Abstract
Introduction and hypothesis
The purpose of the study was to analyze anatomical and functional outcomes after sacrocolpopexy (SCP) for vaginal vault prolapse pelvic organ prolapse quantification (POPQ) II–III by random use of absorbable (Vicryl) and non-absorbable sutures (Ethibond) for vaginal mesh fixation.
Methods
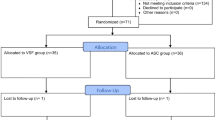
This study was designed as a two-center randomized controlled study (RCT). The primary objective was to evaluate the anatomical outcome. Success was defined when the vaginal apex (point C; POPQ) did not descend more than 50% of the total vaginal length (tvl) during Valsalva. Patients completed a pelvic examination incorporating the POPQ and questionnaires (the German pelvic floor questionnaire and the PISQ-12 questionnaire) at baseline and 6 months postsurgery. Perioperative adverse events (AE) were recorded. Sample size calculations, based on a 10% non-inferiority limit required 100 participants per group, with power = 90%.
Results
In 190 out of 195 women (ETH group n = 96; VIC group n = 94) anatomical success was achieved. The relative risk of anatomical success failure in the VIC group versus the ETH group was 0.69, with a 95% confidence interval 0.12–4.02. The change in the symptom scores did not differ significantly between the ETH and the VIC group. In the ETH group, three suture penetrations into the vagina were observed, and none in the VIC group 6 months postoperatively.
Conclusions
Anatomical success after SCP for vaginal vault prolapse POPQ II–III is not affected by suture type for vaginal monofilament mesh attachment. Moreover, we did not see any differences in functional outcomes between the two groups. Three suture penetrations into the vagina were observed in the ETH group, and none in the VIC group 6 months postoperatively.



Similar content being viewed by others
References
Nygaard I, Brubaker L, Zyczynski HM, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309:2016–24.
Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol. 2004;190:20–6.
Siddiqui NY, Grimes CL, Casiano ER, et al. Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis. Obstet Gynecol. 2015;125:44–55.
Matthews CA, Geller EJ, Henley BR, et al. Permanent compared with absorbable suture for vaginal mesh fixation during total hysterectomy and sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2020;136:355–64. https://doi.org/10.1097/AOG.0000000000003884.
Tagliaferri V, Ruggieri S, Taccaliti C, et al. Comparison of absorbable and permanent sutures for laparoscopic sacrocervicopexy: a randomized controlled trial. Acta Obstet Gynecol Scand. 2021;100:347–52. https://doi.org/10.1111/aogs.13997.
Tan-Kim J, Menefee SA, Lippmann Q, et al. A pilot study comparing anatomic failure after sacrocolpopexy with absorbable or permanent sutures for vaginal mesh attachment. Perm J. 2014;18:40–4. https://doi.org/10.7812/TPP/14-022.
Nygaard IE, McCreery R, Brubaker L, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104:805–23.
Flynn MK, Romero AA, Amundsen CL, Weidner AC. Vascular anatomy of the presacral space: a fresh tissue cadaver dissection. Am J Obstet Gynecol. 2005;192:1501–5.
Wieslander CK, Rahn DD, McIntire DD, et al. Vascular anatomy of the presacral space in unembalmed female cadavers. Am J Obstet Gynecol. 2006;195:1736–41.
North CE, Ali-Ross NS, Smith AR, Reid FM. A prospective study of laparoscopic sacrocolpopexy for the management of pelvic organ prolapse. BJOG. 2009;116:1251–7.
Ganatra AM, Rozet F, Sanchez-Salas R, et al. The current status of laparoscopic sacrocolpopexy: a review. Eur Urol. 2009;55:1089–103.
Shiozawa T, Huebner M, Hirt B, Wallwiener D, Reisenauer C. Nerve-preserving sacrocolpopexy: anatomical study and surgical approach. Eur J Obstet Gynecol Reprod Biol. 2010;152:103–7.
Baessler K, O’Neill SM, Maher CF, Battistutta D. A validated self-administered female pelvic floor questionnaire. Int Urogynecol J. 2010;21:163–72.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2003;14:164–8.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. Erratum: a short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J. 2004;15:219.
Wren PA, Janz NK, Brubaker L, et al. Reliability of health-related quality of life measures 1 year after surgical procedures for pelvic floor disorders. Am J Obstet Gynecol. 2005;192:780–8.
Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
Blackwelder WC. Proving the null hypothesis in clinical trials. Control Clin Trials. 1982;3:345–53. https://doi.org/10.1016/0197-2456(82)90024-1.
Barbolt TA. Biology of polypropylene/polyglactin 910 grafts. Int Urogynecol J. 2006;17:26–30.
North CE, Ali-Ross NS, Smith AR, Reid FM. A prospective study of laparoscopic sacrocolpopexy for the management of pelvic organ prolapse. BJOG. 2009;116:1251–7.
Baessler K, Schuessler B. Abdominal sacrocolpopexy and anatomy and function of the posterior compartment. Obstet Gynecol. 2001;97:678–84.
Fox SD, Stanton SL. Vault prolapse and rectocele: assessment of repair using sacrocolpopexy with mesh interposition. BJOG. 2000;107:1371–5.
Forsgren C, Zetterström J, Zhang A, Iliadou A, Lopez A, Altman D. Anal incontinence and bowel dysfunction after sacrocolpopexy for vaginal vault prolapse. Int Urogynecol J. 2010;21:1079–84.
Geomini PM, Brolmann HA, van Binsbergen NJ, Mol BW. Vaginal vault suspension by abdominal sacral colpopexy for prolapse: a follow up study of 40 patients. Eur J Obstet Gynecol Reprod Biol. 2001;94:234–8.
Lefranc JP, Atallah D, Camatte S, Blondon J. Longterm followup of posthysterectomy vaginal vault prolapse abdominal repair: a report of 85 cases. J Am Coll Surg. 2002;195:352–8.
Mauroy B, Demondion X, Drizenko A, et al. The inferior hypogastric plexus (pelvic plexus): its importance in neural preservation techniques. Surg Radiol Anat. 2003;25:6–15.
Johnson RM, McGuire EJ. Urogenital complications of anterior approaches to the lumbar spine. Clin Orthopaed Relat Res. 1981;154:114–8.
Junginger T, Kneist W, Heintz A. Influence of identification and preservation of pelvic autonomic nerves in rectal cancer surgery on bladder dysfunction after total mesorectal excision. Dis Colon Rectum. 2003;46:621–8.
Kneist W, Heintz A, Wolf HK, Junginger T. Identification of pelvic autonomic nerves during partial and total mesorectal excision—influence parameters and significance for neurogenic bladder. Chirurg. 2004;75:276–83.
Kavvadias T, Schoenfisch B, Huebner M, Brucker SY, Wallwiener D, Reisenauer C. Perioperative adverse events associated with pelvic organ prolapse repair by nerve-preserving sacropexy: an analysis of 768 cases over a 10-year period. Arch Gynecol Obstet. 2018;298:353–61.
Anand M, Woelk JL, Weaver AL, Trabuco EC, Klingele CJ, Gebhart JB. Perioperative complications of robotic sacrocolpopexy for post-hysterectomy vaginal vault prolapse. Int Urogynecol J. 2014;25:1193–200.
Matthews CA. Minimally invasive sacrocolpopexy: how to avoid short- and long-term complications. Curr Urol Rep. 2016;17:81. https://doi.org/10.1007/s11934-016-0638-7.
Acknowledgements
The authors would like to thank Sabine Hahn, MD, for data collection and the gynecological examination of the study participants at the follow-up visits; Jacqueline Behrend, study nurse, for supporting the part of the study in Berlin; and Friederike Moroff for entering the data into the database.
Funding
The study was not funded.
Author information
Authors and Affiliations
Contributions
Christl Reisenauer: concept and design, analysis and interpretation of data, manuscript draft and revision; Juergen Andress: analysis and interpretation of data, manuscript draft; Birgitt Schoenfisch: concept and design, statistics, analysis and interpretation of data, manuscript revision; Markus Huebner: analysis and interpretation of data, manuscript revision; Sara Yvonne Brucker: concept and design, manuscript revision; Kathrin Beilecke: analysis and interpretation of data, manuscript draft; Andrea Lippkowski: analysis and interpretation of data, manuscript draft; Juliane Marschke: analysis and interpretation of data, manuscript draft; Ralf Tunn: concept and design, analysis and interpretation of data, manuscript revision.
Corresponding author
Ethics declarations
Conflicts of interest
Christl Reisenauer, Juergen Andress, Birgitt Schoenfisch: no conflicts of interest; Sara Y. Brucker: personal fees from Pfizer; Novartis, Teva, MSD, AstraZeneca, Storz, and Roche; Markus Huebner: consultant for Promedon GmbH; Andrea Lippkowski: grant from Promedon, support for German Pelvic Floor Center Berlin, personal fee from Coloplast; Kathrin Beilecke: grant from Promedon, support for the German Pelvic Floor Center Berlin; Juliane Marschke: grant from Promedon, support for the German Pelvic Floor Center Berlin; Ralf Tunn: grant from Promedon, support for the German Pelvic Floor Center Berlin.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reisenauer, C., Andress, J., Schoenfisch, B. et al. Absorbable versus non-absorbable sutures for vaginal mesh attachment during sacrocolpopexy: a randomized controlled trial. Int Urogynecol J 33, 411–419 (2022). https://doi.org/10.1007/s00192-021-04853-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04853-4