Abstract
Introduction
How best to treat a small (< 2 cm) umbilical hernia continues to be the subject of controversial debate. The recently published guidelines for treatment of umbilical hernias from the European Hernia Society and Americas Hernia Society recommend open mesh repair for defects ≥ 1 cm. Since the quality of evidence is limited for hernias with defect sizes smaller than 1 cm, suture repair can be considered. To date, little is known about the potential influencing factors on the outcome in small (< 2 cm) umbilical hernia repair. This multivariable analysis of data from the Herniamed Registry now aims to assess these factors.
Methods
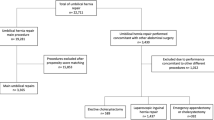
The data of patients with primary elective umbilical hernia repair and defect size < 2 cm entered into the Herniamed Registry from September 1, 2009 to December 31, 2018 were analyzed to assess through multivariable analysis all confirmatory pre-defined potential influencing factors on the primary outcome criteria intraoperative and postoperative complications, general complications, complication-related reoperations, recurrence rate and rates of pain at rest, pain on exertion and chronic pain requiring treatment at 1-year follow-up.
Results
31,965 patients (60%) met the inclusion criteria. The proportion of suture repairs was 78.6% (n = 25,119), of open mesh repairs 15.2% (n = 4853), and of laparoscopic mesh repairs 6.2% (n = 1993). Compared with open mesh repair, suture repair had a highly significantly unfavorable association with the recurrence rate (OR = 1.956 [1.463; 2.614]; p < 0.001). Female gender also had an unfavorable relation to the recurrence rate (OR = 1.644 [1.385; 1.952]; p < 0.001). Compared with open mesh repair, open suture repair had a highly significantly favorable association with the rate of postoperative complications (OR = 0.583 [0.484; 0.702]; p < 0.001) and complication-related reoperations (OR = 0.567 [0.397; 0.810]; p = 0.002).While laparoscopic IPOM showed a favorable relationship with the postoperative complications and complication-related reoperations, it demonstrated an unfavorable association with the intraoperative complications, general complications, recurrence rate and pain rates.
Conclusion
Suture repair continues to be used for 78% of umbilical hernias with a defect < 2 cm. While suture repair has a favorable influence on the rates of postoperative complications and complication-related reoperations, it has a higher risk of recurrence. Female gender also has an unfavorable influence on the recurrence rate. Laparoscopic IPOM appears to be indicated only in settings of obesity (BMI ≥ 30).



Similar content being viewed by others
References
Koebe S, Greenberg J, Huang LC, Phillips S, Lidor A, Funk L, Shada A (2020) Current practice pattern for initial umbilical hernia repair in the United States. Hernia. https://doi.org/10.1007/s10029-020-02164-z(Epub ahead of print)
Statistisches Bundesamt (Destatis), 2019. Artikelnummer: 5231402187005
Alkhatib H, Fafaj A, Olson M, Stewart T, Krpata DM (2019) Primary unclomplicated midline ventral hernias: factors that influence and guide the surgical approach. Hernia. https://doi.org/10.1007/s10029-019-02051-2(Epub ahead of print)
Pawlak M, Tulloh B, de Beaux A (2020) Current trends in hernia surgery in NHS England. Am R Coll Surg Engl 102:25–27. https://doi.org/10.1308/rcsann.2019.0118
Köckerling F, Brunner W, Fortelny R, Mayer F, Adolf D, Niebuhr H, Lorenz R, Reinpold W, Zarras K, Weyhe D. Treatment of small (< 2 cm) umbilical hernias—guidelines and reality. Hernia. (in review)
Aslani N, Brown CJ (2010) Does mesh offer an advantage over tissue in the open repair of umbilical Hernias? A systematic review and meta-analysis. Hernia 14:455–462. https://doi.org/10.1007/s10029-010-0705-9
Nguyen MT, Berger RL, Hicks SC, Davila JA, Li LT, Kao LS, Liang MK (2014) Comparison of outcomes of synthetic mesh versus suture repair of elective primary ventral herniorrhaphy: a systematic review and meta-analysis. JAMA Surg 149:415–421. https://doi.org/10.1001/jamasurg.2013.5014
Mathes T, Walgenbach M, Siegel R (2016) Suture versus mesh repair in primary and incisional ventral hernias: a systematic review and meta-analysis. World J Surg 40:826–835. https://doi.org/10.1007/s00268-015-3311-2
Lopez-Cano M, Martin-Dominguez LA, Pereira JA, Armengo-Carrasco M, Garcia-Alamino JM (2018) Balancing mesh-related complications and benefits in primary ventral and incisional hernia surgery. A meta-analysis and trial sequential analysis. PLoS ONE 13(6):e0197813. https://doi.org/10.1371/journal.pone.01978813
Bisgaard T, Kaufmann R, Christoffersen MW, Strandfelt P, Gluud LL (2019) Lower risk of recurrence after mesh repair versus non-mesh sutured repair in open umbilical hernia repair: a systematic review and meta-analysis of randomized controlled trials. Scand J Surg 108:187–193. https://doi.org/10.1177/1457496918812208
Shrestha D, Shrestha A, Shrestha B (2019) Open mesh versus suture repair of umbilical hernia: meta-analysis of randomized controlled trials. Int J Surg 62:62–66. https://doi.org/10.1016/j.ijsu.2018.12.015
Madsen LJ, Oma E, Jorgensen LN, Jensen KK (2020) Mesh versus suture in elective repair of umbilical hernia systematic review and meta-analysis. BJS Open 3:369–379. https://doi.org/10.1002/bjs5.50276
Aiolfi A, Cavalli M, Micheletto G, Bruni PG, Lombardo F, Morlacchi A, Bonitta G, Campanelli G, Bona D (2020) Open mesh versus. suture umbiloical hernia repair: systematic review and updated trial sequential meta-analysis of randomized controlled trials. Hernia. https://doi.org/10.1007/s10029-020-02146-1
Hajibandeh S, Hajibandeh S, Sreh A, Khan A, Subar D, Jones L (2017) Laparoscopic versus open umbilical or paraumbilical hernia repair: a systematic review and meta-analysis. Hernia. https://doi.org/10.1007/s10029-017-1683-y
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
Kaufmann R, Halm JA, Eker HH, Klitsie PJ, Nieuwenhuizen J, van Geldere D et al (2018) Mesh versus suture repair of umbilical hernia in adults: a randomised, double-blind, controlled, multicentre trial. Lancet 391:860–869. https://doi.org/10.1016/S0140-6736(18)30298-8
Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2015) Long-term recurrence and chronic pain after repair for small umbilical or epigastric hernias: a regional cohort study. Am J Surg 209:725–732. https://doi.org/10.1016/j.amjsurg.2014.05.021
Christoffersen MW, Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T (2013) Lower reoperation rate for recurrence after mesh versus sutured elective repair in small umbilical and epigastric hernias. A nationwide register study. World J Surg 37:2548–2552. https://doi.org/10.1007/s00268-013-2160-0
Henriksen NA, Montgomery A, Kaufmann R, Berrevoet E, East B, Fischer J et al (2020) Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Amercas Hernia Society. BJS 107:171–190. https://doi.org/10.1002/bjs.11489
Mitura K, Skolimowska-Rzewuska M, Rzewuska A, Wyrzykowska D (2020) Is mesh always necessary in every small umbilical hernia repair? Comparison of standardized primary sutured versus patch repair: retrospective cohort study. Hernia. https://doi.org/10.1007/s10029-020-02170-1(Epub ahead of print)
Stechemesser B, Jacob DA, Schug-Pass C, Köckerling F (2012) Herniamed: an internet-based registry for outcome research in hernia surgery. Hernia 16:269–276. https://doi.org/10.1007/s10029-012-0908.3
Kyle-Leinhase I, Köckerling F, Jorgensen LN, Montgomery A, Gillion JF, Rodriguez JAP, Hope W, Muysoms F (2018) Comparison of hernia registries: the CORE project. Hernia 22:561–575. https://doi.org/10.1007/s10029-017-1724-6
Köckerling F, Simon T, Hukauf M, Hellinger A, Fortelny R, Reinpold W, Bittner R (2018) The importance of registries in the postmarketing surveillance of surgical meshes. Ann Surg 268:1097–1104. https://doi.org/10.1097/SLA.0000000000002326
Köckerling F, Hoffmann H, Adolf D, Reinpold W, Kirchhoff P, Mayer F, Weyhe D, Lammers B, Emmanuel K (2020) Potential influencing factors on the outcome in incisional hernia repair: a registry-based multivariable analysis of 22,895 patients. Hernia. https://doi.org/10.1007/s10029-020-02184-9(Epub ahead of print)
Williams KN, Hussain L, Fellner AN, Meister KM (2020) Updated outcomes of laparoscopic versus open umbilical hernia repair in patients with obesity based on a National Surgical Quality Improvement Program review. Surg Endosc. https://doi.org/10.1007/s00464-019-07129-7(Epub ahead of print)
Fafaj A, Tastaldi L, Alkhatib H, Tish S, AlMarzooqu R, Olson MA, Steward TG et al (2020) Is there an advantage to laparoscopy over open repair of primary umbilical hernias in obese patients? An analysis of the Americas Hernia Society Quality Collaborative (AHSQC). Hernia. https://doi.org/10.1007/s10029-020-02218-2(Epub ahead of print)
Cassie S, Okrainec A, Saleh F, Quereshy FS, Jackson TD (2014) Laparocopic versus open elective repair of primary umbilical hernias: short-term outcomes from the American College of Surgeons National Surgery Quality Improvement Program. Surg Endosc 28:741–746. https://doi.org/10.1007/s00464-013-3252-5
Funding
This multivariable analysis was only possible with the funding support of the “Austrian Hernia Forum”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Köckerling reports grants from Johnson & Johnson, Norderstedt, grants from Karl Storz, Tuttlingen, grants from pfm medical, Cologne, grants from Dahlhausen, Cologne, grants from B Braun, Tuttlingen, grants from MenkeMed, Munich, grants from Bard, Karlsruhe, during the conduct of the study; personal fees from Bard, Karlsruhe, outside the submitted work. All other authors have nothing to disclose.
Ethical approval
As only cases of routine hernia surgery are documented in the Herniamed Registry, an ethical approval was not necessary.
Human and animal rights
This article does not contain any study with animals performed by any of the authors.
Informed consent
All patients with routine hernia surgery documented in the Herniamed Registry have signed an informed consent declaration agreeing to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Köckerling, F., Brunner, W., Mayer, F. et al. Assessment of potential influencing factors on the outcome in small (< 2 cm) umbilical hernia repair: a registry-based multivariable analysis of 31,965 patients. Hernia 25, 587–603 (2021). https://doi.org/10.1007/s10029-020-02305-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02305-4