Purpose:
In recent years, the role of intensity-modulated radiotherapy (IMRT) for head and neck irradiation has increased. The main motivation is sparing the parotid gland and reduction of xerostomia. Generally, relative parotid volumes have been evaluated for treatment outcome and planning constraints, neglecting that absolute parotid volumes can vary significantly. The aim of the present study was to investigate changes in parotid gland function and set this in relation to absolute volumes.
Material and Methods:
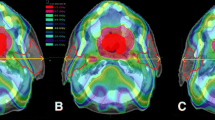
: 46 head and neck patients were treated by sparing at least the contralateral parotid gland. The mean dose to the contralateral gland was limited to 26 Gy. Parotid function was measured with scintigraphy before and at 3, 6, 9, and 12 months after radiotherapy. Gland recovery was correlated with absolute parotid gland volumes and mean dose. Finally the dose–effect relationship was investigated.
Results:
The dose–volume histograms (DVHs) for the ipsi- and contralateral glands were significantly different. A correlation between absolute volumes receiving certain doses and the function loss after 3, 6, 9, and 12 months was found. The most significant correlation was found for the absolute volume that received at least 40 Gy (aV40). ED50 values of 23–38 Gy were observed for more than 50% function loss and and 52–68 Gy afor more than 75% function loss.
Conclusion:
The mean dose, aV40 or aV26, revealed similar correlations with the excretion rate and with recovery. Hence, also absolute volumes can be used for treatment planning. Longer recovery times show higher ED50 values indicating partial regeneration of gland functions.
Ziel:
In den letzten Jahren gewann die Intensitätsmodulierte Strahlentherapie (IMRT) bei der Behandlung von Kopf-Hals Tumoren immer mehr an Bedeutung. Hauptbeweggrund dafür ist die mögliche Schonung der Ohrspeicheldrüse und somit eine Reduktion von Xerostomie. Bisher wurden hauptsächlich relative Parotisvolumina für die Korrelation mit dem Behandlungserfolg und zur Schwellwertvorgabe in der Bestrahlungsplanung verwendet. Vernachlässigt wurde jedoch dabei eine signifikante Variabilität der absoluten Parotisvolumina. Ziel dieser Studie war es deshalb, Funktionsveränderungen zu quantifizieren und mit absoluten Volumina zu korrelieren.
Material und Methoden:
46 Kopf-Hals Patienten wurden mit IMRT behandelt und dabei wurde die kontralaterale Parotis geschont. Deren mittlere Dosis wurde dabei auf 26 Gy limitiert. Die Speicheldrüsenfunktion wurde mittels Szintigraphie vor sowie 3, 6, 9 und 12 Monate nach der Therapie erfasst. Das Erholungsverhalten wurde zu den absoluten Volumina und mittleren Dosen in Korrelation gesetzt. Abschließend wurde die Dosis-Wirkungs Beziehung untersucht.
Ergebnisse:
DVHs für ipsi- and contralaterale Parotis unterschieden sich signifikant. Korrelationen zeigten sich zwischen absoluten Volumina und Funktionsveränderungen nach 3, 6, 9 und 12 Monaten. Korrelation mit der höchsten Signifikanz erwies sich beim Volumen welches mehr als 40 Gy erhalten hatte (aV40). ED50 Werte von 23–38 Gy und 52–68 Gy wurden für mehr als 50 bzw. 75% Funktionsverlust beobachtet.
Schlussfolgerung:
Die mittlere Dosis wie auch aV40 oder aV26 führen zu denselben Korrelationen mit der Funktionsveränderung der Parotis. Somit können auch absolute Volumina bei der Planungsvorgabe verwendet werden. Längere Zeitabstände zur Therapie ergaben auch höhere ED50 Werte, was auf eine partielle Regeneration der Speicheldrüse schließen lässt.
Similar content being viewed by others
References
Barker JL, Garden AS, Ang KK, et al. Quantification of volumetric and geometric changes occurring during fractionated radiotherapy for head-andneck cancer using an integrated CT/linear accelerator system. Int J Radiat Oncol Biol Phys 2004;59:960–70.
Beer KT, Zehnder D, Lussi A, Greiner RH. Sparing of contralateral major salivary glands has a significant effect on oral health in patients treated with radical radiotherapy of head and neck tumors. Strahlenther Onkol 2002;178:722–6.
Bohuslavizki KH, Brenner W, Klutmann S, et al. Implementation and indications for quantitative sialoscintigraphy. Laryngorhinootologie 1997;76: 614–24.
Bussels B, Maes A, Flamen P, et al. Dose-response relationships within the parotid gland after radiotherapy for head and neck cancer. Radiother Oncol 2004;73:297–306.
Chao KS, Deasy JO, Markman J, et al. A prospective study of salivary function sparing in patients with head-and-neck cancers receiving intensitymodulated or three-dimensional radiation therapy: initial results. Int J Radiat Oncol Biol Phys 2001;49(4):907–16.
Cooper JS, Fu K, Marks J, et al. Late effects of radiation therapy in the head and neck region. Int J Radiat Oncol Biol Phys 1995;31:1141–1164.
Deasy JO, Moiseenko V, Marks L, et al. Radiotherapy dose-volume effects on salivary gland function. Int J Radiat Oncol Biol Phys 2010;76(Suppl): S58–S64.
Delana A, Menegotti L, Bolner A, et al. Impact of residual setup error on parotid gland dose in intensity-modulated radiation therapy with or without planning organ-at-risk margin. Strahlenther Onkol 2009;185:453–9.
Eisbruch A, Ship JA, Dawson LA, et al. Salivary gland sparing and improved target irradiation by conformal and intensity modulated irradiation of head and neck cancer. World J Surg 2003;27:832–7.
Eisbruch A, Ten Haken RK, Kim HM, et al. Dose, volume, and function relationships in parotid salivary glands following conformal and intensitymodulated irradiation of head and neck cancer. Int J Radiat Oncol Biol Phys 1999;45:577–87.
Georg D, Bogner J, Dieckmann K, Pötter R. Is mask-based stereotactic headand- neck fixation as precise as stereotactic head fixation for precision radiotherapy? Int J Radiat Oncol Biol Phys 2006;66(4 Suppl):561–566.
Georg D, Georg P, Hillbrand M, et al. Assessment of improved organ at risk sparing for advanced cervix carcinoma utilizing precision radiotherapy techniques. Strahlenther Onkol 2008;184:586–91.
Georg D, Kroupa B, Georg P, et al. Inverse planning–a comparative intersystem and interpatient constraint study. Strahlenther Onkol 2006; 182:473–80.
Gregoire V, Levendag P, Ang KK, et al. CT-based delineation of lymph node levels and related CTVs in the node-negative neck: DAHANCA, EORTC, GORTEC, NCIC,RTOG consensus guidelines. Radiother Oncol 2003; 69:227–36.
Guerrero Urbano MT, Clark CH, Kong C, et al. Target volume definition for head and neck intensity modulated radiotherapy: pre-clinical evaluation of PARSPORT trial guidelines. Clin Oncol (R Coll Radiol) 2007;19:604–13
Hey J, Setz J, Gerlach R, et al. Parotid-gland-sparing 3D conformal radiotherapy in patients with bilateral radiotherapy of the head and neck region – results in clinical practice. Oral Oncol 2009;45:e11–7.
Hsiung CY, Ting HM, Huang HY, et al. Parotid-sparing intensity-modulated radiotherapy (IMRT) for nasopharyngeal carcinoma: Preserved parotid function after IMRT on quantitative salivary scintigraphy, and comparison with historical data after conventional radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:454–461.
Kuhnt T, Janich M, Götz U, et al. Presentation of a 3D conformal radiotherapy technique for head-and-neck tumors resulting in substantial protection of the parotid glands. Strahlenther Onkol 2006;182(6):325–30.
Kuhnt T, Jirsak N, Müller AC, et al. Quantitative and qualitative investigations of salivary gland function in dependence on irradiation dose and volume for reduction of xerostomia in patients with head-and-neck cancer. Strahlenther Onkol 2005;181:520–8.
Kwong DL, Pow EH, Sham JS, et al. Intensity-modulated radiotherapy for early-stage nasopharyngeal carcinoma: a prospective study on disease control and preservation of salivary function. Cancer 2004;101:1584–93.
Lee C, Langen KM, Lu W, et al. Evaluation of geometric changes of parotid glands during head and neck cancer radiotherapy using daily MVCT and automatic deformable registration. Radiother Oncol 2008;89:81–88.
Li C, Taylor JMG, Ten Haken RK, et al. The impact of dose on parotid salivary recovery in head and neck cancer patients treated with radiation therapy. Int J Radiat Oncol Biol Phys 2007;67:660–9.
Lin KK, Pajak TF, Trotti A, et al. A Radiation Therapy Oncology Group (RTOG) phase III randomized study to compare hyperfractionation and two variants of accelerated fractionation to standard fractionation radiotherapy for head and neck squamous cell carcinomas: first report of RTOG 9003. Int J Radiat Oncol Biol Phys 2000;48:7–16.
Marzi S, Iaccarino G, Pasciuti K, et al. Analysis of salivary flow and dosevolume modeling of complication incidence in patients with head-and-neck cancer receiving intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2009;73:1252–9.
Münter MW, Karger CP, Hoffner SG, et al. Evaluation of salivary gland function after treatment of head-and-neck tumors with intensity-modulated radiotherapy by quantitative pertechnetate scintigraphy. Int J Radiat Oncol Biol Phys 2004;58:175–84.
Nutting C, A´Hern R, Rogers MS, et al. First results of a phase III multicenter randomized controlled trial of intensity modulated (IMRT) versus conventional radiotherapy (RT) in head and neck cancer (PARSPORT: ISRCTN48243537; CRUK/03/005). J Clin Oncol 2009;27(suppl):18s (abstr LBA6006).
Ortholan C, Chamorey E, Benezery K, et al. Modeling of salivary production recovery after radiotherapy using mixed models: Determination of optimal dose constraint for IMRT planning and construction of convenient tools to predict salivary function. Int J Radiat Oncol Biol Phys 2009;73:178–86.
Pacholke HD, Amdur RJ, Morris CG, et al. Late xerostomia after intensitymodulated radiation therapy versus conventional radiotherapy. Am J Clin Oncol 2005;28:351–8.
Pow EHN, Kwong DLW, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys 2001;66:981–91.
Rades D, Stoehr M, Meyners T, et al. Evaluation of prognostic factors and two radiation techniques in patients treated with surgery followed by radio(chemo)therapy or definitive radio(chemo)therapy for locally advanced head-and-neck cancer. Strahlenther Onkol 2008;184:198–205.
Roesink JM, Moerland MA, Hoekstra A, et al. Scintigraphic assessment of early and late parotid gland function after radiotherapy for head-and-neck cancer: A prospective study of dose-volume response relationships. Int J Radiat Oncol Biol Phys 2004;58:1451–60.
SAS Institute Inc., Cary, NC, SAS/STAT Users Guide Version 6. 1990.
Voordeckers M, Everaert H, Tournel K, et al. Longitudinal assessment of parotid function in patients receiving tomotherapy for head-and-neck cancer. Strahlenther Onkol 2008;184:400–5.
Wiggenraad R, Mast M, van Santvoort J, et al. ConPas: a 3-D conformal parotid gland-sparing irradiation technique for bilateral neck treatment as an alternative to IMRT. Strahlenther Onkol 2005;181:673–82.
Wilkens JJ, Alaly JR, Zakarian K, et al. IMRT treatment planning based on prioritizing prescription goals. Phys Med Biol 2007;52:1675–92.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stock, M., Dörr, W., Stromberger, C. et al. Investigations on Parotid Gland Recovery after IMRT in Head and Neck Tumor Patients. Strahlenther Onkol 186, 665–671 (2010). https://doi.org/10.1007/s00066-010-2157-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2157-7