Background and Purpose:
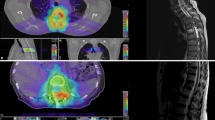
High-dose irradiation or reirradiation of spinal and paraspinal tumors is a challenge particularly in the presence of metal artifacts after surgery. Image-guided advanced intensity-modulated radiotherapy delivers high-dose radiation to the tumor sparing the spinal cord. Precise delineation of the spinal cord is necessary treating para- and intraspinal tumors with a sufficient dose.
Patients and Methods:
The use of myelo-CT was evaluated in 23 patients with spinal and paraspinal tumors. All patients had had previous surgery with metal implants in the radiation area. All patients had an indication for high-dose irradiation. Treatment planning was performed using nonenhanced and contrast-enhanced myelo-CT in the same position and immobilization and both CT scans were matched. Treatment was performed by using a tomotherapy treatment unit.
Results:
Contouring of the myelon in all slices of the myelo-CT was possible in 20 of 23 patients. All these patients were treated with doses of median 69.4 Gy in 2 Gy/1.8 Gy single doses using daily image guidance. One patient received an integrated boost with a TD/SD of 70/2.3 Gy. No side effects have been observed so far during a median follow-up of 15.5 months. No separation between tumor and myelon could be observed in 3 patients.
Conclusion:
Myelo-CT offers a distinct delineation of the myelon and the paraspinal tumor in case of artifacts due to metal implants after surgery. Using this tool in combination with advanced image guidance and IMRT techniques, patients with relatively radioresistent paraspinal tumors might have the chance of improved local control using higher target doses.
Hintergrund:
Hochdosisbestrahlung oder Rebestrahlung von spinalen und paraspinalen Tumoren ist eine Herausforderung, besonders in Gegenwart von Metallartefakten nach Operation. Bildgeführte intensitätsmodulierte Radiotherapie liefert eine hohe Strahlendosis auf den Tumor unter Schonung des Rückenmarks. Daher ist eine genaue Abgrenzung des Rückenmarks notwendig, um die Behandlung para- und intraspinaler Tumoren mit einer ausreichenden Dosis durchführen zu können.
Patienten und Methoden:
Die Verwendung eines Myelo-CT wurde bei 23 Patienten mit spinalen und paraspinalen Tumoren untersucht. Alle Patienten hatten Voroperationen mit Metallimplantaten im Bestrahlungsbereich. Alle Patienten hatten eine Indikation zur Hochdosisbestrahlung. Die Bestrahlungsplanung erfolgte mit einem nativen CT und einem Myelo-CT in gleicher Lagerung und Immobilisation. Die beiden CT-Scans wurden fusioniert. Die Bestrahlung erfolgte mittels einer Tomotherapieeinheit.
Ergebnisse:
Die Konturierung des Myelon in allen Schichten des Myelo-CT war bei 20/23 Patienten möglich. Alle diese Patienten wurden erfolgreich mit einer medianen Dosis von 69.4 Gy in 2-Gy-/1,8-Gy-Einzeldosen behandelt. Ein Patient erhielt einen integrierten Boost mit einer GD/ED von 70/2,3 Gy. Bei einem medianen Follow-up von 15,5 Monaten wurden keine Nebenwirkungen der Behandlung festgestellt. Eine Abgrenzung des Myelon vom Tumorgewebe war bei 3 Patienten nicht möglich.
Schlussfolgerung:
Das Myelo-CT führt zu einer deutlichen Abgrenzbarkeit des Myelons von paraspinalen und spinalen Tumoren bei Metallartefakten nach Operation. Mit diesem Werkzeug in Kombination mit modernen IMRT-Techniken, könnte eine Verbesserung der Lokalrezidivrate bei Patienten mit relativ radioresistenten paraspinalen Tumoren erreicht werden.
Similar content being viewed by others
References
Aarup LR, Nahum AE, Zacharatou C et al. The effect of different lung densities on the accuracy of various radiotherapy dose calculation methods: implications for tumour coverage. Radiother Oncol 2009;91:405–414.
Ahnesjö A, Aspradakis MM. Dose calculations for external photon beams in radiotherapy. Phys Med Biol 1999;44:R99–155.
Ahnesjö A. Collapsed cone convolution of radiant energy for photon dose calculation in heterogeneous media. Med Phys 16:577–592.
Bogner L, Scherer J, Treutwein M et al. Verification of IMRT: techniques and problems. Strahlenther Onkol 2004;180:340–350.
Carrasco P, Jornet N, Duch MA et al. Comparison of dose calculation algorithms in slab phantoms with cortical bone equivalent heterogeneities. Med Phys 2007;34:3323–3333.
Dogan N, Mihaylov I, Wu Y et al. Monte Carlo dose verification of prostate patients treated with simultaneous integrated boost intensity modulated radiation therapy. Radiat Oncol 2009;4:18.
Dogan N, Siebers JV, Keall PJ et al. Improving IMRT dose accuracy via deliverable Monte Carlo optimization for the treatment of head and neck cancer patients. Med Phys. 2006;33:4033–4043.
Fippel M, Haryanto F, Dohm O et al. A virtual photon energy fluence model for Monte Carlo dose calculation. Med Phys 2003;30:301–311.
Fippel M, Laub W, Huber B et al. Experimental investigation of a fast Monte Carlo photon beam dose calculation algorithm. Phys Med Biol 1999;44:3039–3054.
Fippel M. Fast Monte Carlo dose calculation for photon beams based on the VMC electron algorithm Med Phys 1999;26:1466–1475.
Fippel M, Nüsslin F. [Determination of the human tissue interaction parameters for Monte Carlo dose calculations in radiotherapy]. Strahlenther Onkol 2001;177:206–211.
Fippel M. Efficient particle transport simulation through beam modulating devices for Monte Carlo treatment planning Med Phys 2004;31:1235–1242.
Fotina I, Winkler P, Künzler T et al. Advanced kernel methods vs. Monte Carlo-based dose calculation for high energy photon beams. Radiother Oncol 2009;93:645–653.
Francescon P, Cora S, Chiovati P. Dose verification of an IMRT treatment planning system with the BEAM EGS4-based Monte Carlo code. Med Phys 2003;30:144–157.
Georg D, Kroupa B, Georg P et al. Inverse planning-a comparative intersystem and interpatient constraint study. Strahlenther Onkol 2006;182:473–480.
Goldner G, Dimopoulos J, Kirisits C et al. Moderate dose escalation in three-dimensional conformal localized prostate cancer radiotherapy: single-institutional experience in 398 patients comparing 66 Gy versus 70 Gy versus 74 Gy. Strahlenther Onkol 2009;185:438–445.
Haedinger U, Krieger T, Flentje M et al. Influence of calculation model on dose distribution in stereotactic radiotherapy for pulmonary targets. Int J Radiat Oncol Biol Phys 2005;61:239–249.
Haryanto F, Fippel M, Bakai A et al. Study on the tongue and groove effect of the Elekta multileaf collimator using Monte Carlo simulation and film dosimetry. Strahlenther Onkol 2004;180:57–61.
Hasenbalg F, Neuenschwander H, Mini R et al. Collapsed cone convolution and analytical anisotropic algorithm dose calculations compared to VMC++ Monte Carlo simulations in clinical cases. Phys Med Biol 2007;52:3679–3691.
Knöös T, Nilsson M, Ahlgren L. A method for conversion of Hounsfield number to electron density and prediction of macroscopic pair production cross-sections. Radiother Oncol 1986;5:337–345.
Knöös T, Wieslander E, Cozzi L et al. Comparison of dose calculation algorithms for treatment planning in external photon beam therapy for clinical situations. Phys Med Biol 2006;51:5785–5807.
Koelbl O, Krieger T, Haedinger U et al. Influence of calculation algorithm on dose distribution in irradiation of non-small cell lung cancer (NSCLC) collapsed cone versus pencil beam. Strahlenther Onkol 2004;180:783–788.
Krieger T, Sauer OA. Monte Carlo- versus pencil-beam-/collapsed-cone-dose calculation in a heterogeneous multi-layer phantom. Phys Med Biol 2005;50:859–868.
Künzler T, Fotina I, Stock M et al. Experimental verification of a commercial Monte Carlo-based dose calculation module for high-energy photon beams. Phys Med Biol 2009;54:7363–7377.
Low DA, Dempsey JF. Evaluation of the gamma dose distribution comparison method. Med Phys 2003;30:2455–2464.
Mihaylov IB, Siebers JV. Evaluation of dose prediction errors and optimization convergence errors of deliverable-based head-and-neck IMRT plans computed with a superposition/convolution dose algorithm. Med Phys 2008;35:3722–3727.
Paddick I. A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg 2000;93(Suppl 3):219–222.
Paelinck L, Smedt BD, Reynaert N et al. Comparison of dose-volume histograms of IMRT treatment plans for ethmoid sinus cancer computed by advanced treatment planning systems including Monte Carlo. Radiother Oncol 2006;81:250–256.
Polednik M, Abo Madyan Y, Schneider F et al. Evaluation of calculation algorithms implemented in different commercial planning systems on an anthropomorphic breast phantom using film dosimetry. Strahlenther Onkol 2007;183:667–672.
Skrzyński W, Zielińska-Dabrowska S, Wachowicz M et al. Computed tomography as a source of electron density information for radiation treatment planning. Strahlenther Onkol 2010;186:327–333.
Stock M, Dörr W, Stromberger C et al. Investigations on parotid gland recovery after IMRT in head and neck tumor patients. Strahlenther Onkol 2010;186:665–671.
Stock M, Kroupa B, Georg D. Interpretation and evaluation of the gamma index and the gamma index angle for the verification of IMRT hybrid plans. Phys Med Biol 2005;50:399–411.
Treutwein M, Hipp M, Kölbl O et al. IMRT of prostate cancer: a comparison of fluence optimization with sequential segmentation and direct step-and-shoot optimization. Strahlenther Onkol 2009;185:379–383.
Vanderstraeten B, Reynaert N, Paelinck L et al. Accuracy of patient dose calculation for lung IMRT: a comparison of Monte Carlo, convolution/superposition, and pencil beam computations. Med Phys 2006;33:3149–3158.
Wiezorek T, Schwahofer A, Schubert K. The influence of different IMRT techniques on the peripheral dose: a comparison between sMLM-IMRT and helical tomotherapy. Strahlenther Onkol 2009;185:696–702.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uhl, M., Sterzing, F., Habl, G. et al. CT-Myelography for High-Dose Irradiation of Spinal and Paraspinal Tumors with Helical Tomotherapy. Strahlenther Onkol 187, 416–420 (2011). https://doi.org/10.1007/s00066-011-2219-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-011-2219-5