Abstract
Purpose
Recent advances have led to greater recognition of the role of mitochondrial dysfunction in the pathogenesis of chronic kidney disease (CKD). There has been evidence that CKD is also associated with dysbiosis. Here, we aimed to evaluate whether probiotic supplements can have protective effects against kidney injury via improving mitochondrial function.
Methods
An animal model of CKD was induced by feeding C57BL/6 mice a diet containing 0.2% adenine. KBL409, a strain of Lactobacillus acidophilus, was administered via oral gavage at a dose of 1 × 109 CFU daily. To clarify the underlying mechanisms by which probiotics exert protective effects on mitochondria in CKD, primary mouse tubular epithelial cells stimulated with TGF-β and p-cresyl sulfate were administered with butyrate.
Results
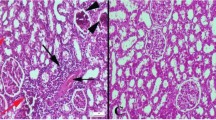
In CKD mice, PGC-1α and AMPK, key mitochondrial energy metabolism regulators, were down-regulated. In addition, mitochondrial dynamics shifted toward fission, the number of fragmented cristae increased, and mitochondrial mass decreased. These alterations were restored by KBL409 administration. KBL409 supplementation also improved defects in fatty acid oxidation and glycolysis and restored the suppressed enzyme levels involved in TCA cycle. Accordingly, there was a concomitant improvement in mitochondrial respiration and ATP production assessed by mitochondrial function assay. These favorable effects of KBL409 on mitochondria ultimately decreased kidney fibrosis in CKD mice. In vitro analyses with butyrate recapitulated the findings of animal study.
Conclusions
This study demonstrates that administration of the probiotic Lactobacillus acidophilus KBL409 protects against kidney injury via improving mitochondrial function.








Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wang Z, Ying Z, Bosy-Westphal A, Zhang J, Schautz B, Later W, Heymsfield SB, Muller MJ (2010) Specific metabolic rates of major organs and tissues across adulthood: evaluation by mechanistic model of resting energy expenditure. Am J Clin Nutr 92(6):1369–1377. https://doi.org/10.3945/ajcn.2010.29885
Che R, Yuan Y, Huang S, Zhang A (2014) Mitochondrial dysfunction in the pathophysiology of renal diseases. Am J Physiol Renal Physiol 306(4):F367-378. https://doi.org/10.1152/ajprenal.00571.2013
Galvan DL, Green NH, Danesh FR (2017) The hallmarks of mitochondrial dysfunction in chronic kidney disease. Kidney Int 92(5):1051–1057. https://doi.org/10.1016/j.kint.2017.05.034
Coughlan MT, Nguyen TV, Penfold SA, Higgins GC, Thallas-Bonke V, Tan SM, Van Bergen NJ, Sourris KC, Harcourt BE, Thorburn DR, Trounce IA, Cooper ME, Forbes JM (2016) Mapping time-course mitochondrial adaptations in the kidney in experimental diabetes. Clin Sci (Lond) 130(9):711–720. https://doi.org/10.1042/cs20150838
Zhan M, Brooks C, Liu FY, Sun L, Dong Z (2013) Mitochondrial dynamics: regulatory mechanisms and emerging role in renal pathophysiology. Kidney Int 83(4):568–581. https://doi.org/10.1038/ki.2012.441
Tang C, Cai J, Dong Z (2016) Mitochondrial dysfunction in obesity-related kidney disease: a novel therapeutic target. Kidney Int 90(5):930–933. https://doi.org/10.1016/j.kint.2016.07.045
Szeto HH (2017) Pharmacologic approaches to improve mitochondrial function in AKI and CKD. J Am Soc Nephrol 28(10):2856–2865. https://doi.org/10.1681/ASN.2017030247
Forbes JM, Thorburn DR (2018) Mitochondrial dysfunction in diabetic kidney disease. Nat Rev Nephrol 14(5):291–312. https://doi.org/10.1038/nrneph.2018.9
Bhatia D, Capili A, Choi ME (2020) Mitochondrial dysfunction in kidney injury, inflammation, and disease: potential therapeutic approaches. Kidney Res Clin Pract 39(3):244–258. https://doi.org/10.23876/j.krcp.20.082
Dare AJ, Bolton EA, Pettigrew GJ, Bradley JA, Saeb-Parsy K, Murphy MP (2015) Protection against renal ischemia-reperfusion injury in vivo by the mitochondria targeted antioxidant MitoQ. Redox Biol 5:163–168. https://doi.org/10.1016/j.redox.2015.04.008
Park CW, Zhang Y, Zhang X, Wu J, Chen L, Cha DR, Su D, Hwang MT, Fan X, Davis L, Striker G, Zheng F, Breyer M, Guan Y (2006) PPARalpha agonist fenofibrate improves diabetic nephropathy in db/db mice. Kidney Int 69(9):1511–1517. https://doi.org/10.1038/sj.ki.5000209
Yang HC, Deleuze S, Zuo Y, Potthoff SA, Ma LJ, Fogo AB (2009) The PPARgamma agonist pioglitazone ameliorates aging-related progressive renal injury. J Am Soc Nephrol 20(11):2380–2388. https://doi.org/10.1681/ASN.2008111138
Ayanga BA, Badal SS, Wang Y, Galvan DL, Chang BH, Schumacker PT, Danesh FR (2016) Dynamin-related protein 1 deficiency improves mitochondrial fitness and protects against progression of diabetic nephropathy. J Am Soc Nephrol 27(9):2733–2747. https://doi.org/10.1681/ASN.2015101096
Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar Reddy D (2015) Role of the normal gut microbiota. World J Gastroenterol 21(29):8787–8803. https://doi.org/10.3748/wjg.v21.i29.8787
Koppe L, Mafra D, Fouque D (2015) Probiotics and chronic kidney disease. Kidney Int 88(5):958–966. https://doi.org/10.1038/ki.2015.255
Lau WL, Savoj J, Nakata MB, Vaziri ND (2018) Altered microbiome in chronic kidney disease: systemic effects of gut-derived uremic toxins. Clin Sci (Lond) 132(5):509–522. https://doi.org/10.1042/CS20171107
Andrade-Oliveira V, Amano MT, Correa-Costa M, Castoldi A, Felizardo RJ, de Almeida DC, Bassi EJ, Moraes-Vieira PM, Hiyane MI, Rodas AC, Peron JP, Aguiar CF, Reis MA, Ribeiro WR, Valduga CJ, Curi R, Vinolo MA, Ferreira CM, Câmara NO (2015) Gut bacteria products prevent AKI induced by ischemia-reperfusion. J Am Soc Nephrol 26(8):1877–1888. https://doi.org/10.1681/asn.2014030288
Yang J, Lim SY, Ko YS, Lee HY, Oh SW, Kim MG, Cho WY, Jo SK (2019) Intestinal barrier disruption and dysregulated mucosal immunity contribute to kidney fibrosis in chronic kidney disease. Nephrol Dial Transplant 34(3):419–428. https://doi.org/10.1093/ndt/gfy172
Iwashita Y, Ohya M, Yashiro M, Sonou T, Kawakami K, Nakashima Y, Yano T, Iwashita Y, Mima T, Negi S, Kubo K, Tomoda K, Odamaki T, Shigematsu T (2018) Dietary changes involving bifidobacterium longum and other nutrients delays chronic kidney disease progression. Am J Nephrol 47(5):325–332. https://doi.org/10.1159/000488947
Yoshifuji A, Wakino S, Irie J, Tajima T, Hasegawa K, Kanda T, Tokuyama H, Hayashi K, Itoh H (2016) Gut Lactobacillus protects against the progression of renal damage by modulating the gut environment in rats. Nephrol Dial Transplant 31(3):401–412. https://doi.org/10.1093/ndt/gfv353
Wei M, Wang Z, Liu H, Jiang H, Wang M, Liang S, Shi K, Feng J (2014) Probiotic Bifidobacterium animalis subsp. lactis Bi-07 alleviates bacterial translocation and ameliorates microinflammation in experimental uraemia. Nephrology (Carlton) 19(8):500–506. https://doi.org/10.1111/nep.12272
Xia B, Yu J, He T, Liu X, Su J, Wang M, Wang J, Zhu Y (2020) Lactobacillus johnsonii L531 ameliorates enteritis via elimination of damaged mitochondria and suppression of SQSTM1-dependent mitophagy in a Salmonella infantis model of piglet diarrhea. Faseb j 34(2):2821–2839. https://doi.org/10.1096/fj.201901445RRR
Tunapong W, Apaijai N, Yasom S, Tanajak P, Wanchai K, Chunchai T, Kerdphoo S, Eaimworawuthikul S, Thiennimitr P, Pongchaidecha A, Lungkaphin A, Pratchayasakul W, Chattipakorn SC, Chattipakorn N (2018) Chronic treatment with prebiotics, probiotics and synbiotics attenuated cardiac dysfunction by improving cardiac mitochondrial dysfunction in male obese insulin-resistant rats. Eur J Nutr 57(6):2091–2104. https://doi.org/10.1007/s00394-017-1482-3
d’Ettorre G, Rossi G, Scagnolari C, Andreotti M, Giustini N, Serafino S, Schietroma I, Scheri GC, Fard SN, Trinchieri V, Mastromarino P, Selvaggi C, Scarpona S, Fanello G, Fiocca F, Ceccarelli G, Antonelli G, Brenchley JM, Vullo V (2017) Probiotic supplementation promotes a reduction in T-cell activation, an increase in Th17 frequencies, and a recovery of intestinal epithelium integrity and mitochondrial morphology in ART-treated HIV-1-positive patients. Immun Inflamm Dis 5(3):244–260. https://doi.org/10.1002/iid3.160
Ren T, Zhu L, Shen Y, Mou Q, Lin T, Feng H (2019) Protection of hepatocyte mitochondrial function by blueberry juice and probiotics via SIRT1 regulation in non-alcoholic fatty liver disease. Food Funct 10(3):1540–1551. https://doi.org/10.1039/c8fo02298d
Kim WK, Han DH, Jang YJ, Park S, Jang SJ, Lee G, Han HS, Ko G (2021) Alleviation of DSS-induced colitis via Lactobacillus acidophilus treatment in mice. Food Funct 12(1):340–350. https://doi.org/10.1039/d0fo01724h
Kim H, Nam BY, Park J, Song S, Kim WK, Lee K, Nam TW, Park JT, Yoo TH, Kang SW, Ko G, Han SH (2022) Lactobacillus acidophilus KBL409 reduces kidney fibrosis via immune modulatory effects in mice with chronic kidney disease. Mol Nutr Food Res:e2101105. https://doi.org/10.1002/mnfr.202101105
Murase M, Kimura Y, Nagata Y (1995) Determination of portal short-chain fatty acids in rats fed various dietary fibers by capillary gas chromatography. J Chromatogr B Biomed Appl 664(2):415–420. https://doi.org/10.1016/0378-4347(94)00491-m
Li YJ, Chen X, Kwan TK, Loh YW, Singer J, Liu Y, Ma J, Tan J, Macia L, Mackay CR, Chadban SJ, Wu H (2020) Dietary fiber protects against diabetic nephropathy through short-chain fatty acid-mediated activation of G protein-coupled receptors GPR43 and GPR109A. J Am Soc Nephrol 31(6):1267–1281. https://doi.org/10.1681/ASN.2019101029
Huang W, Guo HL, Deng X, Zhu TT, Xiong JF, Xu YH, Xu Y (2017) Short-chain fatty acids inhibit oxidative stress and inflammation in mesangial cells induced by high glucose and lipopolysaccharide. Exp Clin Endocrinol Diabetes 125(2):98–105. https://doi.org/10.1055/s-0042-121493
Matsumoto N, Riley S, Fraser D, Al-Assaf S, Ishimura E, Wolever T, Phillips GO, Phillips AO (2006) Butyrate modulates TGF-beta1 generation and function: potential renal benefit for Acacia(sen) SUPERGUM (gum arabic)? Kidney Int 69(2):257–265. https://doi.org/10.1038/sj.ki.5000028
Mollica MP, Mattace Raso G, Cavaliere G, Trinchese G, De Filippo C, Aceto S, Prisco M, Pirozzi C, Di Guida F, Lama A, Crispino M, Tronino D, Di Vaio P, Berni Canani R, Calignano A, Meli R (2017) Butyrate regulates liver mitochondrial function, efficiency, and dynamics in insulin-resistant obese mice. Diabetes 66(5):1405–1418. https://doi.org/10.2337/db16-0924
Gao Z, Yin J, Zhang J, Ward RE, Martin RJ, Lefevre M, Cefalu WT, Ye J (2009) Butyrate improves insulin sensitivity and increases energy expenditure in mice. Diabetes 58(7):1509–1517. https://doi.org/10.2337/db08-1637
Hu J, Kyrou I, Tan BK, Dimitriadis GK, Ramanjaneya M, Tripathi G, Patel V, James S, Kawan M, Chen J, Randeva HS (2016) Short-chain fatty acid acetate stimulates adipogenesis and mitochondrial biogenesis via GPR43 in brown adipocytes. Endocrinology 157(5):1881–1894. https://doi.org/10.1210/en.2015-1944
Hu S, Kuwabara R, de Haan BJ, Smink AM, de Vos P (2020) Acetate and butyrate improve β-cell metabolism and mitochondrial respiration under oxidative stress. Int J Mol Sci. https://doi.org/10.3390/ijms21041542
Vaziri ND, Wong J, Pahl M, Piceno YM, Yuan J, DeSantis TZ, Ni Z, Nguyen TH, Andersen GL (2013) Chronic kidney disease alters intestinal microbial flora. Kidney Int 83(2):308–315. https://doi.org/10.1038/ki.2012.345
Diwan V, Brown L, Gobe GC (2018) Adenine-induced chronic kidney disease in rats. Nephrology (Carlton) 23(1):5–11. https://doi.org/10.1111/nep.13180
Charan J, Kantharia ND (2013) How to calculate sample size in animal studies? J Pharmacol Pharmacother 4(4):303–306. https://doi.org/10.4103/0976-500X.119726
Oh HJ, Nam BY, Wu M, Kim S, Park J, Kang S, Park JT, Yoo TH, Kang SW, Han SH (2018) Klotho plays a protective role against glomerular hypertrophy in a cell cycle-dependent manner in diabetic nephropathy. Am J Physiol Renal Physiol 315(4):F791–F805. https://doi.org/10.1152/ajprenal.00462.2017
Nangaku M, Pippin J, Couser WG (1999) Complement membrane attack complex (C5b–9) mediates interstitial disease in experimental nephrotic syndrome. J Am Soc Nephrol 10(11):2323–2331. https://doi.org/10.1681/ASN.V10112323
Vaziri ND, Yuan J, Rahimi A, Ni Z, Said H, Subramanian VS (2012) Disintegration of colonic epithelial tight junction in uremia: a likely cause of CKD-associated inflammation. Nephrol Dial Transpl 27(7):2686–2693. https://doi.org/10.1093/ndt/gfr624
Andersen K, Kesper MS, Marschner JA, Konrad L, Ryu M, Kumar Vr S, Kulkarni OP, Mulay SR, Romoli S, Demleitner J, Schiller P, Dietrich A, Muller S, Gross O, Ruscheweyh HJ, Huson DH, Stecher B, Anders HJ (2017) Intestinal dysbiosis, barrier dysfunction, and bacterial translocation account for CKD-related systemic inflammation. J Am Soc Nephrol 28(1):76–83. https://doi.org/10.1681/ASN.2015111285
Miranda Alatriste PV, Urbina Arronte R, Gomez Espinosa CO, Espinosa Cuevas Mde L (2014) Effect of probiotics on human blood urea levels in patients with chronic renal failure. Nutr Hosp 29(3):582–590. https://doi.org/10.3305/nh.2014.29.3.7179
Natarajan R, Pechenyak B, Vyas U, Ranganathan P, Weinberg A, Liang P, Mallappallil MC, Norin AJ, Friedman EA, Saggi SJ (2014) Randomized controlled trial of strain-specific probiotic formulation (Renadyl) in dialysis patients. Biomed Res Int 2014:568571. https://doi.org/10.1155/2014/568571
Rossi M, Johnson DW, Morrison M, Pascoe EM, Coombes JS, Forbes JM, Szeto CC, McWhinney BC, Ungerer JP, Campbell KL (2016) Synbiotics easing renal failure by improving gut microbiology (SYNERGY): a randomized trial. Clin J Am Soc Nephrol 11(2):223–231. https://doi.org/10.2215/CJN.05240515
Borges NA, Carmo FL, Stockler-Pinto MB, de Brito JS, Dolenga CJ, Ferreira DC, Nakao LS, Rosado A, Fouque D, Mafra D (2018) Probiotic supplementation in chronic kidney disease: a double-blind, randomized, placebo-controlled. Trial J Ren Nutr 28(1):28–36. https://doi.org/10.1053/j.jrn.2017.06.010
Eidi F, Poor-Reza Gholi F, Ostadrahimi A, Dalili N, Samadian F, Barzegari A (2018) Effect of Lactobacillus Rhamnosus on serum uremic toxins (phenol and P-Cresol) in hemodialysis patients: a double blind randomized clinical trial. Clin Nutr ESPEN 28:158–164. https://doi.org/10.1016/j.clnesp.2018.08.010
Borges NA, Stenvinkel P, Bergman P, Qureshi AR, Lindholm B, Moraes C, Stockler-Pinto MB, Mafra D (2019) Effects of probiotic supplementation on trimethylamine-N-oxide plasma levels in hemodialysis patients: a pilot study. Probiotics Antimicrob Proteins 11(2):648–654. https://doi.org/10.1007/s12602-018-9411-1
Lopes R, Theodoro JMV, da Silva BP, Queiroz VAV, de Castro Moreira ME, Mantovani HC, Hermsdorff HH, Martino HSD (2019) Synbiotic meal decreases uremic toxins in hemodialysis individuals: a placebo-controlled trial. Food Res Int 116:241–248. https://doi.org/10.1016/j.foodres.2018.08.024
Fontecha-Barriuso M, Martin-Sanchez D, Martinez-Moreno JM, Monsalve M, Ramos AM, Sanchez-Nino MD, Ruiz-Ortega M, Ortiz A, Sanz AB (2020) The role of PGC-1alpha and mitochondrial biogenesis in kidney diseases. Biomolecules 10(2):347. https://doi.org/10.3390/biom10020347
Hong Q, Zhang L, Das B, Li Z, Liu B, Cai G, Chen X, Chuang PY, He JC, Lee K (2018) Increased podocyte Sirtuin-1 function attenuates diabetic kidney injury. Kidney Int 93(6):1330–1343. https://doi.org/10.1016/j.kint.2017.12.008
Zhang T, Chi Y, Kang Y, Lu H, Niu H, Liu W, Li Y (2019) Resveratrol ameliorates podocyte damage in diabetic mice via SIRT1/PGC-1α mediated attenuation of mitochondrial oxidative stress. J Cell Physiol 234(4):5033–5043. https://doi.org/10.1002/jcp.27306
Kim MY, Lim JH, Youn HH, Hong YA, Yang KS, Park HS, Chung S, Ko SH, Shin SJ, Choi BS, Kim HW, Kim YS, Lee JH, Chang YS, Park CW (2013) Resveratrol prevents renal lipotoxicity and inhibits mesangial cell glucotoxicity in a manner dependent on the AMPK-SIRT1-PGC1alpha axis in db/db mice. Diabetologia 56(1):204–217. https://doi.org/10.1007/s00125-012-2747-2
Kang HM, Ahn SH, Choi P, Ko YA, Han SH, Chinga F, Park AS, Tao J, Sharma K, Pullman J, Bottinger EP, Goldberg IJ, Susztak K (2015) Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development. Nat Med 21(1):37–46. https://doi.org/10.1038/nm.3762
Han SH, Wu MY, Nam BY, Park JT, Yoo TH, Kang SW, Park J, Chinga F, Li SY, Susztak K (2017) PGC-1alpha protects from notch-induced kidney fibrosis development. J Am Soc Nephrol 28(11):3312–3322. https://doi.org/10.1681/ASN.2017020130
Nam BY, Jhee JH, Park J, Kim S, Kim G, Park JT, Yoo TH, Kang SW, Yu JW, Han SH (2022) PGC-1alpha inhibits the NLRP3 inflammasome via preserving mitochondrial viability to protect kidney fibrosis. Cell Death Dis 13(1):31. https://doi.org/10.1038/s41419-021-04480-3
Chung KW, Lee EK, Lee MK, Oh GT, Yu BP, Chung HY (2018) Impairment of PPARalpha and the fatty acid oxidation pathway aggravates renal fibrosis during aging. J Am Soc Nephrol 29(4):1223–1237. https://doi.org/10.1681/ASN.2017070802
Brooks C, Cho SG, Wang CY, Yang T, Dong Z (2011) Fragmented mitochondria are sensitized to Bax insertion and activation during apoptosis. Am J Physiol Cell Physiol 300(3):C447-455. https://doi.org/10.1152/ajpcell.00402.2010
Zhan M, Usman IM, Sun L, Kanwar YS (2015) Disruption of renal tubular mitochondrial quality control by Myo-inositol oxygenase in diabetic kidney disease. J Am Soc Nephrol 26(6):1304–1321. https://doi.org/10.1681/asn.2014050457
Wong J, Piceno YM, DeSantis TZ, Pahl M, Andersen GL, Vaziri ND (2014) Expansion of urease- and uricase-containing, indole- and p-cresol-forming and contraction of short-chain fatty acid-producing intestinal microbiota in ESRD. Am J Nephrol 39(3):230–237. https://doi.org/10.1159/000360010
Wang JJ, Zhang QM, Ni WW, Zhang X, Li Y, Li AL, Du P, Li C, Yu SS (2019) Modulatory effect of Lactobacillus acidophilus KLDS 1.0738 on intestinal short-chain fatty acids metabolism and GPR41/43 expression in beta-lactoglobulin-sensitized mice. Microbiol Immunol 63(8):303–315. https://doi.org/10.1111/1348-0421.12723
Li Z, Wang W, Liu D, Guo Y (2017) Effects of Lactobacillus acidophilus on gut microbiota composition in broilers challenged with Clostridium perfringens. PLoS ONE 12(11):e0188634. https://doi.org/10.1371/journal.pone.0188634
Sivieri K, Morales ML, Adorno MA, Sakamoto IK, Saad SM, Rossi EA (2013) Lactobacillus acidophilus CRL 1014 improved “gut health” in the SHIME reactor. BMC Gastroenterol 13:100. https://doi.org/10.1186/1471-230X-13-100
Berni Canani R, Sangwan N, Stefka AT, Nocerino R, Paparo L, Aitoro R, Calignano A, Khan AA, Gilbert JA, Nagler CR (2016) Lactobacillus rhamnosus GG-supplemented formula expands butyrate-producing bacterial strains in food allergic infants. ISME J 10(3):742–750. https://doi.org/10.1038/ismej.2015.151
Duncan SH, Louis P, Flint HJ (2004) Lactate-utilizing bacteria, isolated from human feces, that produce butyrate as a major fermentation product. Appl Environ Microbiol 70(10):5810–5817. https://doi.org/10.1128/AEM.70.10.5810-5817.2004
Bourriaud C, Robins RJ, Martin L, Kozlowski F, Tenailleau E, Cherbut C, Michel C (2005) Lactate is mainly fermented to butyrate by human intestinal microfloras but inter-individual variation is evident. J Appl Microbiol 99(1):201–212. https://doi.org/10.1111/j.1365-2672.2005.02605.x
Wang MX, Lin L, Chen YD, Zhong YP, Lin YX, Li P, Tian X, Han B, Xie ZY, Liao QF (2020) Evodiamine has therapeutic efficacy in ulcerative colitis by increasing Lactobacillus acidophilus levels and acetate production. Pharmacol Res 159:104978. https://doi.org/10.1016/j.phrs.2020.104978
Duncan SH, Barcenilla A, Stewart CS, Pryde SE, Flint HJ (2002) Acetate utilization and butyryl coenzyme A (CoA):acetate-CoA transferase in butyrate-producing bacteria from the human large intestine. Appl Environ Microbiol 68(10):5186–5190. https://doi.org/10.1128/AEM.68.10.5186-5190.2002
Kumar A, Alrefai WA, Borthakur A, Dudeja PK (2015) Lactobacillus acidophilus counteracts enteropathogenic E. coli-induced inhibition of butyrate uptake in intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol 309(7):G602–607. https://doi.org/10.1152/ajpgi.00186.2015
Zhao T, Gu J, Zhang H, Wang Z, Zhang W, Zhao Y, Zheng Y, Zhang W, Zhou H, Zhang G, Sun Q, Zhou E, Liu Z, Xu Y (2020) Sodium butyrate-modulated mitochondrial function in high-insulin induced HepG2 cell dysfunction. Oxid Med Cell Longev 2020:1904609. https://doi.org/10.1155/2020/1904609
Koh A, De Vadder F, Kovatcheva-Datchary P, Backhed F (2016) From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165(6):1332–1345. https://doi.org/10.1016/j.cell.2016.05.041
Lopez-Armada MJ, Riveiro-Naveira RR, Vaamonde-Garcia C, Valcarcel-Ares MN (2013) Mitochondrial dysfunction and the inflammatory response. Mitochondrion 13(2):106–118. https://doi.org/10.1016/j.mito.2013.01.003
Yu JW, Lee MS (2016) Mitochondria and the NLRP3 inflammasome: physiological and pathological relevance. Arch Pharm Res 39(11):1503–1518. https://doi.org/10.1007/s12272-016-0827-4
Funding
This research was supported by a faculty research grant of Yonsei University College of Medicine for 2021, Seoul, Korea (6-2021-0220).
Author information
Authors and Affiliations
Contributions
TN, GK, and SHH designed the study; JP, KHN, BYN, GK, SCS, WK, KUL, and TN carried out experiments; JP, KHN, BYN, SCS, WK, KUL, and TN made figures; JP, KHN, JTP, TY, SK, GK, and SHH analyzed the data; KHN, JP, and SHH drafted the manuscript; SCS, WK, KUL, TN, JTP, TY, SK, GK, and SHH revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
GwangPyo Ko is a founder and board member of KoBioLabs, Inc., a company characterizing the role of host–microbiome interaction in chronic diseases. The other authors declare no competing interests.
Ethical approval
The animal study was reviewed and approved by Institutional Animal Care and Use Committee, Yonsei University (2018-0281).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, J., Nam, K.H., Nam, B.Y. et al. Lactobacillus acidophilus KBL409 protects against kidney injury via improving mitochondrial function with chronic kidney disease. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03408-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03408-9