Abstract
Background
Economic dimensions of implementing quality improvement for diabetes care are understudied worldwide. We describe the economic evaluation protocol within a randomised controlled trial that tested a multi-component quality improvement (QI) strategy for individuals with poorly-controlled type 2 diabetes in South Asia.
Methods/design
This economic evaluation of the Centre for Cardiometabolic Risk Reduction in South Asia (CARRS) randomised trial involved 1146 people with poorly-controlled type 2 diabetes receiving care at 10 diverse diabetes clinics across India and Pakistan. The economic evaluation comprises both a within-trial cost-effectiveness analysis (mean 2.5 years follow up) and a microsimulation model-based cost-utility analysis (life-time horizon). Effectiveness measures include multiple risk factor control (achieving HbA1c < 7% and blood pressure < 130/80 mmHg and/or LDL-cholesterol< 100 mg/dl), and patient reported outcomes including quality adjusted life years (QALYs) measured by EQ-5D-3 L, hospitalizations, and diabetes related complications at the trial end. Cost measures include direct medical and non-medical costs relevant to outpatient care (consultation fee, medicines, laboratory tests, supplies, food, and escort/accompanying person costs, transport) and inpatient care (hospitalization, transport, and accompanying person costs) of the intervention compared to usual diabetes care. Patient, healthcare system, and societal perspectives will be applied for costing. Both cost and health effects will be discounted at 3% per year for within trial cost-effectiveness analysis over 2.5 years and decision modelling analysis over a lifetime horizon. Outcomes will be reported as the incremental cost-effectiveness ratios (ICER) to achieve multiple risk factor control, avoid diabetes-related complications, or QALYs gained against varying levels of willingness to pay threshold values. Sensitivity analyses will be performed to assess uncertainties around ICER estimates by varying costs (95% CIs) across public vs. private settings and using conservative estimates of effect size (95% CIs) for multiple risk factor control. Costs will be reported in US$ 2018.
Discussion
We hypothesize that the additional upfront costs of delivering the intervention will be counterbalanced by improvements in clinical outcomes and patient-reported outcomes, thereby rendering this multi-component QI intervention cost-effective in resource constrained South Asian settings.
Trial registration
ClinicalTrials.gov: NCT01212328.
Similar content being viewed by others
Background
Diabetes is one of the fastest growing public health problems with huge financial burdens. The global costs of diabetes were US$ 1.31 trillion (1.8% of global GDP) in 2015 [1]. A 2018 systematic review found that annual costs of diabetes care (out of pocket medical expenditure) in South Asia ranged between US$ 575 to US $1216 per person [2]. Diabetes is a progressive disease which requires increasingly more clinic visits, laboratory tests, and patients need to engage with the healthcare system and providers over years for better management of diabetes which can arrest disease progression. However, current chronic care for diabetes is sub-optimal, costly, and lower socioeconomic status or uninsured individuals may be more likely to experience poor control [3,4,5,6,7].
Several barriers at the patient- (e.g., low motivation, financial barriers), provider- (e.g., inertia to intensify treatments), and system-level (e.g., complicated and/or fragmented care system), individually or together, cause patient and system “fatigue” and disrupt achievement of diabetes care goals [8,9,10]. In the Centre for Cardio-metabolic Risk Reduction in South Asia (CARRS) Trial, we targeted different levels of barriers together (e.g., patient motivation and provider inertia) [9, 11] and demonstrated sustainable and larger improvements in outcomes and satisfaction for people with diabetes with a multicomponent strategy of decision support-electronic health records (DS-EHR) and non-physician care coordinators (CC), compared to usual diabetes care [12].
However, enhancements or changes to the status quo of care delivery come at a cost, and in order to formulate useful recommendations for practicing clinicians, health systems, payers (health insurance, governments, patients paying out-of-pocket), and policymakers, there is an imperative to assess the value of investing in quality improvement (QI) care models. Knowing the upfront costs is also necessary to guide decision makers as they consider implementation of QI interventions in clinical care.
A 2018 systematic review of economic evaluations of QI interventions for glycaemic control among adults with type 1 or type 2 diabetes from high income countries found that multifaceted QI interventions that lower HbA1c was good value for money versus usual care, depending on society’s willingness to pay [13]. However, in our review of cost-effectiveness of interventions to control cardiovascular diseases and diabetes mellitus, we found a scarcity of cost-effectiveness studies related to QI interventions for diabetes care in South Asia [14]. Here, we describe the economic evaluation protocol to assess the within-trial cost-effectiveness and broader societal value of the CARRS diabetes care model consisting of DS-EHR and non-physician CCs compared to usual diabetes care.
Methods/Design of Economic Evaluation
Overview
The objectives of the economic evaluation are to assess: a) the incremental cost of delivering multicomponent QI interventions compared to usual diabetes care in tertiary care settings over a period of 2.5 years; b) whether the intervention provides value for money (cost-effectiveness) to patients, healthcare systems and society than usual care, and if so; c) the extent of uncertainty over the cost-effectiveness of the intervention and value of conducting further research to reduce this uncertainty.
The CARRS Trial’s economic evaluation will follow standard international methodological guidelines [15,16,17,18]. Given, more than 80% of medical expenses in India and Pakistan are out-of-pocket expenditures borne by the patient, we will apply the patient viewpoint as the predominant perspective, in addition to healthcare system and societal perspectives for costing resource use. Cost data will be reported in 2018 United States Dollars (US$). Both cost and health effects will be discounted at 3% per year as per the World Health Organization’s (WHO) guidelines for conducting economic evaluations in developing countries.
The CARRS trial and study population
The CARRS Trial randomised 1146 eligible patients with poorly controlled type 2 diabetes (HbA1c > 8% and SBP > 140 mmHg or LDLc> 130 mg/dl) to intervention (n = 575) or usual care (n = 571) across 10 diverse diabetes clinics in India and Pakistan. At baseline, participants’ mean age was 54 years, 45% were males, mean HbA1c was 9.9%, LDLc 123.2 mg/dl, BP 144.2/82.3 mmHg, and median duration of diabetes was 7 years [12].
Intervention and comparator
Detailed information about the CARRS-Trial intervention and protocol has been published previously [19]. Briefly, the CARRS intervention consisted of DS-EHRs to enhance physicians’ responsiveness to consider treatment modification and non-physician CCs to support patients in their adherence to prescribed therapies. The DS-EHR stored all consultation, laboratory, self-care, and diabetes related complications data for patients in one easily accessible web portal to monitor patient progress; and provided decision-support system (DSS) prompts to facilitate achievement of guideline-recommended glycemic, blood pressure, and lipid goals. The CCs fully managed the DS-EHR data-entry for intervention group participants and all communication of DSS prompts to the physician during consultations via print-out or electronic display. Physicians could, at their discretion, accept or reject DSS prompts and modify treatment plans based on clinical judgment, so long as justification was provided.
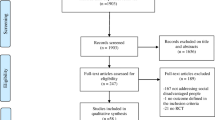
The intervention was compared with usual diabetes care at nine clinics/hospitals across India and one site in Pakistan. Figure 1 demonstrates the study flow.
Study flow - Economic evaluation alongside CARRS Trial. Abbreviations: CARRS=Centre for Cardiometabolic Risk Reduction in South Asia), DS-EHR = decision-support electronic health records; HbA1c = glycated hemoglobin, BP = blood pressure, SBP = systolic blood pressure, LDLc = low-density lipoprotein cholesterol, EQ5D-3 L = European quality of life 5 dimension 3 levels; mg/dl = milligrams per deciliter, mmHg = millimeter of mercury
Effectiveness measures
To evaluate incremental effectiveness, we will compare the proportions of intervention and control arm participants achieving multiple risk factor control defined as HbA1c < 7% and BP < 130/80 mmHg or LDLc< 100 mg/dl (and < 70 mg/dl for those with history of cardiovascular disease). Data on health-related quality of life (EQ5D-3 L); new-onset cardiovascular events, new onset microvascular events, and other hospitalizations would also be used.
The CARRS Trial is currently ongoing and we will project cardiovascular and microvascular outcomes using proxy indicators (intermediate risk factors: HbA1c, BP, LDLc). Relative risk reductions for major adverse cardiovascular events with intervention or comparator will also be calculated separately for each participant, using United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Models 2 which has been validated for use in South Asians [20]. Table 1 summarizes the study outcomes (effectiveness measures) to be considered in the cost-effectiveness analysis.
Resource use and cost data
Resource utilization and costs will be estimated using data from the CARRS Trial population (1146 participants). The study paid the costs of annual laboratory investigations, but patients had to bear the cost of clinic visits and laboratory tests for regular follow-up visits or any other interim clinic visits, tests, medication changes, or procedures advised by the treating physician. CARRS Trial data will be extracted from clinic and study records for the following: medication use, laboratory tests, consultations with healthcare professionals (outpatient attendance for diabetes); preventive screening (eye examination, foot examination, ECG, microalbuminuria test), emergency department attendances (when not admitted to hospital); and serious adverse events (including all hospital admissions).
Patients’ self-reported expenditures and costs of outpatient visits and hospitalizations related to diabetes complications will be extracted from the trial annual visit case report forms (CRF). Out-of-pocket expenses reported by the patients will permit estimation of economic value from the patient’s perspective.
To estimate value from a healthcare system perspective, unit costs for outpatient visits and in-patient hospitalizations, and processes of care measures including preventive examinations will be obtained from participating hospitals. For treatment of cardiovascular and microvascular events, we will extract detailed information concerning diagnosis; length of hospital stay; diagnostic/therapeutic procedures and any ongoing treatment and support. Additionally, the unit price of medications will be obtained from the PharmaTrac database for January 2014 [21]. PharmaTrac provides the market retail price (MRP) of all drugs by drug class, brand name, generic composition, formulation (oral/injectables), dose, and packs being sold in India. PharmaTrac has an extensive coverage of drug retailers and is believed to be a reliable source to estimate unit cost of drug prices in India. The IMS Health drug database will be used to estimate drug prices in Pakistan.
To estimate costs from the societal perspective, indirect costs due to lost productivity (number of work days missed due to out-patient or in-patient care) will be valued using the human capital approach [22]. Finally, total costs over the trial period and annual cost per patient (both undiscounted and discounted) will be estimated for individual patients by multiplying resource use by unit costs.
Intervention costs
Intervention development and delivery costs will be derived from the CARRS Trial expense records (accounts register) and will be estimated from the health system perspective. Intervention costs include DS-EHR development, implementation, and maintenance costs; intervention training; care coordinator salary; and the incremental health care costs associated with the intervention delivery (i.e. the costs of additional medicines, additional clinic visits that patients bear and whether it is different between the treatment groups). These costs will be calculated as average costs of implementation per person and exclude any research specific costs. The cost estimates assume that the DS-EHR is implemented in a relatively large tertiary care hospital having additional resource facilities to implement the intervention (i.e. workspace for the care coordinator, and access to internet service providers is considered a maintenance cost). DS-EHR development and maintenance costs will include software programmer’s time, expert consultant’s/physicians time in developing and reviewing the diabetes management algorithm. DS-EHR implementation cost will include care coordinators and site physician’s time to enter patient details in the EHR system and review of software generated diabetes management plans, respectively. Intervention training costs include training materials, the time of the trainers and the staff participating in the training, and training for physicians to use the DS-EHR algorithms. These costs will be estimated using the study’s accounting data. Training material and time costs will be estimated from the first year of the intervention. Tables 2 and 3 present an overview of cost measures, health service use, and source of data.
Within trial cost-effectiveness analysis
Based on estimates of between-group differences in mean healthcare costs and outcomes (adjusting for differences in baseline characteristics) over the study period, we will estimate the following incremental cost-effectiveness ratios (ICERs):
-
Incremental cost per primary outcome achieved (i.e. multiple risk factor control: HbA1c < 7% and BP < 130/80 mmHg and/or LDLc< 100 mg/dl)
-
Incremental cost per unit reduction in single risk factors: HbA1c (1% point reduction), SBP (5 mmHg reduction), and LDLc (10 mg/dl reduction)
-
Incremental cost per quality adjusted life years (QALYs) gained
Non-parametric bootstrapping will be used to report 95% confidence intervals around the ICER estimates [23]. ICERs will be reported in US$ 2018. Cost effectiveness acceptability curves against a wide range of willingness to pay values will be presented [24]. Cost-effectiveness results will be also presented by major sub-groups: age, gender, education, income level, types of health setting (public, private or semi-private) and history of macro- and micro-vascular complications.
Missing data
The CARRS Trial has a minimal loss to follow-up including consent withdrawals and deaths at 2.5 years (9.2%) but, if needed; multiple imputation approaches will be used to handle missing outcomes data [12]. For EQ5D-3 L scores, which will be used for QALY estimation, we will follow the developer’s guideline for missing data; that is, missing data will be handled by imputing values within each dimension [25,26,27,28]. To address potential biases due to incomplete follow-up, we will use multiple imputation approaches to replace missing cost values if missing data accounts for more than 10% of a domain/variable [29,30,31]. Since cost data are unlikely to be normally distributed, [29] we will use the multiple imputation chained equations approach to impute missing cost data. Costs will be imputed at the total cost level [29].
Decision-modeling based cost-utility analysis
A decision-analytic microsimulation model will be developed to evaluate long-term costs and health consequences of delivering care for people with type 2 diabetes using a multicomponent QI strategy rather than current standard care approaches. A microsimulation model is chosen as it is very flexible and can reflect complex treatment pathways and relationships between individuals’ characteristics, histories, and outcomes; it can be used to examine the impact of real resource constraints within a healthcare system.
The microsimulation decision model will be implemented using appropriate software: STATA or a programming language (e.g. R). To assure the credibility of our model, we will follow international guidelines for verification and validation of decision models [32].
Model analysis
All analyses will compare results for the CARRS multicomponent QI care delivery model versus usual diabetes care. In the CARRS Trial microsimulation model, costs and QALYs will be recorded for each individual and an average cost and QALY for the simulated population will be estimated. The microsimulation model will be run twice, once to simulate costs and QALYs under usual care and the other to simulate costs and QALYs under the intervention scenario (multicomponent QI strategy). Individuals representing the CARRS trial inclusion criteria will enter the model and their baseline risk for CVD events and diabetes-related microvascular complications will be estimated using the UKPDS Outcomes Model 2 algorithm. Costs and QALYs will be recorded for each event (including adverse events). Individuals can experience more than one event (model run for lifetime horizon) and patient characteristics such as age and history of previous events, such as a stroke or diabetic retinopathy, will be updated as the model is being run, with ensuing reflective increases in the risk of an event. The simulation model will run for a sufficient number of iterations to provide stable results. If there is a trade-off between costs and health effects (higher costs and better health outcomes for the CARRS intervention, or vice versa), the incremental cost per cardiovascular event averted, incremental cost per diabetes-related microvascular complication averted, and incremental cost per quality adjusted life year (QALY) gained will be reported. Projections of cost-effectiveness estimates over a lifetime horizon will be made for India and Pakistan.
Sensitivity analysis
Several one-way sensitivity analyses will be carried out to estimate the uncertainties around ICERs. First, to address the uncertainty around the ICER relating to external validity, we will carry out sensitivity analyses on the most important cost drivers (medications, hospitalizations, and consultation fees) to assess the impact of protocol-driven healthcare use. Second, total cost will be calculated with and without the costs of developing the intervention (DS-EHR) to ascertain whether an increased cost in the intervention arm could be explained by costs for some of the components of the intervention. Lastly, sensitivity analyses would vary the effectiveness of the intervention in trial vs. non-trial settings based on the lower and upper limit of 95% confidence intervals (CI) of the effect estimates. Results of probabilistic sensitivity analyses will be presented using a scatter plot of points on the cost-effectiveness plane – illustrating the possible ranges of estimates of incremental costs and incremental QALYs [24].
Discussion
The publication and peer-review of economic evaluation protocols alongside clinical trials is recommended to increase transparency and minimise bias [33]. Here, we describe the protocol of an economic evaluation of a multicomponent QI strategy compared to usual diabetes care in South Asia from patient, healthcare system, and societal perspectives. There are very few economic evaluations of QI strategies for chronic disease management in South Asia [34] or in LMICs in general, and so this report fills a gap. Following internationally recognised guidelines [15], this protocol serves to heighten the transparency of our economic evaluation approach.
Economic evaluations from high-income countries demonstrate that multifactorial QI strategies are cost-effective. For example, the STENO-2 study showed that, from a health care payer perspective in Denmark, intensive multifactorial intervention was more cost-effective than conventional treatment (ICER: €2538 or US$ 2954 per QALY gained) over a lifetime horizon [35]. Increased costs with intensive treatment were due to increased pharmacy and consultation costs. However, this also resulted in more QALYs gained for intensive treatment versus conventional treatment (+ 1.66 QALYs). The ADDITION-UK trial based cost-effectiveness analysis comparing intensive versus conventional treatment demonstrated an ICER of £71,232 (US$93566)/QALY, £28,444 (US$37362)/QALY, and £27,549 (US$36186)/QALY over 10-, 20-, and 30-year time horizons respectively [36]. Given the United Kingdom’s willingness-to-pay thresholds in patients with diabetes, intensive treatment was of borderline cost-effectiveness over a time horizon of ≥20 years. The estimates of cost-effectiveness from the CARRS Trial will provide much needed data on whether a simple multifactorial intervention can improve health outcomes with modest increases in costs in resource-constrained settings.
To enhance external validity, it is recommended that evaluations using randomised controlled trials should identify threats to validity such as recruitment/selection bias, protocol-driven utilisation, and enhanced compliance [34, 37]. Regarding recruitment biases, the CARRS Trial’s multicentre approach and inclusion of public, private, and semi-private practices increases the generalisability and transferability of our economic evaluation findings [38]. Further, we will extrapolate the decision analytic microsimulation model beyond the within-trial analysis by using a sample population of poorly controlled type 2 diabetes patients in India / Pakistan stratified by age-group, gender, and location. Also, although Markov models can also be adapted for this purpose, microsimulation models are better suited for analysis of a mixed population with both incident and prevalent diabetes complications (cardiovascular diseases and microvascular events) [39].
This study has several strengths. First, the economic evaluation protocol follows recognised international guidelines to design and report on the relative costs and benefits of an intervention tested in a randomised trial [15, 37]. Second, the economic evaluation will include individual patient-level data over a lengthy 2.5 years of follow up, which are preferable for economic evaluations [15]. Importantly, these patient-level data include objective measures of health outcomes, health service use, and medicine use, all obtained during the trial [40]. Reliable economic evaluations are crucial to shape healthcare policy, in particular when the possibility of bias in economic evidence has been minimised by randomisation [40]. Third, our cost-effectiveness results will also provide a range of values for both the cost of achieving multiple risk factor targets but also costs to achieve single and combined risk factor improvements from poorly controlled baseline values (mean baseline HbA1c = 9.9) from various perspectives (patient, healthcare system and societal). Given a large proportion of healthcare in South Asia is paid for out-of-pocket, our economic analyses consider that scenario explicitly with a patient perspective analysis. Fourth, our proposed micro-simulation model based on UKPDS Outcomes Model 2 will enable long-term cost-effectiveness analysis and a population budget impact analysis which will provide cross-sectional estimates of population impact by year for planning purposes and scalability of the intervention.
This study has a few noteworthy limitations. First, reliance on patient self-reported out-of-pocket medical cost data may impact the validity of study results. A 2016 systematic review of validated self-reported questionnaires to measure resource utilization and costs in economic evaluation concluded that self-reported questionnaires had good agreement with administrative data and are a valid method of collecting data on health resource utilization and associated costs [41]. However, to overcome any reporting bias in self-reported costs data, a sub-set of self-reported costs will be verified against the administrative data and we will carry out several one-way and probabilistic sensitivity analyses around the self-reported costs in the microsimulation model to estimate the confidence in the reported ICER values. Another limitation of the proposed evaluation is that in India and Pakistan, there is not an explicit willingness to pay threshold for reduction of cardiovascular risk in people with diabetes, or an explicit willingness to pay threshold for cost per unit reductions in CVD risk factors. As such, it is hard to declare how patients value the intervention. The Commission for Macroeconomics and Health recommends using a threshold of 1-3x GDP per capita per QALY gained or DALYs averted to define cost-effectiveness of a new intervention when conducting global or regional economic evaluations [16, 42]. Although arbitrary, we will use this threshold as it has been used previously and has some philosophical underpinnings [43]. We will apply these and then perform a sensitivity analysis for the main economic outcome and present the cost-effectiveness results on a cost-effectiveness acceptability curve considering a wide range of willingness to pay values. Common to all cost-effectiveness analyses conducted alongside randomised trials, external validity of the results may be influenced by restrictive inclusion criteria and protocol-driven resource use, among other factors [15, 37]. Therefore, we will conduct a range of sensitivity analyses around key variables (cost drivers, total cost calculated with and without the cost of the intervention development, patient characteristics, and effectiveness of the intervention) to address the uncertainties around the ICERs.
In conclusion, we hypothesise that the additional upfront cost of delivering the intervention will be counterbalanced by improvements in clinical practice and patient related outcomes, thereby rendering the CARRS QI strategy cost-effective. The results of this study will be of immediate relevance for decision makers of all sorts –patients, healthcare providers, and policy makers– concerning implementation of this healthcare delivery intervention to improve diabetes care goals.
Abbreviations
- €:
-
Euros
- BP:
-
Blood pressure
- CARRS:
-
Centre for Cardiometabolic Risk Reduction in South Asia
- CC:
-
Care coordinator
- CI:
-
Confidence interval
- CRF:
-
Case report form
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- DS-HER:
-
Decision support electronic health records
- DSS:
-
Decision support software
- ECG:
-
Electrocardiogram
- EQ-5D 3 L:
-
European Quality of Life 5 dimensions - 3 levels
- GDP:
-
Gross domestic product
- HbA1c:
-
Glycated haemoglobin
- ICER:
-
Incremental cost-effectiveness ratio
- LDLc:
-
Low-density lipoprotein cholesterol
- LMIC:
-
Low- and middle- income countries
- QALYs:
-
Quality adjusted life years
- QI:
-
Quality improvement
- SBP:
-
Systolic blood pressure
- UK:
-
United Kingdom
- UKPDS:
-
United Kingdom Prospective Diabetes Study
- US$:
-
United States dollar
References
Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Barnighausen T, Vollmer S. The global economic burden of diabetes in adults aged 20-79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5(6):423–30.
Basu S, Bendavid E, Sood N. Health and economic implications of National Treatment Coverage for cardiovascular disease in India: cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes. 2015;8(6):541–51.
Deepa M, Anjana RM, Manjula D, Narayan KM, Mohan V. Convergence of prevalence rates of diabetes and cardiometabolic risk factors in middle and low income groups in urban India: 10-year follow-up of the Chennai urban population study. J Diabetes Sci Technol. 2011;5(4):918–27.
Decker SL, Kostova D, Kenney GM, Long SK. Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs uninsured low-income adults potentially eligible for Medicaid under the affordable care act. JAMA. 2013;309(24):2579–86.
Shivashankar R, Kirk K, Kim WC, Rouse C, Tandon N, Narayan KM, Ali MK. Quality of diabetes care in low- and middle-income Asian and middle eastern countries (1993-2012): 20-year systematic review. Diabetes Res Clin Pract. 2015;107(2):203–23.
Tharkar S, Devarajan A, Kumpatla S, Viswanathan V. The socioeconomics of diabetes from a developing country: a population based cost of illness study. Diabetes Res Clin Pract. 2010;89(3):334–40.
Tharkar S, Satyavani K, Viswanathan V. Cost of medical care among type 2 diabetic patients with a co-morbid condition--hypertension in India. Diabetes Res Clin Pract. 2009;83(2):263–7.
Chin MH, Cook S, Jin L, Drum ML, Harrison JF, Koppert J, Thiel F, Harrand AG, Schaefer CT, Takashima HT, et al. Barriers to providing diabetes care in community health centers. Diabetes Care. 2001;24(2):268–74.
Sohal T, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for Type-2 diabetes Management in South Asians: a systematic review. PLoS One. 2015;10(9):e0136202.
Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93(1):1–9.
Wangnoo SK, Maji D, Das AK, Rao PV, Moses A, Sethi B, Unnikrishnan AG, Kalra S, Balaji V, Bantwal G, et al. Barriers and solutions to diabetes management: an Indian perspective. Indian J Endocrinol Metab. 2013;17(4):594–601.
Ali MK, Singh K, Kondal D, Devarajan R, Patel SA, Shivashankar R, Ajay VS, Unnikrishnan AG, Menon VU, Varthakavi PK, et al. Effectiveness of a multicomponent quality improvement strategy to improve achievement of diabetes care goals: a randomized, controlled trial. Ann Intern Med. 2016;165(6):399–408.
Nuckols TK, Keeler E, Anderson LJ, Green J, Morton SC, Doyle BJ, Shetty K, Arifkhanova A, Booth M, Shanman R, et al. Economic evaluation of quality improvement interventions designed to improve glycemic control in diabetes: a systematic review and weighted regression analysis. Diabetes Care. 2018;41(5):985–93.
Singh K, Chandrasekaran AM, Bhaumik S, Chattopadhyay K, Gamage AU, Silva P, Roy A, Prabhakaran D, Tandon N. Cost-effectiveness of interventions to control cardiovascular diseases and diabetes mellitus in South Asia: a systematic review. BMJ Open. 2018;8(4):e017809.
Ramsey SD, Willke RJ, Glick H, Reed SD, Augustovski F, Jonsson B, Briggs A, Sullivan SD. Cost-effectiveness analysis alongside clinical trials II-an ISPOR good research practices task force report. Value Health. 2015;18(2):161–72.
Tan-Torres Edejer T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, Murray CJL. WHO Guide to Cost-effectiveness analysis; 2003.
Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, Kuntz KM, Meltzer DO, Owens DK, Prosser LA, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. Panel on cost-effectiveness in health and medicine. JAMA. 1996;276(16):1339–41.
The CARRS Trial Writing Group, Shah S, Singh K, Ali MK, Mohan V, Kadir MM, Unnikrishnan AG, Sahay RK, Varthakavi P, Dharmalingam M, et al. Improving diabetes care: multi-component cardiovascular disease risk reduction strategies for people with diabetes in South Asia--the CARRS multi-center translation trial. Diabetes Res Clin Pract. 2012;98(2):285–94.
Hayes AJ, Leal J, Gray AM, Holman RR, Clarke PM. UKPDS outcomes model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom prospective diabetes study: UKPDS 82. Diabetologia. 2013;56(9):1925–33.
Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012;366(1):54–63.
Krol M, Brouwer W. How to estimate productivity costs in economic evaluations. Pharmacoeconomics. 2014;32(4):335–44.
Nixon RM, Wonderling D, Grieve RD. Non-parametric methods for cost-effectiveness analysis: the central limit theorem and the bootstrap compared. Health Econ. 2010;19(3):316–33.
Fenwick E, Marshall DA, Levy AR, Nichol G. Using and interpreting cost-effectiveness acceptability curves: an example using data from a trial of management strategies for atrial fibrillation. BMC Health Serv Res. 2006;6:52.
Sonntag M, Konnopka A, Leichsenring F, Salzer S, Beutel ME, Herpertz S, Hiller W, Hoyer J, Joraschky P, Nolting B, et al. Reliability, validity and responsiveness of the EQ-5D in assessing and valuing health status in patients with social phobia. Health Qual Life Outcomes. 2013;11:215.
Horowitz E, Abadi-Korek I, Shani M, Shemer J. EQ-5D as a generic measure of health-related quality of life in Israel: reliability, validity and responsiveness. Isr Med Assoc J. 2010;12(12):715–20.
Yordanova S, Petkova V, Petrova G, Dimitrov M, Naseva E, Dimitrova M, Petkova E. Comparison of health-related quality-of-life measurement instruments in diabetic patients. Biotechnol Biotechnol Equip. 2014;28(4):769–74.
Simons CL, Rivero-Arias O, Yu LM, Simon J. Multiple imputation to deal with missing EQ-5D-3L data: should we impute individual domains or the actual index? Qual Life Res. 2015;24(4):805–15.
Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. Pharmacoeconomics. 2014;32(12):1157–70.
Briggs A, Clark T, Wolstenholme J, Clarke P. Missing... presumed at random: cost-analysis of incomplete data. Health Econ. 2003;12(5):377–92.
Schafer JL. Multiple imputation: a primer. Stat Methods Med Res. 1999;8(1):3–15.
Eddy DM, Hollingworth W, Caro JJ, Tsevat J, McDonald KM, Wong JB. Model transparency and validation: a report of the ISPOR-SMDM modeling good research practices task force--7. Value Health. 2012;15(6):843–50.
Godlee F. Publishing study protocols: making them visible will improve registration, reporting and recruitment. BMC News Views. 2001;2:4.
O'Sullivan AK, Thompson D, Drummond MF. Collection of health-economic data alongside clinical trials: is there a future for piggyback evaluations? Value Health. 2005;8(1):67–79.
Gaede P, Valentine WJ, Palmer AJ, Tucker DM, Lammert M, Parving HH, Pedersen O. Cost-effectiveness of intensified versus conventional multifactorial intervention in type 2 diabetes: results and projections from the Steno-2 study. Diabetes Care. 2008;31(8):1510–5.
Tao L, Wilson EC, Wareham NJ, Sandbaek A, Rutten GE, Lauritzen T, Khunti K, Davies MJ, Borch-Johnsen K, Griffin SJ, et al. Cost-effectiveness of intensive multifactorial treatment compared with routine care for individuals with screen-detected type 2 diabetes: analysis of the ADDITION-UK cluster-randomized controlled trial. Diabet Med. 2015;32(7):907–19.
Ramsey S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, Cook J, Glick H, Liljas B, Petitti D, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA task force report. Value Health. 2005;8(5):521–33.
Johnston K, Buxton MJ, Jones DR, Fitzpatrick R. Assessing the costs of healthcare technologies in clinical trials. Health Technol Assess. 1999;3(6):1–76.
Davis S, Stevenson M, Tappenden P, Wailoo A. NICE DSU Technical support Document 15: cost-effectiveness modelling using patient level simulation; 2014.
Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials. 2nd ed. Oxford: Oxford University Press; 2015.
Leggett LE, Khadaroo RG, Holroyd-Leduc J, Lorenzetti DL, Hanson H, Wagg A, Padwal R, Clement F. Measuring resource utilization: a systematic review of validated self-reported questionnaires. Medicine (Baltimore). 2016;95(10):e2759.
World Health Organization 2001. Macroeconomics and Health: Investing in Health for Economic Development. http://www1.worldbank.org/publicsector/pe/PEAMMarch2005/CMHReport.pdf. Accessed 21 Feb 2019.
Ali M, Siegel K, Chandrasekar E, Tandon N, Montoya P, et. al. “Diabetes: An Update on the Pandemic and Potential Solutions”. In: Disease Control Priorities (third edition): Volume 5, Cardiovascular, Respiratory, and Related Disorders, edited by D. Prabhakaran, S. Anand, T. Gaziano, J. Mbanya, Y. Wu, R. Nugent. Washington, DC: World Bank.
Funding
The CARRS trial was funded in part by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services, under contract number HHSN268200900026C, and by UnitedHealth Group, Minneapolis, Minnesota. Several members of the research team at the Public Health Foundation of India and Emory University were supported by the Fogarty International Clinical Research Scholars and Fellows program through grant number 5R24TW007988 from the National Institutes of Health, Fogarty International Center through Vanderbilt University, Emory Global Health Institute, and D43 NCDs in India Training Program through award number 1D43HD05249 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and Fogarty International Center. Dr. Kavita Singh was supported by the Fogarty International Center, National Institutes of Health, under award number D43TW008332 (ASCEND Research Network). Dr. M K Ali is supported by the National Institute of Mental Health supplemental grant under award number: R01MH100390-04S1.
We also acknowledge the contributions of the software development team: Mr. Prashant Tandon and Mr. Ajeet Kushwaha.
The funding sources were not involved in the data collection, analysis, writing or interpretation of the manuscript or the decision to submit it for publication.
Availability of data and materials
Not applicable as this manuscript represent a study protocol for the cost-effectiveness analysis.
Author information
Authors and Affiliations
Consortia
Contributions
KS, NT, DP, KMVN, MKA, and VP have formulated the design of the economic evaluation carried out alongside the CARRS randomised controlled trial. KS, NT, MKA, KMVN and DP have composed the questionnaires. All authors have taken part in preparation of the manuscript and have reviewed critically for the intellectual content and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional ethics committees at each participating site and the research coordinating centres (Public Health Foundation of India and Emory University, USA) approved the study and all physicians and patients gave written informed consent prior to participating in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Singh, K., Ali, M.K., Devarajan, R. et al. Rationale and protocol for estimating the economic value of a multicomponent quality improvement strategy for diabetes care in South Asia. glob health res policy 4, 7 (2019). https://doi.org/10.1186/s41256-019-0099-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41256-019-0099-x