Abstract
Aims/hypothesis
Many of the effects of resveratrol are consistent with the activation of AMP-activated protein kinase (AMPK), silent information regulator T1 (SIRT1) and peroxisome proliferator-activated receptor (PPAR)γ co-activator 1α (PGC-1α), which play key roles in the regulation of lipid and glucose homeostasis, and in the control of oxidative stress. We investigated whether resveratrol has protective effects on the kidney in type 2 diabetes.
Methods
Four groups of male C57BLKS/J db/m and db/db mice were used in this study. Resveratrol was administered via gavage to diabetic and non-diabetic mice, starting at 8 weeks of age, for 12 weeks.
Results
The db/db mice treated with resveratrol had decreased albuminuria. Resveratrol ameliorated glomerular matrix expansion and inflammation. Resveratrol also lowered the NEFA and triacylglycerol content of the kidney, and this action was related to increases in the phosphorylation of AMPK and the activation of SIRT1–PGC-1α signalling and of the key downstream effectors, the PPARα–oestrogen-related receptor (ERR)-1α–sterol regulatory element-binding protein 1 (SREBP1). Furthermore, resveratrol decreased the activity of phosphatidylinositol-3 kinase (PI3K)–Akt phosphorylation and class O forkhead box (FOXO)3a phosphorylation, which resulted in a decrease in B cell leukaemia/lymphoma 2 (BCL-2)-associated X protein (BAX) and increases in BCL-2, superoxide dismutase (SOD)1 and SOD2 production. Consequently, resveratrol reversed the increase in renal apoptotic cells and oxidative stress, as reflected by renal 8-hydroxy-deoxyguanosine (8-OH-dG), urinary 8-OH-dG and isoprostane concentrations. Resveratrol prevented high-glucose-induced oxidative stress and apoptosis in cultured mesangial cells through the phosphorylation of AMPK and activation of SIRT1–PGC-1α signalling and the downstream effectors, PPARα–ERR-1α–SREBP1.
Conclusions/interpretation
The results suggest that resveratrol prevents diabetic nephropathy in db/db mice by the phosphorylation of AMPK and activation of SIRT1–PGC-1α signalling, which appear to prevent lipotoxicity-related apoptosis and oxidative stress in the kidney.
Similar content being viewed by others
Introduction
Diabetic nephropathy is the most prevalent cause of end-stage renal disease in developed countries, including Korea [1]. Despite progress in pharmacological strategies to modulate diabetes, the number of patients entering renal failure remains extremely high and the development of new classes of therapeutic agents is eagerly anticipated. Lipotoxicity is one of the causal factors of the progression of diabetic and obesity-induced renal damage [2], but the underlying molecular mechanism remains elusive.
Resveratrol is a natural plant polyphenol that may target ageing and obesity-related chronic diseases by preventing inflammation and oxidative stress [3–6]. Resveratrol activates silent information regulator T1 (SIRT1), an NAD+-dependent protein deacetylase, and AMP-activated protein kinase (AMPK). It subsequently augments peroxisome proliferator-activated receptor (PPAR)γ co-activator 1α (PGC-1α), endothelial nitric oxide synthase (eNOS) and class O forkhead box (FOXO) activation, which is followed by catabolic metabolism, mitochondrial activation, angiogenesis and enhanced cell survival [3–6]. Some of the best-characterised effects of SIRT1 include increased stress resistance and altered metabolism mediated by changes in the activity of the transcriptional factor FOXO [3], suppression of nuclear factor κ B (NF-κB)-dependent inflammatory responses [4] and the promotion of gluconeogenesis, fatty acid oxidation and mitochondrial biogenesis, through PGC-1α [5, 6]. The activation of SIRT1 by resveratrol is substrate dependent and many of its effects are consistent with the modulation of its target genes [7, 8]. Hepatocyte-specific deletion of Sirt1 impairs PPARα signalling and decreases fatty acid β-oxidation, whereas the overexpression of Sirt1 induces the expression of PPARα targets. SIRT1 interacts with PPARα, and this is required to activate the PPARα co-activator PGC-1α. It has been reported that SIRT1 and PGC-1α form a stable complex and that SIRT1 regulates the activity and acetylation status of PGC-1α [9]. AMPK is a fuel-sensing enzyme that is activated by decreases in the cellular energy state, as reflected by an increased AMP/ATP ratio [10]. When activated, AMPK initiates metabolic and genetic processes that generate ATP (fatty acid oxidation), and inhibits other processes that consume ATP. The former occurs via its effects on various transcriptional activators and co-activators, including PGC-1α and PPARα [11]. The collective results favour the view that SIRT1 and AMPK play a vital role in the regulation of organic lipid homeostasis, and that pharmacological activation of SIRT1 and AMPK may be important for the prevention of obesity-associated metabolic diseases [8, 10, 11].
Accumulated experimental evidence suggests that PPARα activation attenuates or inhibits several mediators of vascular injury, including lipotoxicty, inflammation, reactive oxygen species (ROS) generation, endothelial dysfunction, angiogenesis and thrombosis in type 2 diabetes and high-fat-diet-induced renal damage [12, 13], which are all associated with AMPK activation and eNOS production [14–16]. PPARs activate PGC-1α/β and its key downstream effector oestrogen-related receptor (ERR)-1α, which induces mitochondrial biogenesis and enhanced mitochondrial antioxidative capacity to provide relief from oxidative stress [17, 18]. Additionally, PPARα activation can suppress the sterol regulatory element-binding protein 1 (SREBP1) pathway through the reduction of liver X receptor (LXR)/retinoid X receptor (RXR) formation in the liver, which plays a crucial role in the regulation of fatty acid metabolism [19]. Notably, FOXO3a is a direct transcriptional regulator of a group of oxidative protection genes and this regulation requires PGC-1α. FOXO3A and PGC-1α interact directly and cooperatively and their interaction regulates mitochondrial oxidative stress [20].
We hypothesised that resveratrol can potentially prevent renal cell apoptosis and oxidative stress, which are the main causes of renal damage in diabetic nephropathy, via activation of AMPK–SIRT1–PGC-1α and the consequent effects on its target molecules PPARα–ERR-1α and the phosphatidylinositol-3 kinase (PI3K)–Akt–FOXO3a pathway.
Methods
Experimental methods
Male 6-week-old C57BLKS/J db/m and db/db mice were purchased from Jackson Laboratories (Bar Harbor, ME, USA). Four groups of male C57BLKS/J db/m and db/db mice were used in this study. Resveratrol (Sigma-Aldrich, St Louis, MO, USA) dissolved with 0.5% carboxymethyl cellulose sodium salt (CMC), 20 mg kg−1 day−1, was administered via gavage to diabetic mice (db/db Res, n = 8) and non-diabetic mice (db/m Res, n = 8) starting at 8 weeks of age, for 12 weeks [21]. The diabetic db/db group (n = 8) and the non-diabetic db/m control group (n = 8) received only 0.5% CMC. The mice were placed in individual metabolism cages (Nalgene, Rochester, NY, USA) with access to water and food ad libitum. After 12 weeks of treatment, the systolic BP was determined by the non-invasive tail-cuff system in conscious mice (IITC Life Science, Woodland Hill, CA, USA) after a 5 day accommodation period. At week 20, all animals were anaesthetised by intraperitoneal injection of a mixture of Rompun, 10 mg/kg (Bayer Korea, Ansan, Gyeonggi-Do, Korea) and Zoletil, 30 mg/kg (Virbac, Carros, France). The mice were killed and the kidneys removed. Immediately following removal, each kidney was divided into the cortex and medullar. All our experiments, including western blots, were performed with renal cortex. The kidneys were rapidly dissected and stored in buffered formalin (10%) for subsequent immunohistochemical analyses. Blood was collected from the left ventricle and the plasma was stored at –70°C for subsequent analyses. HbA1c was determined from the red cell lysates by HPLC (Bio-Rad, Richmond, CA, USA). The total cholesterol and triacylglycerol concentrations were measured by an autoanalyser (Hitachi 917, Tokyo, Japan) using commercial kits (Wako, Osaka, Japan). NEFA levels were measured with a JCA-BM1250 automatic analyser (JEOL, Tokyo, Japan). The experiments were performed in accordance with our institutional animal care guidelines, and all the procedures complied with the Guide for the Care and Use of Laboratory Animals (National Institutes of Health Publication No. 85–23, revised 1996).
Assessment of renal function and the lipid contents
At week 20, the animals were housed in metabolism cages (Nalgene) for 24 h to collect urine for subsequent measurements of the albumin concentrations by an immunoassay (Bayer, Elkhart, IN, USA). Plasma and urine creatinine concentrations were measured, using HPLC (Beckman Instruments, Fullerton, CA, USA). The kidney lipids were extracted using the method of Bligh and Dyer with slight modifications, as previously described [22].
Light microscopy study
The mesangial matrix and glomerular tuft areas were quantified for each glomerular cross-section, using sections stained with periodic acid–Schiff's reagent. More than 30 glomeruli, cut through the vascular pole, were counted per kidney and the average was used for analysis.
Immunohistochemistry for TGF-β1, type IV collagen, PPARα, cell surface glycoprotein F4/80, 8-hydroxy-deoxyguanosine and TUNEL assay
We performed immunohistochemistry for type IV collagen, TGF-β1, PPARα, cell surface glycoprotein F4/80 (F4/80), 8-hydroxy-deoxyguanosine (8-OH-dG) and active caspase-3. We also performed a TUNEL assay. See the electronic supplementary material (ESM) Methods for further details.
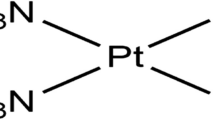
Western blots
The total protein of the renal cortical tissues was extracted with a Pro-Prep Protein Extraction Solution (Intron Biotechnology, Gyeonggi-Do, Korea) according to the manufacturer's instructions. Western blot analysis was performed to further confirm the responses using epitope-specific antibodies. Blots were carried out for SIRT1, PPARα, PGC-1α, ERR-1α, SREBP1, carnitine palmitoyltransferase-1A (CPT-1A), total AMPK, phosphorylated (phospho)-AMPK Thr172, PI3K, total Akt, phospho-Akt Ser473, total FOXO3a, phospho-FOXO3a Ser253, active caspase-3, B cell leukaemia/lymphoma 2 (BCL-2), superoxide dismutase (SOD)1 and SOD2. We also measured PI3K activity. See ESM Methods for further details.
Immunoprecipitation for acetylated PGC-1α assay
Acetylated-lysine PGC-1α was analysed by immunoprecipitation of PGC-1α from the renal cortex protein lysates with anti-PGC-1α (Santa Cruz Biotechnology, Santa Cruz, CA, USA) followed by western blotting using an acetyl-lysine antibody (Cell Signaling, Denvers, MA, USA).
Assessment of renal oxidative stress
To evaluate the oxidative DNA damage and lipid peroxidation, the 24 h urinary 8-OH-dG (OXIS Health Products, Portland, OR, USA) and 24 h urinary 8-epi-prostaglandin F2α (8-epi-PGF2α; OxisResearch, Foster City, CA, USA) concentrations were measured, respectively.
Cell culture
To find the effects of high glucose and resveratrol on NMS2 mesangial cells [23] with regard to the activation of the AMPK–SIRT1–PGC-1α pathway and apoptosis, mesangial cells were grown in 5 mmol/l d-glucose (low glucose), 30 mmol/l d-glucose (high glucose) or 5 mmol/l d-glucose plus 25 mmol/l mannitol (as an osmotic control for 30 mmol/l d-glucose). After reaching 80% confluency, the mesangial cells were exposed to low glucose, high glucose or mannitol control, with or without the additional 48 h application of resveratrol (1, 10 or 50 ng/ml), 5-aminoimidazole-4-carboxamide-1β-d-ribofuranoside (AICAR), 0.5 mmol/l, or metformin (1 mmol/l). The small interfering (si)RNA targeted to Ampkα1 (also known as Prkaa1), Ampkα2 (also known as Prkaa1), Sirt1 and scrambled siRNA (siRNA control) were complexed with transfection reagent (G-Fectin; Genolution, Seoul, Korea), according to the manufacturer's instructions. We also performed a TUNEL assay to evaluate the effects of siRNAs on mesangial cell apoptosis. See ESM Methods for further details.
Statistical analysis
The data are expressed as the means±SD. Differences between the groups were tested for statistical significance by ANOVA with Bonferroni correction, using SPSS version 11.5 (SPSS, Chicago, IL, USA). A p value <0.05 was considered to show a statistically significant difference.
Results
Physical and biochemical characteristics of mice
The diabetic db/db mice were heavier than the non-diabetic db/m mice (Table 1). Kidney weight, blood glucose and HbA1c, together with the amount of food eaten, were significantly higher for the db/db mice than for the db/m mice (Table 1). There were no differences in serum creatinine level and systolic BP between the study groups. There was significantly increased albuminuria and creatinine clearance in the db/db mice compared with the db/m and db/m Res mice. Despite the same degree of hyperglycaemia in the db/db Res and db/db mice, resveratrol treatment restored the albuminuria and creatinine clearance to the levels of the db/m and db/m Res mice (Table 1).
Effects of resveratrol on renal phenotype, TGF-β1, type IV collagen and F4/80
There were no differences in the fractional mesangial areas between the db/m and db/m Res mice (Fig. 1a). In contrast, there was a marked (2.6-fold) increase in the mesangial area in the db/db mice compared with the db/m mice (p < 0.01). Consistent with the changes of the mesangial fractional area, the levels of the pro-fibrotic growth factor TGF-β1 and associated extracellular matrix type IV collagen and inflammatory cell glomerular infiltration were significantly increased in the db/db mice compared with the db/m and db/m Res mice (Fig. 1a–e). All of the diabetes-induced renal phenotypic changes and inflammation seen in the db/db mice were reversed by resveratrol treatment. The significantly increased production of type IV collagen in db/db mice was reversed by resveratrol treatment (ESM Fig. 1 and ESM Results).
Changes in glomerular phenotypes in resveratrol-treated db/db mice. Glomerular mesangial fractional area, pro-fibrotic TGF-β1 and type IV collagen, and F4/80-positive cell infiltration in the cortical glomerulus of db/m and db/db mice, with or without resveratrol treatment. Representative sections stained with periodic acid–Schiff reagent are shown for estimation of the mesangial fractional area (%) (a), together with quantitative analysis by group (b). Immunohistochemical staining and quantitative analyses are shown for TGF-β1 (a, c), type IV collagen (a, d) and F4/80-positive cells (a, e). Col IV, type IV collagen; Cont, control; PAS, periodic acid–Schiff stain. ** p < 0.01 vs the db/m control, db/m Res and db/db Res mice
Renal levels of phospho-AMPK Thr172and total AMPK, SIRT1, total and acetylated-Lys-PGC-1α, PPARα–ERR-1α–PGC-1α signalling, and intra-renal triacylglycerol and NEFA
Western blot analysis showed that diabetes markedly decreased the phospho-AMPK Thr172/total AMPK ratio and the SIRT1 protein levels in db/db mice compared with db/m and db/m Res mice (Fig. 2). Resveratrol treatment restored the phospho-AMPK Thr172/total AMPK, SIRT1 and total and acetylated Lys-PGC-1α levels in db/db mice to the levels of db/m and db/m Res mice (Fig. 2a–e; p < 0.01). Interestingly, the PPARα level was lower in the db/db mice compared with that in the db/m and db/m Res mice, as assessed by immunohistochemical and western blot analyses (Fig. 2f, g). The levels of ERR-1α and SREBP1 in the kidney were evaluated to determine the changes in the PPARα target proteins. There was a decrease in ERR-1α and an increase in SREBP1 levels in db/db mice, both of which were restored with resveratrol treatment (Fig. 2g). Consistent with the PPARα–ERR-1α–SREBP1 changes in the db/db mice, direct measurement of the intra-renal lipid concentrations showed increases in triacylglycerol and NEFA concentrations, but not in the total cholesterol concentration, in this group (Fig. 2 h–j). Intra-renal triacylglycerol and NEFA concentrations were decreased by resveratrol treatment (p < 0.05, Fig. 2i, j).
Phospho-AMPK Thr172, total AMPK, SIRT1, acetylated PGC-1α, total PGC-1α, PPARα, ERR-1α, SREBP1 and intra-renal lipid levels in the renal cortex of the db/m and db/db mice, with or without resveratrol treatment. Protein lysates (40 μg) from renal cortex were separated by SDS-PAGE and analysed by western blotting. Representative western blotting (a) is shown for phospho-AMPK Thr172, total AMPK, SIRT1, PGC-1α, total PGC-1α and β-actin. Quantitative analyses are shown for phospho-AMPK Thr172/total AMPK (b), SIRT1/β-actin (c), PGC-1α/β-actin (d) and acetylated Lys-PGC-1α/β-actin (e). (f) Representative immunohistochemical staining for PPARα and quantitative analysis of the results. (g) Western blot of PPARα and ERR-1α, SREBP1 and β-actin and the corresponding quantitative analyses. (h–j) Quantitative analyses of intra-renal total cholesterol (h), NEFA (i) and triacylglycerol (j) concentrations. ** p < 0.01 vs the db/m control, db/m Res and db/db Res mice; ††† p < 0.001 vs the db/m control and db/m Res mice; and ‡ p < 0.05 vs the db/db Res mice. Cont, control; pAMPK, phospho-AMPK Thr172
Renal levels of PI3K, phospho-Akt Ser473 and pFOXO3a
We determined the levels of intra-renal PI3K and phospho-Akt Ser473 using western blot analysis and PI3K activity by ELISA. The PI3K level and activity, as well as the phospho-Akt Ser473/total Akt ratio were significantly increased in db/db mice compared with db/m and db/m Res mice (Fig. 3a–d, p < 0.01 [PI3K activity and level] and p <0.05 [phospho-Akt Ser473/total Akt ratio]). Resveratrol treatment of db/db mice decreased the PI3K level and phospho-Ser473 Akt /total Akt ratio compared with the levels of the db/db mice. An increased level of phospho-FOXO3a Ser253 was noted in db/db mice compared with db/m and db/m Res mice (Fig. 3e; p < 0.05). Treatment with resveratrol markedly decreased the level of phospho-FOXO3a Ser253 in db/db mice, which resulted in an increase in total FOXO3a, according to the western blot analysis (Fig. 3a, f).
PI3K activity, PI3K, phosphor–Akt Ser472, total Akt, phospho-FOXO3a Ser253 and total FOXO3a in the renal cortex of the db/m and db/db mice with or without resveratrol treatment. Protein lysates (40 μg) from renal cortex were separated by SDS-PAGE and analysed by western blotting. Representative western blot showing PI3K, phospho-Akt Ser472, total Akt, phospho-FOXO3a Ser253, total FOXO3a and β-actin levels (a). (b) PI3K activity. (c–f) Quantitative analyses of the results from the blot: (c) PI3K/β-actin; (d) phospho-Akt Ser472/total Akt; (e) phospho-FOXO3a Ser253/β-actin; and (f) phospho-FOXO3a/total FOXO3a. * p < 0.05 and ** p <0.01 vs db/m control, db/m Res and db/db Res mice. Cont, control; pAkt, phospho-Akt Ser472; pFOXO3a, phospho-FOXO3a Ser253
Renal levels of pro-apoptotic BAX, anti-apoptotic BCL-2, cleaved caspase-3 and TUNEL-positive cells
It is well known that FOXO3a activation has an anti-stress and anti-apoptotic action via the enhancement of BCL-2 activity and the downregulation of pro-apoptotic BCL-2-associated X protein (BAX) activity. Consistent with the changes in FOXO3a, the BAX level on western blot was increased in samples from db/db mice compared with those from db/m and db/m Res mice (Fig. 4a). However, the BCL-2 protein level was decreased in db/db mice compared with the db/m and db/m Res mice (Fig. 4a). Consequently, the BAX/BCL-2 ratio was significantly increased in db/db mice, resulting in an increase in cleaved caspase-3 (Fig. 4a, c, p < 0.01), which is a critical executioner of apoptosis. In contrast, resveratrol treatment in db/db mice resulted in increased BCL-2 protein and decreased BAX protein, which resulted in a threefold increase in the ratio of BAX/BCL-2 (p < 0.01) and, ultimately, a decrease in cleaved caspase-3 (Fig. 4a, c). Furthermore, there was a significant increase in the number of TUNEL-positive cells in the glomeruli of db/db mice compared with db/m and db/m Res mice. The number of TUNEL-positive cells in db/db mice was decreased after resveratrol treatment (Fig. 4d).
Pro-apoptotic BAX, anti-apoptotic BCL-2 and cleaved caspase-3 levels in the renal cortices of db/m and db/db mice with or without resveratrol treatment. Protein lysates (40 μg) from renal cortex were separated by SDS-PAGE and analysed by western blotting. Representative western blot analysis of the BAX, BCL-2, cleaved caspase-3 and β-actin levels (a) and the quantitative analyses of the results of the BAX/BCL-2 ratio (b) and cleaved caspase-3 (c) are shown. Representative immunohistochemical staining for TUNEL-positive cells and the quantitative analyses of the results are shown (d). ** p < 0.01 vs db/m control, db/m Res and db/db Res mice. Cont, control
Effects of resveratrol on SOD1, SOD2, and renal and 24 h urinary 8-OH-dG and isoprostane concentrations
We investigated the changes in SOD1 and SOD2 content associated with FOXO3a activation. SOD1 and SOD2 levels were lower in db/db mice than in db/m and db/m Res mice (Fig. 5a–c). In contrast, SOD1 and SOD2 levels were significantly increased in db/db Res mice compared with db/db mice. Increases in the renal oxidative DNA damage and lipid peroxidation, as reflected by the renal and urinary 8-OH-dG and urinary 8-isoprostane concentrations, respectively, were observed in db/db mice and were compared with the levels in db/m and db/m Res mice (Fig. 5e–f). However, 12 weeks of resveratrol treatment decreased not only the renal 8-OH-dG level and the urinary 8-OH-dG concentration, but also the urinary 8-isoprostane concentration in db/db mice. Taken together, these findings suggest that oxidative stress in the db/db mice could be ameliorated by resveratrol treatment.
Intra-renal SOD1, SOD2 and 8-OH-dG levels, and 24 h urinary 8-OH-dG and isoprostane concentrations in db/m and db/db mice with or without resveratrol treatment. Protein lysates (10 μg) from renal cortex were separated by SDS-PAGE and analysed by western blotting. Representative western blot analysis of the SOD1 and SOD2 (a) and the quantitative analyses of the results are shown: (b) SOD1; and (c) SOD2. Representative immunohistochemical staining for 8-OH-dG and the quantitative analyses of the results are shown (d). The 24 h urinary 8-OH-dG (e) and isoprostane (f) concentrations of the study mice are shown. * p < 0.05 and ** p < 0.01 vs the db/m control, db/m Res and db/db Res mice. Cont, control
In vitro studies
In diabetic db/db mice, mesangial matrix expansion, with an increased number of apoptotic mesangial cells, is one of the characteristic phenotypes of oxidative stress. As resveratrol reversed the diabetes-induced detrimental renal effects in db/db mice, we evaluated the effects of several doses of resveratrol on high-glucose-induced oxidative stress, and the effects of apoptosis related to AMPK–SIRT1–PGC-1α signalling and its downstream effector, the PPARα–ERR-1α–FOXO3a axis, in cultured mesangial cells. High glucose (30 mmol/l d-glucose) induced significant decreases in the activation of phospho-AMPK Thr172–SIRT1–PGC-1α signalling (Fig. 6a) and the levels of PPARα–ERR-1α (Fig. 6b). Consistent with the change in PPARα–ERR-1α, high glucose increased the level of the lipogenic enzyme SREBP1 and decreased the lipolytic enzyme CPT-1A (Fig. 6b). High glucose additionally increased PI3K–Akt phosphorylation and subsequent FOXO3a phosphorylation (Fig. 6b), which related to decreases in SOD1 and SOD2 content, and an increase in the number of apoptotic mesangial cells (Fig. 6c, d). In contrast, resveratrol, 1–50 ng/ml, prevented high-glucose-induced oxidative stress and apoptosis related to the activation of AMPK–SIRT1–PGC-1α signalling and the PPARα–ERR-1α pathway. When compared with high glucose, the addition of resveratrol in low glucose did not affect the intracellular signalling and mesangial cell apoptosis. Mannitol was without any effect on the intracellular signalling (data not shown). To validate the pro-apoptotic effect of resveratrol as AMPK dependent, we performed additional experiments using the AMPK activators AICAR and metformin, and siRNAs for Ampkα1, Ampkα2 and Sirt1 in cultured mesangial cells. Similar to resveratrol, AICAR and metformin also activated AMPK–SIRT1–PGC-1α signalling in high-glucose conditions (Fig. 7a). In contrast, transfection with Ampkα1, Ampkα2 and Sirt1 siRNAs suppressed resveratrol-induced AMPK–SIRT1–PGC-1α signalling, respectively, compared with resveratrol treatment only in high-glucose media (Fig. 7b, c). Moreover, transfection with Ampkα1, Ampkα2, Sirt1 and Pgc-1α (also known as Ppargc1a) siRNAs prevented the resveratrol-induced anti-apoptotic effect in mesangial cells in high-glucose media (Fig. 7d).
The effect of resveratrol on intracellular signalling and apoptosis in the mesangial cells cultured in low glucose (5 mmol/l d-glucose) or high glucose (30 mmol/l d-glucose) with or without resveratrol at different concentrations (1 μg/ml, 10 μg/ml or 50 μg/ml, as shown). Phospho-AMPK Thr172, total AMPK, SIRT1 and total PGC-1α levels were assessed in the cultured mesangial cells. Protein lysates (10 μg) were separated by SDS-PAGE and analysed by western blotting. Representative western blot analysis of the phospho-AMPK Thr172, total AMPK, SIRT1, PGC-1α and β-actin levels and the quantitative analyses of the results are shown (a). (b) Representative western blot analysis of PPARα, ERR-1α, SREBP1, CPT-1A, PI3K, phospho-Akt Ser472, total Akt, phospho-FOXO3a Ser253 and total FOXO3a levels in the cultured mesangial cells, and quantitative analyses of the results. (c) Representative western blot analysis of SOD1 and SOD2 in cultured mesangial cells and the quantitative analyses of the results. (d) Representative pictures of TUNEL-positive mesangial cells (original magnification ×400) and quantitative analyses of the results. n = 4; * p < 0.05 and ** p < 0.01 compared with low glucose. +1/+10/+50, +1/+10/+50 μg/ml resveratrol; HG, high glucose; LG, low glucose; pAkt, phospho-Akt Ser472; pAMPK, phospho-AMPK Thr172; pFOXO3a, phospho-FOXO3a Ser253
Effect of AICAR and metformin, AMPK activators, and Ampkα1, Ampkα2 and Sirt1 siRNA on the resveratrol-stimulated AMPK–SIRT1–PGC-1α signalling in mesangial cells. The cultured mesangial cells in high glucose were stimulated by AICAR and metformin. Protein lysates (10 μg) from the cultured mesangial cells were separated by SDS-PAGE and analysed by western blotting. (a) Representative western blot analysis of phospho-AMPK Thr172, SIRT1, PGC-1α and β-actin levels and the quantitative analyses of the results. * p < 0.05 compared with low glucose, high glucose, high glucose + AICAR and high glucose + metformin. (b) The cultured mesangial cells were transfected with 50 nmol/l control siRNA, or 50 nmol/l Ampkα1, Ampkα2 or Sirt1 siRNA using tranfection reagent (G-Fectin). Approximately 48 h after transfection, the levels of phospho-AMPK Thr172, total AMPK, SIRT1 and PGC-1α signalling in low-glucose media were analysed. Representative western blot analysis and quantitative analyses of the results are shown. ** p < 0.01 compared with siRNA control. (c) The cultured mesangial cells were transfected with 50 nmol/l control siRNA or 50 nmol/l Ampkα1, Ampkα2 or Sirt1 siRNA and stimulated with resveratrol in high-glucose media. Approximately 48 h after stimulation, the levels of phospho-AMPK Thr172, total AMPK, SIRT1 and PGC-1α signalling in high-glucose media were analysed. Representative western blot analysis of the phospho-AMPK Thr172, total AMPK, SIRT1, PGC-1α and β-actin levels and the quantitative analyses of the results are shown. * p < 0.05 and ** p < 0.01 compared with other groups. (d) The cultured mesangial cells were transfected with 50 nmol/l control siRNA or 50 nmol/l Ampkα1, Ampkα2, Sirt1 or Pgc-1α siRNA and stimulated with resveratrol in high-glucose media. Representative pictures of TUNEL-positive mesangial cells (original magnification ×400) and the quantitative analyses of the results are shown. n = 4; ** p < 0.01 compared with other cell groups. Cont, control; HG, high glucose; LG, low glucose; Met, metformin; pAMPK, phospho-AMPK Thr172
Discussion
Pharmacologically targeting transcriptional networks to regulate or modulate the gene-expression programmes that favour energy expenditure is an attractive concept to combat metabolic diseases, particularly the complications of diabetes. Both AMPK and SIRT1 have emerged as interesting targets as they are heavily involved in catabolic metabolism, mitochondrial activation, angiogenesis and enhanced cell survival [3–6]. It is well known that the effects of resveratrol are mediated by both SIRT1 and AMPK [24]. However, the effects of resveratrol in the kidneys of an animal model of type 2 diabetes are not well known. The results of the present study demonstrate that diabetic nephropathy in db/db mice is associated with increases in renal lipid accumulation, apoptotic renal cell injury and oxidative stress that relate to the inactivation of AMPK–SIRT1–PGC-1α signalling and the deregulation of their target molecules, PPARα–ERR-1α and PI3K–Akt–FOXO3a. Diabetic nephropathy was ameliorated by resveratrol treatment via the activation of AMPK–SIRT1–PGC-1α signalling and the subsequent activation of PPARα–ERR-1α and FOXO3a, which reversed renal lipid accumulation, apoptotic renal cell injury and oxidative stress.
It is notable that AMPK and SIRT1 regulated each other and share many common target molecules, such as PGC-1α, PPARs, FOXOs, and NF-κB. Moreover, AMPK and SIRT1 have clinical relevance with regard to metabolic syndrome and type 2 diabetes, as their effects on target molecules lead to insulin resistance, mitochondrial dysfunction, oxidative and endoplasmic reticulum stress, and lipotoxicity associated with ectopic lipid accumulation [12]. SIRT1 also responds to changes in the availability of nutrients, such as in conditions of energy-intake restriction or starvation, and energy expenditure, through a forkhead-dependent pathway [25] and PGC-1α [9]. Thus, it has been suggested that the activation of AMPK and SIRT1 allows for the concurrent deacetylation and phosphorylation of their target molecules and decreases the susceptibility to diabetes-associated disorders. The current study demonstrates that the activation of AMPK and SIRT1 by resveratrol may prevent renal lipid accumulation and cell injury related to the activation of PGC-1α. This in vitro study demonstrated that the high-glucose-induced suppression of AMPK–SIRT1–PGC-1α signalling was activated by AMPK activators, such as resveratrol, AICAR and metformin. Additionally, increased AMPK–SIRT1–PGC-1α production mediated by resveratrol in high-glucose media was suppressed with the introduction of Ampkα1, Ampkα2 and Sirt1 siRNAs. When any of one of AMPK, SIRT1 and PGC-1α was knocked down in mesangial cells, levels of the others were also reduced. These results suggest that AMPK and SIRT1 activate each other and jointly regulate the downstream PGC-1α in the mesangial cells, as in the skeletal muscles [11, 26]. Consistent with our results, several recent studies have demonstrated that AMPK activation by adiponectin [27] or AICAR [28] protected renal podocytes and diminished albuminuria in diabetic animals by decreasing NADPH oxidase 4 (NOX4)-dependent oxidative stress and apoptosis. However, Kitada et al demonstrated that resveratrol protects against diabetic nephropathy through the direct scavenging of ROS, normalisation of the Mn-SOD function and glucose–lipid metabolism via AMPK/SIRT1-independent mechanisms [29]. The discrepancy between our results and previous studies regarding AMPK/SIRT1 signalling might reflect differences in the dose of resveratrol administered (0.3% vs 20 mg kg−1 day−1), the part of the renal tissue examined (whole kidney vs renal cortex) and the renal cell type studied (proximal epithelial cell vs mesangial cell).
PGC-1α exerts a wide array of effects and it directly co-activates multiple transcription factors, including nuclear receptors such as the PPARs [30, 31], glucocorticoid receptors [24], oestrogen receptors and ERRs [32, 33], and non-nuclear receptor transcription factors, such as myocyte enhancer factor-2 [34] and the family of FOXO transcription factors [35]. By simultaneously co-activating these transcription factors, PGC-1α can quickly and coordinately modulate a transcriptional programme that governs the energy metabolism. Although PGC-1α co-activation can change in response to different stimuli or in a tissue-specific manner, in the current study, PGC-1 exerted, in part, various renal effects by enhancing the production of PPARα and its target molecule ERR-1α, in addition to co-activating FOXO3a in relation to the PI3K–Akt axis.
We and others have demonstrated that PPARα activation by PPARα agonist prevents and improves diabetes- or high-fat-diet-induced renal injury by increasing the production of lipolytic enzymes and reducing lipid accumulation, oxidative stress and renal cell apoptosis, while inhibiting the development of albuminuria and glomerular fibrosis [12, 13, 36]. ERR-1α activation by PGC-1α and PPARα induces genes with roles in lipid transport [36], oxidative phosphorylation [17, 37], fatty acid oxidation [38, 39], the tricarboxylic acid cycle [30, 34, 35], mitochondrial biogenesis [17, 39] and oxidative stress defence [18]. In the current study, resveratrol increased PPARα–ERR-1α production and decreased SREBP1, and this was closely associated with decreased lipid content in the kidney. We also showed that high-glucose treatment of mesangial cells inhibits the expression of genes involved in lipolysis, such as those encoding PPARα and CPT-1A. Additionally, lipogenic genes, such as that encoding SREBP1, were induced by high-glucose treatment. Resveratrol treatment in the presence of high glucose reversed these changes, suggesting that the renoprotective impact of resveratrol may be mediated by shifting the gene-expression profile of the cells to a state that favours lipolysis.
The db/db mouse, which lacks signalling through the leptin receptor, is an excellent model of type 2 diabetes because it develops hyperphagia, obesity, hyperleptinaemia and overt hyperglycaemia [40]. In this study, db/db mice, with or without resveratrol treatment, ate about twice the amount eaten by the db/m mice. Leptin increases glucose uptake and type 1 collagen in db/db mesangial cells through a TGF-β–PI3K-dependent pathway [41]. In addition, transgenic mice with leptin overexpression demonstrated an increase in collagen type IV and fibronectin mRNA in the kidney [42]. Recently, it has been demonstrated that the reduced AMPK and SIRT1 function in db/db mice causes dysregulation of adipogenic, lipogenic and lipo-oxidative genes, including leptin, to favour an obese phenotype [42]. These results suggest that resveratrol treatment might partially improve leptin-related TGF-β–PI3K and lipid dysregulation through the activation of AMPK–SIRT1–PGC-1α in the db/db mouse kidney.
In the current study, we found that resveratrol treatment increased the production of AMPK and SIRT1 and decreased PI3K–Akt signalling in the kidneys of db/db mice and the mesangial cells in high-glucose media. In contrast, Schenk et al demonstrated that restriction of energy intake induced SIRT1 activation in mice, resulting in enhanced skeletal muscle insulin sensitivity, via PI3K modulation, and suggested that insulin-stimulated PI3K signalling is essential for the functional improvement of glucose transport in the skeletal muscle, and that SIRT1 is a key orchestrator of adaptation mediated by restriction of energy intake [43]. The discrepancy in effects in this study and the previous energy-restriction study might be because of differences in plasma insulin concentration and target organ. Restriction of energy intake augments insulin-stimulated PI3K activity in response to a physiological insulin concentration (60 μU/ml) [29]. In contrast, at the supraphysiological concentration of insulin, such as in db/db (more than 200 μU/ml) mice, PI3K would be activated in the kidney [44].
Regarding FOXO signalling in diabetic nephropathy, a novel mechanism of diabetic nephropathy has been suggested [39]. Diabetic conditions increase TGF-β abundance in the mesangial cells and TGF-β activates p38 mitogen-activated protein kinase (MAPK), extracellular signal-regulated kinases (ERKs), PI3K–Akt and Smads [45]. Among these, PI3K–Akt activation by TGF-β induces FOXO3a phosphorylation that results in decreased BCL-2 interacting mediator of cell death (BIM) and Mn-SOD. In contrast, another study has demonstrated that the PI3K–Akt pathway acts as a survival and anti-apoptotic signal in the renal cells [46]. Overall, the data from the present study indicate that diabetes increases PI3K–Akt phosphorylation and FOXO3a phosphorylation, and this is accompanied by significant changes in the expression of key FOXO3a target genes, as reflected by the decreases in anti-apoptotic BCL-2 and the antioxidants SOD1 and SOD2, and the increase in the expression of the pro-apoptotic gene Bax. Consequently, FOXO3a inactivation resulted in apoptotic renal cell death and oxidative stress. However, it is interesting that 12 weeks of treatment with resveratrol led to a protective increase in FOXO3a in the kidney, where it contributed to protection against apoptotic cell death and oxidative stress.
In conclusion, our results demonstrate that activation of AMPK and SIRT1 was associated with PCG-1α-ameliorated lipotoxicity in the kidney, which could be related to apoptosis and oxidative stress in diabetic nephropathy. Resveratrol, as an activator of AMPK–SIRT1–PGC-1α signalling, affected at least two pathways in the development of diabetic nephropathy. One pathway enhanced the PPARα–ERR-1α–SREBP1-mediated removal of lipids that had accumulated in the kidney. The other pathway decreased apoptotic renal cell death and oxidative stress related to FOXO3a activation. These signalling events may improve glomerular matrix accumulation, inflammation and albuminuria. Our data further substantiate the suggestion that high-glucose-induced mesangial cell damage translates into lower AMPK–SIRT1–PGC-1α activity and exacerbated oxidative stress and apoptotic cell damage in the setting of diabetes. All of the changes in AMPK–SIRT1–PGC-1α signalling were reversed by resveratrol treatment. These results suggest that resveratrol may be a novel therapeutic agent for type 2 diabetic nephropathy.
Abbreviations
- 8-OH-dG:
-
8-Hydroxy-deoxyguanosine
- AICAR:
-
5-Aminoimidazole-4-carboxamide-1β-d-ribofuranoside
- AMPK:
-
AMP-activated protein kinase
- BAX:
-
BCL-2-associated X protein
- BCL:
-
B cell leukaemia/lymphoma 2
- CMC:
-
Cellulose sodium salt
- CPT-1A:
-
Carnitine palmitoyltransferase-1A
- db/db Res:
-
Diabetic mice receiving resveratrol
- db/m Res:
-
Non-diabetic mice receiving resveratrol
- eNOS:
-
Endothelial nitric oxide synthase
- ERR:
-
Oestrogen-related receptor
- F4/80:
-
Cell surface glycoprotein F4/80
- FOXO:
-
Class O forkhead box
- NF-κB:
-
Nuclear factor κB
- PGC-1α:
-
PPARγ co-activator 1α
- PI3K:
-
Phosphatidylinositol-3 kinase
- PPAR:
-
Peroxisome proliferator-activated receptor
- ROS:
-
Reactive oxygen species
- si:
-
Small interfering
- SIRT1:
-
Silent information regulator T1
- SOD:
-
Superoxide dismutase
- SREBP1:
-
Sterol regulatory element-binding protein 1
References
Jin DC, Ha IS, Kim NH et al (2012) Brief report: renal replacement therapy in Korea, 2010. Kidney Res Clin Pract 31:62–71
Murea M, Freedman BI, Parks JS, Antinozzi PA, Elbein SC, Ma L (2010) Lipotoxicity in diabetic nephropathy: the potential role of fatty acid oxidation. Clin J Am Soc Nephrol 5:2373–2379
Brunet A, Sweeney LB, Sturgill JF et al (2004) Stress-dependent regulation of FOXO transcriptional factors by the SIRT1 deaceylase. Science 303:2011–2015
Yeung F, Hoberg JE, Ramsay CS et al (2004) Modulation of NF-kappaB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J 23:2369–2380
Rodgers JT, Lerin W, Haas W, Gygi SP, Spiegelman BM, Puigserver P (2005) Nutrient control of glucose homeostasis through a complex of PGC-1alpha and SIRT1. Nature 434:113–118
Lagouge M, Argmann C, Gerhart-Hines Z et al (2006) Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell 127:1109–1122
Picard F, Kurtev M, Chung N et al (2004) Sirt1 promotes fat mobilization in white adipocytes by repressing PPAR-gamma. Nature 429:771–776
Purushotham A, Schug TT, Xu Q, Surapureddi S, Guo X, Li X (2009) Hepatocyte-specific deletion of SIRT1 alters fatty acid metabolism and results in hepatic steatosis and inflammation. Cell Metab 9:327–338
Nemoto S, Fergusson MM, Finkel T (2005) SIRT1 functionally interacts with the metabolic regulator and transcriptional coactivator PGC-1α. J Biol Chem 280:16456–16460
Kahn BB, Alquier T, Carling D, Hardie DG (2005) AMP-activated protein kinase: an ancient energy gauge provides clues to modern understanding of metabolism. Cell Metab 1:15–25
Ruderman NB, Xu XJ, Nelson L et al (2010) AMPK and SIRT1: a long-standing partnership? Am J Physiol Endocrinol Metab 298:E751–E760
Park CW, Zhang Y, Zhang X et al (2006) PPARalpha agonist fenofibrate improves diabetic nephropathy in db/db mice. Kidney Int 69:1511–1517
Shin SJ, Lim JHM, Chung S et al (2009) Peroxisome proliferator-activated receptor-alpha activator fenofibrate prevents high-fat diet-induced renal lipotoxicity in spontaneously hypertensive rats. Hypertens Res 32:835–845
Fissithaler B, Fleming I (2009) Activation and signaling by the AMP-activated protein kinase in endothelial cells. Circ Res 105:114–127
Goya K, Sumitani S, Xu X et al (2004) Peroxisome proliferator-activated receptor α agonists increase nitric oxide synthase expression in vascular endothelial cells. Arterioscler Thromb Vasc Biol 24:658–663
Okayasu Y, Tomizawa A, Suzuki A, Manaka K, Httori Y (2008) PPARα activators upregulate eNOA activity and inhibit cytokine-induced NF-κB activation through AMP-activated protein kinase activation. Life Sci 82:884–891
Schreiber SN, Emter R, Hock MB et al (2004) The estrogen-related receptor alpha (ERRalpha) functions in PPARgamma coactivator 1alpha(PGC-1alpha)-induced mitochondrial biogenesis. Proc Natl Acad Sci USA 101:6472–6477
Rangwala SM, Li X, Lindsley L et al (2007) Estrogen-related receptor alpha is essential for the expression of antioxidant protection genes and mitochondrial function. Biochem Biophys Res Commun 357:231–236
Yoshikawa T, Ide T, Shimano H et al (2003) Cross-talk between peroxisome proliferator-activated receptor (PPAR) alpha and liver X receptor (LXR) in nutritional regulation of fatty acid metabolism. I. PPARs suppress sterol regulatory element binding protein-1c through inhibition of LXR signaling. Mol Endocrinol 17:1240–1254
Olmos Y, Valle I, Borniquel S et al (2009) Mutual dependence of FoxO3a and PGC-1alpha in the induction of oxidative stress genes. J Biol Chem 284:14476–14484
Pearson KI, Baur JA, Lewis KN et al (2008) Resveratrol delays age-related deterioration and mimics transcriptional aspects of dietary restriction without extending life span. Cell Metab 8:157–168
Delaney B, Nicolosi RJ, Wilson TA et al (2003) Beta-glucan fractions from barley and oats are similarly antiatherogenic in hypercholesterolemic Syrian golden hamsters. J Nutr 133:468–475
Park CW, Kim JH, Lee JH et al (2002) High glucose-induced intercellular adhesion molecule-1 (ICAM-1) expression through an osmotic effect in rat mesangial cells is PKC-NF-kappa B-dependent. Diabetologia 43:1544–1553
Baur JA, Pearson KJ, Price NL et al (2006) Resveratrol improves health and survival of mice on a high-calorie diet. Nature 444:337–342
Nemoto S, Fergusson MM, Finkel T (2004) Nutrient availability regulates SIRT1 through a forkhead-dependent pathway. Science 306:2105–2108
Canto C, Gerhart-Hines Z, Feige JN et al (2009) AMPK regulates energy expenditure by modulating NAD+ metabolism and SIRT1 activity. Nature 458:1056–1060
Sharma K, RamachandraRao S, Qiu G et al (2008) Adiponectin regulates albuminuria and podocyte function in mice. J Clin Invest 118:1645–1656
Eld AA, Ford BM, Block K et al (2010) AMP-activated protein kinase (AMPK) negatively regulates Nox-4-dependent activation of p53 and epithelial cell apoptosis in diabetes. J Biol Chem 285:37503–37512
Kitada M, Kume S, Imazumi N, Koya D (2011) Resveratrol improves oxidative stress and protects against diabetic nephropathy through normalization of Mn-SOD dysfunction in AMPK/SIRT1-independent pathway. Diabetes 60:634–643
Vega RB, Huss JM, Kelly DP (2000) The coactivator PGC-1 cooperates with peroxisome proliferator-activated receptor alpha in transcriptional control of nuclear genes encoding mitochondrial fatty acid oxidation enzymes. Mol Cell Biol 20:1868–1876
Wang YX, Lee CH, Tiep S et al (2003) Peroxisome-proliferator-activated receptor delta activates fat metabolism to prevent obesity. Cell 113:159–170
Huss JM, Kopp RP, Kelly DP (2002) Peroxisome proliferator-activated receptor coactivator-1alpha (PGC-1alpha) coactivates the cardiac-enriched nuclear receptor estrogen-related receptor-alpha and -gamma. Identification of novel leucine-rich interaction motif within PGC-1alpha. J Biol Chem 277:20265–20274
Schreiber SN, Knutti D, Brogli K, Uhlmann T, Kralli A (2003) The transcriptional coactivator PGC-1 regulated the expression and activity of the orphan nuclear receptor estrogen-related receptor alpha (ERRalpha). J Biol Chem 278:9013–9018
Michael LF, Wu Z, Cheatham RB et al (2001) Restoration of insulin-sensitive glucose transporter (GLUT4) gene expression in muscle cells by the transcriptional coactivator PGC-1. Proc Natl Acad Sci USA 98:3820–3825
Puigserver P, Rhee J, Donocan J (2003) Insulin-required hepatic gluconeogenesis through FOXO1-PGC-1alpha interaction. Nature 423:550–555
Tanaka Y, Kume S, Araki S et al (2011) Fenofibrate, a PPARα agonist, has renoprotective effects by enhancing renal lipolysis. Kidney Int 71:871–882
Huss JM, Torra IP, Staels B, Giquere V, Kelly DP (2004) Estrogen-related receptor alpha directs peroxisome proliferator-activated receptor alpha signaling in the transcriptional control of energy metabolism in cardiac and skeletal muscle. Mol Cell Biol 24:9079–9091
Carrier JC, Delblois G, Champigny C, Levy E, Giquere V (2004) Estrogen-related receptor alpha (ERRalpha) is a transcription regulator of apolipoprotein A-IV and controls lipid handling in the intestine. J Biol Chem 279:52052–52058
Villena JA, Hock MB, Chang WY, Barcas JE, Giquere V, Kralli A (2007) Orphan nuclear receptor estrogen-related receptor alpha is essential for adaptive thermogenesis. Proc Natl Acad Sci USA 104:1418–1423
Han DC, Isono M, Chen S et al (2001) Leptin stimulates type 1 collagen production in db/db mesangial cells: glucose uptake and TGF-β type II receptor expression. Kidney Int 59:1315–1323
Ninichuk V, Khandoga AG, Segerer S et al (2007) The role of interstitial macrophages in nephropathy of type 2 db/db mice. Am J Pathol 170:1267–1276
Schung TT, Li X (2011) Sirtuin 1 in lipid metabolism and obesity. Ann Med 43:196–211
Schenk S, McCurby CE, Philp A et al (2011) Sirt1 enhances skeletal muscle insulin sensitivity in mice during caloric restriction. J Clin Invest 121:4281–4288
Lee MJ, Felers D, Mariappan MM et al (2007) A role for AMP-activated protein kinase in diabetes-induced renal hypertrophy. Am J Physiol Renal Physiol 292:F617–F627
Kato M, Yuan H, Xu ZG et al (2006) Role of the Akt/FoxO3a pathway in TGF-β1-mediated mesangial cell dysfunction: a novel mechanism related to diabetic kidney disease. J Am Soc Nephrol 17:3325–3335
Shimamura H, Terade Y, Okado T, Tanaka H, Inoshita S, Sasaki S (2003) The PI3-kinase-Akt pathway promotes mesangial cell survival and inhibits apoptosis in vitro via NF-κB and Bad. J Am Soc Nephrol 14:1427–1434
Acknowledgements
The authors would like to thank S. W. Kim, Division of Urology, The Catholic University of Korea, and B. S. Choi, Seogang University, for their valuable discussion.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Minister of Education, Science and Technology (to C. W. Park; A111055).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
MYK, JHL, HHY, YAH, KSY, HSP, SC, SHK, SJS, BSC, HWK, YSK, JHL, YSC and CWP designed and performed the studies and analysed data. CWP directed the study, interpreted the data and wrote the paper. All authors critically revised and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary materials
Below is the link to the electronic supplementary material.
ESM Methods
(PDF 144 kb)
ESM Results
(PDF 5 kb)
ESM Fig. 1
(PDF 39 kb)
Rights and permissions
About this article
Cite this article
Kim, M.Y., Lim, J.H., Youn, H.H. et al. Resveratrol prevents renal lipotoxicity and inhibits mesangial cell glucotoxicity in a manner dependent on the AMPK–SIRT1–PGC1α axis in db/db mice. Diabetologia 56, 204–217 (2013). https://doi.org/10.1007/s00125-012-2747-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2747-2