Abstract
Introduction
Rectus abdominis diastasis (RAD) ± concomitant hernia is a complex hernia entity of growing significance in everyday clinical practice. Due to a multitude of described surgical techniques, a so far missing universally accepted classification and hardly existing comparative studies, there are no clear recommendations in guidelines. Therefore, “RAD ± concomitant hernia” will be documented as a separate hernia entity in the Herniamed Registry in the future. For this purpose, an appropriate case report form will be developed on the basis of the existing literature.
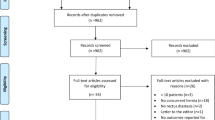
Methods
A systematic search of the available literature was performed in March 2021 using Medline, PubMed, Google Scholar, Scopus, Embase, Springer Link, and the Cochrane Library. 93 publications were identified as relevant for this topic.
Results
In total 45 different surgical techniques for the repair of RAD ± concomitant hernia were identified in the surgical literature. RAD ± concomitant hernia is predominantly repaired by plastic but also by general surgeons. Classification of RAD ± concomitant hernia is based on a proposal of the German Hernia Society and the International Endohernia Society. Surgical techniques are summarized as groups subject to certain aspects: Techniques with abdominoplasty, open techniques, mini-less-open and endoscopic sublay techniques, mini-less-open and endoscopic subcutaneous/preaponeurotic techniques and laparoscopic techniques. Additional data impacting the outcome are also recorded as is the case for other hernia entities. Despite the complexity of this topic, documentation of RAD ± concomitant hernia has not proved to be any more cumbersome than for any of the other hernia entities when using this classification.
Conclusion
Using the case report form described here, the complex hernia entity RAD ± concomitant hernia can be recorded in a registry for proper analysis of comparative treatment options.

Similar content being viewed by others
References
Brooks DC, Butler CE, Collins KA (2015) Rectus abdominis diastasis UpToDate www.uptodate.com. Accessed 6 July 2015
Nahabedian MY (2018) Management strategies for diastasis recti. Semin Plast Surg 32:147–154. https://doi.org/10.1055/s-0038-1661380
Jessen ML, Öberg S, Rosenberg J (2019) Treatment options for abdominal rectus diastasis. Front Surg 19(6):65. https://doi.org/10.3389/fsurg.2019.00065
ElHawary H, Abdelhamid K, Meng F, Janis JE (2020) A comprehensive, evidence-based literature review of the surgical treatment of rectus diastasis. Plast Reconstr Surg 146:1151–1164. https://doi.org/10.1097/PRS.0000000000007252
Akram J, Matzen SH (2014) Rectus abdominis diastasis. J Plast Surg Hand Surg 48:163–169. https://doi.org/10.3109/2000656X.2013.859145
Hickey F, Finch JG, Khanna A (2011) A systematic review on the outcomes of correction of diastasis of the recti. Hernia 15:607–614. https://doi.org/10.1007/s10029-011-0839-4
Mommers EHH, Ponten JEH, Al Omar AK, de Vries Reilingh TS, Bouvy ND, Nienhuijs SW (2017) The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc 31:4934–4949. https://doi.org/10.1007/s00464-017-5607-9
Henriksen NA, Kaufmann R, Simons MP, Berrevoet F, East B, Fischer J, Hope W, Klassen D, Lorenz R, Renard Y, Urena MAG, Montgomery A, European and Americas Hernia Societies (EHS and AHS) (2020) EHS and AHS guidelines for treatment of primary ventral hernias in rare locations or special circumstances. BJS Open 4:342–353. https://doi.org/10.1002/bjs5.50252
Carlstedt A, Bringman S, Egberth M, Emanuelsson P, Olsson A, Petersson U, Pålstedt J, Sandblom G, Sjödahl R, Stark B, Strigård K, Tall J, Theodorsson E (2020) Management of diastasis of the rectus abdominis muscles: recommendations for Swedish national guidelines. Scand J Surg. https://doi.org/10.1177/1457496920961000 (Online ahead of print)
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D et al (2019) Update of guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—part A. Surg Endosc 33:3069–3139. https://doi.org/10.1007/s00464-019-06907-7
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D et al (2019) Update of guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—part B. Surg Endosc 33:3511–3549. https://doi.org/10.1007/s00464-019-06908-6
Bougard H, Collen D, de Beer R, Foscher D, Kloppers JC, Koto MZ et al (2016) HIG (SA) guidelines for the management of ventral hernias hernia interest group South Africa—guideline. SAJS 54:1–29
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault DD, Chelala E et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
Ranney B (1990) Diastasis recti and umbilical hernia causes, recognition and repair. S D J Med 43:5–8
Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny R, Koch A, Kukleta J, Kuthe A, Lorenz R, Stechemesser B (2019) Classification of rectus diastasis—a proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg 3:27. https://doi.org/10.3389/fsurg.2019.00001
Köckerling F, Hoffmann H, Adolf D, Reinpold W, Kirchhoff P, Mayer F, Weyhe D, Lammers B, Emmanuel K (2020) Potential influencing factors on the outcome in incisional hernia repair: a registry-based multivariable analysis of 22,895 patients. Hernia. https://doi.org/10.1007/s10029-020-02184-9 (epub ahead of print)
Köckerling F, Brunner W, Mayer F, Fortelny R, Adolf D, Niebuhr H, Lorenz R, Reinpold W, Zarras K, Weyhe D (2020) Assessment of potential influencing factors on the outcome in small (< 2 cm) umbilical hernia repair—a registry-based multivariable analysis of 31,965 patients. Hernia. https://doi.org/10.1007/s10029-020-02305-4
Axer H, Keyserlingk DG, Prescher A (2001) Collagen fibers in linea alba and rectus sheats. J Surg Res 96:127–134. https://doi.org/10.1006/jsre.2000.6070
Pulei AN, Odula PO, Abdel-Malek AK, Ogeng’o JA (2015) Distribution of elastic fibres in the human abdominal lineal alba anatomy. J Afr 4:476–480
Fachinelli A, Trindade MR, Fachinelli FA (2011) Elastic fibers in the anterior abdominal wall. Hernia 15:409–415. https://doi.org/10.1007/s10029-011-0804-2
Rath AM, Attali P, Dumas JL, Goldlust D, Zhang J, Chevrel JP (1996) The abdominal linea alba: an anatomo-radiologic and biomechanical study. Surg Radiol Anat 18:281–288. https://doi.org/10.1007/BF01627606
Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA (2009) The normal width of the linea alba in nulliparous women. Clin Anat 22:706–711. https://doi.org/10.1002/ca.20836
Qu E, Wu J, Zhang M, Wu L, Zhang T, Xu J, Zhang X (2021) The ultrasound diagnostic criteria for diastasis recti and its correlation with pelvic floor dysfunction in early postpartum women. Quant Imaging Med Surg 11:706–713. https://doi.org/10.21037/qims-20-596
Petrenko AP, Castelo-Branco C, Marshalov DV, Kuligin AV, Mysovskaya YS, Shifman EM, Abdulaev AMR (2020) Physiology of intra-abdominal volume during pregnancy. J Obstet Gynaecol 29:1–7. https://doi.org/10.1080/01443615.2020.1820470 (Online ahead of print)
Lambert DM, Marceau S, Forse RA (2005) Intra-abdominal pressure in the morbidly obese. Obes Surg 15:1225–1232. https://doi.org/10.1381/096089205774512546
Grossi JV, Nicola FF, Zepeda IA, Becker M, Trindade EN, Diemen VV, Cavazzola LT, Trindade MR (2016) Linea alba collagen assessment in morbidly obese patients. Arq Bras Cir Dig 29(Suppl 1):8–11. https://doi.org/10.1590/0102-6720201600S10003
Van de Water AT, Benjamin DR (2016) Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): a systematic review of their measurement properties and meta-analytic reliability generalization. Man Ther 21:41–53. https://doi.org/10.1016/j.math.2015.09.013
Gunnarsson U, Stark B, Dahlstrand U, Strigård K (2015) Correlation between abdominal rectus diastasis width and abdominal muscle strength. Dig Surg 32:112–116. https://doi.org/10.1159/000371859
Wu L, Gu Y, Gu Y, Wang Y, Lu X, Zhu C, Lu Z, Xu H (2021) Diastasis recti abdominis in adult women based on abdominal computed tomography imaging: prevalence, risk factors and its impact on life. J Clin Nurs 30(3–4):518–527. https://doi.org/10.1111/jocn.15568 (Epub 2020 Dec 14)
Aswini D, Shara KNS (2019) An overview of the studies on diastasis recti abdominis in postpartum women. J Gynecol Women’s Health 14(5):JGWH.MS.ID.555900
Emanuelsson P, Gunnarsson U, Dahlstrand U, Strigård K, Stark B (2016) Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: a randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures. Surgery 160:1367–1375. https://doi.org/10.1016/j.surg.2016.05.035
Cheesborough JE, Dumanian GA (2015) Simultaneous prosthetic mesh abdominal wall reconstruction with abdominoplasty for ventral hernia and severe rectus diastasis repairs. Plast Reconstr Surg 135:268–276. https://doi.org/10.1097/PRS.0000000000000840
Carrara A, Catarci M, Fabris L, Zuolo M, Pellecchia L, Moscatelli P, Dorna A, Motter M, Pertile R, Tirone G (2020) Prospective observational study of abdominal wall reconstruction with THT technique in primary midline defects with diastasis recti: clinical and functional outcomes in 110 consecutive patients. Surg Endosc. https://doi.org/10.1007/s00464-020-07997-4 (Online ahead of print)
Köhler G, Luketina RR, Emmanual K (2015) Sutured repair of primary small umbilical and epigastric hernias: concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg 39:121–126. https://doi.org/10.1007/s00268-014-2765-y (discussion 127)
Nishihara Y, Asami M, Shimada T, Kawaguchi Y, Omoto K (2020) Comorbid rectus abdominis diastasis is a risk factor for recurrence of umbilical hernia in Japanese patients. Asian J Endosc Surg. https://doi.org/10.1111/ases.12868 (Online ahead of print)
Reinpold W, Schröder M, Berger C, Stoltenberg W, Köckerling F (2019) MILOS and EMILOS repair of primary umbilical and epigastric hernias. Hernia 23:935–944. https://doi.org/10.1007/s10029-019-02056-x
Lockwood T (1998) Rectus muscle diastasis in males: primary indication for endoscopically assisted abdominoplasty. Plast Reconstr Surg 101:1685–1691. https://doi.org/10.1097/00006534-199805000-00042 (discussion 1692–4)
Chang CJ (2015) Assessment of videoendoscopy-assisted abdominoplasty for diastasis recti patients. Biomed J 36:252–256. https://doi.org/10.4103/2319-4170.113374
Core GB, Mizgala CL, Bowen JC 3rd, Vasconez LO (1995) Endoscopic abdominoplasty with repair of diastasis recti and abdominal wall hernia. Clin Plast Surg 22:707–722
Iglesias M, Bravo L, Chavez-Muñoz C, Barajas-Olivas A (2006) Endoscopic abdominoplasty: an alternative approach. Ann Plast Surg 57:489–494. https://doi.org/10.1097/01.sap.0000229004.25059.87
Ramirez OM (2000) Abdominoplasty and abdominal wall rehabilitation: a comprehensive approach. Plast Reconstr Surg 105:425–435. https://doi.org/10.1097/00006534-200001000-00069
Bruner TW, Salazar-Reyes H, Friedman JD (2009) Umbilical hernia repair in conjunction with abdominoplasty: a surgical technique to maintain umbilical blood supply. Aesthet Surg J 29:333–334. https://doi.org/10.1016/j.asj.2009.02.012
Lari A, Curings P, Person H, Demian H, Braye F, Mabrut J, Mojallal A, Shipkov H (2019) Abdominoplasty with simultaneous laparoscopic umbilical hernia repair: a practical approach to preserve the umbilical vascularization. Ann Chir Plast Esthet 64:237–244. https://doi.org/10.1016/j.anplas.2018.06.015
Van Schalkwyk CP, Dusseldorp JR, Liang DG, Keshava A, Gilmore AJ, Merten S (2018) Concomitant abdominoplasty and laparoscopic umbilical hernia repair. Aesthet Surg J 38:NP196–NP204. https://doi.org/10.1093/asj/sjy100
Person H, Mojallal A, Braye F, Shipkov H (2021) Techniques of concomitant abdominoplasty and umbilical hernia repair: a review. Aesthet Surg J 22:sjab094. https://doi.org/10.1093/asj/sjab094 (Online ahead of print)
McKnight CL, Fowler JL, Cobb WS, Smith DE, Carbonell AM (2012) Concomitant sublay mesh repair of umbilical hernia and abdominoplasty. Can J Plast Surg 20:258–260. https://doi.org/10.1177/229255031202000413
Halsey JN, Ayyala HS, Eid SR, Ciminello FS (2021) Laparoscopic-assisted relocation of the umbilicus with umbilicoplasty in complex abdominal wall reconstruction. Am Surg. https://doi.org/10.1177/00031348211003068 (Online ahead of print)
Phan R, Kaplan E, Porrett JK, Ho YH, Rozen WM (2018) Incisional abdominal hernia repair with concomitant abdominoplasty: maintaining umbilical viability. JPRAS Open 9(16):100–104. https://doi.org/10.1016/j.jpra.2017.09.002
Neinstein RM, Matarasso A, Abramson DL (2015) Concomitant abdominoplasty and umbilical hernia repair using the Ventralex hernia patch. Plast Reconstr Surg 135(4):1021–1025. https://doi.org/10.1097/PRS.0000000000001135
Povedano A, D’allessandro GS, dos Santos LKIL, Munhoz AM, Gemperli R, Goes JCS (2018) Subdermal neo-umbilicoplasty in abdominoplasty. Eur J Plast Surg 41:335–344. https://doi.org/10.1007/s00238-017-1374-z
Pfulg M, Van de Sijpe K, Blondeel P (2005) A simple new technique for neo-umbilicoplasty. Br J Plast Surg 58:688–691. https://doi.org/10.1016/j.bjps.2005.01.013
Lee YT, Kwon C, Rhee SC, Cho SH, Eo SR (2015) Four flaps technique for neo-umbilicoplasty. Arch Plast Surg 42:351–355. https://doi.org/10.5999/aps.2015.42.3.351
Ngaage LM, Kokosis G, Kachniarz B, Pedreira R, Rada EM, Nam AJ, Pearl J, Kavic S, Rasko YM (2019) A two-step technique for neo-umbilicoplasty in the abdominal reconstructive population. Plast Reconstr Surg Glob Open 25(7):e2341. https://doi.org/10.1097/GOX.0000000000002341
Joseph WJ, Sinno S, Brownstone ND, Mirrer J, Thanik VD (2016) Creating the perfect umbilicus: a systematic review of recent literature. Aesthetic Plast Surg 40:372–379. https://doi.org/10.1007/s00266-016-0633-x
da Silva Júnior VV, de Sousa FRS (2017) Improvement on the neo-umbilicoplasty technique and review of the literature. Aesthetic Plast Surg 41:600–607. https://doi.org/10.1007/s00266-017-0847-6
Shiffman MA (2017) Adult umbilical reconstruction: principles and techniques. Springer
Rhemtulla IA, Fischer JP (2018) Retromuscular sublay technique for ventral hernia repair. Semin Plast Surg 32:120–126. https://doi.org/10.1055/s-0038-1666800
Köckerling F, Schug-Pass C, Scheuerlein H (2018) What is he current knowledge about sublay/retro-rectus repair of incisional hernias? Front Surg 5:47. https://doi.org/10.3389/fsurg.2018.00047
Köckerling F (2019) What do we know about the Chevrel technique in ventral incisional hernia repair? Front Surg 6:15. https://doi.org/10.3389/fsurg.2019.00015
El Maksoud WMA, Abbas KS (2018) Onlay hernioplasty versus Rives-Stoppa repair for paraumbilical hernia associated divarication of recti in diabetics in terms of recurrence and surgical site infection: a prospective randomized controlled trial. Egypt J Surg 37:453–459. https://doi.org/10.4103/ejs.ejs_42_18
Privett BJ, Ghusn M (2016) Proposed technique for open repair of a small umbilical hernia and rectus divarication with self-gripping mesh. Hernia 20:527–530. https://doi.org/10.1007/s10029-016-1470-1
Fiori F, Ferrara F, Gobatti D, Gentile D, Stella M (2020) Surgical treatment of diastasis recti: the importance of an overall view of the problem. Hernia. https://doi.org/10.1007/s10029-020-02252-0 (Online ahead of print)
Olsson A, Kiwanuka O, Wilhelmsson S, Sandblom G, Stackelberg O (2019) Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open 3:750–758. https://doi.org/10.1002/bjs5.50213
Schwarz J, Reinpold W, Bittner R (2017) Endoscopic mini-less-open sublay technique (EMILOS) a new technique for ventral hernia repair. Langenbecks Arch Surg 402:173–180. https://doi.org/10.1007/s00423-016-1522-0
Belyansky I, Daes J, Radu VG et al (2018) A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc 32(3):1525–1532. https://doi.org/10.1007/s00464-017-5840-2
Penchev D, Kotashev G, Mutafchiyski V (2019) Endoscopic enhanced-view totally extraperitoneal retromuscular approach for ventral hernia repair. Surg Endosc 33:3749–3756. https://doi.org/10.1007/s00464-019-06669-2
Radu VG, Lica M (2019) The endoscopic retromuscular repair of ventral hernia: the eTEP technique and early results. Hernia 23:945–955. https://doi.org/10.1007/s10029-019-01931-x
Khetan M, Dey A, Bindal V, Suviraj J, Mittal T, Kalhan S, Malik VK, Ramana B (2021) e-TEP repair for midline primary and incisional hernia: technical considerations and initial experience. Hernia. https://doi.org/10.1007/s10029-021-02397-6 (Online ahead of print)
Köhler G, Kaltenböck R, Pfandner R, Dauser B, Lechner M (2020) Precostal top-down extended totally extraperitoneal ventral hernia plasty (eTEP): simplification of a complex technical approach. Hernia 24:527–535. https://doi.org/10.1007/s10029-019-02076-7
Lu R, Addo A, Ewart Z, Broda A, Parlacoski S, Zahiri HR, Belyansky I (2020) Comparative review of outcomes: laparoscopic and robotic enhanced-view totally extraperitoneal (eTEP) access retrorectus repairs. Surg Endosc 34:3597–3605. https://doi.org/10.1007/s00464-019-07132-y
Ngo P, Cossa JP, Largenton C, Johanet H, Gueroult S, Pélissier E (2021) Ventral hernia repair by totally extraperitoneal approach (VTEP): technique description and feasibility study. Surg Endosc 35:1370–1377. https://doi.org/10.1007/s00464-020-07519-2
Li B, Qin C, Bittner R (2020) Totally endoscopic sublay (TES) repair for midline ventral hernia: surgical technique and preliminary results. Surg Endosc 34:1543–1550. https://doi.org/10.1007/s00464-018-6568-3
Tang R, Jiang H, Wu W, Wang T, Meng X, Liu G, Cai X, Liu J, Cui X, Si X, Liu N, Wei N (2020) A preliminary multicenter evaluation of endoscopic sublay repair for ventral hernia from China. BMC Surg 20:233. https://doi.org/10.1186/s12893-020-00888-4
Costa TN, Abdalla RZ, Santo MA, Tavares RR, Abdalla BM, Cecconello I (2016) Transabdominal midline reconstruction by minimally invasive surgery: technique and results. Hernia 20:257–265. https://doi.org/10.1007/s10029-016-1457-y
Manetti G, Lolli MG, Belloni E, Nigri G (2021) A new minimally invasive technique for the repair of diastasis recti: a pilot study. Surg Endosc. https://doi.org/10.1007/s00464-021-08393-2 (Online ahead of print)
Carrara A, Lauro E, Fabris L, Frisini M, Rizzo S (2019) Endo-laparoscopic reconstruction of the abdominal wall midline with linear stapler, the THT technique. Early results of the first case series. Ann Med Surg 38:1–7. https://doi.org/10.1016/j.amsu.2018.12.002
Köckerling F, Botsinis MD, Rohde C, Reinpold W (2016) Endoscopic-assisted linea alba reconstruction plus mesh augmentation for treatment of umbilical and/or epigastric hernias and rectus abdominis diastasis—early results. Front Surg 3:27. https://doi.org/10.3389/fsurg.2016.00027
Köckerling F, Botsinis MD, Rohde C, Reinpold W, Schug-Pass C (2017) Endoscopic-assisted linea alba reconstruction: new technique for treatment of symptomatic umbilical, trocar, and/or epigastric hernias with concomitant rectus abdominis diastasis. Eur Surg 49:71–75. https://doi.org/10.1007/s10353-017-0473-1
Köhler G, Fischer I, Kaltenböck R, Schrittwieser R (2018) Minimal invasive linea alba reconstruction for the treatment of umbilical and epigastric hernias with coexisting rectus abdominis diastasis. J Laparoendosc Adv Surg Tech A 28:1223–1228. https://doi.org/10.1089/lap.2018
Luque JB, Luque AB, Valdivia J, Gráu JMS, Menchero JG, Moreno JG, Jurado JG (2015) Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia 19:493–501. https://doi.org/10.1007/s10029-014-1300-2
Nardi WS, Busnelli GL, Tchercansky A, Pirchi DE, Medina PJ (2018) Diastasis recti associated with midline hernias: totally subcutaneous video-endoscopic repair. J Minim Access Surg 14:161–163. https://doi.org/10.4103/jmas.JMAS_103_17
Claus CMP, Malcher F, Cavazzola LT, Furtado M, Morrell A, Azevedo M, Meirelles LG, Santos H, Garcia R (2018) Systemization of laparoscopic inguinal hernia repair (TAPP) based on a new anatomical concept: inverted y and five triangles. Arq Bras Cir Dig 31(4):e1399. https://doi.org/10.1590/0102-672020180001e1399
Muas DMJ (2019) Preaponeurotic endoscopic repair (REPA) of diastasis recti associated or not to midline hernias. Surg Endosc 33:1777–1782. https://doi.org/10.1007/s00464-018-6450-3
Kler A, Wilson P (2020) Total endoscopic-assisted linea alba reconstruction (TESLAR) for treatment of umbilical/paraumbilical hernia and rectus abdominus diastasis is associated with unacceptable persistent seroma formation: a single centre experience. Hernia 24:1379–1385. https://doi.org/10.1007/s10029-020-02266-8 (Epub 2020 Jul 20)
Schroeder AD, Debus ES, Schroeder M, Reinpold WM (2013) Laparoscopic transperitoneal sublay mesh repair: a new technique for the cure of ventral and incisional hernias. Surg Endosc 27:648–654. https://doi.org/10.1007/s00464-012-2508-9
Siddiky AH, Kapadia CR (2010) Laparoscopic plication of the linea alba as a repair for diastasis recti—a mesh free approach. J Surg Case Rep 2010(5):3. https://doi.org/10.1093/jscr/2010.5.3
Palanivelu C, Rangarajan M, Jategaonkar PA, Amar V, Gokul KS, Srikanth B (2009) Laparoscopic repair of diastasis recti using the ‘Venetian blinds’technique of plication with prosthetic reinforcement: a retrospective study. Hernia 13:287–292. https://doi.org/10.1007/s10029-008-0464-z
Wiessner R, Vorwerk T, Tolla-Jensen C, Gehring A (2017) Continuous laparoscopic closure of the linea alba with barbed sutures combined with laparoscopic mesh implantation (IPOM plus repair) as a new technique for treatment of abdominal hernias. Front Surg 4:62. https://doi.org/10.3389/fsurg.2017.00062
Barbato G, Rollo S, Maggioni C, Cianchi F, Coratti F (2020) Laparoscopic diastasis recti abdominis and midline hernia repair. Minerva Chir. https://doi.org/10.23736/S0026-4733.20.08404-7 (Online ahead of print)
Gómez-Menchero J, Jurado JFG, Grau JMS, Luque JAB, Moreno JLG, Del Agua IA, Morales-Conde S (2018) Laparoscopic intracorporeal rectus aponeuroplasty (LIRA technique): a step forward in minimally invasive abdominal wall reconstruction for ventral hernia repair (LVHR). Surg Endosc 32:3502–3508. https://doi.org/10.1007/s00464-018-6070-y
Sharbaugh ME, Patel PB, Zaman JA, Ata A, Feustel P, Singh K, Singh TP (2021) Robotic ventral hernia repair: a safe and durable approach. Hernia 25:305–312. https://doi.org/10.1007/s10029-019-02074-9
Muysoms F, Van Cleven S, Pletinckx P, Ballecer C, Ramaswamy A (2018) Robotic transabdominal retromuscular umbilical prosthetic hernia repair (TARUP): observational study on the operative time during the learning curve. Hernia 22:1101–1111. https://doi.org/10.1007/s10029-018-1825-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Köckerling, R. Lorenz, B. Stechemesser, J. Conze, A. Kuthe, W. Reinpold, H. Niebuhr, B. Lammers, K. Zarras, R. Fortelny, F. Mayer, H. Hoffmann, J. F. Kukleta, D. Weyhe: nothing to disclose.
Ethical approval
Not applicable.
Human and animal rights
Not applicable.
Informend consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Köckerling, F., Lorenz, R., Stechemesser, B. et al. Comparison of outcomes in rectus abdominis diastasis repair—which data do we need in a hernia registry?. Hernia 25, 891–903 (2021). https://doi.org/10.1007/s10029-021-02466-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02466-w