Abstract
Introduction and hypothesis
We compared vaginal hysterectomy with bilateral sacrospinous fixation plus an anterior polyvinylidene fluoride mesh versus abdominal sacrocolpopexy for the treatment of primary apical prolapse in postmenopausal women.
Methods
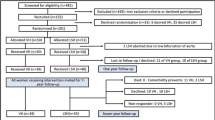
A prospective, randomized, single-blind, parallel study [Registro Brasileiro de Ensaios Clinicos (REBEC) trial register code RBR-7t6rg2] was performed from October 2015 to May 2016. A total of 71 postmenopausal women with advanced pelvic organ prolapse (POP) and undergoing surgery were randomized to the abdominal sacrocolpopexy (ASC) (n = 36) or the vaginal sacrospinous fixation with anterior mesh (VSF-AM) (n = 35) groups. Pelvic Organ Prolapse Quantification (POP-Q) system classification was performed for objective assessment, and the International Consultation on Incontinence Questionnaire–Vaginal Symptoms (ICIQ-VS), International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), and International Consultation on Incontinence Questionnaire Overactive Bladder (ICIQ-OAB) questionnaires were filled out for subjective evaluation by women before and 1 year after surgery. All procedures were performed by a single surgeon.
Results
Both groups had improvement in almost POP-Q points (except for vaginal length in the VSF-AM group) and all ICIQ scores. The ASC group had a longer operative time (129 versus 117 min, p = 0.0038) and duration for return to activities (103 versus 57 days, p < .05). Four women (11%) in the VSF-AM group were reoperated versus none from the ASC group (p = .05).
Conclusions
Although the study did not achieve the planned recruitment, after 12 months of follow-up, ASC did not differ from VSF-AM in objective and subjective scores (ICIQ questionnaires; POP-Q measurements). Recovery time was longer after open abdominal surgery.

Similar content being viewed by others
References
Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001;184(7):1496–501.
Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int Urogynecol J. 2018;29(1):13–21.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10:CD012376.
de Castro EB, Juliato CR, Piedemonte LA, dos Santos Júnior LC. Impact of sacrospinous colpopexy associated with anterior colporrhaphy for the treatment of dome prolapse on all three vaginal compartments. Rev Bras Ginecol Obstet. 2016;38(7):356–64.
Sze EH, Karram MM. Transvaginal repair of vault prolapse: a review. Obstet Gynecol. 1997;89(3):466–75.
Morgan DM, Rogers MA, Huebner M, Wei JT, DeLancey JO. Heterogeneity in anatomic outcome of sacrospinous ligament fixation for prolapse: a systematic review. Obstet Gynecol. 2007;109(6):1424–33.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;30(4):CD004014.
Lo TS, Tan YL, Khanuengkitkong S, Dass AK. Surgical outcomes of anterior transobturato rmesh and vaginal sacrospinous ligament fixation for severe pelvic organ prolapse in overweight and obese Asian women. Int Urogynecol J. 2013;24(5):809–16.
Juliato CR, Mazzer MF, Diniz JM, Farias CH, de Castro EB. Sacrospinous ligament suspension with transobturator mesh versus sacral colpopexy for genital prolapse. Clinics. 2016;71(9):487–93.
To V, Hengrasmee P, Lam A, Luscombe G, Lawless A, Lam J. Evidence to justify retention of transvaginal mesh: comparison between laparoscopic sacral colpopexy and transvaginal elevate mesh. Int Urogynecol J. 2017;28(12):1825–32.
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. PLoS Med. 2010;357:e1000251.
de Castro EB, Brito LGO, Giraldo PC, Teatin Juliato CR. Does the vaginal flora modify when a synthetic mesh is used for genital prolapse repair in postmenopausal women? A pilot, randomized controlled study. Female Pelvic Med Reconstr Surg. 2018. https://doi.org/10.1097/SPV.0000000000000539.
Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7.
Price N, Jackson SR, Avery K, Brookes ST, Abrams P. Development and psychometric evaluation of the ISIQ vaginal symptoms questionnaire: the ICIQ-VS. BJOG. 2006;113(6):700–12.
Tamanini JT, Almeida FG, Girotti ME, Riccetto CL, Palma PC, Rios LA. The Portuguese validation of the international consultation on incontinence questionnaire-vaginal symptoms (ICIQ-VS) for Brazilian women with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(10):1385–91.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30.
Tamanini JT, Dambros M, D’Ancona CA, Palma PC, Rodrigues Netto N Jr. Validation of the “international consultation on incontinence questionnaire-short form” (ICIQ-SF) for Portuguese. Rev Saude Publica. 2004;38(3):438–44.
International Consultation on Incontinence Modular Questionnaire. ICIQ-overactive bladder: ICIQ-OAB [Internet]. Bristol Urological Institute [cited 2009 Out 16]. Available from: <http://www.iciq.net/ICIQ.OABmodule.html>.
Pereira SB, Thiel RRC, Riccetto C, Silva JM, Pereira LC, Herrmann V, et al. Validation of the international consultation on incontinence questionnaire overactive bladder (ICIQ-OAB) for Portuguese. Rev Bras Ginecol Obstet. 2010;32(6):273–8.
Benson J, Lucente V, McClellan E. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol. 1996;175:1418–22.
Juliato CR, Santos Júnior LC, Haddad JM, Castro RA, Lima M, Castro EB. Mesh surgery for anterior vaginal wall prolapse: a meta-analysis. Rev Bras Ginecol Obstet. 2016;38(7):356–64.
Tan YL, Lo TS, Khanuengkitkong S, Krishna Dass A. Comparison of outcomes after vaginal reconstruction surgery between elderly and younger women. Taiwan J Obstet Gynecol. 2014;53(3):348–54.
Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol. 2004;190:20–6.
Baessler K, Maher C. Pelvic organ prolapse surgery and bladder function. Int Urogynecol J. 2013;24(11):1843–52.
Balsamo R, Illiano E, Zucchi A, Natale F, Carbone A, Sio M, et al. Sacrocolpopexy with polyvinylidene fluoride mesh for pelvic organ prolpase: mid term comparative outcomes with polypropylene mesh. Eur J Obstet Gynecol Reprod Biol. 2018;220:74–8.
Barski D, Arndt C, Gerullis H, Yang J, Boros M, Otto T, et al. Transvaginal PVDF-mesh for cystocele repair: a cohort study. Int J Surg. 2017;39:249–54.
Eisenberg VH, Callewaert G, Sindhwani N, Housmans S, van Schoubroeck D, Lowenstein L, et al. Ultrasound visualization of sacrocolpopexy polyvinylidene fluoride meshes containing paramagnetic Fe particles compared with polypropylene mesh. Int Urogynecol J. 2018. https://doi.org/10.1007/s00192-018-3728-x.
Acknowledgments
The authors thank all patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None. FEG Textiltechnik donated the synthetic mesh (Dynamesh®) but had no influence regarding the study design and data collection/analysis.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Castro, E.B., Brito, L.G.O. & Juliato, C.R.T. Vaginal hysterectomy with bilateral sacrospinous fixation plus an anterior mesh versus abdominal sacrocervicopexy for the treatment of primary apical prolapse in postmenopausal women: a randomized controlled study. Int Urogynecol J 31, 365–372 (2020). https://doi.org/10.1007/s00192-019-03948-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03948-3