Abstract
Background
Fecal incontinence is a multifactorial problem and its etiology is complex. Various therapies are available and different success rates have been described. The aim of this study was to assess the effectiveness and safety of non-dynamic graciloplasty in patients with passive fecal incontinence.
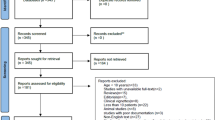
Methods
We retrospectively studied charts of patients with fecal incontinence treated with graciloplasty at our institution from November 2015 until June 2018. Patients were included according to the following criteria: (1) presence of predominantly passive fecal incontinence and (2) presence of a lax perineal body. Primary outcome was the effectiveness, defined as a significant reduction or absence of the complaints of passive fecal incontinence at 3, 6 and 12 months after surgery. Second, we studied the safety of the procedure evaluating the complications within 30 days after surgery.
Results
Thirty-one patients met the inclusion criteria. Twenty-six of them, in addition to passive incontinence as the main symptom, had some degree of fecal urgency. The median age at the first visit to the outpatient clinic was 64.0 years (IQR 52–68). Most patients were female (n = 29, 94%). At 3 months after graciloplasty, 71% (22 of 31) of patients were successfully treated for their passive fecal incontinence. At 6 months, the success rate of the graciloplasty increased to 77%. At 12 months among the patients who were still seen in the clinic, the success rate was 58% (18/31). Two patients cancelled follow-up visits after 3 months, because of failure to control symptoms in 1 case. After 6 months, 9 patients were given the choice to do telephone follow-up only. Of these 11 patients without in-person follow-up, 10 were contacted 1 year after surgery and in 7 of them, the graciloplasty was effective in controlling their passive fecal incontinence for an overall success rate of 80% (25/31). Of the 26 patients with mixed passive and urge incontinence, 6 (23%) still complained of urge incontinence at 1 year. Of these patients with persistent urge incontinence, 6 underwent sacral nerve stimulation which was successful in 4. Two serious complications occurred within 30 days. A rectal perforation requiring temporary colostomy and a recto-vaginal fistula which was successfully repaired.
Conclusion
Non-dynamic graciloplasty is an effective treatment for passive fecal incontinence. Differentiation based on subtypes of fecal incontinence might be important for a pattern-specific approach to treatment. More research is necessary to determine the right indications for more invasive treatments of fecal incontinence.

Similar content being viewed by others
References
Bharucha AE, Zinsmeister AR, Locke GR et al (2005) Prevalence and burden of fecal incontinence: a population-based study in women. Gastroenterology 129:42–49
Ng KS, Sivakumaran Y, Nassar N et al (2015) Fecal incontinence: community prevalence and associated factors—a systematic review. Dis Colon Rectum 58:1194–1209
Simren M, Palsson OS, Whitehead WE (2017) Update on Rome IV criteria for colorectal disorders: implications for clinical practice. Curr Gastroenterol Rep 19:15
Rao SS, Bharucha AE, Chiarioni G et al (2016) Functional anorectal disorders. Gastroenterology 150:143–1442
Van Meegdenburg MM, Meinds RJ, Trzpis M et al (2018) Subtypes and symptoms of fecal incontinence in the Dutch population: a cross-sectional study. Int J Colorectal Dis 33:919–925
Melenhorst J, Koch SM, Uludag O et al (2008) Is a morphologically intact anal sphincter necessary for success with sacral nerve modulation in patients with faecal incontinence? Colorectal Dis 10:257–262
Uludag O, Koch SM, Vliegen RF (2010) Sacral neuromodulation: does it affect the rectoanal angle in patients with fecal incontinence? World J Surg 34:1109–1114
Wald A (2018) Diagnosis and management of fecal incontinence. Curr Gastroenterol Rep 20:9
Mathai V, Seow-Choen F (1995) Anterior rectal mucosal prolapse: an easily treated cause of anorectal symptoms. Br J Surg 82:753–754
Mattana C, Maria G, Pescatori M (1989) Rubber band ligation of hemorrhoids and rectal mucosal prolapse in constipated patients. Dis Colon Rectum 32:372–375
Pickrell KL, Broadbent TR, Masters FW et al (1952) Construction of a rectal sphincter and restoration of anal continence by transplanting the gracilis muscle; a report of four cases in children. Ann Surg 135:853–862
Leguit P Jr, van Baal JG, Brummelkamp WH (1985) Gracilis muscle transposition in the treatment of fecal incontinence. Long-term follow-up and evaluation of anal pressure recordings. Dis Colon Rectum 28:1–4
Christiansen J, Sørensen M, Rasmussen OO (1990) Gracilis muscle transposition for faecal incontinence. Br J Surg 77:1039–1040
Faucheron JL, Hannoun L, Thome C et al (1994) Is fecal continence improved by nonstimulated gracilis muscle transposition? Dis Colon Rectum 37:979–983
Pickrell K, Masters F, Georgiade N et al (1954) Rectal sphincter reconstruction using gracilis muscle transplant. Plast Reconstr Surg (1946) 13:46–55
Pickrell K, Georgiade N, Maguire C et al (1955) Correction of rectal incontinence; transplantation of the gracilis muscle to construct a rectal sphincter. Am J Surg 90:721–726
Corman ML (1985) Gracilis muscle transposition for anal incontinence: late results. Br J Surg 72(Suppl):S21-22
Eccersley AJ, Lunniss PJ, Williams NS (1999) Unstimulated graciloplasty in traumatic faecal incontinence. Br J Surg 86:1071–1072
Baeten C, Spaans F, Fluks A (1988) An implanted neuromuscular stimulator for fecal continence following previously implanted gracilis muscle. report of a case. Dis Colon Rectum 31:134–137
Boyle DJ, Murphy J, Hotouras A et al (2014) Electrically stimulated gracilis neosphincter for end-stage fecal incontinence: the long-term outcome. Dis Colon Rectum 57:215–222
Rongen MJ, Uludag O, El Nagger K (2003) Long-term follow-up of dynamic graciloplasty for fecal incontinence. Dis Colon Rectum 46:716–721
Walega P, Romaniszyn M, Siarkiewicz B et al (2015) Dynamic versus adynamic graciloplasty in treatment of end-stage fecal incontinence: is the implantation of the pacemaker really necessary? 12-month follow-up in a clinical, physiological, and functional study. Gastroenterol Res Pract 2015:698516
Gohil AJ, Gupta AK, Jesudason MR et al (2019) Graciloplasty for anal incontinence—is electrical stimulation necessary? Ann Plast Surg 82:671–678
Baeten CG, Geerdes BP, Adang EM et al (1995) Anal dynamic graciloplasty in the treatment of intractable fecal incontinence. N Engl J Med 322:1600–1605
Pickrell K, Georgiade N, Richard EF et al (1959) Gracilis muscle transplant for the correction of neurogenic rectal incontinence. Surg Clin North Am 39:1405–1415
Baeten CG, Bailey HR, Bakka A et al (2000) Safety and efficacy of dynamic graciloplasty for fecal incontinence: report of a prospective, multicenter trial. Dynamic Graciloplasty Therapy Study Group. Dis Colon Rectum 43:743–751
Chapman AE, Geerdes B, Hewett P et al (2002) Systematic review of dynamic graciloplasty in the treatment of faecal incontinence. Br J Surg 89:138–153
Rosen HR, Novi G, Zoech G et al (1998) Restoration of anal sphincter function by single-stage dynamic graciloplasty with a modified (split sling) technique. Am J Surg 175:187–193
Janssen PTJ, Komen N, Melenhorst J et al (2017) Sacral neuromodulation for fecal incontinence: a review of the central mechanisms of action. J Clin Gastroenterol 51:669–676
Koch SM, Uludag O, El Nagger K et al (2008) Colonic irrigation for defecation disorders after dynamic graciloplasty. Int J Colorectal Dis 32:195–200
Koch SM, Uludag O, Rongen MJ et al (2004) Dynamic graciloplasty in patients born with anal atresia. Dis Colon Rectum 47:1711–1719
Acknowledgements
We would like to thank Herand Abcarian for his critical view and constructive comments on this manuscript.
Author information
Authors and Affiliations
Contributions
MEK: contribution to the study conception and design, collecting data, conduct statistical analysis, interpreting data, drafting the manuscript. HSS: contribution to the study conception and design, interpreting data, commenting on the manuscript. MCD: interpreting data, commenting on the manuscript. SMPK: interpreting data, commenting on the manuscript. JTMH: contribution to the study conception and design, interpreting data, commenting on the manuscript. CIMB: contribution to the study conception and design, interpreting data, commenting on the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Conflict of interest
The study has been approved by the local research comittee (Ll/2018-36).
Conflict of interest
Written informed consent was obtained from patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Knol, M.E., Snijders, H.S., DeRuiter, M.C. et al. Non-dynamic graciloplasty is an effective treatment for patients with passive fecal incontinence. Tech Coloproctol 25, 849–855 (2021). https://doi.org/10.1007/s10151-021-02455-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-021-02455-2