Abstract
Cancer is a dysregulated cellular level pathological condition that results in tumor formation followed by metastasis. In the heterogeneous tumor architecture, cancer stem cells (CSCs) are essential to push forward the progression of tumors due to their strong pro-tumor properties such as stemness, self-renewal, plasticity, metastasis, and being poorly responsive to radiotherapy and chemotherapeutic agents. Cancer stem cells have the ability to withstand various stress pressures by modulating transcriptional and translational mechanisms, and adaptable metabolic changes. Owing to CSCs heterogeneity and plasticity, these cells display varied metabolic and redox profiles across different types of cancers. It has been established that there is a disparity in the levels of Reactive Oxygen Species (ROS) generated in CSCs vs Non-CSC and these differential levels are detected across different tumors. CSCs have unique metabolic demands and are known to change plasticity during metastasis by passing through the interchangeable epithelial and mesenchymal-like phenotypes. During the metastatic process, tumor cells undergo epithelial to mesenchymal transition (EMT) thus attaining invasive properties while leaving the primary tumor site, similarly during the course of circulation and extravasation at a distant organ, these cells regain their epithelial characteristics through Mesenchymal to Epithelial Transition (MET) to initiate micrometastasis. It has been evidenced that levels of Reactive Oxygen Species (ROS) and associated metabolic activities vary between the epithelial and mesenchymal states of CSCs. Similarly, the levels of oxidative and metabolic states were observed to get altered in CSCs post-drug treatments. As oxidative and metabolic changes guide the onset of autophagy in cells, its role in self-renewal, quiescence, proliferation and response to drug treatment is well established. This review will highlight the molecular mechanisms useful for expanding therapeutic strategies based on modulating redox regulation and autophagy activation to targets. Specifically, we will account for the mounting data that focus on the role of ROS generated by different metabolic pathways and autophagy regulation in eradicating stem-like cells hereafter referred to as cancer stem cells (CSCs).

Similar content being viewed by others
Abbreviations
- CSCs:
-
Cancer stem cells
- ROS:
-
Reactive oxygen species
- O2− :
-
Superoxide
- H2O2 :
-
Hydrogen peroxide
- OH• :
-
Hydroxyl radical
- NADPH:
-
Reduced nicotinamide adenine dinucleotide phosphate
- HSCs:
-
Haematopoietic stem cells
- EMT:
-
Epithelial-mesenchymal transition
- PIP3:
-
Phosphatidylinositol 3,4,5-trisphosphate
- PIP2:
-
Phosphatidylinositol 4,5-bisphosphate
- HIF-1:
-
Hypoxia-inducible factor-1
- Keap1:
-
Kelch-like ECH-associated protein 1
- PTEN:
-
Phosphatase and tensin homolog deleted on chromosome 10
- LSCs:
-
Leukemic stem cells
- SODs:
-
Superoxide dismutases
- Nrf2:
-
Nuclear factor erythroid 2-related factor
- GSH:
-
Glutathione
- ATM:
-
Ataxia telangiectasia mutation
- PI3K:
-
Phosphoinositide 3-kinase
- EMT:
-
Epithelial-mesenchymal transition
- JNK:
-
C-Jun N-terminal kinase
- AML:
-
Acute myelogenous leukemia
- Trx:
-
Thioredoxin
- TrxR:
-
Thioredoxin reductase
- Grx:
-
Glutaredoxin
- Prdx:
-
Peroxiredoxins
- VEGF:
-
Vascular endothelial growth factor
- TXNIP:
-
Thioredoxin-interacting protein
- COX:
-
Cyclooxygenase
- FOXO:
-
Forkhead homeobox type O
- PHDs:
-
Prolyl hydroxylase domain proteins
References
Sameer Ullah, Khan Kaneez, Fatima Shariqa, Aisha Baseerat, Hamza Fayaz, Malik (2023) Redox balance and autophagy regulation in cancer progression and their therapeutic perspective. Medical Oncology 40(1):12. https://doi.org/10.1007/s12032-022-01871-0
Mittler R. ROS are good. Trends Plant Sci. 2017;22(1):11–9.
Clerkin J, Naughton R, Quiney C, Cotter T. Mechanisms of ROS modulated cell survival during carcinogenesis. Cancer lett. 2008;266(1):30–6.
Kim HS, Loughran PA, Rao J, Billiar TR, Zuckerbraun BS. Carbon monoxide activates NF-κB via ROS generation and Akt pathways to protect against cell death of hepatocytes. Am J of Physiol-Gastrointest Liver Physiol. 2008;295(1):G146–52.
Komatsu W, Itoh K, Akutsu S, Kishi H, Ohhira S. Nasunin inhibits the lipopolysaccharide-induced pro-inflammatory mediator production in RAW264 mouse macrophages by suppressing ROS-mediated activation of PI3 K/Akt/NF-κB and p38 signaling pathways. Biosci Biotechnol Biochem. 2017;81(10):1956–66.
Lim W, Yang C, Bazer FW, Song G. Chrysophanol induces apoptosis of choriocarcinoma through regulation of ROS and the AKT and ERK1/2 pathways. J Cell Physiol. 2017;232(2):331–9.
Son Y, Cheong Y-K, Kim N-H, Chung H-T, Kang DG, Pae H-O. Mitogen-activated protein kinases and reactive oxygen species: how can ROS activate MAPK pathways? J Signal Transduct. 2011;2011:1–6.
Jalmi SK, Sinha AK. ROS mediated MAPK signaling in abiotic and biotic stress-striking similarities and differences. Front plant sci. 2015;6:769.
Wang J, Huang J, Wang L, Chen C, Yang D, Jin M, et al. Urban particulate matter triggers lung inflammation via the ROS-MAPK-NF-κB signaling pathway. J Thorac Dis. 2017;9(11):4398.
Lennicke C, Cochemé HM. Redox metabolism: ROS as specific molecular regulators of cell signaling and function. Mol Cell. 2021;81(18):3691–707.
Aggarwal V, Tuli HS, Varol A, Thakral F, Yerer MB, Sak K, et al. Role of reactive oxygen species in cancer progression: molecular mechanisms and recent advancements. Biomolecules. 2019;9(11):735.
Zhao Y, Hu X, Liu Y, Dong S, Wen Z, He W, et al. ROS signaling under metabolic stress: cross-talk between AMPK and AKT pathway. Mol cancer. 2017;16(1):1–12.
Jin F, Wu Z, Hu X, Zhang J, Gao Z, Han X, et al. The PI3K/Akt/GSK-3β/ROS/eIF2B pathway promotes breast cancer growth and metastasis via suppression of NK cell cytotoxicity and tumor cell susceptibility. Cancer biol & med. 2019;16(1):38.
Zhang Z, Duan Q, Zhao H, Liu T, Wu H, Shen Q, et al. Gemcitabine treatment promotes pancreatic cancer stemness through the Nox/ROS/NF-κB/STAT3 signaling cascade. Cancer let. 2016;382(1):53–63.
Gao L, Loveless J, Shay C, Teng YJ. Targeting ROS-mediated crosstalk between autophagy and apoptosis in cancer. Rev New Drug Targ Age-Related Disord. 2020;1260:1–12.
Gopal YV, Rizos H, Chen G, Deng W, Frederick DT, Cooper ZA, et al. Inhibition of mTORC1/2 overcomes resistance to MAPK pathway inhibitors mediated by PGC1α and oxidative phosphorylation in melanoma. Cancer res. 2014;74(23):7037–47.
Haq R, Shoag J, Andreu-Perez P, Yokoyama S, Edelman H, Rowe GC, et al. Oncogenic BRAF regulates oxidative metabolism via PGC1α and MITF. Cancer Cell. 2013;23(3):302–15.
Gureev AP, Shaforostova EA, Popov VN. Regulation of mitochondrial biogenesis as a way for active longevity: interaction between the Nrf2 and PGC-1α signaling pathways. Front genet. 2019;10:435.
de la Vega MR, Chapman E, Zhang DD. NRF2 and the Hallmarks of Cancer. Cancer Cell. 2018;34(1):21–43.
Evans MJ, Scarpulla RC. NRF-1: a trans-activator of nuclear-encoded respiratory genes in animal cells. Genes & Dev. 1990;4(6):1023–34.
Blesa JR, Hernandez-Yago J. Distinct functional contributions of 2 GABP–NRF-2 recognition sites within the context of the human TOMM70 promoter. Biochem cell biol. 2006;84(5):813–22.
Zhang DD, Hannink M. Distinct cysteine residues in Keap1 are required for Keap1-dependent ubiquitination of Nrf2 and for stabilization of Nrf2 by chemopreventive agents and oxidative stress. Mole cell biol. 2003;23(22):8137–51.
Giudice A, Arra C, Turco MC. Review of molecular mechanisms involved in the activation of the Nrf2-ARE signaling pathway by chemopreventive agents. Transcr Factors. 2010;647:37–74.
Harris IS, DeNicola GM. The complex interplay between antioxidants and ROS in cancer. Trends cell biol. 2020;30(6):440–51.
Dinkova-Kostova AT, Abramov AY. The emerging role of Nrf2 in mitochondrial function. Free Radic Biol Med. 2015;88:179–88.
Kahroba H, Shirmohamadi M, Hejazi MS, Samadi N. The Role of Nrf2 signaling in cancer stem cells: From stemness and self-renewal to tumorigenesis and chemoresistance. Life Sci. 2019;239:116986.
Pillai R, Hayashi M, Zavitsanou A-M, Papagiannakopoulos TJ. NRF2: KEAPing tumors protected. Cancer Discov. 2022;12(3):625–43.
Torrente L, DeNicola GM. Targeting NRF2 and its downstream processes: opportunities and challenges. Annu Rev Pharmacol Toxicol. 2022;62:279–300.
Sabharwal SS, Schumacker PT. Mitochondrial ROS in cancer: initiators, amplifiers or an Achilles’ heel? Nat Rev Cancer. 2014;14(11):709–21.
Sullivan LB, Chandel NS. Mitochondrial reactive oxygen species and cancer. Cancer Metab. 2014;2(1):1–12.
Jäger S, Handschin C, St-Pierre J, Spiegelman BM. AMP-activated protein kinase (AMPK) action in skeletal muscle via direct phosphorylation of PGC-1α. Proc Natl Acad Sci. 2007;104(29):12017–22.
Hinchy EC, Gruszczyk AV, Willows R, Navaratnam N, Hall AR, Bates G, et al. Mitochondria-derived ROS activate AMP-activated protein kinase (AMPK) indirectly. J Biol Chem. 2018;293(44):17208–17.
Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A, Vasquez DS, et al. AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol cell. 2008;30(2):214–26.
Inoki K, Zhu T, Guan K-L. TSC2 mediates cellular energy response to control cell growth and survival. Cell. 2003;115(5):577–90.
Meley D, Bauvy C, Houben-Weerts JH, Dubbelhuis PF, Helmond MT, Codogno P, et al. AMP-activated protein kinase and the regulation of autophagic proteolysis. Curr Biol. 2006;281(46):34870–9.
Li Y, Chen Y. AMPK and autophagy. Adv Exp Med Biol. 2019. https://doi.org/10.1007/978-981-15-0602-4_4.
Alers S, Löffler AS, Wesselborg S, Stork B. Role of AMPK-mTOR-Ulk1/2 in the regulation of autophagy: cross talk, shortcuts, and feedbacks. Mol Cell Biol. 2012;32(1):2–11.
Egan DF, Shackelford DB, Mihaylova MM, Gelino S, Kohnz RA, Mair W, et al. Phosphorylation of ULK1 (hATG1) by AMP-activated protein kinase connects energy sensing to mitophagy. Science. 2011;331(6016):456–61.
Nazio F, Bordi M, Cianfanelli V, Locatelli F, Cecconi F. Autophagy and cancer stem cells: molecular mechanisms and therapeutic applications. Cell Death Differ. 2019;26(4):690–702.
Ippolito L, Giannoni E, Chiarugi P, Parri M. Mitochondrial redox hubs as promising targets for anticancer therapy. Front Oncol. 2020;10:256.
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Rad Biol Med. 2010;49(11):1603–16.
Lei Y, Zhang D, Yu J, Dong H, Zhang J, Yang S. Targeting autophagy in cancer stem cells as an anticancer therapy. Cancer Lett. 2017;393:33–9.
Liu J, Wang Z. Increased oxidative stress as a selective anticancer therapy. Oxidat Med Cell Longev. 2015;2015:1–12.
Hüser L, Novak D, Umansky V, Altevogt P, Utikal J. Targeting SOX2 in anticancer therapy. Expert Opin Ther Targ. 2018;22(12):983–91.
Ng P, Cheng W. The Dark Side of Pluripotency–Cancer Stem Cell. In: Pluripotent Stem Cells. IntechOpen; 2013.
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci. 2003;100(7):3983–8.
Dalerba P, Dylla SJ, Park I-K, Liu R, Wang X, Cho RW, et al. Phenotypic characterization of human colorectal cancer stem cells. Proc Natl Acad Sci. 2007;104(24):10158–63.
Eramo A, Lotti F, Sette G, Pilozzi E, Biffoni M, Di Virgilio A, et al. Identification and expansion of the tumorigenic lung cancer stem cell population. Cell Death Differ. 2008;15(3):504–14.
Yu Z, Pestell TG, Lisanti MP, Pestell RG. Cancer stem cells. Int J Biochem Cell Biol. 2012;44(12):2144–51.
Beck B, Blanpain C. Unravelling cancer stem cell potential. Nat Rev Cancer. 2013;13(10):727–38.
Jones RJ, Matsui W. Cancer stem cells: from bench to bedside. Biol Blood Marrow Trans. 2007;13:47–52.
Lin TL, Fu C, Sakamoto KM. Cancer stem cells: the root of the problem. Pediatr Res. 2007;62(3):239.
Zhu X, Chen H-H, Gao C-Y, Zhang X-X, Jiang J-X, Zhang Y, et al. Energy metabolism in cancer stem cells. World J Stem Cells. 2020;12(6):448.
Peiris-Pagès M, Martinez-Outschoorn UE, Pestell RG, Sotgia F, Lisanti MP. Cancer stem cell metabolism. Breast Cancer Res. 2016;18(1):1–10.
Swartz MA, Iida N, Roberts EW, Sangaletti S, Wong MH, Yull FE, et al. Tumor microenvironment complexity: emerging roles in cancer therapytumor microenvironment. Cancer Res. 2012;72(10):2473–80.
Dougan M, Dougan SK. Targeting immunotherapy to the tumor microenvironment. J cell biochem. 2017;118(10):3049–54.
Wu T, Dai Y. Tumor microenvironment and therapeutic response. Cancer Lett. 2017;387:61–8.
Sung P-J, Rama N, Imbach J, Fiore S, Ducarouge B, Neves D, et al. Cancer-associated fibroblasts produce netrin-1 to control cancer cell plasticity. Cancer Res. 2019;79(14):3651–61.
Su S, Chen J, Yao H, Liu J, Yu S, Lao L, et al. CD10+ GPR77+ cancer-associated fibroblasts promote cancer formation and chemoresistance by sustaining cancer stemness. Cell. 2018;172(4):841–56.
Huang T-X, Guan X-Y, Fu L. Therapeutic targeting of the crosstalk between cancer-associated fibroblasts and cancer stem cells. Am J Cancer Res. 2019;9(9):1889.
Rao G, Wang H, Li B, Huang L, Xue D, Wang X, et al. Reciprocal interactions between tumor-associated macrophages and cd44-positive cancer cells via osteopontin/CD44 promote tumorigenicity in colorectal cancerthe interaction of OPN and CD44 in colorectal cancer. Clinical Cancer Res. 2013;19(4):785–97.
Doherty MR, Parvani JG, Tamagno I, Junk DJ, Bryson BL, Cheon HJ, et al. The opposing effects of interferon-beta and oncostatin-M as regulators of cancer stem cell plasticity in triple-negative breast cancer. Breast Cancer Res. 2019;21(1):1–12.
Debele TA, Yu L-Y, Yang C-S, Shen Y-A, Lo C-L. pH-and GSH-sensitive hyaluronic acid-MP conjugate micelles for intracellular delivery of doxorubicin to colon cancer cells and cancer stem cells. Biomacromol. 2018;19(9):3725–37.
Jung N, Kwon HJ, Jung HJ. Downregulation of mitochondrial UQCRB inhibits cancer stem cell-like properties in glioblastoma. Int J Oncol. 2018;52(1):241–51.
Weinberg F, Ramnath N, Nagrath D. Reactive oxygen species in the tumor microenvironment: an overview. Cancers. 2019;11(8):1191.
Aboelella NS, Brandle C, Kim T, Ding Z-C, Zhou G. Oxidative stress in the tumor microenvironment and its relevance to cancer immunotherapy. Cancers. 2021;13(5):986.
Chen Y, McMillan-Ward E, Kong J, Israels SJ, Gibson SB. Mitochondrial electron-transport-chain inhibitors of complexes I and II induce autophagic cell death mediated by reactive oxygen species. J Cell Sci. 2007;120(23):4155–66.
Salmeen A, Barford D. Functions and mechanisms of redox regulation of cysteine-based phosphatases. Antioxid & Redox Signal. 2005;7(5–6):560–77.
Leslie NR. The redox regulation of PI 3-kinase–dependent signaling. Antioxid & Redox Signal. 2006;8(9–10):1765–74.
Choi S-L, Kim S-J, Lee K-T, Kim J, Mu J, Birnbaum MJ, et al. The regulation of AMP-activated protein kinase by H2O2. Biochem Biophys Res. 2001;287(1):92–7.
Ojha R, Bhattacharyya S, Singh SK. Autophagy in cancer stem cells: a potential link between chemoresistance, recurrence, and metastasis. BioRes open access. 2015;4(1):97–108.
Khan SU, Pathania AS, Wani A, Fatima K, Mintoo MJ, Hamza B, et al. Activation of lysosomal mediated cell death in the course of autophagy by mTORC1 inhibitor. Sci Rep. 2022;12(1):1–13.
Wani A, Al Rihani SB, Sharma A, Weadick B, Govindarajan R, Khan SU, et al. Crocetin promotes clearance of amyloid-β by inducing autophagy via the STK11/LKB1-mediated AMPK pathway. Autophagy. 2021;17(11):3813–32.
Xie K, Tian L, Guo X, Li K, Li J, Deng X, et al. BmATG5 and BmATG6 mediate apoptosis following autophagy induced by 20-hydroxyecdysone or starvation. Autophagy. 2016;12(2):381–96.
Puente C, Hendrickson RC, Jiang XJ. Nutrient-regulated phosphorylation of ATG13 inhibits starvation-induced autophagy. J Biol Chem. 2016;291(11):6026–35.
Wei Y, An Z, Zou Z, Sumpter R Jr, Su M, Zang X, et al. The stress-responsive kinases MAPKAPK2/MAPKAPK3 activate starvation-induced autophagy through Beclin 1 phosphorylation. Elife. 2015;4:0528.
Rashid H-O, Yadav RK, Kim H-R, Chae H-J. ER stress: Autophagy induction, inhibition and selection. Autophagy. 2015;11(11):1956–77.
Fang Y, Tan J, Zhang Q. Signaling pathways and mechanisms of hypoxia-induced autophagy in the animal cells. Cell Biol Int. 2015;39(8):891–8.
He C, Klionsky DJ. Regulation mechanisms and signaling pathways of autophagy. Annu Rev Genet. 2009;43(1):67–93.
Wang L, Ye X, Zhao T. The physiological roles of autophagy in the mammalian life cycle. Biol Rev. 2019;94(2):503–16.
Umanah GK, Abalde-Atristain L, Khan MR, Mitra J, Dar MA, Chang M, et al. AAA+ ATPase Thorase inhibits mTOR signaling through the disassembly of the mTOR complex 1. Nat Commun. 2022;13(1):1–18.
Sengupta S, Peterson TR, Sabatini DM. Regulation of the mTOR complex 1 pathway by nutrients, growth factors, and stress. Mol cell. 2010;40(2):310–22.
Hosokawa N, Hara T, Kaizuka T, Kishi C, Takamura A, Miura Y, et al. Nutrient-dependent mTORC1 association with the ULK1–Atg13–FIP200 complex required for autophagy. Mol Biol cell. 2009;20(7):1981–91.
Kim J, Kundu M, Viollet B, Guan K-L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol. 2011;13(2):132–41.
Holczer M, Hajdú B, Lőrincz T, Szarka A, Bánhegyi G, Kapuy OJ. A double negative feedback loop between mTORC1 and AMPK kinases guarantees precise autophagy induction upon cellular stress. Int J Mol Sci. 2019;20(22):5543.
Jung CH, Jun CB, Ro S-H, Kim Y-M, Otto NM, Cao J, et al. ULK-Atg13-FIP200 complexes mediate mTOR signaling to the autophagy machinery. Mol Biol cel. 2009;20(7):1992–2003.
Axe EL, Walker SA, Manifava M, Chandra P, Roderick HL, Habermann A, et al. Autophagosome formation from membrane compartments enriched in phosphatidylinositol 3-phosphate and dynamically connected to the endoplasmic reticulum. J Cell Biol. 2008;182(4):685–701.
Lu Q, Yang P, Huang X, Hu W, Guo B, Wu F, et al. The WD40 repeat PtdIns (3) P-binding protein EPG-6 regulates progression of omegasomes to autophagosomes. Dev Cell. 2011;21(2):343–57.
Dooley HC, Razi M, Polson HE, Girardin SE, Wilson MI, Tooze SA. WIPI2 links LC3 conjugation with PI3P, autophagosome formation, and pathogen clearance by recruiting Atg12–5–16L1. Mol Cell. 2014;55(2):238–52.
Nakatogawa H, Ichimura Y, Ohsumi Y. Atg8, a ubiquitin-like protein required for autophagosome formation, mediates membrane tethering and hemifusion. Cell. 2007;130(1):165–78.
Mizushima N, Yoshimori T, Ohsumi Y. The role of Atg proteins in autophagosome formation. Annu Rev Cell Dev Biol. 2011;27:107–32.
Chang C, Jensen LE, Hurley JH. Autophagosome biogenesis comes out of the black box. Nat Cell Biol. 2021;23(5):450–6.
El Hout M, Cosialls E, Mehrpour M, Hamaï A. Crosstalk between autophagy and metabolic regulation of cancer stem cells. Mol Cancer. 2020;19(1):1–17.
Lleonart ME, Abad E, Graifer D, Lyakhovich A. Reactive oxygen species-mediated autophagy defines the fate of cancer stem cells. Antioxid & Redox Signal. 2018;28(11):1066–79.
Ding W-X, Yin X-M. Mitophagy: mechanisms, pathophysiological roles, and analysis. Biol Chem. 2012;393(7):547–64.
Wallace DC. Mitochondria and cancer. Nat Rev Cancer. 2012;12(10):685–98.
Janku F. Tumor heterogeneity in the clinic: is it a real problem? Ther Adv Med Oncol. 2014;6(2):43–51.
El-Osta H, Hong D, Wheler J, Fu S, Naing A, Falchook G, et al. Outcomes of research biopsies in phase I clinical trials: the MD anderson cancer center experience. The Oncol. 2011;16(9):1292–8.
Anderson K, Lutz C, Van Delft FW, Bateman CM, Guo Y, Colman SM, et al. Genetic variegation of clonal architecture and propagating cells in leukaemia. Nature. 2011;469(7330):356–61.
Prasetyanti PR, Medema JP. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol Cancer. 2017;16(1):1–9.
Mintoo M, Khan S, Wani A, Malik S, Bhurta D, Bharate S, et al. A rohitukine derivative IIIM-290 induces p53 dependent mitochondrial apoptosis in acute lymphoblastic leukemia cells. Mol Carcinog. 2021;60(10):671–83.
Khan SU, Fatima K, Malik F. Understanding the cell survival mechanism of anoikis-resistant cancer cells during different steps of metastasis. Clin Exp Metastasis. 2022;39(5):715–26.
Driessens G, Beck B, Caauwe A, Simons BD, Blanpain C. Defining the mode of tumour growth by clonal analysis. Nature. 2012;488(7412):527–30.
Chen J, Li Y, Yu T-S, McKay RM, Burns DK, Kernie SG, et al. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature. 2012;488(7412):522–6.
Gao Z, Liu H, Shi Y, Yin L, Zhu Y, Liu R. Identification of cancer stem cell molecular markers and effects of hsa-miR-21–3p on stemness in esophageal squamous cell carcinoma. Cancers. 2019;11(4):518.
Snyder V, Reed-Newman TC, Arnold L, Thomas SM, Anant S. Cancer stem cell metabolism and potential therapeutic targets. Front Oncol. 2018;8:203.
Yang M, Liu P, Huang P. Cancer stem cells, metabolism, and therapeutic significance. Tumor Biol. 2016;37(5):5735–42.
Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23(10):1124–34.
Valle S, Alcalá S, Martin-Hijano L, Cabezas-Sáinz P, Navarro D, Muñoz ER, et al. Exploiting oxidative phosphorylation to promote the stem and immunoevasive properties of pancreatic cancer stem cells. Nat Commun. 2020;11(1):1–19.
Tian H, Zhang B, Li L, Wang G, Li H, Zheng J. Manipulation of mitochondrial plasticity changes the metabolic competition between “Foe” and “Friend” during tumor malignant transformation. Front Oncol. 2020;10:1692.
Deshmukh A, Deshpande K, Arfuso F, Newsholme P, Dharmarajan A. Cancer stem cell metabolism: a potential target for cancer therapy. Mol Cancer. 2016;15(1):1–10.
Folmes CD, Dzeja PP, Nelson TJ, Terzic A. Metabolic plasticity in stem cell homeostasis and differentiation. Cell Stem Cell. 2012;11(5):596–606.
Rahman M, Deleyrolle L, Vedam-Mai V, Azari H, Abd-El-Barr M, Reynolds BA. The cancer stem cell hypothesis: failures and pitfalls. Neurosurgery. 2011;68(2):531–45.
Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. 2001;414(6859):105–11.
Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. 2009;324(5930):1029–33.
Abraham BK, Fritz P, McClellan M, Hauptvogel P, Athelogou M, Brauch H. Prevalence of CD44+/CD24−/low cells in breast cancer may not be associated with clinical outcome but may favor distant metastasis. Clin Cancer Res. 2005;11(3):1154–9.
Moitra K, Lou H, Dean M. Multidrug efflux pumps and cancer stem cells: insights into multidrug resistance and therapeutic development. Clin Pharmacol Ther. 2011;89(4):491–502.
Serafino A, Zonfrillo M, Andreola F, Psaila R, Mercuri L, Moroni N, et al. CD44-targeting for antitumor drug delivery: a new SN-38-hyaluronan bioconjugate for locoregional treatment of peritoneal carcinomatosis. Curr Cancer Drug Targ. 2011;11(5):572–85.
Tamada M, Nagano O, Tateyama S, Ohmura M, Yae T, Ishimoto T, et al. Modulation of glucose metabolism by CD44 contributes to antioxidant status and drug resistance in cancer cells. Cancer Res. 2012;72(6):1438–48.
Kuramoto K, Yamamoto M, Suzuki S, Sanomachi T, Togashi K, Seino S, et al. Verteporfin inhibits oxidative phosphorylation and induces cell death specifically in glioma stem cells. Genes. 2020;287(10):2023–36.
Yasuda T, Ishimoto T, Baba H. Conflicting metabolic alterations in cancer stem cells and regulation by the stromal niche. Regen Ther. 2021;17:8–12.
Sancho P, Burgos-Ramos E, Tavera A, Kheir TB, Jagust P, Schoenhals M, et al. MYC/PGC-1α balance determines the metabolic phenotype and plasticity of pancreatic cancer stem cells. Cell Metabol. 2015;22(4):590–605.
De Francesco EM, Ózsvári B, Sotgia F, Lisanti MP. Dodecyl-TPP targets mitochondria and potently eradicates cancer stem cells (CSCs): synergy with FDA-approved drugs and natural compounds (vitamin C and berberine). Front Oncol. 2019;9:615.
Sotgia F, Martinez-Outschoorn UE, Lisanti MP. Mitochondrial oxidative stress drives tumor progression and metastasis: should we use antioxidants as a key component of cancer treatment and prevention? BMC Med. 2011;9(1):1–5.
Lamb R, Ozsvari B, Lisanti CL, Tanowitz HB, Howell A, Martinez-Outschoorn UE, et al. Antibiotics that target mitochondria effectively eradicate cancer stem cells, across multiple tumor types: treating cancer like an infectious disease. Oncotarget. 2015;6(7):4569.
Chu D, Yao D, Zhuang Y, Hong Y, Zhu X, Fang Z, et al. Azithromycin enhances the favorable results of paclitaxel and cisplatin in patients with advanced non-small cell lung cancer. Genet Mol Res. 2014;13(2):2796–805.
Andrzejewski S, Gravel S-P, Pollak M, St-Pierre J. Metformin directly acts on mitochondria to alter cellular bioenergetics. Cancer Metabol. 2014;2(1):1–14.
Mayer M, Klotz L, Venkateswaran V. Metformin and prostate cancer stem cells: a novel therapeutic target. Prostate Cancer and Prostatic Dis. 2015;18(4):303–9.
Redza-Dutordoir M, Averill-Bates DA. Activation of apoptosis signalling pathways by reactive oxygen species. Biochimica et Biophysica Acta (BBA)-Mol Cell Res. 2016;1863(12):2977–92.
贾晓晖. Hypoxia-inducible Factor-1 (HIF-1) in Pancreatic Cancer Cell Aggressiveness and Therapeutic Resistance and the Potential Role for Pancreatic Endocrine Cells in Islet Transplantation. 2014.
Menendez JA, Alarcón T. Metabostemness: a new cancer hallmark. Front Oncol. 2014;4:262.
Singh SS, Vats S, Chia AY-Q, Tan TZ, Deng S, Ong MS, et al. Dual role of autophagy in hallmarks of cancer. Oncogene. 2018;37(9):1142–58.
Rao S, Tortola L, Perlot T, Wirnsberger G, Novatchkova M, Nitsch R, et al. A dual role for autophagy in a murine model of lung cancer. Nat Commun. 2014;5(1):1–15.
Borah A, Raveendran S, Rochani A, Maekawa T, Kumar D. Targeting self-renewal pathways in cancer stem cells: clinical implications for cancer therapy. Oncogenesis. 2015;4(11):e177.
Yoo YD, Kwon YT. Molecular mechanisms controlling asymmetric and symmetric self-renewal of cancer stem cells. J Analyt Sci Technol. 2015;6(1):1–6.
Mehta P, Novak C, Raghavan S, Ward M, Mehta G. Self-renewal and CSCs in vitro enrichment: growth as floating spheres. Cancer Stem Cells: Springer; 2018. p. 61–75.
Singh AK, Arya RK, Maheshwari S, Singh A, Meena S, Pandey P, et al. Tumor heterogeneity and cancer stem cell paradigm: updates in concept, controversies and clinical relevance. Int J Cancer. 2015;136(9):1991–2000.
Wang G, Xu J, Zhao J, Yin W, Liu D, Chen W, et al. Arf1-mediated lipid metabolism sustains cancer cells and its ablation induces anti-tumor immune responses in mice. Nat Commun. 2020;11(1):1–16.
Brunel A, Bégaud G, Auger C, Durand S, Battu S, Bessette B, et al. Autophagy and extracellular vesicles, connected to rabGTPase family, support aggressiveness in cancer stem cells. Cells. 2021;10(6):1330.
Clarke AJ, Simon AK. Autophagy in the renewal, differentiation and homeostasis of immune cells. Nat Rev Immunol. 2019;19(3):170–83.
Morishita H, Mizushima N. Diverse cellular roles of autophagy. Annu Rev Cell Dev Biol. 2019;35(1):453–75.
Cho YH, Han KM, Kim D, Lee J, Lee SH, Choi KW, et al. Autophagy regulates homeostasis of pluripotency-associated proteins in hESCs. Stem Cells. 2014;32(2):424–35.
Abd El-Aziz YS, Gillson J, Jansson PJ, Sahni S. A promising target for triple negative breast cancers. Autophagy. 2022;175:106006.
McCubrey JA, Davis NM, Abrams SL, Montalto G, Cervello M, Libra M, et al. Targeting breast cancer initiating cells: advances in breast cancer research and therapy. Adv Biol Regul. 2014;56:81–107.
Wolf J, Dewi DL, Fredebohm J, Müller-Decker K, Flechtenmacher C, Hoheisel JD, et al. A mammosphere formation RNAi screen reveals that ATG4A promotes a breast cancer stem-like phenotype. Breast Cancer Res. 2013;15(6):1–13.
Gong C, Bauvy C, Tonelli G, Yue W, Delomenie C, Nicolas V, et al. Beclin 1 and autophagy are required for the tumorigenicity of breast cancer stem-like/progenitor cells. Breast Cancer Res. 2013;32(18):2261–72.
Jang K. Exploring Mechanisms Linking Signal Transduction and Cancer Stem Cell Expansion: University of Miami; 2017.
Antonelli M, Strappazzon F, Arisi I, Brandi R, D’Onofrio M, Sambucci M, et al. ATM kinase sustains breast cancer stem-like cells by promoting ATG4C expression and autophagy. Oncotarget. 2017;8(13):21692.
Maycotte P, Gearheart CM, Barnard R, Aryal S, Mulcahy Levy JM, Fosmire SP, et al. STAT3-mediated autophagy dependence identifies subtypes of breast cancer where autophagy inhibition can be efficaciousautophagy and STAT3 control breast cancer survival. Cancer res. 2014;74(9):2579–90.
Qin J-J, Yan L, Zhang J, Zhang W-D. STAT3 as a potential therapeutic target in triple negative breast cancer: a systematic review. J Exp & Clin Cancer Res. 2019;38(1):1–16.
Ortiz-Montero P, Londoño-Vallejo A, Vernot J-P. Senescence-associated IL-6 and IL-8 cytokines induce a self-and cross-reinforced senescence/inflammatory milieu strengthening tumorigenic capabilities in the MCF-7 breast cancer cell line. Cell Commun Signal. 2017;15(1):1–18.
Yin P, Wang W, Gao J, Bai Y, Wang Z, Na L, et al. Fzd2 contributes to breast cancer cell mesenchymal-like stemness and drug resistance. Oncol Res. 2020;28(3):273.
Mathieu J, Zhang Z, Zhou W, Wang AJ, Heddleston JM, Pinna CM, et al. HIF induces human embryonic stem cell markers in cancer cells. Cancer Res. 2011;71(13):4640–52.
Kimmelman AC, White E. Autophagy and tumor metabolism. Cell Metab. 2017;25(5):1037–43.
Zhu H, Wang D, Zhang L, Xie X, Wu Y, Liu Y, et al. Upregulation of autophagy by hypoxia-inducible factor-1α promotes EMT and metastatic ability of CD133+ pancreatic cancer stem-like cells during intermittent hypoxia. Oncol Rep. 2014;32(3):935–42.
Qureshi-Baig K, Kuhn D, Viry E, Pozdeev VI, Schmitz M, Rodriguez F, et al. Hypoxia-induced autophagy drives colorectal cancer initiation and progression by activating the PRKC/PKC-EZR (ezrin) pathway. Autophagy. 2020;16(8):1436–52.
Park SJ, Kim JG, Kim ND, Yang K, Shim JW, Heo KJOL. Estradiol, TGF-β1 and hypoxia promote breast cancer stemness and EMT-mediated breast cancer migration. Oncol Lett. 2016;11(3):1895–902.
Viale A, Pettazzoni P, Lyssiotis CA, Ying H, Sánchez N, Marchesini M, et al. Oncogene ablation-resistant pancreatic cancer cells depend on mitochondrial function. Nature. 2014;514(7524):628–32.
O’Brien CA, Kreso A, Jamieson CH. Cancer Stem Cells and Self-renewalCancer Stem Cells and Self-renewal. Clin Cancer Res. 2010;16(12):3113–20.
Liu C, Liu L, Chen X, Cheng J, Zhang H, Zhang C, et al. LSD1 Stimulates cancer-associated fibroblasts to drive notch3-dependent self-renewal of liver cancer stem–like CellsLSD1 regulates liver CSC self-renewal via notch3 signaling. Cancer Res. 2018;78(4):938–49.
Klionsky DJ, Emr SD. Autophagy as a regulated pathway of cellular degradation. Science. 2000;290(5497):1717–21.
Morrison SJ, Spradling ACJC. Stem cells and niches: mechanisms that promote stem cell maintenance throughout life. Cell. 2008;132(4):598–611.
Mazure NM, Pouysségur J. Hypoxia-induced autophagy: cell death or cell survival? Current Opin Cell Biol. 2010;22(2):177–80.
Song Y-j, Zhang S-s, Guo X-l, Sun K, Han Z-p, Li R, et al. Autophagy contributes to the survival of CD133+ liver cancer stem cells in the hypoxic and nutrient-deprived tumor microenvironment. Cancer Lett. 2013;339(1):70–81. https://doi.org/10.1016/j.canlet.2013.07.021.
Tao J, Yang G, Zhou W, Qiu J, Chen G, Luo W, et al. Targeting hypoxic tumor microenvironment in pancreatic cancer. 2021;14(1):1–25.
Held NM, Houtkooper RHJB. Mitochondrial quality control pathways as determinants of metabolic health. BioEssays. 2015;37(8):867–76.
Peixoto J, Lima J. Metabolic traits of cancer stem cells. Dis Models Mech. 2018;11(8):dmm033464.
Menendez J, Joven J, Cufí S, Corominas-Faja B, Oliveras-Ferraros C, Cuyàs E, et al. The Warburg effect version 20: metabolic reprogramming of cancer stem cells. Cell Cycle. 2013;12(8):1166–79.
Shen Y-A, Wang C-Y, Hsieh Y-T, Chen Y-J, Wei Y-H. Metabolic reprogramming orchestrates cancer stem cell properties in nasopharyngeal carcinoma. Cell Cycle. 2015;14(1):86–98.
Molina JR, Sun Y, Protopopova M, Gera S, Bandi M, Bristow C, et al. An inhibitor of oxidative phosphorylation exploits cancer vulnerability. Nat Med. 2018;24(7):1036–46.
Galluzzi L, Baehrecke EH, Ballabio A, Boya P, Bravo-San Pedro JM, Cecconi F, et al. Molecular definitions of autophagy and related processes. EMBO J. 2017;36(13):1811–36.
Kasahara A, Scorrano L. Mitochondria: from cell death executioners to regulators of cell differentiation. Trends in cell biol. 2014;24(12):761–70.
Twig G, Shirihai OS. The interplay between mitochondrial dynamics and mitophagy. Antioxid Redox Signal. 2011;14(10):1939–51.
Hou W, Zhang Q, Yan Z, Chen R, Zeh Iii H, Kang R, et al. Strange attractors: DAMPs and autophagy link tumor cell death and immunity. Cell Death Dis. 2013;4(12):e966.
Boya P, Codogno P, Rodriguez-Muela NJD. Autophagy in stem cells: repair, remodelling and metabolic reprogramming. Development. 2018;145(4):146506.
Carnero A, Lleonart M. The hypoxic microenvironment: A determinant of cancer stem cell evolution. Inside the Cell. 2016;1(2):96–105.
Sowter HM, Ratcliffe PJ, Watson P, Greenberg AH, Harris AL. HIF-1-dependent regulation of hypoxic induction of the cell death factors BNIP3 and NIX in human tumors. Cancer Res. 2001;61(18):6669–73.
Roscigno G, Puoti I, Giordano I, Donnarumma E, Russo V, Affinito A, et al. MiR-24 induces chemotherapy resistance and hypoxic advantage in breast cancer. Oncotarget. 2017;8(12):19507.
Naik PP, Birbrair A, Bhutia SKJC, Sciences ML. Mitophagy-driven metabolic switch reprograms stem cell fate. Cel Mol Life Sci. 2019;76(1):27–43.
Vlashi E, Lagadec C, Vergnes L, Matsutani T, Masui K, Poulou M, et al. Metabolic state of glioma stem cells and nontumorigenic cells. Proc Natl Acad Sci. 2011;108(38):16062–7.
Reitzer LJ, Wice BM, Kennell DJ. Evidence that glutamine, not sugar, is the major energy source for cultured HeLa cells. Proc Natl Acad Sci. 1979;254(8):2669–76.
Nieman KM, Kenny HA, Penicka CV, Ladanyi A, Buell-Gutbrod R, Zillhardt MR, et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nature Med. 2011;17(11):1498–503.
Vazquez Rodriguez G, Abrahamsson A, Jensen LDE, Dabrosin C. Adipocytes promote early steps of breast cancer cell dissemination via interleukin-8. Front Immunol. 2018;9:1767.
Al-Khalaf HH, Al-Harbi B, Al-Sayed A, Arafah M, Tulbah A, Jarman A, et al. Interleukin-8 activates breast cancer-associated adipocytes and promotes their angiogenesis-and tumorigenesis-promoting effects. Mol Cell Biol. 2019;39(2):e00332-e418.
Razmkhah M, Jaberipour M, Hosseini A, Safaei A, Khalatbari B, Ghaderi A. Expression profile of IL-8 and growth factors in breast cancer cells and adipose-derived stem cells (ASCs) isolated from breast carcinoma. Cellular Immunol. 2010;265(1):80–5.
Yasumoto Y, Miyazaki H, Vaidyan LK, Kagawa Y, Ebrahimi M, Yamamoto Y, et al. Inhibition of fatty acid synthase decreases expression of stemness markers in glioma stem cells. PLoS ONE. 2016;11(1): e0147717.
Choi S, Yoo YJ, Kim H, Lee H, Chung H, Nam M-H, et al. Clinical and biochemical relevance of monounsaturated fatty acid metabolism targeting strategy for cancer stem cell elimination in colon cancer. Biochem Biophys Res Commun. 2019;519(1):100–5.
Wang C, Ma J, Zhang N, Yang Q, Jin Y, Wang Y. The acetyl-CoA carboxylase enzyme: a target for cancer therapy? Expert Rev Anticancer Ther. 2015;15(6):667–76.
Lucenay KS, Doostan I, Karakas C, Bui T, Ding Z, Mills GB, et al. Cyclin E associates with the lipogenic enzyme ATP-citrate lyase to enable malignant growth of breast cancer cells. Cancer Res. 2016;76(8):2406–18.
Beloribi-Djefaflia S, Vasseur S, Guillaumond F. Lipid metabolic reprogramming in cancer cells. Oncogenesis. 2016;5(1):e189.
Tyanova S, Albrechtsen R, Kronqvist P, Cox J, Mann M, Geiger T. Proteomic maps of breast cancer subtypes. Nature commun. 2016;7(1):1–11.
Cao MD, Lamichhane S, Lundgren S, Bofin A, Fjøsne H, Giskeødegård GF, et al. Metabolic characterization of triple negative breast cancer. BMC Cancer. 2014;14(1):1–12.
El Ansari R, Craze ML, Miligy I, Diez-Rodriguez M, Nolan CC, Ellis IO, et al. The amino acid transporter SLC7A5 confers a poor prognosis in the highly proliferative breast cancer subtypes and is a key therapeutic target in luminal B tumours. Breast Cancer Res. 2018;20(1):1–17.
El Ansari R, McIntyre A, Craze ML, Ellis IO, Rakha EA, Green AR. Altered glutamine metabolism in breast cancer; subtype dependencies and alternative adaptations. Histopathology. 2018;72(2):183–90.
Sun X, Wang M, Wang M, Yu X, Guo J, Sun T, et al. Metabolic reprogramming in triple-negative breast cancer. Front oncol. 2020;10:428.
Wang Z, Jiang Q, Dong C. Metabolic reprogramming in triple-negative breast cancer. Front onco. 2020;17(1):44.
Gong Y, Ji P, Yang Y-S, Xie S, Yu T-J, Xiao Y, et al. Metabolic-pathway-based subtyping of triple-negative breast cancer reveals potential therapeutic targets. Cell metabol. 2021;33(1):51–64.
Kuzu OF, Noory MA, Robertson GP. The role of cholesterol in cancer. Cancer Res. 2016;76(8):2063–70.
Lee J, Shin JE, Lee B, Kim H, Jeon Y, Ahn SH, et al. The stem cell marker Prom1 promotes axon regeneration by down-regulating cholesterol synthesis via Smad signaling. Proc Natl Acad Sci. 2020;117(27):15955–66.
Li X, Wu JB, Li Q, Shigemura K, Chung LW, Huang W-C. SREBP-2 promotes stem cell-like properties and metastasis by transcriptional activation of c-Myc in prostate cancer. Oncotarget. 2016;7(11):12869.
Visweswaran M, Arfuso F, Warrier S, Dharmarajan A. Aberrant lipid metabolism as an emerging therapeutic strategy to target cancer stem cells. Front Oncol. 2020;38(1):6–14.
Corominas-Faja B, Cuyàs E, Gumuzio J, Bosch-Barrera J, Leis O, Martin ÁG, et al. Chemical inhibition of acetyl-CoA carboxylase suppresses self-renewal growth of cancer stem cells. Oncotarget. 2014;5(18):8306.
Zhang T, Xie J, Arai S, Wang L, Shi X, Shi N, et al. The efficacy and safety of anti-PD-1/PD-L1 antibodies for treatment of advanced or refractory cancers: a meta-analysis. 2016;7(45):73068.
Cole AJ, Fayomi AP, Anyaeche VI, Bai S, Buckanovich RJ. An evolving paradigm of cancer stem cell hierarchies: therapeutic implications. Theranostics. 2020;10(7):3083.
Verbaanderd C, Maes H, Schaaf MB, Sukhatme VP, Pantziarka P, Sukhatme V, et al. Repurposing Drugs in Oncology (ReDO)—chloroquine and hydroxychloroquine as anti-cancer agents. 2017;11.
Rahman MA, Saha SK, Rahman MS, Uddin MJ, Uddin MS, Pang M-G, et al. Molecular insights into therapeutic potential of autophagy modulation by natural products for cancer stem cells. Front Cell Dev Biol. 2020;8:283.
Rath S, Liebl J, Fürst R, Vollmar AM, Zahler S. Regulation of endothelial signaling and migration by v-ATPase. Angiogenesis. 2014;17(3):587–601.
Garza-Lombó C, Pappa A, Panayiotidis MI, Franco R. Redox homeostasis, oxidative stress and mitophagy. Circul Res. 2020;51:105–17.
Kubli DA, Gustafsson ÅB. Mitochondria and mitophagy: the yin and yang of cell death control. Circul Res. 2012;111(9):1208–21.
Ngabire D, Kim G-D. Autophagy and inflammatory response in the tumor microenvironment. Int J Mol Sci. 2017;18(9):2016.
Yang X, Yu D-D, Yan F, Jing Y-Y, Han Z-P, Sun K, et al. The role of autophagy induced by tumor microenvironment in different cells and stages of cancer. Cell Biosci. 2015;5(1):1–11.
Maes H, Rubio N, Garg AD, Agostinis P. Autophagy: shaping the tumor microenvironment and therapeutic response. Trends Mol Med. 2013;19(7):428–46.
Mowers EE, Sharifi MN, Macleod KF. Functions of autophagy in the tumor microenvironment and cancer metastasis. 2018;285(10):1751–66.
Katheder NS, Khezri R, O’Farrell F, Schultz SW, Jain A, Rahman MM, et al. Microenvironmental autophagy promotes tumour growth. Nature. 2017;541(7637):417–20.
Ho TT, Warr MR, Adelman ER, Lansinger OM, Flach J, Verovskaya EV, et al. Autophagy maintains the metabolism and function of young and old stem cells. Nature. 2017;543(7644):205–10.
Pietrocola F, Pol J, Kroemer G. Fasting improves anticancer immunosurveillance via autophagy induction in malignant cells. Cell Cycle. 2016;15(24):3327–8.
Turcotte S, Giaccia AJ. Targeting cancer cells through autophagy for anticancer therapy. Curr Opin Cell Biol. 2010;22(2):246–51.
Janku F, McConkey DJ, Hong DS, Kurzrock R. Autophagy as a target for anticancer therapy. Nat Rev Clin Oncol. 2011;8(9):528–39.
Hashimoto D, Bläuer M, Hirota M, Ikonen NH, Sand, Laukkarinen J. Autophagy is needed for the growth of pancreatic adenocarcinoma and has a cytoprotective effect against anticancer drugs. Eur J Cancer. 2014;50(7):1382–90.
Heddleston J, Li Z, Lathia J, Bao S, Hjelmeland A, Rich J. Hypoxia inducible factors in cancer stem cells. Br J Cancer. 2010;102(5):789–95.
Rozpedek W, Pytel D, Mucha B, Leszczynska H, Diehl JA, Majsterek IJCmm. The role of the PERK/eIF2α/ATF4/CHOP signaling pathway in tumor progression during endoplasmic reticulum stress. 2016;16(6):533–44.
Russell RC, Yuan H-X, Guan K-L. Autophagy regulation by nutrient signaling. Cell Res. 2014;24(1):42–57.
Mauthe M, Orhon I, Rocchi C, Zhou X, Luhr M, Hijlkema K-J, et al. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy. 2018;14(8):1435–55.
Xu R, Ji Z, Xu C, Zhu JJM. The clinical value of using chloroquine or hydroxychloroquine as autophagy inhibitors in the treatment of cancers: A systematic review and meta-analysis. 2018;97(46).
Vega-Rubín-de-Celis S, Zou Z, Fernández ÁF, Ci B, Kim M, Xiao G, et al. Increased autophagy blocks HER2-mediated breast tumorigenesis. 2018;115(16):4176–81.
Muntean AG, Hess JL. Epigenetic dysregulation in cancer. Am J Pathol. 2009;175(4):1353–61.
Audia JE, Campbell RM. Histone modifications and cancer. Cold Spring Harbor perspect biol. 2016;8(4): a019521.
Casalino L, Verde P. Multifaceted roles of DNA methylation in neoplastic transformation, from tumor suppressors to EMT and metastasis. Genes. 2020;11(8):922.
Temian DC, Pop LA, Irimie AI, Berindan-Neagoe IJ. The epigenetics of triple-negative and basal-like breast cancer: current knowledge. J Breast Cancer. 2018;21(3):233–43.
Berger SL, Sassone-Corsi P. Metabolic signaling to chromatin. Cold Spring Harbor perspect biol. 2016;8(11): a019463.
Aldana-Masangkay GI, Sakamoto KMJJoB, Biotechnology. The role of HDAC6 in cancer. 2010;2011.
Rao M, Chinnasamy N, Hong JA, Zhang Y, Zhang M, Xi S, et al. Inhibition of histone lysine methylation enhances cancer–testis antigen expression in lung cancer cells: Implications for adoptive immunotherapy of cancer. 2011;71(12):4192–204.
Mandhair HK, Novak U, Radpour R. Epigenetic regulation of autophagy: A key modification in cancer cells and cancer stem cells. World Journal Stem Cells. 2021;13(6):542.
Liao Y-P, Chen L-Y, Huang R-L, Su P-H, Chan MW, Chang C-C, et al. Hypomethylation signature of tumor-initiating cells predicts poor prognosis of ovarian cancer patients. Human mol genet. 2014;23(7):1894–906.
Mandhair HK, Arambasic M, Novak U, Radpour R. WJSC. 2020.
Zhu J, Huang G, Hua X, Li Y, Yan H, Che X, et al. CD44s is a crucial ATG7 downstream regulator for stem-like property, invasion, and lung metastasis of human bladder cancer (BC) cells. 2019;38(17):3301–15.
Kim TW, Lee SY, Kim M, Cheon C, Ko S-GJCd, disease. Kaempferol induces autophagic cell death via IRE1-JNK-CHOP pathway and inhibition of G9a in gastric cancer cells. 2018;9(9):1–14.
Sharif T, Martell E, Dai C, Ghassemi-Rad MS, Hanes MR, Murphy PJ, et al. HDAC6 differentially regulates autophagy in stem-like versus differentiated cancer cells. 2019;15(4):686–706.
Yang W, Liu Y, Gao R, Yu H, Sun TJCl. HDAC6 inhibition induces glioma stem cells differentiation and enhances cellular radiation sensitivity through the SHH/Gli1 signaling pathway. 2018;415:164–76.
Feinberg AP, Koldobskiy MA, Göndör A. Epigenetic modulators, modifiers and mediators in cancer aetiology and progression. Nat Rev Genet. 2016;17(5):284–99.
Kim J-A, Yeom YI. Metabolic signaling to epigenetic alterations in cancer. Biomol ther. 2018;26(1):69.
Stellingwerff T, LeBlanc PJ, Hollidge MG, Heigenhauser GJ, Spriet LL. Metabolism Hyperoxia decreases muscle glycogenolysis, lactate production, and lactate efflux during steady-state exercise. Am J Physiol-Endocrinol Metabol. 2006;290(6):E1180–90.
Ullmann P, Qureshi-Baig K, Rodriguez F, Ginolhac A, Nonnenmacher Y, Ternes D, et al. Hypoxia-responsive miR-210 promotes self-renewal capacity of colon tumor-initiating cells by repressing ISCU and by inducing lactate production. Oncotarget. 2016;7(40):65454.
Romero-Garcia S, Moreno-Altamirano MMB, Prado-Garcia H, Sánchez-García FJ. Lactate contribution to the tumor microenvironment: mechanisms, effects on immune cells and therapeutic relevance Frontiers in immunology. Front Immunol. 2016;7:52.
Dhup S, Kumar Dadhich R, Ettore Porporato P, Sonveaux P. Multiple biological activities of lactic acid in cancer: influences on tumor growth, angiogenesis and metastasis. Curr Pharm Des. 2012;18(10):1319–30.
Lardner A. The effects of extracellular pH on immune function. J leukocyte biology. 2001;69(4):522–30.
Dayem AA, Choi H-Y, Kim J-H, Cho S-G. Role of oxidative stress in stem, cancer, and cancer stem cells. Cancers. 2010;2(2):859–84.
Garcia-Mayea Y, Mir C, Masson F, Paciucci R, LLeonart M, editors. Insights into new mechanisms and models of cancer stem cell multidrug resistance.In: Seminars in cancer biology. Amsterdam: Elsevier. 2020
Chandel NS. NADPH—the forgotten reducing equivalent. Cold Spring Harb Perspect Biol. 2021;13(6):a040550.
Fang Y-Z, Yang S, Wu GJN. Free radicals, antioxidants, and nutrition. Nutrition. 2002;18(10):872–9.
Ju H-Q, Lin J-F, Tian T, Xie D, Xu R-H. NADPH homeostasis in cancer: functions, mechanisms and therapeutic implications. Signal Transduct Target Ther. 2020;5(1):1–12.
Kozovska Z, Patsalias A, Bajzik V, Durinikova E, Demkova L, Jargasova S, et al. ALDH1A inhibition sensitizes colon cancer cells to chemotherapy. BMC Cancer. 2018;18(1):1–11.
Xu M, Luo JJC. Alcohol and cancer stem cells. Cancers. 2017;9(11):158.
Pastò A, Bellio C, Pilotto G, Ciminale V, Silic-Benussi M,Guzzo G, et al. Cancer stem cells from epithelial ovarian cancer patients privilege oxidative phosphorylation, and resist glucose deprivation. Oncotarget. 2014;5(12):4305.
Guo JY, Karsli-Uzunbas G, Mathew R, Aisner SC, Kamphorst JJ, Strohecker AM, et al. Autophagy suppresses progression of K-ras-induced lung tumors to oncocytomas and maintains lipid homeostasis. Genes Dev. 2013;27(13):1447–61.
Pitolli C, Wang Y, Candi E, Shi Y, Melino G, Amelio IJC. p53-mediated tumor suppression: DNA-damage response and alternative mechanisms. Cancers. 2019;11(12):1983.
Liberti MV, Locasale JW. The Warburg effect: how does it benefit cancer cells? Trends Biochem Sci. 2016;41(3):211–8.
Hart PC, Mao M, De Abreu ALP, Ansenberger-Fricano K, Ekoue DN, Ganini D, et al. MnSOD upregulation sustains the Warburg effect via mitochondrial ROS and AMPK-dependent signalling in cancer. Nat Commun. 2015;6(1):1–14.
Shibuya K, Okada M, Suzuki S, Seino M, Seino S, Takeda H, et al. Targeting the facilitative glucose transporter GLUT1 inhibits the self-renewal and tumor-initiating capacity of cancer stem cells. Oncotarget. 2015;6(2):651.
Zhou J, Ng S-B, Chng W-J. LIN28/LIN28B: an emerging oncogenic driver in cancer stem cells. Int J Biochem Cell Biol. 2013;45(5):973–8.
Ma W, Ma J, Xu J, Qiao C, Branscum A, Cardenas A, et al. Lin28 regulates BMP4 and functions with Oct4 to affect ovarian tumor microenvironment. Cell Cycle. 2013;12(1):88–97.
Chen C, Bai L, Cao F, Wang S, He H, Song M, et al. Targeting LIN28B reprograms tumor glucose metabolism and acidic microenvironment to suppress cancer stemness and metastasis. Oncogene. 2019;38(23):4527–39.
Arnér ES, Holmgren A. Physiological functions of thioredoxin and thioredoxin reductase. Eur J Biochem. 2000;267(20):6102–9.
Rundlöf A-K, Arnér ES. Regulation of the mammalian selenoprotein thioredoxin reductase 1 in relation to cellular phenotype growth and signaling events. Antioxid Redox Signal. 2004;6(1):41–52.
Gencheva R, Arnér ES. Thioredoxin reductase inhibition for cancer therapy. Annu Rev Pharmacol Toxicol. 2022;62:177–96.
Cadenas C, Franckenstein D, Schmidt M, Gehrmann M, Hermes M, Geppert B, et al. Role of thioredoxin reductase 1 and thioredoxin interacting protein in prognosis of breast cancer. Breast Cancer Res. 2010;12(3):1–15.
Casagrande N, DePaoli M, Celegato M, Borghese C, Mongiat M, Colombatti A, et al. Preclinical evaluation of a new liposomal formulation of cisplatin, lipoplatin, to treat cisplatin-resistant cervical cancer. Gynecol Oncol. 2013;131(3):744–52.
He C, Danes JM, Hart PC, Zhu Y, Huang Y, de Abreu AL, et al. SOD2 acetylation on lysine 68 promotes stem cell reprogramming in breast cancer. Proc Natl Acad Sci. 2019;116(47):23534–41.
Ciavardelli D, Rossi C, Barcaroli D, Volpe S, Consalvo A, Zucchelli M, et al. Breast cancer stem cells rely on fermentative glycolysis and are sensitive to 2-deoxyglucose treatment. Cell Death Dis. 2014;5(7):e1336.
Dong C, Yuan T, Wu Y, Wang Y, Fan TW, Miriyala S, et al. Loss of FBP1 by Snail-mediated repression provides metabolic advantages in basal-like breast cancer. Cancer Cell. 2013;23(3):316–31.
Nagy P, Sándor GO, Juhász G. Autophagy maintains stem cells and intestinal homeostasis in Drosophila. Sci Rep. 2018;8(1):1–9.
García-Prat L, Martínez-Vicente M, Perdiguero E, Ortet L, Rodríguez-Ubreva J, Rebollo E, et al. Autophagy maintains stemness by preventing senescence. Nature. 2016;529(7584):37–42.
Peng Q, Qin J, Zhang Y, Cheng X, Wang X, Lu W, et al. Autophagy maintains the stemness of ovarian cancer stem cells by FOXA2. J Exp Clin Cancer Res. 2017;36(1):1–12.
Babaei G, Aziz SG-G, Jaghi NZZ. EMT, cancer stem cells and autophagy; The three main axes of metastasis. Biomed Pharmacother. 2021;133:110909.
Lunt SJ, Chaudary N, Hill RP. metastasis e The tumor microenvironment and metastatic disease. Clin Exp Metas. 2009;26(1):19–34.
Goubran HA, Kotb RR, Stakiw J, Emara ME, Burnouf T. metastasis Regulation of tumor growth and metastasis: the role of tumor microenvironment. Cancer growth and metastasis. 2014;7:11285.
Wood SL, Pernemalm M, Crosbie Whetton PAAD. The role of the tumor-microenvironment in lung cancer-metastasis and its relationship to potential therapeutic targets. Cancer Treat Rev. 2014;40(4):558–66.
Esendagli G, Bruderek K, Goldmann T, Busche A, Branscheid D, Vollmer E, et al. Malignant and non-malignant lung tissue areas are differentially populated by natural killer cells and regulatory T cells in non-small cell lung cancer. Lung Cancer. 2008;59(1):32–40.
Qian B-Z, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9(4):239–52.
Ahmed N, Escalona R, Leung D, Chan E, Kannourakis G, editors. Tumour microenvironment and metabolic plasticity in cancer and cancer stem cells: Perspectives on metabolic and immune regulatory signatures in chemoresistant ovarian cancer stem cells. Seminars in Cancer Biology; Elsevier. 2018.
Mitchem JB, Brennan DJ, Knolhoff BL, Belt BA, Zhu Y, Sanford DE, et al. Targeting tumor-infiltrating macrophages decreases tumor-initiating cells, relieves immunosuppression, and improves chemotherapeutic responses. Can Res. 2013;73(3):1128–41.
Kobune M, Iyama S, Kikuchi S, Horiguchi H, Sato T, Murase K, et al. Stromal cells expressing hedgehog-interacting protein regulate the proliferation of myeloid neoplasms. Blood cancer Jornal. 2012;2(9):e87.
Lonardo E, Frias-Aldeguer J, Hermann PC, Heeschen C. Pancreatic stellate cells form a niche for cancer stem cells and promote their self-renewal and invasiveness. Cell Cycle. 2012;11(7):1282–90.
Ye J, Wu D, Wu P, Chen Z, Huang J. The cancer stem cell niche: cross talk between cancer stem cells and their microenvironment. Tumor Biol. 2014;35(5):3945–51.
Varas-Godoy M, Rice G, Illanes SE. The crosstalk between ovarian cancer stem cell niche and the tumor microenvironment. Stem Cells Int. 2017. https://doi.org/10.1155/2017/5263974.
Movahed ZG, Yarani R, Mohammadi P, Mansouri KJB. Pharmacotherapy Sustained oxidative stress instigates differentiation of cancer stem cells into tumor endothelial cells: Pentose phosphate pathway, reactive oxygen species and autophagy crosstalk. Biomed Pharmacother. 2021;139: 111643.
Beck B, Driessens G, Goossens S, Youssef KK, Kuchnio A, Caauwe A, et al. A vascular niche and a VEGF–Nrp1 loop regulate the initiation and stemness of skin tumours. Nature. 2011;478(7369):399–403.
Fitzgerald G, Soro-Arnaiz I, De Bock K. The Warburg effect in endothelial cells and its potential as an anti-angiogenic target in cancer. Fron Cell Dev Biol. 2018;6:100.
Ricci-Vitiani L, Pallini R, Biffoni M, Todaro M, Invernici G, Cenci T, et al. Tumour vascularization via endothelial differentiation of glioblastoma stem-like cells. Nature. 2010;468(7325):824–8.
Krishnamurthy S, Warner KA, Dong Z, Imai A, Nör C, Ward BB, et al. Endothelial interleukin-6 defines the tumorigenic potential of primary human cancer stem cells. Stem cells. 2014;32(11):2845–57.
Acknowledgements
We would also like to thank –Kaneez Fatima and Shariqa Aisha (CSIR-IIIM, India) for critically reading the manuscript, and our colleagues particularly Dr. Reyaz Hassan (University of Kashmir, India), Dr. Abubakar Wani (St. Jude Children's Research Hospital, US) for their fruitful discussions. CSIR for providing publication approval-Institutional publication ID No. CSIR-IIIM/IPR/00475.
Funding
Funding for FM laboratory was provided by the Council of Scientific and Industrial Research (CSIR) India fellowship, a grant from the Department of Biotechnology Ministry of Science and Technology (DBT) (BT/IN/Swiss/48/FM/2018–19). CSIR-SRF budget head for providing fellowship to SK, SR is the recipient of DBT-Ramalingaswami, Government of India.
Author information
Authors and Affiliations
Contributions
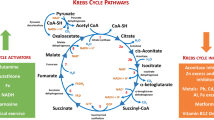
FM supervised the work; SK conceived the idea; SK designed the work; SK, SR, and PS wrote the manuscript; SK, and FM edited the manuscript; SR prepared Fig. 1 and SK prepared Figs. 2 and 3; FM and SK read and approved the final manuscript.
2,
Cancer stem cells sustain mitochondrial health and activity. Cancer stem cells under hypoxia cause metabolic reprogramming and maintain the survival and energetics of cells by activating mitophagy of damaged or excessive mitochondria. Moreover, CSCs activate the antioxidant machinery to remove accumulated genotoxic mitochondria ROS in the cells
3.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khan, S.U., Rayees, S., Sharma, P. et al. Targeting redox regulation and autophagy systems in cancer stem cells. Clin Exp Med 23, 1405–1423 (2023). https://doi.org/10.1007/s10238-022-00955-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-022-00955-5