Abstract
Introduction
The World Health Organization’s (WHO) update of 2017 defines the cut-off for BCL2 in immunohistochemistry (IHC) in 50% of stained cells in diffuse large B-cell lymphomas (DLBCL). The WHO’s 2017 classification, however, has no standardized value. This study analyzes associations between immunohistochemistry results for BCL2 in relation to the detection of translocations of MYC, BCL2, and BCL6 in DLBCL.
Method
Sixty-seven patients with DLBCL were evaluated using IHC, with CD20, CD10, BCL6, BCL2, MUM1, TDT and MYC, and fluorescence in situ hybridization (FISH) for translocations involving the BCL2, BCL6, and MYC. Two cut-offs for BCL2 in IHC were used (50 and 70%), with the calculation of sensitivity (S), specificity (E), positive predictive value (PPV), negative predictive value (NPV), accuracy and concordance test, with a significance level of 5%.
Results
Using a 70% cut-off, there is a good relationship between S (88.9%, IC95% = 68.4–109.4) and E (67.2, 95% CI = 55.2–79.3), with a high NPV (97.5, 95% CI = 92.7–102.3) and statistically significant agreement (K = 0.30, p = 0.02). Using a 50% cut-off, S and NPV increase to 100%, with a specificity of 39.7% (95% CI = 27.1–52.2) and a statistically significant concordance (K = 0.15, p = 0.017).
Conclusion
Reduction in the percentage of immunostaining increases the detection of DLBCL with a “double-expressor” immunophenotype. The lower criterion amplifies the S and the NPV of IHC to detect translocations involving the BCL2 gene, with an impact on the diagnosis of DLBCL “double expressor”, an unfavorable prognostic group.
Similar content being viewed by others
Highlights
-
The association between the results of immunohistochemistry and the results of molecular tests represents a challenge for pathologists. Cut-offs or scores of immunohistochemistry are resources for pathologists during their diagnostic routines.
-
MYC and BCL2 are important genes in high-grade lymphomas. Pathologists must report their status with their prognosis impact. For these genes, the literature shows there are differences concerning the cut-off point for use in immunohistochemistry.
-
The fluorescent in situ hybridization (FISH) molecular test was used in this study. Finding the correct cut-off points for patients with lymphoma is very important because FISH is a special technique with a high cost and low availability. When confident immunohistochemistry results are obtained, an algorithm for the selection of patients to undergo molecular tests may be proposed.
-
The WHO’s 2017 classification discussed this question, but it does not conclude a standardized value. The WHO recommends that all patients with DLBCL must be submitted to the FISH test.
-
Reduction in the percentage of immunostaining increases the detection of DLBCL with “double-expressor” immunophenotype. The lower criteria amplify the S and the NPV of IHC to detect translocations involving the BCL2 gene, with an impact on the diagnosis of DLBCL “double expressor”, an unfavorable prognostic group.
Introduction
In 2016, Swerdlow et al. (2016) published a review of the classification of the World Health Organization (WHO) for hematopoietic tumors. One of the most important focuses of this review concerns high-grade B lymphomas (HGBL). The authors proposed modifications to replace the terminology suggested in the 2008 edition, which defined the provisional entity of unclassifiable B-cell lymphomas with intermediate characteristics between diffuse large B-cell lymphoma and Burkitt’s lymphoma (UBL/DLBCL/BL). Due to the updated classification, the name UBL/DLBCL/BL was extinguished, favoring the use of the term HGBL, without other specifications, or double-hit lymphoma (DHL) or triple-hit lymphoma (THL) (Swerdlow et al. 2016; Swerdlow et al. 2008).
For this correct diagnostic classification, it is fundamental to use molecular cytogenetic techniques to search for translocations involving MYC, BCL2, and/or BCL6 genes. One point that is regularly discussed by pathologists is the associations between molecular and immunohistochemistry (IHC) findings. The definition of the best criteria of positivity in the IHC with the best correlations with molecular results (Oliveira et al. 2017) is important.
In this context, there are variabilities in the sensitivity and specificity of the immunohistochemistry to detect the MYC, BCL2, and BCL6 rearrangements, reflecting the different immunostaining cut-offs.
The literature defines the BCL2 marker as positive when the percentages of immunostaining range from 40 to 70%. In the 2016 update, Swerdlow et al. (2016) propose a cut-off point of at least 50% of the cells evaluated with positivity in the immunohistochemical study. However, in the new WHO edition (Oliveira and Domingues 2017), officially published in 2017, there is no specific cut-off. Thus, this study analyzes the diagnostic power of IHC for BCL2 in the detection of molecular rearrangements in DLBCL samples, comparing the use of two different cut-offs.
Method
Patients with DLBCL who were diagnosed between 1998 and 2013 made up the samples of this study. There were 67 patients in the Department of Pathology, Botucatu School of Medicine, São Paulo State University (FMB UNESP). These patients were reviewed for morphological and immunohistochemistry revaluation and diagnostic confirmation. The project was approved by the research ethics committee of the institution where it was carried out. Informed consent was obtained from all individual participants included in the study as the rules and recommendations of the Research Ethics Committee of FMB UNESP.
Central nervous system (CNS) and/or bone marrow (BM) infiltration, Ann-Arbor staging, therapeutic management, and outcome (remission or death) were the clinical aspects reviewed in this study. The death rate was defined considering the 5 years after diagnosis.
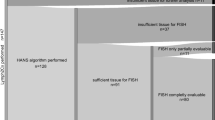
IHC and fluorescence in situ hybridization (FISH) studies were performed on tissue microarray (TMA).
CD10 (clone 56C6, ready for use, Dako), BCL6 (clone PGB6-P, ready for use, Dako), BCL2 (clone 124, ready for use, Dako), CD20 (clone L26, dilution 1: 250, Cell Marque), CD10 Dako), MUM1 (clone MUM1P, ready for use, Dako), TDT (polyclonal, ready for use, Dako) and C-MYC (clone EP121 ready for use, Biocare) were the antibodies used for IHC evaluation.
For MYC and BCL6, samples were considered positive when marker expression was greater than 40 and 50% of tumor cells, respectively. For BCL2, two criteria were adopted: 70% or more of immunostaining and 50% or more of immunostaining.
The FISH analysis was performed using specific probes to detect translocations involving the loci of the MYC (Vysis LSI, MYC dual color, break apart rearrangement probe, Abbott Molecular Des Plaines, IL, USA), BCL2 (Dako, BCL2 FISH DNA probe split signal) and BCL6 (Vysis LSI, BCL6 dual color, break apart rearrangement probe; Abbott Molecular Des Plaines, IL, USA). The cases were considered positive when, in one sample, 5.0% of the cells (at least 40 neoplastic cells were counted) showed the orange and green signs apart.
The concordances between the immunohistochemical and cytogenetic tests for the MYC, BCL2 and BCL6 markers were evaluated with sensitivity (S), specificity (E), positive predictive value (PPV) and negative predictive value (NPV), accuracy (A) and Kappa coefficient of agreement (K), presented with their respective 95% confidence intervals. The strength of the agreement determined by the Kappa coefficient was thus analyzed: poor (< 0.20), regular (0.21–0.40), moderate (0.41–0.60), good (0.61–0.0, 80), very good (0.81 to 1.00). The level of significance (p-value) tested was 0.05.
Results
Among 67 patients with DLBCL, 40 (59.7%) were women, and the median age was 56.5 years old (ranging from 25 to 88). The majority of patients (34/65; 52.3%) were classified as non-germinal center-like (NGC). The high level of Ann-Arbor staging (III and IV) was detected in 25/65 (38.5%) patients. BM was infiltrated by the neoplasm in 11/64 (17.2%) patients, and CNS was positive for lymphoma cells in 4/64 (6.2%) patients. After 5 years of the diagnosis, 26/54 (44.1%) patients’ conditions had resulted in death.
For the MYC gene, the association between the IHC and FISH findings had a regular agreement (Kappa = 0.23). It was not statistically significant (p = 0.070). For the BCL6 gene, this association was poor (K = 0.01, p = 0.583).
The use of the 70% cut-off value for BCL2 in IHC leads to a good relationship with BCL2 FISH results in relation to S and E, with high NPV, regular agreement (K = 0.30) and statistically significant (p = 0.02). The use of the 50% cut-off value for BCL2 in IHC increases S and VPN to 100% for the detection of BCL2 FISH (p = 0.017). However, the use of a lower cut-off value had a poor agreement (K = 0.15, Tables 1 and 2).
The DLBCL double-expressor immunophenotype is the group of patients with positivity for MYC and BCL2 in IHC. Reduction in the cut-off value of immunostaining for BCL2 also increases the detection of DLBCL with double-expressor immunophenotype from 22 to 27 patients.
The “double-expressor” group defined by a cut-off of 50% in the IHC (DE50) included 27 patients, of which 14 (51.8%, p = 0.575) were consistent with non-germinal center-like (NGC) through the Hans algorithm, and 13 (48.1%, p = 0.266) had Ann-Arbor III or IV. BM and CNS infiltrations occurred in three (11.1%, p = 0.224) and in two (7.4%, p = 0.566) individuals, respectively. In DE50, 28% (7/27, p = 0.030) of the deaths were patients from the double-expressor group (Table 3 and Table 4).
The “double-expressor” group defined by 70% cutoff in IHC (DE70) included 22 patients, ten (45.4%, p = 0.298) consistent with non-germinal center-like (NGC) in the Hans algorithm. Advanced staging III or IV was observed in 11 (50%, p = 0.206) individuals. BM and CNS were infiltrated in three (13.6%, p = 0.432) and two (9.0%, p = 0.426) patients, respectively. In DE70, 30% (6/20, p = 0.099) of the deaths were patients from the double-expressor group (Table 3 and Table 4).
Another important aspect is the evaluation of the meaning of the BCL2 staining in IHC in relation to the presence of MYC rearrangement using the FISH exam. Using the 50% cut-off, there was only one patient positive for BCL2 in the IHC and positive for MYC rearrangement in the FISH test (p = 0.190). In this group, 47 patients were positive for BCL2 IHC and negative for MYC FISH. Accuracy was 26.9%. The group analyzed with 70% cut-off for BCL2 in IHC, showed no patients with double-positive for BCL2 in IHC and for MYC rearrangement.
Discussion
Variations in the S and E of IHC for detecting molecular rearrangements involving MYC, BCL2, and BCL6 genes reflect the percentages of immunostaining considered by the different authors. For a BCL2 IHC reaction, in the literature, the positivity ranges from 30 to 70% of cells stained (Perry et al. 2014; Swerdlow et al. 2017; Swerdlow 2014). Swedlow et al. (2016) define 50% as a cut-off. The WHO 2017 publication (Swerdlow et al. 2017), did not define criteria for a cut-off and did not indicate criteria for selecting patients for the FISH evaluation (Swerdlow et al. 2016; Oliveira and Domingues 2017; Swerdlow et al. 2017).
Initially, all cases of DLBCL should be submitted to molecular evaluation to search for MYC, BCL2, and BCL6 rearrangements (Swerdlow et al. 2016; Oliveira and Domingues 2017). The idea to use IHC to screen individuals at higher risk of the presence of translocations motivates studies like this one (Oliveira and Domingues 2017). Moreover, considering that DLBCL is the most common lymphoma in several countries, the number of molecular tests that should be performed is high and, consequently, costs are elevated. Therefore, studies about the prognosis impact of these translocations in DLBCL patients emphasizes the importance of knowledge development regardless of the possible criteria to select patients for expensive molecular exams.
Green et al. (2012) worked with an MYC index greater than 40% and BCL2 index higher than 70% at IHC and found good associations. Oliveira et al. (2017) showed that the best associations applied to BCL2, MYC, and BCL6, in this order.The diagnosis of DHL/THL depends on the molecular study (Swerdlow et al. 2016; Oliveira and Domingues 2017). However, those with double staining at IHC, for example, patients positive for MYC and BCL2, called double-expressors, would have a nine times higher chance of death, sharing the poor prognosis with DHL/THL (Perry et al. 2014; Swerdlow et al. 2017).
The main point in this study is the reduction of false-positive patients in two situations. The first one is the comparison between BCL2 IHC and BCL2 FISH. The second one is the comparison between BCL2 IHC and MYC FISH. In these two situations, there is a reduction in the number of false-positives patients (Table 3 and Table 4). Thus, by using a 50% cut-off, more patients would be submitted to molecular tests. However, many of these exams may be unnecessary due to the index of false-positive.
The results presented in this research pointed out other aspects that deserve attention in future and broader studies. First, is the question of the clone used for BCL2 evaluation. In this study, we used clone 124, widely used in diagnostic routines, which may present false negatives compared to other clones (E17 and SP66) (Kendrick et al. 2014). Another important point is regarding the evaluation of MYC gene alterations from the FISH exam. A recent article by King et al. (2019) indicated that false negative rates in the MYC gene evaluation by break-apart probes and MYC/IGH fusion probes are approximately 4 and 22%, respectively. The combined use of the probes may represent an alternative to minimize these values, or the use of other molecular techniques to detect changes in this gene may be further explored.
The IHC BCL2 cut-offs reduction expands the detection of double-expressors and may select more patients for the FISH exam. However, discrepant results can occur depending on the clones and probe models used. There is still not an effective model for selection patients for molecular tests, and the number of HGBL cases does not seem high in the diagnostic routine. Certainly, the main difficulty for a more precise association between IHC and FISH results involves other paths that justify the discrepancies observed in diagnostic routines and in different articles. The results obtained through this study add to other groups’ results to discuss a definition of IHC interpretation cut-offs of these markers.
Our group is using a cut-off of 50% for BCL2 and a cut-off of 40% form MYC in IHC, as Swerdlow et al. (2016) because, at this moment, we understand that the main objective is to select the largest number of patients for molecular tests.
Conclusion
The use of the 50% immunostaining criterion instead of 70% amplifies the S and the immunohistochemical NPV to detect translocations involving the BCL2 gene, with an impact on the diagnosis of DLBCL double-expressor, an unfavorable prognostic group. This study encourages discussions about the utility of IHC for MYC and/or BCL2 for screener evaluations of individuals using FISH. No specific values have been classified, including the classification provided by WHO 2017. IHC may be an alternative for hospitals where this kind of service is not offered to people. The limits of this study include sampling and retrospective design. However, the data reaffirm the recommendations of Swerdlow et al. (2016) about the possibility of a 50% cut-off for BCL2 in IHC to select patients for the molecular approach.
Availability of data and materials
All the data may be accessed by the email contact of the author.
Abbreviations
- WHO:
-
World Health Organization
- HGBL:
-
High grade B lymphomas
- UBL/DLBCL/BL:
-
Unclassifiable B-cell lymphomas with intermediate characteristics between diffuse large B-cell lymphoma and Burkitt’s lymphoma
- BL:
-
Burkitt lymphoma
- DLBCL:
-
Diffuse large B-cell lymphoma
- DHL:
-
Double-hit lymphoma
- THL:
-
Triple-hit lymphoma
- CNS:
-
Central nervous system
- BM:
-
Bone marrow
- IHC:
-
Immunohistochemistry
- FISH:
-
Fluorescence in situ hybridization
- S:
-
Sensitivity
- E:
-
Specificity
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- A:
-
Accuracy
- DE50:
-
“Double-expressors” group defined by a cut-off of 50% in the IHC
- DE70:
-
“Double-expressors” group defined by 70% cut-off in IHC
- NGC:
-
Non-germinal center-like
- CGB:
-
Germinal center-like
References
Green TM, Young KH, Visco C et al (2012) Immunohistochemical double-hit score is a strong predictor of outcome in patients with diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol 30:3460–3467
Kendrick SL, Redd L, Muranvi A, Henricksen LA, Stanislaw S, Smith LM et al (2014) BCL2 antibodies targeted at different epitopes detect varying levels of protein expression and correlate with frequent gene amplification in diffuse large B-cell lymphoma. Hum Pathol 45(10):2144–2153
King RL, McPhail ED, Meyer RG, Vasmatzis G, Pearce K, Smadbeck JB et al (2019) False-negative rates for MYC fluorescence in situ hybridization probes in B-cell neoplasms. Haematologica. 104(6):e248–e251
Oliveira CC, Domingues MAC (2017) Double-Hit and Triple-Hit Lymphomas: New Perspectives for Their Classification. EMJ Hematol 5(1):95–103
Oliveira CC, Maciel-Guerra H, Kucko L, Hirama EJ, Brilhante AD, Quevedo FC et al (2017) Double-hit lymphomas: clinical, morphological, immunohistochemical and cytogenetic study in a series of Brazilian patients with high-grade non-Hodgkin lymphoma. Diagn Pathol. 12(1):3
Perry AM, Alvarado-Bernal Y, Laurini JA et al (2014) MYC and BCL2 protein expression predicts survival in patients with diffuse large B-cell lymphoma treated with rituximab. Br J Hematol 165:382–391
Swerdlow SH (2014) Diagnosis of ‘double-hit’ diffuse large B-cell lymphoma and B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and Burkitt lymphoma: when and how, FISH versus IHC. Hematol Am soc Hematol Educ Prog 5(1):90–99
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al (2008) WHO classification of tumours of haematopoietic and lymphoid tissues, vol 2, 4th edn. IARC, Lyon, p 265
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues, revised 4th ed. Lyon: IARC; 2017. p. 581
Swerdlow SH, Campo E, Pileri SA et al (2016) The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 127(20):2375–2390
Acknowledgments
Not applicable.
Funding
No financial support was provided to the authors or the paper during the research.
Author information
Authors and Affiliations
Contributions
CCO is the main author, having started with the idea of the project that is a continuation of his PhD. Project idealization, project writing, and project execution, and writing of the manuscript using a statistical methodology. MACD collaborated on the design of the research and the analysis of the slides. CCO, FAS, and IWC were responsible for the molecular evaluation of the cases. Everyone discussed the text and made their final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research had the approval of the research ethics council of FMB UNESP.
Consent for publication
The research had the approval of the research ethics council of FMB UNESP. The consent for publications and to participate were obtained according to availability and under the guidance of the council.
Competing interests
The authors do not have any conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oliveira, C.C., Domingues, M.A.C., da Cunha, I.W. et al. 50% versus 70%: is there a difference between these BCL2 cut-offs in immunohistochemistry for diffuse large B-cell lymphomas (DLBCL)?. Surg Exp Pathol 3, 18 (2020). https://doi.org/10.1186/s42047-020-00070-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42047-020-00070-3