, Imnell A, Kalman S. Towards individualized perioperative, goal-directed haemodynamic algorithms for patients of advanced age: observations during a randomized controlled trial (NCT01141894). Br J Anaesth. 2016;116:486–92.
Miller J, Ho C-X, Tang J, Thompson R, Goldberg J, Amer A, et al. Assessing fluid responsiveness in spontaneously breathing patients. Acad Emerg Med. 2016;23:186–90.
Derichard A, Robin E, Tavernier B, Costecalde M, Fleyfel M, Onimus J, et al. Automated pulse pressure and stroke volume variations from radial artery: evaluation during major abdominal surgery. Br J Anaesth. 2009;103:678–84.
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J-C, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011;12:77.
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot J-J, Vallet B, et al. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “Gray Zone” approach. Anesthesiology 2011;115:231–41.
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2014. http://www.r-project.org/.
Willars C, Dada A, Hughes T, Green D. Functional haemodynamic monitoring: The value of SVV as measured by the LiDCORapid™ in predicting fluid responsiveness in high risk vascular surgical patients. Int J Surg. 2012;10:148–52.
Toscani L, Aya HD, Antonakaki D, Bastoni D, Watson X, Arulkumaran N, et al. What is the impact of the fluid challenge technique on diagnosis of fluid responsiveness? A systematic review and meta-analysis. Crit Care. 2017;21:207.
Cecconi M, Monti G, Hamilton MA, Puntis M, Dawson D, Tuccillo ML, et al. Efficacy of functional hemodynamic parameters in predicting fluid responsiveness with pulse power analysis in surgical patients. Minerva Anestesiol. 2012;78:527–33.
Lahner D, Kabon B, Marschalek C, Chiari A, Pestel G, Kaider A, et al. Evaluation of stroke volume variation obtained by arterial pulse contour analysis to predict fluid responsiveness intraoperatively. Br J Anaesth. 2009;103:346–51.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Mahjoub Y, Touzeau J, Airapetian N, Lorne E, Hijazi M, Zogheib E, et al. The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med. 2010;38:1824–9.
Cherpanath TGV, Hirsch A, Geerts BF, Lagrand WK, Leeflang MM, Schultz MJ, et al. Predicting fluid responsiveness by passive leg raising: a systematic review and meta-analysis of 23 clinical trials. Crit Care Med. 2016;44:981–91.
Jammer I, Tuovila M, Ulvik A. Stroke volume variation to guide fluid therapy: is it suitable for high-risk surgical patients? A terminated randomized controlled trial. Perioper Med. 2015;4:6.
Meng L, Heerdt PM. Perioperative goal-directed haemodynamic therapy based on flow parameters: a concept in evolution. Br J Anaesth. 2016;117:iii3–17.
Joris JL, Chiche JD, Canivet JL, Jacquet NJ, Legros JJ, Lamy ML. Hemodynamic changes induced by laparoscopy and their endocrine correlates: effects of clonidine. J Am Coll Cardiol. 1998;32:1389–96.
Alfonsi P, Vieillard-Baron A, Coggia M, Guignard B, Goeau-Brissonniere O, Jardin F, et al. Cardiac function during intraperitoneal CO2 insufflation for aortic surgery: a transesophageal echocardiographic study. Anesth Analg. 2006;102:1304–10.
Kubitz JC, Annecke T, Forkl S, Kemming GI, Kronas N, Goetz AE, et al. Validation of pulse contour derived stroke volume variation during modifications of cardiac afterload. Br J Anaesth. 2007;98:591–7.
Suehiro K, Tanaka K, Funao T, Matsuura T, Mori T, Nishikawa K. Systemic vascular resistance has an impact on the reliability of the Vigileo-FloTrac system in measuring cardiac output and tracking cardiac output changes. Br J Anaesth. 2013;111:170–7.
Rhodes A, Sunderland R. Arterial pulse power analysis: the LiDCOplus system. In: Pinsky M, Payen D, editors. Functional hemodynamic monitoring. Berlin: Springer; 2005. pp. 183–92.
Costa MG, Della Rocca G, Chiarandini P, Mattelig S, Pompei L, Barriga MS, et al. Continuous and intermittent cardiac output measurement in hyperdynamic conditions: pulmonary artery catheter vs. lithium dilution technique. Intensive Care Med. 2008;34:257–63.
Mora B, Ince I, Birkenberg B, Skhirtladze K, Pernicka E, Ankersmit HJ, et al. Validation of cardiac output measurement with the LiDCO™ pulse contour system in patients with impaired left ventricular function after cardiac surgery. Anaesthesia 2011;66:675–81.
Marquez J, McCurry K, Severyn DA, Pinsky MR. Ability of pulse power, esophageal Doppler, and arterial pulse pressure to estimate rapid changes in stroke volume in humans. Crit Care Med. 2008;36:3001–7.
Hadian M, Severyn DA, Pinsky MR. The effects of vasoactive drugs on pulse pressure and stroke volume variation in postoperative ventilated patients. J Crit Care. 2011;26:328.e1–8.
O’Loughlin E, Ward M, Crossley A, Hughes R, Bremner AP, Corcoran T. Evaluation of the utility of the Vigileo FloTrac(™), LiDCO(™), USCOM and CardioQ(™) to detect hypovolaemia in conscious volunteers: a proof of concept study. Anaesthesia 2015;70:142–9.
Krejci V, Vannucci A, Abbas A, Chapman W, Kangrga IM. Comparison of calibrated and uncalibrated arterial pressure-based cardiac output monitors during orthotopic liver transplantation. Liver Transplant. 2010;16:773–82.
Gruenewald M, Renner J, Meybohm P, Höcker J, Scholz J, Bein B. Reliability of continuous cardiac output measurement during intra-abdominal hypertension relies on repeated calibrations: an experimental animal study. Crit Care. 2008;12:R132.
Nordström J, Hällsjö-Sander C, Shore R, Björne H. Stroke volume optimization in elective bowel surgery: a comparison between pulse power wave analysis (LiDCOrapid) and oesophageal Doppler (CardioQ). Br J Anaesth. 2013;110:374–80.
Tavernier B, Robin E. Assessment of fluid responsiveness during increased intra-abdominal pressure: keep the indices, but change the thresholds. Crit Care. 2011;15:134.
Wajima Z, Shiga T, Imanaga K. Pneumoperitoneum affects stroke volume variation in humans. J Anesth. 2014;29:508–14.
Liu Y, Lou J-S, Mi W-D, Yuan W-X, Fu Q, Wang M, et al. Pulse pressure variation shows a direct linear correlation with tidal volume in anesthetized healthy patients. BMC Anesthesiol. 2016;16:75.
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Åneman A, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124–34.
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11.
Acknowledgements
Authors would like to thank Lea Andjelkovic MD, for her help in patient recruitment and critical suggestions.
Funding
This work was supported by the research fund of the University Medical Centre Ljubljana (20140007).
Author information
Authors and Affiliations
Contributions
MZ study design, patient recruitment, data collection and writing the first draft of the manuscript, final approval; VNJ study design, revision, final approval; RB data analysis, drafting, final approval and MC original idea, study design, revision, final approval.
Corresponding author
Ethics declarations
Conflict of interest
MZ has acted as a lecturer for Edwards Lifesciences. VNJ has no interests to declare. RB has no interests to declare. MC acts as a consultant for Edwards Lifesciences, LiDCO, Masimo, Cheetah and Directed Systems.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Zlicar, M., Novak-Jankovic, V., Blagus, R. et al. Predictive values of pulse pressure variation and stroke volume variation for fluid responsiveness in patients with pneumoperitoneum. J Clin Monit Comput 32, 825–832 (2018). https://doi.org/10.1007/s10877-017-0081-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-017-0081-4