Abstract
Background
One standard repair technique for groin hernias does not exist. The objective of this study is to perform an update meta-analysis and trial sequential analysis to investigate if there is a difference in terms of recurrence between laparoscopic and open primary unilateral uncomplicated inguinal hernia repair.
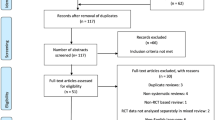
Methods
The reporting methodology conforms to PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines. Randomised controlled trials only were included. The intervention was laparoscopic mesh repair (transabdominal preperitoneal (TAPP) and totally extraperitoneal (TEP)). The control group was Lichtenstein repair. The primary outcome was recurrence rate and secondary outcomes were acute and chronic post-operative pain, morbidity and quality of life.
Results
This study included 12 randomised controlled trials with 3966 patients randomised to Lichtenstein repair (n = 1926) or laparoscopic repair (n = 2040). There were no significant differences in recurrence rates between the laparoscopic and open groups (odds ratio (OR) 1.14, 95% CI 0.51–2.55, p = 0.76). Laparoscopic repair was associated with reduced rate of acute pain compared to open repair (mean difference 1.19, CI − 1.86, − 0.51, p ≤ 0.0006) and reduced odds of chronic pain compared to open (OR 0.41, CI 0.30–0.56, p ≤ 0.00001). The included trials were, however, of variable methodological quality. Trial sequential analysis reported that further studies are unlikely to demonstrate a statistically significant difference between the two techniques.
Conclusion
This meta-analysis and trial sequential analysis report no difference in recurrence rates between laparoscopic and open primary unilateral inguinal hernia repairs. Rates of acute and chronic pain are significantly less in the laparoscopic group.










Similar content being viewed by others
References
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362(9395):1561–1571
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–65
Simons MP, Aufenacker TJ, Berrevoet F, Bingener J, Bisgaard T, Bittner R, Bonjer HJ, Bury K, Campanelli G, Chen DC, Chowbey PK (2017) World guidelines for groin hernia management. http://news.europeanherniasociety.eu/sites/www.europeanherniasociety.eu/files/medias/PDF/HerniaSurgeGuidelinesPART1TREATMENT.pdf. Accessed 1 Apr 2019
Nordin P, Bartelmess P, Jansson C, Svensson C, Edlund G (2002) Randomized trial of Lichtenstein versus Shouldice hernia repair in general surgical practice. Br J Surg 89(1):45–49
Lange JFM, Kaufmann R, Wijsmuller AR, Pierie JPEN, Ploeg RJ, Chen DC, Amid PK (2015) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19(1):33–43
O’reilly EA, Burke JP, O’connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255(5):846–853
Bobo Z, Nan W, Qin Q, Tao W, Jianguo L, Xianli H (2014) Meta-analysis of randomized controlled trials comparing Lichtenstein and totally extraperitoneal laparoscopic hernioplasty in treatment of inguinal hernias. J Surg Res 192(2):409–420
Scheuermann U, Niebisch S, Lyros O, Jansen-Winkeln B, Gockel I (2017) Transabdominal Preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair: a systematic review and meta-analysis of randomized controlled trials. BMC Surg 17(1):55
Patterson TJ, Beck J, Currie PJ, Spence RA, Spence G (2019) Meta-analysis of patient-reported outcomes after laparoscopic versus open inguinal hernia repair. Br J Surg. https://doi.org/10.1002/bjs.11139
Köckerling F, Stechemesser B, Hukauf M, Kuthe A, Schug-Pass C (2016) TEP versus Lichtenstein: which technique is better for the repair of primary unilateral inguinal hernias in men? Surg Endosc 30(8):3304–3313
University of York, Centre for Reviews and Dissemination. PROSPERO; International prospective register of systematic reviews. http://www.crd.york.ac.uk/PROSPERO. Accessed 1 Apr 2019
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Robinson KA, Dickersin K (2002) Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol 31(1):150–153
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA (2015) A classification of chronic pain for ICD-11. Pain 156(6):1003
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, Di Miceli D, Doglietto GB (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239. https://doi.org/10.1007/s10029-011-0798-9
Higgins JPT, Deeks JJ (2011) Obtaining standard deviations from standard errors, confidence intervals, t values and p values for differences in means. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. https://handbook-5-1.cochrane.org/. Accessed 1 Apr 2019
DeMets D, Lan KK (1994) Interim analysis: the alpha spending function approach. Stat Med 12:1341–1352
O’Brien PC, Fleming TR (1979) A multiple testing procedure for clinical trials. Biometrics 35:549–556
Higgins JP, Altman DG (2009) Assessing risk of bias in included studies. In: Higgins JP, Green S (eds) Cochrane handbook for systematic reviews of interventions. Wiley, West Sussex, pp 187–235
Sevi̇nç B, Damburaci N, Güner M, Karahan Ö (2019) Comparison of early and long term outcomes of open Lichtenstein repair and totally extraperitoneal herniorrhaphy for primary inguinal hernias. Turk J Med Sci 49(1):38–41
Koju R, Koju RB, Malla B, Dongol Y, Thapa LB (2017) Transabdominal pre-peritoneal mesh repair versus Lichtenstein’ s hernioplasty. J Nepal Health Res Counc 15(2):135–140
Westin L, Wollert S, Ljungdahl M, Sandblom G, Gunnarsson U, Dahlstrand U (2016) Less pain 1 year after total extra-peritoneal repair compared with Lichtenstein using local anesthesia: data from a randomized controlled clinical trial. Ann Surg 263(2):240–243
Dahlstrand U, Sandblom G, Ljungdahl M, Wollert S, Gunnarsson U (2013) TEP under general anesthesia is superior to Lichtenstein under local anesthesia in terms of pain 6 weeks after surgery: results from a randomized clinical trial. Surg Endosc 27(10):3632–3638
Wang WJ, Chen JZ, Fang Q, Li JF, Jin PF, Li ZT (2013) Comparison of the effects of laparoscopic hernia repair and Lichtenstein tension-free hernia repair. J Laparoendosc Adv Surg Tech 23(4):301–305
Eker HH, Langeveld HR, Klitsie PJ, van’t Riet M, Stassen LP, Weidema WF, Steyerberg EW, Lange JF, Bonjer HJ, Jeekel J (2012) Randomized clinical trial of total extraperitoneal inguinal hernioplasty vs Lichtenstein repair: a long-term follow-up study. Arch Surg 147(3):256–260
Langeveld HR, van’t Riet M, Weidema WF, Stassen LP, Steyerberg EW, Lange J, Bonjer HJ, Jeekel J (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251(5):819–824
Eklund A, Montgomery A, Bergkvist L, Rudberg C (2010) Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg 97(4):600–608
Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LÅ, Rudberg CR (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg 249(1):33–38
Eklund A, Rudberg C, Smedberg S, Enander LK, Leijonmarck CE, Österberg J, Montgomery A (2006) Short-term results of a randomized clinical trial comparing Lichtenstein open repair with totally extraperitoneal laparoscopic inguinal hernia repair. Br J Surg: Inc Eur J Surg Swiss Surg 93(9):1060–1068
Pokorny H, Klingler A, Schmid T, Fortelny R, Hollinsky C, Kawji R, Steiner E, Pernthaler H, Függer R, Scheyer M (2008) Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia 12(4):385–389
Butters M, Redecke J, Köninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg: Inc Eur J Surg Swiss Surg 94(5):562–565
Köninger J, Redecke J, Butters M (2004) Chronic pain after hernia repair: a randomized trial comparing Shouldice, Lichtenstein and TAPP. Langenbeck’s Arch Surg 389(5):361–365
Lau H, Patil NG, Yuen WK (2006) Day-case endoscopic totally extraperitoneal inguinal hernioplasty versus open Lichtenstein hernioplasty for unilateral primary inguinal hernia in males. Surg Endosc Other Interv Tech 20(1):76–81
Heikkinen T, Bringman S, Ohtonen P, Kunelius P, Haukipuro K, Hulkko A (2004) Five-year outcome of laparoscopic and Lichtenstein hernioplasties. Surg Endosc Other Interv Tech 18(3):518–522
Heikkinen TJ, Haukipuro K, Hulkko A (1998) A cost and outcome comparison between laparoscopic and Lichtenstein hernia operations in a day-case unit. Surg Endosc 12(10):1199–1203
Heikkinen TJ, Haukipuro K, Koivukangas P, Hulkko A (1998) A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus Lichtenstein hernia operation among employed patients. Surg Laparosc Endosc 8(5):338–344
Heikkinen T, Haukipuro K, Leppälä J, Hulkko A (1997) Total costs of laparoscopic and Lichtenstein inguinal hernia repairs: a randomized prospective study. Surg Laparosc Endosc 7(1):1–5
Anadol ZA, Ersoy E, Taneri F, Tekin E (2004) Outcome and cost comparison of laparoscopic transabdominal preperitoneal hernia repair versus open Lichtenstein technique. J Laparoendosc Adv Surg Tech 14(3):159–163
Gokalp A, Inal M, Maralcan G, Baskonus I (2003) A prospective randomized study of Lichtenstein open tension-free versus laparoscopic totally extraperitoneal techniques for inguinal hernia repair. Acta Chir Belg 103(5):502–506
http://www.rcseng.ac.uk/commisioning/groin-hernia-commissioning-guide. Accessed 1 May 2019
https://www.precis-2.org/. Accessed 1 May 2019
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350(18):1819–1827
Blencowe NS, Skilton A, Gaunt D, Brierley R, Hollowood A, Dwerryhouse S, Higgs S, Robb W, Boddy A, Hanna G, Barham CP (2019) Protocol for developing quality assurance measures to use in surgical trials: an example from the ROMIO study. BMJ Open 9(3):e026209
Daes J, Felix E (2017) Critical view of the myopectineal orifice. Ann Surg 266(1):e1–e2
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD, De Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Bhangu A, Singh P, Pinkney T, Blazeby JM (2015) A detailed analysis of outcome reporting from randomised controlled trials and meta-analyses of inguinal hernia repair. Hernia 19(1):65–75
Gohel MS, Chetter I. Are clinical trials units essential for a successful trial?. Bmj. 2015 May 27;350:h2823
Funding
There were no sources of funding associated with this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
NLB, LHM, SAA, NJS and RHF declare no conflict of interest.
Ethical approval
Approval from the institutional review board was not required for this study.
Human and animal rights
This article is a systematic review and meta-analysis and it contains data collected through literature review. It does not include research directly involving human or animal participation.
Informed consent
For this literature review, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The article is part of the Topical Collection “Forum on primary monolateral uncomplicated inguinal hernia”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bullen, N.L., Massey, L.H., Antoniou, S.A. et al. Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23, 461–472 (2019). https://doi.org/10.1007/s10029-019-01989-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01989-7