Abstract
Background
Uterine fibroids are the most common benign tumor of the reproductive tract in women. Uterine artery embolization has been approved as an alternative treatment option for uterine fibroids to reduce uterine and fibroid volumes as well as to relieve the patient symptoms. The current study included 80 patients with symptomatic uterine fibroids. All patients underwent pre-embolization MRI, uterine artery embolization, and follow-up post-embolization MRI at 6 months post procedure for a reduction in uterine and dominant fibroid volumes. The aim of the study was to assess the role of transcatheter uterine artery embolization in reducing the uterine fibroid volume.
Results
There was a significant difference in the uterine volume reduction between a group with single fibroids and a group with multiple uterine fibroids The mean uterine volume reduction in the first group was 46.5% compared to 37.4% reduction in the second group. While there was no significant difference in the dominant fibroid volume reduction between both groups (48.8% and 44.9% respectively).
Conclusions
UAE has a high efficacy in the reduction of both the uterine volume and the dominant fibroid volume, which results in improvement in patient’s quality of life.
Similar content being viewed by others
Background
Uterine fibroids (UF) are the commonest benign tumor in women of reproductive age [1]. Fibroids may vary in size from a few millimeters to large sizes (over 10 cm) and can be classified into single or multiple uterine fibroids [2].
Uterine artery embolization (UAE) is an interventional radiological (IR) technique to occlude the arterial supply to the uterus for various reasons [3].
The technique was first reported as an effective technique for the treatment of uterine fibroids in 1995, when it was noted that women with symptomatic fibroids who underwent UAE as a pre-hysterectomy treatment had significant clinical improvement to the extent that hysterectomy was no longer required [4].
UAE has proved to be an effective treatment for symptomatic fibroids and it is now considered as an alternative to myomectomy and hysterectomy [5, 6]. Standard imaging protocols for UAE are the pre-procedural assessment by magnetic resonance imaging (MRI) followed by a post-procedural MRI 3–6 months later [7, 8].
Embolization procedures are performed with 4F RIM catheter, microcatheters, and a variety of embolic agents. One of the decisions that an operator must make before performing a uterine artery embolization procedure is which embolic agent to use. Originally, irregularly shaped polyvinyl alcohol (PVA) particles were used, although more recently other spherical-shaped embolic agents have been developed [9, 10].
Infarction of a fibroid is indicated by the absence of contrast enhancement in follow-up T1-weighted MR images in comparison to pre-embolization MRI images. The degree of infarction is expressed by using a scale from 0 to 100% infarction, where 100% is complete infarction and 0% is non-infarction [11].
Persistent symptoms after UFE can be due to incomplete fibroid infarction, and the subsequent regrowth of an incompletely treated fibroid contributes to earlier symptom recurrence [12].
Methods
Eighty female patients were referred for UAE for symptomatic fibroids. UAE for fibroids was decided after discussion of treatment options in a fibroid multidisciplinary team meeting. Exclusion criteria were a positive pregnancy test, uterine or adnexal infection, suspected gynecologic malignancy, patients with renal impairment, and hypersensitivity to contrast media.
Patients were examined in both gynecology and IR clinics with a full detailed history, including the menstrual history, duration and amount of bleeding, and full laboratory investigations. Informed consent was obtained from all patients and patient information leaflets were given to them during the clinic visit.
Pre and post procedure pelvic MRI
Pelvic MRI was performed using a GE Signa Excite (GE Medical Systems, USA) 1.5 Tesla MRI scanner. Pre- and post-interventional MRIs were performed according to standard identical protocols.
The MRI sequences used in the study were sagittal T2 fast spin echo (FSE), axial T2 FSE, axial T1 FSE, and post contrast axial T1 fat-saturated imaging. Assessment criteria were the site and number of fibroids, the calculation of pre and post embolization uterine and dominant fibroid volumes, and the estimation of the percentage of dominant fibroid infarction on the post embolization MRI scans.
Clinical symptomatic improvement was assessed with by calculation of symptom severity score and a health-related quality of life questionnaire (HR-QOL) before and 6 months after UAE.
Technique of uterine artery embolization
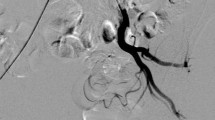
The procedure was done under fluoroscopic guidance using a Siemens Artis-Q Angiography machine with a ceiling mounted system. The machine is capable of serial radiography and digital subtraction. Non-ionic contrast media (Omnipaque 300) was used in all patients (Figs. 1 and 2).
Forty year-old-female patient. a Sagittal T2-weighted MR image shows a single large intramural fibroid. b A baseline MRI scan shows intense enhancement of the fibroid. c Uterine arteriograms before embolization: Fluoroscopic image obtained in the arterial phase shows bilateral hypertrophied uterine arteries with a large fibroid uterus due to uterine fibroids. d Sagittal T2-weighted MRI 6 months following uterine artery embolization demonstrates a reduction in the uterine and fibroid volume. e Post embolization T1-weighted MR image shows 100% infarction with decreased fibroid volume
Thirty-five year-old-female patient. a Sagittal T2-weighted MR image demonstrates multiple variably sized uterine fibroids. b Baseline T1-weighted fat-suppressed image shows an intense enhancement of the uterine fibroids. c Uterine angiograms before embolization: fluoroscopic image obtained in the arterial phase shows bilateral enlarged uterine arteries with an enlarged uterus due to multiple fibroids. d Post embolization T1-weighted fat-suppressed image shows 100% infarction of the dominant fibroid and decreased uterine and fibroid volumes. e MRI scan 6 months post UAE shows a reduction in the uterine and fibroid volumes
The embolization procedure was performed by certified interventional radiologists in our institution (R.M. with 30 years experience in interventional radiology, A.K. 15 years experience, and A.E. 10 years experience). Each operation was performed by two operators to decrease operative time and radiation exposure.
The patient is positioned in the supine position, and both groins are prepped with antiseptic solution. Bilateral common femoral arteries access is achieved using the Seldinger technique after infiltration of local anesthesthetic agent (10 ml lidocaine) around the femoral artery.
Then 4F Rim catheters (Rosch Inferior Mesenteric Torcon Beacon Tip catheter, Cook Medical, USA) are advanced over the aortic bifurcation over 0.035 hydrophilic guidewires (Radiofocus® Terumo) to reach the contra-lateral internal iliac artery. Catheterization of the uterine artery is then performed, and the catheter tip is placed in the transverse portion of the uterine artery. Arteriography is performed to confirm a satisfactory position.
In some patients, it was difficult to access the correct position with the Rim catheter. In these cases, a 2.7F microcatheter (Progreat 2.7F microcatheter, Terumo Medical Corporation, Europe) was used to go further to access the appropriate position. Pulsed fluoroscopy (2 pulses per second) is used to opacify the entire fibroid uterus and to decrease patient radiation dose.
Embolization is started using 355 to500 μm non-spherical polyvinyl alcohol particles (Contour PVA, Boston Scientific, USA), which are then upsized to 500 to 710 μm and 710–1000 μm.
The end point for embolization is stasis of contrast within the transverse segments of the uterine arteries for approximately 10 cardiac pulsations.
The operators usually wait for a period of 5 min to allow any remaining embolic material clumping to redistribute, and they then reconfirm adequate stasis by performing repeat angiography.
Following UAE, patient-controlled analgesia with the administration of intravenous analgesia and anti-inflammatory drugs may be used to assist in pain control in the early post procedure period.
After UAE, patients are observed overnight in the hospital to ensure adequate access to pain and anti-nausea medications and to enable observation of the femoral access site.
Merits and limitation of technique
The merits of the uterine fibroid embolization are as follows: avoidance of hysterectomy, minimally invasive technique, shorter hospital stay, and shorter recovery time. However, this technique cannot be used in patients with uterine or adnexal infections, renal impairment, and patients with known history of hypersensitivity to contrast media.
Statistical analysis
The collected data were coded, tabulated, and statistically analyzed using the SPSS program (Statistical Package for Social Sciences) software version 25.
Descriptive statistics were done for parametric quantitative data by mean, minimum, and maximum of the range, while they were done for categorical data by number and percentage.
Analyses were done for parametric quantitative data using paired samples T test.
The level of significance was taken at a P value of < 0.05.
Results
Eighty patients with uterine leiomyomata were referred to the IR department between February 2018 and October 2019. They were recruited into the study after fulfillment of the inclusion criteria; their ages ranged from 34 to 54 years old; the patients were classified into 2 groups: 21 patients in the first group (group 1) had a solitary large fibroid, and 59 patients in the second group (group 2) had multiple fibroids. Patients complained of uterine bleeding and/or pelvic pressure symptoms in the form of pelvic heaviness and urinary disturbance (as in Table 1).
There was a significant difference in the percentage of uterine volume reduction between the two groups. In group 1, the pre-embolization uterine volume was 179–3628 cm3 with a mean volume = 608.1 cm3 and total volume reduction was 46.5%. The pre-embolization total uterine volume in group 2 was 84.3–2179 cm3 with a mean volume = 872.9 cm3 and total volume reduction was 37.4% (significant difference, P = 0.01) (as shown in Table 2).
However, there was no significant difference of the volume reduction of the dominant fibroid between the 2 groups. The pre-embolization dominant fibroid volume in group 1 group ranged from 52–290 cm3 (mean = 270 cm3), and the volume reduction was 48.8%. In group 2, the pre-embolization volume ranged from 23–170 cm3 (mean = 247 cm3) and the volume reduction was 44.9% (no significant difference, P = 0.57) (as shown in Table 3).
The number of PVA vials that were used in group 1 ranged from 2–10 vials with a mean of 4.7 vials, while in group 2, the number of PVA vials that were used ranged from 2–12 vials with a mean of 5 vials.
As regarding procedural complications, expulsion of the infarcted fibroid occurred in 2 patients who presented with severe colicky pain. No major complication or puncture site hematoma was encountered.
The mean screening time was 15.68 min; the mean radiation dose was 191 mGy; and there was no significant difference in the dose area product (DAP) of 2520 μGym2, fluoroscopy time, or radiation dose between the two groups.
In group 2, failure to cannulate the left uterine artery by the RIM catheter was experienced in 5 patients and the right uterine artery in one patient with the result that microcatheters were used in these patients. In group 1, there was failure to catheterize the left uterine artery with the RIM catheter in one patient, and a microcatheter was used successfully.
In group 1, the mean symptom severity score was 65.8 before UAE and was 30.4 after UAE. The mean HR-QOL before UAE was 33.3, was 78.2 after UAE, which was not statistically significant different (P value = 0.67) from group 2. In group 2, the mean pre-UAE symptom severity score was 70.1 and was 32.8 after UAE, and the HRQOL was 40.2 and 74, respectively (Table 4).
At 6 months follow-up at the MRI unit, complete infarction of the dominant leiomyoma was achieved in 18 patients (85.7 %) in group 1, which had a statistically significant difference (P value 0.03*) compared with the group 2 in which complete infarction was achieved in 34 patients (57.6%), as listed in Table 5.
Complications in group 2 included severe pain in two patients after discharge from hospital within 1 week that required readmission and IV analgesia, complete expulsion of a dominant fibroid in one patient, and infection in two patients, which was treated by IV antibiotics and hospital readmission.
Spasm of right uterine artery was experienced in one patient with a failed embolization from that side and successful embolization of the left uterine artery. At follow-up, successful fibroid infarction was achieved.
Complications in group 1 were expulsion of the fibroid in one patient, severe pain in one patient requiring readmission, and pain control.
Discussion
UAE has become a popular treatment option for women with symptomatic fibroids who desire uterine preservation and/or the avoidance of surgical intervention [7].
Our results have demonstrated that there was a significant reduction in the uterine volume between the studied groups with total volume reduction in 46.5% and 37.4 % in group 1 and group 2, respectively (P = 0.01). However, there was no significant difference in the reduction of the dominant fibroid volume between the two groups with volume reduction of 48.8% and 44.9% in group 1 and group 2, respectively (no significant difference, P = 0.57).
Das et al.’s [9] study revealed that the dominant fibroid volume mean reduction was 50% at 6 months, while the mean uterine volume reduction was 42% at 4 months.
At 6 months MRI follow-up, complete infarction of the dominant leiomyoma was achieved in 18 patients (85.7 %) in group 1, and complete infarction was achieved in 34 patients in group 2 (57.6%). In the study of Richard et al. [13], complete dominant tumor infarction was maintained at 3 months in 82.1% of patients in the PVA UAE group.
With the use of PVA as our main embolic agent, we achieved satisfactory clinical success. In group 1, the mean symptom severity score markedly decreased from 65.8 to 30.4 after treatment, and the mean HRQOL improved from 33.3 to 78.2. While in group 2, the mean symptom severity score was 70.1 pre-procedure and 32.8 post procedure, and the HRQOL improved from 40.2 to 74.
In a study by Das et al. in 2014 [9], HR-QOL improved from 39.1 pre UAE to 76.2 post UAE, and symptom severity score decreased from 55.9 to 26.6 before and after UAE, respectively.
All patients with uterine fibroids were treated by UAE using bilateral arterial femoral artery access. The mean screening time was 15.68 min, the mean dose was 191 mGy, and the dose area product (DAP) was = 2520 μGym2 with no significant differences detected with respect to fluoroscopy time or radiation dose between the two groups.
In a study by Bratby et al. [14], elective bilateral arterial punctures were reported aiming to reduce patient irradiation by using pulsed fluoroscopy, avoidance of aortography, and simultaneous bilateral embolization.
The study results are limited by unequal number of patients in the study groups, so further study from multiple centers is recommended for better assessment.
Conclusion
UAE has high efficacy in reducing uterine volumes in the patients with a single fibroid. The results of UAE are improved in patients with single fibroids rather than multiple fibroids. UAE improved the quality of life whether patients had single or multiple fibroids.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- F:
-
French
- FSE:
-
Fast spin echo
- HR-QOL:
-
Health-related quality of life questionnaire
- IR:
-
Interventional radiology
- MRI:
-
Magnetic resonance imaging
- PVA:
-
Polyvinyl alcohol
- UAE:
-
Uterine artery embolization
References
Zimmermann A, Bernuit D, Gerlinger C et al (2012) Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC Womens Health 12:6
Donnez J, Dolmans M (2016) Uterine fibroid management: from the present to the future. Hum Reprod Update. 22(6):665–686
Deshmukh SP, Gonsalves CF, Guqlielmo FF et al (2012) Role of MR imaging of uterine leiomyomas before and after embolization. Radiographics. 32(6):E251–E281
Bulman JC, Ascher SM, Spies JB (2012) Current concepts in uterine fibroid embolization. Radiographics. 32(6):1735–1750
Dariushnia SR, Nikolic B, Stokes LS et al (2014) Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. J Vasc Interv Radiol. 25(11):1737–1747
Manyonda IT, Bratby M, Horst JS et al (2012) Uterine artery embolization versus myomectomy: impact on quality of life-results of the FUME (fibroids of the uterus: myomectomy versus embolization) trial. Cardiovasc Interv Radiol. 35(3):530–536
Siddiqui N, Nikolaidis P, Hammond N et al (2013) Uterine artery embolization: pre- and post-procedural evaluation using magnetic resonance imaging. Abdom Imaging. 38:1161–1177
Verma SK, Gonsalves CF, Baltarowich OH et al (2010) Spectrum of imaging findings on MRI and CT after uterine artery embolization. Abdom Imaging. 35(1):118–128
Das R, Rita Champaneria R, Daniels JP et al (2014) Comparison of embolic agents used in uterine artery embolisation: a systematic review and meta-analysis. Cardiovasc Intervent Radiol 37:1179–1190
Kroencke TJ, Kluner C, Hamm B, Gauruder-Burmester A (2007) Use of the 4F Rosch inferior mesenteric catheter in embolization procedures in the pelvis: a review of 300 cases. Cardiovasc Intervent Radiol. 30(2):268–272
Kroencke TJ, Scheurig C, Poellinger A et al (2010) Uterine artery embolization for leiomyomas: percentage of infarction predicts clinical outcome. Radiology 255:834–841
Das R, Gonsalves M, Vlahos I, Manyonda I, Belli AM (2013) MRI assessment of uterine artery patency and fibroid infarction rates 6 months after uterine artery embolization with nonspherical polyvinyl alcohol. Cardiovasc Intervent Radiol 36(5):1280–1287
Richard SG (2014) D., Mark R.A., Jeffrey M.I., et al. Comparison of polyvinyl alcohol microspheres and Tris-Acryl gelatin microspheres for uterine fibroid embolization: results of a single-center randomized study. J Vasc Interv Radiol 25:823–832
Bratby MJ, Ramachandran N, Sheppard N et al (2007) Prospective study of elective bilateral versus unilateral femoral. Cardiovasc Intervent Radiol. 30:1139–1143
Acknowledgements
To all the participants for their cooperation and patience.
Funding
No funding sources.
Author information
Authors and Affiliations
Contributions
AME suggested the research idea, ensured the original figures and data in the work, correlated the study concept and design, collected data in all stages of manuscript, and had the major role in analysis. ME and HE supervised the study with significant contribution to design the methodology, manuscript revision, and preparation. RM correlated the clinical data of patient and matched it with the findings, drafted, and revised the work. AK performed data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consents were taken from the patients. The study was approved by ethical committee of Tanta University Hospital, Faculty of Medicine number 30361/06/2015.
Consent for publication
Participants included in the research gave written consent to publish the data included in the study. Authors accepted to publish the paper.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsharkawy, A.M., Elsaeed, H.H., Kamel, A.H. et al. Comparison between the outcome of single versus multiple uterine fibroids after uterine artery embolization. Egypt J Radiol Nucl Med 51, 77 (2020). https://doi.org/10.1186/s43055-020-00192-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00192-4