Abstract
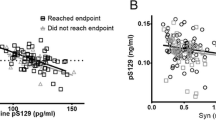
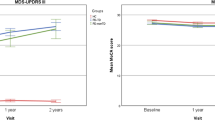
The development of biomarkers to predict the progression of Parkinson’s disease (PD) from its earliest stage through its heterogeneous course is critical for research and therapeutic development. The Parkinson’s Progression Markers Initiative (PPMI) study is an ongoing international multicenter, prospective study to validate biomarkers in drug-naïve PD patients and matched healthy controls (HC). We quantified cerebrospinal fluid (CSF) alpha-synuclein (α-syn), amyloid-beta1-42 (Aβ1-42), total tau (t-tau), and tau phosphorylated at Thr181 (p-tau) in 660 PPMI subjects at baseline, and correlated these data with measures of the clinical features of these subjects. We found that CSF α-syn, t-tau and p-tau levels, but not Aβ1-42, were significantly lower in PD compared with HC, while the diagnostic value of the individual CSF biomarkers for PD diagnosis was limited due to large overlap. The level of α-syn, but not other biomarkers, was significantly lower in PD patients with non-tremor-dominant phenotype compared with tremor-dominant phenotype. In addition, in PD patients the lowest Aβ1-42, or highest t-tau/Aβ1-42 and t-tau/α-syn quintile in PD patients were associated with more severe non-motor dysfunction compared with the highest or lowest quintiles, respectively. In a multivariate regression model, lower α-syn was significantly associated with worse cognitive test performance. APOE ε4 genotype was associated with lower levels of Aβ1-42, but neither with PD diagnosis nor cognition. Our data suggest that the measurement of CSF biomarkers in early-stage PD patients may relate to disease heterogeneity seen in PD. Longitudinal observations in PPMI subjects are needed to define their prognostic performance.


Similar content being viewed by others
References
Aarsland D, Andersen K, Larsen JP et al (2003) Prevalence and characteristics of dementia in Parkinson disease: an 8-year prospective study. Arch Neurol 60:387–392
Aarsland D, Kurz MW (2010) The epidemiology of dementia associated with Parkinson disease. J Neurol Sci 289:18–22
Alves G, Larsen JP, Emre M et al (2006) Changes in motor subtype and risk for incident dementia in Parkinson’s disease. Mov Disord 21:1123–1130
Alves G, Brønnick K, Aarsland D et al (2010) CSF amyloid-beta and tau proteins, and cognitive performance, in early and untreated Parkinson’s disease: the Norwegian ParkWest study. J Neurol Neurosurg Psychiatry 81:1080–1086
Alves G, Lange J, Blennow K et al (2014) CSF Aβ42 predicts early-onset dementia in Parkinson disease. Neurology 82:1784–1790
Compta Y, Parkkinen L, O’Sullivan SS et al (2011) Lewy- and Alzheimer-type pathologies in Parkinson’s disease dementia: which is more important? Brain 134:1493–1505
Duka T, Duka V, Joyce JN, Sidhu A (2009) α-Synuclein contributes to GSK-3β-catalyzed tau phosphorylation in Parkinson’s disease model. FASEB J 23:2820–2830
Giasson BI, Forman MS, Higuchi M et al (2003) Initiation and synergistic fibrillization of tau and alpha-synuclein. Science 300:636–640
Gomperts SN, Locascio JJ, Rentz D et al (2013) Amyloid is linked to cognitive decline in patients with Parkinson disease without dementia. Neurology 80:85–91
Guo JL, Covell DJ, Daniels JP et al (2013) Distinct α-synuclein strains differentially promote tau inclusions in neurons. Cell 154:103–117
Halliday GM, Holton JL, Revesz T, Dickson DW (2011) Neuropathology underlying clinical variability in patients with synucleinopathies. Acta Neuropathol 122:187–204
Hobson P, Meara J (2004) Risk and incidence of dementia in a cohort of older subjects with Parkinson’s disease in the United Kingdom. Mov Disord 19:1043–1049
Hughes TA, Ross HF, Musa S et al (2000) A 10-year study of the incidence of and factors predicting dementia in Parkinson’s disease. Neurology 54:1596–1602
Irwin DJ, White MT, Toledo JB et al (2012) Neuropathologic substrates of Parkinson disease dementia. Ann Neurol 72:587–598
Irwin DJ, Lee VM, Trojanowski JQ (2013) Parkinson’s disease dementia: convergence of α-synuclein, tau and amyloid-β pathologies. Nat Rev Neurosci 14:626–636
Jankovic J, McDermott M, Carter J et al (1990) Variable expression of Parkinson’s disease: a base-line analysis of the DATATOP cohort. Neurology 40:1529–1534
Jellinger KA (1999) Post mortem studies in Parkinson’s disease-is it possible to detect brain areas for specific symptoms? J Neural Transm Suppl 56:1–29
Kang JH, Irwin DJ, Chen-Plotkin AS et al (2013) Association of cerebrospinal fluid β-amyloid 1-42, t-tau, p-tau181, and α-synuclein levels with clinical features of drug-naïve patients with early Parkinson disease. JAMA Neurol 70:1277–1287
Levy G, Tang MX, Louis ED et al (2002) The association of incident dementia with mortality in PD. Neurology 59:1708–1713
Lewis SJG, Foltynie T, Blackwell AD et al (2005) Heterogeneity of Parkinson’s disease in the early clinical stages using a data driven approach. J Neurol Neurosurg Psychiatry 76:343–348
Mata IF, Leverenz JB, Weintraub D et al (2014) APOE, MAPT, and SNCA genes and cognitive performance in Parkinson disease. JAMA Neurol 71:1405–1412
Mollenhauer B, Locascio JJ, Schulz-Schaeffer W et al (2011) α-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: a cohort study. Lancet Neurol 10:230–240
Montine TJ, Shi M, Quinn JF et al (2010) CSF Aβ42 and tau in Parkinson’s disease with cognitive impairment. Mov Disord 25:2682–2685
Nalls MA, Pankratz N, Lill CM et al (2014) Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat Genet 46:989–993
Parashos SA, Swearingen CJ, Biglan KM et al (2009) Determinants of the timing of symptomatic treatment in early Parkinson disease: the National Institutes of Health Exploratory Trials in Parkinson Disease (NET-PD) Experience. Arch Neurol 66:1099–1104
Parashos SA, Luo S, Biglan KM et al (2014) Measuring disease progression in early Parkinson disease: the National Institutes of Health Exploratory Trials in Parkinson Disease (NET-PD) Experience. JAMA Neurol 71:710–716
Initiative Parkinson Progression Marker (2011) The Parkinson Progression Marker Initiative (PPMI). Prog Neurobiol 95:629–635
Parnetti L, Tiraboschi P, Lanari A et al (2008) Cerebrospinal fluid biomarkers in Parkinson’s disease with dementia and dementia with Lewy bodies. Biol Psychiatry 64:850–855
Parnetti L, Chiasserini D, Bellomo G et al (2011) Cerebrospinal fluid tau/α-synuclein ratio in Parkinson’s disease and degenerative dementia. Mov Disord 8:1428–1435
Paulus W, Jellinger K (1991) The neuropathologic basis of different clinical subgroups of Parkinson’s disease. J Neuropathol Exp Neurol 50:743–755
Rajput AH, Sitte HH, Rajput A et al (2008) Globus pallidus dopamine and Parkinson motor subtype: clinical and brain biochemical correlation. Neurology 70:1403–1410
Rajput AH, Voll A, Rajput ML et al (2009) Course in Parkinson disease subtypes: a 39-year clinicopathologic study. Neurology 73:206–212
Selikhova M, Williams DR, Kempster PA et al (2009) A clinico-pathological study of subtypes in Parkinson’s disease. Brain 132:2947–2957
Shi M, Bradner J, Hancock AM et al (2011) Cerebrospinal fluid biomarkers for Parkinson disease diagnosis and progression. Ann Neurol 69:570–580
Siderowf A, Xie SX, Hurtig H et al (2010) CSF amyloid β1-42 predicts cognitive decline in Parkinson disease. Neurology 75:1055–1061
Stebbins GT, Goetz CG, Burn DJ et al (2013) How to identify tremor dominant and postural instability/gait difficulty groups with the Movement Disorder Society Unified Parkinson’s Disease Rating Scale: comparison with the Unified Parkinson’s Disease Rating Scale. Mov Disord 28:668–670
Toledo JB, Korff A, Shaw LM et al (2013) CSF α-synuclein improves diagnostic and prognostic performance of CSF tau and Aβ in Alzheimer’s disease. Acta Neuropathol 126:683–697
Toledo JB, Gopal P, Raible K et al (2015) Pathological a-synuclein distribution in subjects with coincident Alzheimer’s and Lewy body pathology. Acta Neuropathol (E-pub)
Tsuang D, Leverenz JB, Lopez OL et al (2013) APOE e4 increases risk for dementia in pure synucleinopathies. JAMA Neurol 70:223–228
van de Berg WD, Hepp DH, Dijkstra AA et al (2012) Patterns of α-synuclein pathology in incidental cases and clinical subtypes of Parkinson’s disease. Parkinsonism Relat Disord 18(Suppl 1):S28–S30
Williams-Gray CH, Foltynie T, Brayne CEG et al (2007) Evolution of cognitive dysfunction in an incident Parkinson’s disease cohort. Brain 130:1787–1798
Williams-Gray CH, Goris A, Saiki M et al (2009) Apolipoprotein E genotype as a risk factor for susceptibility to and dementia in Parkinson’s disease. J Neurol 256:493–498
Wills J, Jones J, Haggerty T et al (2010) Elevated tauopathy and alpha-synuclein pathology in postmortem Parkinson’s disease brains with and without dementia. Exp Neurol 225:210–218
Acknowledgments
The Parkinson’s Progression Markers Initiative Group includes Shirley Lasch; Emily Flagg; Werner Poewe, MD; Todd Sherer, PhD; Claire Meunier; Alice Rudolph, PhD; Cindy Casaceli, MBA; John Seibyl, MD; Susan Mendick, MPH; Norbert Schuff, PhD; Liz Uribe, MS; Jon Yankey, MS; Karen Crawford; Tatiana Foroud, PhD; Paola Casalin, MD, PhD, FRCP; Giulia Malferrari, PhD; Keith Hawkins, PsyD; David Russell, MD, PhD; Laura Leary, BS; Stewart Factor, DO; Barbara Sommerfeld, RN, MSN; Penelope Hogarth, MD; Emily Pighetti; Karen Williams; David Standaert, MD, PhD; Stephanie Guthrie, MSN; Robert Hauser, MD, MBA; Joseph Jankovic, MD; Christine Hunter, RN; Matthew Stern, MD; Abigail Darin; Jim Leverenz, MD; Marne Baca; Sam Frank, MD; Cathi-Ann Thomas, RN, MS; Irene Richard, MD; Cheryl Deeley, MSN; Linda Rees, MPH; Fabienne Sprenger, MD; Wolfgang Oertel, MD; Diana Willeke; Holly Shill, MD; Hubert Fernandez, MD; Jennifer Mule; Daniela Berg, MD; Katharina Gauss; Douglas Galasko, MD; Deborah Fontaine, BSN, MS; Zoltan Mari, MD; Arita McCoy, RN; David Brooks, MD; Bina Shah, BSc; Paolo Barone, MD, PhD; Stuart Isaacson, MD; Angela James; Alberto Espay, MD, MSc; Kristy Espay; Dominic Rowe, MD, PhD; Madelaine Ranola, BN.
The Parkinson’s Progression Markers Initiative Group Affiliations Institute for Neurodegenerative Disorders, New Haven, Connecticut (Lasch, Seibyl, Mendick, Russell, Leary); Clinical Trials Coordination Center, University of Rochester, Rochester, New York (Flagg, Casaceli); Innsbruck Medical University, Innsbruck, Austria (Poewe, Sprenger); The Michael J. Fox Foundation for Parkinson’s Research, New York, New York (Sherer, Meunier); Institute on Aging, Center for Neurodegenerative Disease Research, Perelman School of Medicine, University of Pennsylvania, Philadelphia (Rudolph); University of California, San Francisco (Schuff); University of Iowa, Iowa City (Uribe, Yankey); Laboratory of Neuro Imaging, Department of Neurology, David Geffen School of Medicine, University of California, Los Angeles (Crawford); Coriell Institute for Medical Research, Camden, New Jersey (Scutti); BioRep, Milan, Italy (Casalin, Malferrari); Yale University, New Haven, Connecticut (Hawkins); Emory University School of Medicine, Atlanta, Georgia (Factor, Sommerfeld); Oregon Health and Science University, Portland (Hogarth, Pighetti); Northwestern University, Chicago, Illinois (Williams); University of Alabama at Birmingham (Standaert, Guthrie); Baylor College of Medicine, Houston, Texas (Hauser, Jankovic, Hunter); University of Pennsylvania, Philadelphia (Stern, Darin); University of Washington, Seattle (Leverenz, Baca); Boston University, Boston, Massachusetts (Frank, Thomas); University of Rochester, Rochester, New York (Richard, Deeley); Parkinson’s Institute, Sunnyvale, California (Rees); Paracelsus-Elena-Klinik, Kassel, Germany (Oertel, Willeke); Cleveland Clinic, Cleveland, Ohio (Shill, Fernandez, Mule); University of Tuebingen, Tuebingen, Germany (Berg, Gauss); University of California, San Diego (Galasko, Fontaine); Johns Hopkins University, Baltimore, Maryland (Mari, McCoy); Imperial College London, London, England (Brooks, Shah); University of Salerno, Salerno, Italy (Barone); Parkinson’s Disease and Movement Disorders Center of Boca Raton, Boca Raton, Florida (Isaacson, James); University of Cincinnati, Cincinnati, Ohio (A. Espay, K. Espay); Macquarie University, Sydney, Australia (Rowe, Ranola).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Frasier is an employee of The Michael J. Fox Foundation for Parkinson’s Research. Marek has been a consultant for Pfizer Inc, GE Healthcare, Merck and Co, Eli Lilly and Co, Bristol-Myers Squibb, Piramal, Neotope Biosciences, and Neuro Phage Pharmaceuticals and has equity interest in Molecular NeuroImaging. Kieburtz has been a consultant for the National Institute of Neurological Disorders and Stroke, National Institutes of Health, US Food and Drug Administration, Veterans Affairs, Abbott, Acorda, Aptiv, Astra-Zeneca, Auspex, BiogenIdec, Biotie, Biovail, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Ceregene, CHDI, Civitas, Clintrex, Cynapsus, Eli Lilly and Co, Endo, Impax, Intec, Ipsen, Isis, Knopp, Lundbeck, LZ Therapeutics, Medivation, Merck and Co, Merz, Neotope/Elan, Novartis, Orion, Otsuka, Pharma2B, Phytopharm, Roche, Siena Biotech, Sofinnova, Synagile, Synosia, Teva, UCB Pharma, Upsher-Smith, US World Meds, Vaccinex, Vectura, and Xenoport; and has performed legal consulting for Thompson Hine. Tanner has served on the scientific advisory boards of The Michael J. Fox Foundation for Parkinson’s Research and the National Spasmodic Dystonia Association; has been a consultant for Impax Pharmaceuticals and Adamas Pharmaceuticals; and is an employee of the Parkinson’s Institute and Clinical Center. Chowdhury is an employee of The Michael J. Fox Foundation for Parkinson’s Research. Shaw was previously a consultant for Fujirebio and collaborates on quality assessment activities as part of the Parkinson’s Progression Markers Initiative and as part of the Alzheimer’s Disease Neuroimaging Initiative. Leverenz has received compensation for consultation from Bayer Pharmaceuticals, Navidea Biopharmaceuticals, and Piramal Healthcare. Galasko serves as editor of Alzheimer’s Disease Research and Treatment; serves on data safety monitoring boards for Elan, Janssen, and Balance Pharmaceuticals; and is a consultant for Elan Pharmaceuticals; No other disclosures were reported.
Funding/Support
This work was supported by The Michael J. Fox Foundation for Parkinson’s Research, Abbott, Avid Radiopharmaceuticals, BiogenIdec, Covance, Elan, Eli Lilly and Co, F. Hoffman–LaRoche Ltd, GE Healthcare, Genentech, Glaxo Smith Kline, Merck and Co, Pfizer Inc, and UCB Pharma SA. Trojanowski and Chen-Plotkin were supported by core grant P50NS053488-05 from the Morris K. Udall Center of Excellence for Parkinson’s Disease Research. Irwin was supported by Training in Age-Related Neurodegenerative Diseases grant T32-AG000255 from the National Institute on Aging, National Institutes of Health. Singleton was supported by Grant Z01AG000949-06 from the Intramural Research Program, National Institute on Aging, National Institutes of Health. Ju-Hee was supported by Grant MRC 2014009392 from the National Research Foundation of Korea, Ministry of Science, ICT and Future Planning. Kieburtz has received grants and/or research support from the National Eye Institute, National Institute of Neurological Disorders and Stroke, National Institute on Aging, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Neurosearch, and Medication. Tanner has received grants and/or research support from Brin Foundation, James and Sharron Clark, Parkinson’s Institute and Clinical Center, Parkinson’s Disease Foundation, US Army Medical Research Acquisition Activity (Telemedicine and Advanced Technology Research Center—managed Neurotoxin Exposure Treatment Research Program), National Institute of Neurological Disorders and Stroke, Agency for Healthcare and Research Quality, and National Institute of Environmental Health Sciences. Galasko receives research support from the National Institutes of Health, and the Alzheimer’s Drug Discovery Foundation.
Additional information
The members of the Parkinson’s Progression Markers Initiative are listed in “Acknowledgments”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kang, JH., Mollenhauer, B., Coffey, C.S. et al. CSF biomarkers associated with disease heterogeneity in early Parkinson’s disease: the Parkinson’s Progression Markers Initiative study. Acta Neuropathol 131, 935–949 (2016). https://doi.org/10.1007/s00401-016-1552-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-016-1552-2