Abstract
Background
Due to greater infection susceptibility, sepsis is the main cause of death in burn patients. Quick diagnosis and patient stratification, early and appropriated antimicrobial therapy, and focus control are crucial for patients’ survival. On the other hand, superfluous extension of therapy is associated with adverse events and arousal of microbial resistance. The use of biomarkers, necessarily coupled with close clinical examination, may predict outcomes, stratifying patients who need more intensive care, and monitor the efficacy of antimicrobial therapy, allowing faster de-escalation or stop, reducing the development of resistance and possibly the financial burden, without increasing mortality. The aim of this work is to check the suitability of procalcitonin (PCT) to fulfill these goals in a large sample of septic burn patients.
Methods
One hundred and one patients, with 15% or more of total body surface area (TBSA) burned, admitted from January 2011 to December 2014 at Coimbra Burns Unit (CBU), in Portugal were included in the sample. All patients had a diagnosis of sepsis, according to the American Burn Association (ABA) criteria. The sample was factored by survival (68 survivors and 33 non-survivors). The maximum value of PCT in each day was used for statistical analysis. Data were summarized by location measures (mean, median, minimum, maximum, quartiles) and dispersion measures (standard error and range measures). Statistical analysis was performed with SPSS© 23.0 IBM© for Windows©.
Results
There were statistically significant differences between PCT levels of patients from the survivor and non-survivor groups during the first and the last weeks of hospitalization as well as during the first week after sepsis suspicion, being slightly higher during this period. During the first 7 days of antimicrobial therapy, PCT was always higher in the non-survivor, still without reaching statistical significance, but when the analysis was extended till the 15th day, PCT increased significantly, rapidly, and steadily, denouncing therapy failure.
Conclusion
Despite being not an ideal biomarker, PCT proved to have good prognostic power in septic burn patients, paralleling the evolution of the infectious process and reflecting the efficacy of antimicrobial therapy, and the inclusion of its serial dosing may be advised to reinforce antimicrobial stewardship programs at burn units; meanwhile, more accurate approaches are not available.
Similar content being viewed by others
Background
Sepsis is still nowadays the main cause of death in burn patients due to the impact of extensive burns in all organ systems, affecting homeostatic mechanisms, and to the greater susceptibility of this population to infection [1, 2], related to the loss of the cutaneous barrier, immunosuppression, use of invasive devices, nosocomial flora, etc. Survival is directly dependent on the institution of prompt and adequate antimicrobial therapy [3]. However, the gold standard for sepsis diagnosis still relies on the identification of microorganisms in blood cultures, which unfortunately are positive only in 20–30% of all confirmed bloodstream infections, and their results may take 48 to 72 h to reach the prescriber [4]. While more rapid methods of microbiological identification, such as polymerase-chain reaction (PCR) [5], matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS), gene expression profiling, aptamer panels, etc. [6], are not either widely available or fully developed, the use of early empirical often broad-spectrum antibiotic therapy is warranted. This empirical strategy increases the likelihood of cure of infection and survival but negatively impacts in terms of microbiome, leading to the selection and emergence of antimicrobial resistance. In this context, biochemical biomarkers, namely procalcitonin (PCT) alone [7, 8] or integrating a composite panel [9,10,11,12], and always coupled with thorough clinical examination, may be an important aid for the early suspicion of sepsis and rapid institution of therapy, which is strongly associated with improved outcomes [13, 14].
PCT is a 116-amino acid precursor of calcitonin, which synthesis and secretion, encoded by first calcitonin gene (CALC-I gene), and normally restricted to thyroid C cells and some neuroendrocrine cells of the lungs and gut, is upregulated by the presence in the blood of microbial toxins, necrotic body cells, and some proinflammatory cytokines (IL-1, IL-6, TNF-α, etc.), in a synergistic way, starting to be produced in great amounts by many other nonendocrine types of cells, including monocytes and adipocytes [15], reaching measurable levels in 2–4 h after onset of the infectious process, peaking at 24–30 h, and rapidly subsiding with recovery. PCT increment is less pronounced with fungal infection and is absent in viral disease, allegedly due to inhibition of its secretion by some cytokines released as a response to viral infection, like interferon-γ [16].
Besides its utility to help clinicians in the diagnosis of sepsis [17] including patients admitted to burn units [18], the magnitude and duration of PCT elevation seems to correlate with injury severity and outcome, and there are several published works analyzing its potential for the prognosis and for the monitoring of antimicrobial therapy, helping decisions on early antibiotic de-escalation or rescue therapy [19,20,21]. Most of these are focused in lower respiratory tract infections and/or intensive care patients, while papers on septic burn patients are scarce [22].
The purpose of this work is to evaluate the feasibility of PCT use to predict the outcome and to monitor the efficacy of antimicrobial therapy in a sample of severe adult burn patients.
Methods
The sample under analysis was composed by 101 burn patients, with 15% or more of total body surface area (TBSA) burned, admitted from January 2011 to December 2014 at Coimbra Burns Unit (CBU), a department of Coimbra Hospital and University Center (CHUC), in Portugal. Being a retrospective observational study of patients from a suitably anonymized dataset, involving only recording data from the medical record, the Ethics Committee from CHUC, according to the Declaration of Helsinki and Council for International Organizations of Medical Sciences (CIOMS) International Ethics Guidelines, waived the need of informed consent.
All the patients had a diagnosis of sepsis. This diagnosis was done according to the American Burn Association (ABA) criteria [23]: a clinical suspicion of infection coupled with the presence of three or more of the following parameters: temperature > 39 or < 36.5 °C; tachycardia > 110 beats per minute; tachypnea > 25 breaths per minute or minute ventilation > 12 L/min; thrombocytopenia < 100,000/μL; hyperglycemia (untreated plasma glucose > 200 mg/dL or intravenous glucose requirement > 7 U/h over 24 h); and enteral feeding intolerance: abdominal distension or gastric residuals more than two times feeding rate or diarrhea > 2500 mL/24 h.
PCT was measured with time-resolved amplified cryptate emission (TRACE) technology (Kryptor PCT; Brahms AG; Hennigsdorf, Germany). The sample was factored by survival (68 survivors and 33 non-survivors). The maximum value of PCT in each day of the study was used for statistical analysis and when samples were not collected in some days (till a maximum of 5 days), the missing values of the interval were calculated as the median value between the PCT determinations available.
Statistical analysis
Data were summarized by location measures (mean, median, minimum, maximum, quartiles) and dispersion measures (standard error and range measures).
The variables under study present a non-Gaussian distribution. Under a nonparametric approach, the quantitative variables were compared with the Mann-Whitney U tests and qualitative variables were compared with the Pearson chi-square test. Time variations of PCT levels were tested using Friedman’s test and Kendall’s W ranges from 0 (no agreement) to 1 (complete agreement).
To measure the difference effect size between the two independent groups, the probability of superiority (PS) was used. PS ranges from 0.0 to 1.0 and PS = 0.5 state that there are no differences between the groups [A] and PS = 0 or PS = 1 states the maximum effect.
Statistical analysis was performed with SPSS© 23.0 IBM© for Windows©, and in a statistical hypothesis test, a p value ≤ 0.05 means the effect was considered significant.
Results
Sample description
Population characteristics are described in Table 1. After factorization by survival, a significant heterogeneity was found between the two groups (68 survivors and 33 non-survivors) for the age of the patients, the Abbreviated Burn Severity Index (ABSI) score (Additional file 1) [24], the TBSA burned, the presence of inhalation injury, the need of mechanical ventilation and its duration, the number of surgical interventions, the duration of sepsis episode, and the length of the stay at the burn unit. Heterogeneity was not found for gender, burn degree, and duration of antimicrobial therapy.
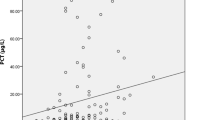
Table 2 shows the comparison of individual PCT location measures, presenting significant differences between survivors and non-survivors in all statistical parameters (minimum, median, mean, maximum).
The box plots of individual median PCT levels for each group are presented in Fig. 1, being significantly lower for survivors.
PCT evolution along the first week of stay
Table 3 shows the evolution PCT levels in patients from the survivor and non-survivor groups during the first week of stay at CBU. The data presents missing values of the PCT in some of the days of hospitalization and this is the reason for this variation in the number of individuals by scenario. Differences between PCT levels of patients from the survivor and non-survivor groups during the first week of hospitalization are statistically significant (Fig. 2a and Table 6).
Line plots of procalcitonin (PCT) levels evolution along the first week of hospitalization (a), last week of hospitalization (b), first week after suspicion of sepsis (c), and first week of antimicrobial therapy (d), showing significant differences between survivor and non-survivor groups in a, b, c, d
PCT evolution along the last week of stay
The evolution of PCT levels for survivor and non-survivor groups in their last week of stay at CBU is presented in Table 4. A statistically significant difference was also demonstrated for this period of time (Fig. 2b and Table 6).
PCT evolution in the first week after suspicion of sepsis
A statistical analysis of PCT evolution in the first week after suspicion of sepsis, as defined by ABA criteria, was also carried out. Data are presented in Table 5. A significant difference between survivor and non-survivor groups was detected (Fig. 2c and Table 6).
In order to compare the relative prognostic value of PCT levels in each of the abovementioned periods (first week of hospitalization, last week of hospitalization, and first week after sepsis suspicion), statistical tests were done, namely Friedman test p value and Mann-Whitney U test p values with Sidak correction (Table 6).
Furthermore, the PS effect [25] was determined. The results are transcribed in Table 7.
PCT evolution with antimicrobial therapy
No statistically significant difference was found between the groups, but a within-group significant variation was detected, with a progressive decline along the first 7 days, supposedly due to antimicrobial action (Fig. 2d and Table 8). When the analysis was extended to the 15th day, it was found that PCT levels increased rapidly and steadily until the day of death in non-survivors, what did not happen in the survivor group, as seen in Fig. 3.
Discussion
Even acknowledging all advances in critical care, extensive burns are still associated with high morbidity and mortality mainly due to septic episodes [26, 27]. In the last years, diverse studies were published showing the utility of dosing PCT levels as an aid to the diagnosis of systemic infection in burn patients [28,29,30,31,32,33,34], particularly when a dynamic approach is used [35]. Notwithstanding the core decision should rely on the clinical features and never on a biomarker alone [36], PCT dosing may support the suspect of ongoing and uncontrolled systemic infection when its values keep rising, or at least does not subside in consecutive analysis, indicating that something must be done to control a probable septic process before it can lead to irreversible damage. Apart its potential to improve clinicians’ diagnostic capacity, PCT has been used with success at the emergency departments [37, 38], to predict the prognosis of suspected septic patients and to stratify them according to the risk of death and the necessity of admission in intensive care units (ICU) [39,40,41]. PCT levels at admission and, much more reliable [42], its evolution on subsequent days may give insights on the ultimate outcome, which is crucial to clinical management and may be of great importance to inform patient’s relatives and for judicial concerning [43,44,45,46,47]. This valuable predictive power was not found for C-reactive protein (CRP) or white blood cells counting, another currently employed blood biomarkers [48,49,50,51,52,53]. The prognostic power of PCT dosing has also been stated for burned patients by Kim et al. [54] who, in a prospective observational study with a cohort of 175 patients, showed a significant correlation between PCT levels and mortality rate. In this context, it is worth to note, as referred by Piroglu et al. [55], that clinical scoring systems used to predict mortality of intensive care patients, like Acute Physiology and Chronic Health Evaluation Score II (APACHE II), Simplified Acute Physiology Score (SAPS), Sequential Organ Failure Assessment (SOFA), and Pediatric Risk of Mortality (PRISM), do not include parameters specific for burn patients, and these authors showed that combination of the former score with PCT significantly increased its accuracy. A prospectively study of Lavrentieva et al. [31], including 145 patients, concluded that the maximum PCT level has prognostic value in burn patients, and Mokline et al. [32] found a close correlation of PCT levels with sepsis severity, showing that increasing values were linked with worse outcomes and vice versa.
Another important use of PCT dosing is guiding antimicrobial therapy in septic ICU patients, which is becoming generally accepted [56], supported by several trials [57,58,59,60,61,62], systematic reviews, and meta-analysis [63,64,65,66,67]; however, some authors still consider that more studies on its safety and efficacy are needed yet [68, 69]. Once a clinical suspicion of sepsis is done, and in particular if corroborated by abnormally elevated PCT levels, empirical antimicrobial therapy, coupled with focus control when feasible, must be immediately started because survival is mostly depending on it and any delay, even hourly, is directly related with an increase in mortality [13, 70, 71]. On the other hand, there is an overwhelming acceptation that a lengthening of antimicrobial therapy beyond that strictly necessary to control the infectious process favors the development of microbial resistance, contributing to the soaring public health risk of having each time less sensitive microorganisms and lack of antimicrobials to combat them [72]. Many published works describe PCT kinetics as a mirror of the evolution of the infectious episode [73,74,75] as well as a trustable indicator of the antimicrobial therapy efficacy, allowing an early de-escalation and/or stopping of drug administration when its levels progress and consistently subside [76, 77]. When PCT levels keep elevated or even increasing, this is a sound indication that therapy is not working and/or that there are still infectious foci to clean, and if the situation is not rapidly controlled, a bad outcome is foreseeable.
Several authors have discussed in recent works this use of PCT, and a body of evidence is growing to support this approach. Jensen et al. in a trial (PASS Study) [78] published in 2011 advised against PCT-guided antimicrobial escalation, linking it to increased organ-related harm and length of stay at the ICU, without improvement in the outcomes. However, the sample analyzed came from just one developed country with antimicrobial restriction and a traditionally low microbial resistance. On the other hand, focus was not put on the possibility of using PCT levels to help decision on antibiotherapy discontinuation neither a subgroup analysis on burn patients was done. Nevertheless, and even if antimicrobial escalation may be somewhat controversial, PCT has proven to be very useful to monitor antimicrobials efficacy, with its levels paralleling clinical evolution, and to indicate when it is safe to stop it without prejudice to the patients [79]. Indeed, this methodology has proved to safely decrease antimicrobial consumption [80] by reducing days of antimicrobial therapy with strong potential to lower resistance development. This approach has already been validated for use in ICUs, with proven reduction of antimicrobial consumption without increase in morbidity or mortality [81]. Indeed, de Jong et al., in the largest prospective study in ICU patients published to date (SAPS Study) [61], were even able to show a significant reduction of mortality rate. The ever wider diffusion of PCT test, reducing its costs, and its efficacy in this setting, made also possible for some authors to consider it as probably cost-effective [82,83,84,85,86]. In a recent paper, Lavrentieva et al. [87] reported significantly shorter durations of antibiotic treatment in a PCT-guided group of burns patients compared to controls without differences in main outcome characteristics, including mortality rate, length of mechanical ventilation, and length of stay.
Among the limitations of this study are naturally its single-center, retrospective observational character as well as lacking of subgroup analysis according to concomitant pathologies. The definition of a precise cutoff of PCT levels for predicting outcomes or stopping antimicrobial therapy was also beyond the scope of this analysis and, as recognized in the literature, it will always be dependent on patient characteristics and facility features, and it is PCT kinetics that deserved authors attention, in spite of 100 ng/mL was often taken as an alert signal. On the positive aspects are the sample size and the strict use of ABA burn sepsis definitions for inclusion criteria. The strength of results from the present study would be largely enhanced by a desirable prospective multicentric trial.
The use of prognostic biomarkers in order to predict outcomes as well for guiding antimicrobial therapy in sepsis patients is nowadays a common practice in intensive care wards. As anytime more acknowledged in the literature, antimicrobial stewardship programs employing current available biomarkers or preferably, a panel of diverse ones, always associated with repeated clinical evaluation, may decisively improve patients’ stratification and antimicrobial use, optimizing patients outcome, reducing the spread of microbial resistance, and cutting financial burden [88,89,90,91,92,93]. Meanwhile more sophisticated and individualized system-based (integrating genomics, metabolomics, and proteomics) [94,95,96] data are not available to more accurately predict outcomes and tailor treatment options for burn victims, as well as other intensive care patients, PCT dosing will remain one of the more useful tools to help clinicians decisions.
Conclusion
In spite of its limitations, the close correlation between PCT levels and patients’ outcomes statistically demonstrated in the present work backs its use for prognosis determination in severe burn patients. Additionally, this study showed that the persistency of abnormally elevated PCT along the days of antimicrobial therapy was linked with poor outcomes in this set of patients, opposed to what happens when their levels fall in a consistent way, reflecting its efficacy.
Prospective multicentric studies would surely give more strength to the generalization of PCT use for prognosis and antimicrobial stewardship in burn patients and are much needed.
References
Hidalgo F, Mas D, Rubio M, Garcia-Hierro P. Infections in critically ill burn patients. Med Int. 2016;40:179–85. https://doi.org/10.1016/j.medin.2016.02.001.
Yan S, Tsurumi A, Que YA, Ryan CM, Bandyopadhaya A, Morgan AA, et al. Prediction of multiple infections after severe burn trauma: a prospective cohort study. Ann Surg. 2015;261(4):781–92. https://doi.org/10.1097/SLA.0000000000000759.
Ruiz-Castilla M, Roca O, Masclans JR, Barret JP. Recent advances in biomarkers in severe burns. Shock. 2016;45:117–25. https://doi.org/10.1097/SHK.0000000000000497.
Marik PE. Don’t miss the diagnosis of sepsis! Crit Care. 2014;18:589. https://doi.org/10.1186/s13054-014-0529-6.
Vincent JL. Rapid diagnosis of infection in the critically ill, a multicenter study of molecular detection in bloodstream infections, pneumonia, and sterile site infections. Crit Care Med. 2015;43:2283–91. https://doi.org/10.1371/journal.pmed.1002022.
Mitsuma SF, Mansour MK, Dekker JP, Kim J, Rahman MZ, Tweed-Kent A, et al. Promising new assays and technologies for the diagnosis and management of infectious diseases. Clin Infect Dis. 2013;56:996–1002. https://doi.org/10.1093/cid/cis1014.
Tsangaris I, Plachouras D, Kavatha D, Gourgoulis GM, Tsantes A, Kopterides P, et al. Diagnostic and prognostic value of procalcitonin among febrile critically ill patients with prolonged ICU stay. BMC Infect Dis. 2009:213–21. https://doi.org/10.1186/1471-2334-9-213.
Shiferaw B, Bekele E, Kumar K, Boutin A, Frieri M. The role of procalcitonin as a biomarker in sepsis. J Inf Dis Epid. 2016;2:2006. https://doi.org/10.23937/2474-3658/1510006.
Gibot S, Bene MC, Noel R, Massin F, Guy J, Cravoisy A, et al. Combination biomarkers to diagnose sepsis in the critically ill patient. Am J Respir Crit Care Med. 2012;186:65–71. https://doi.org/10.1164/rccm.201201-0037OC.
Angeletti S, Battistoni F, Fioravanti M, Bernardini S, Dicuonzo G. Procalcitonin, MR-proadrenomedullin, and cytokines measurement in sepsis diagnosis: advantages from test combination. Dis Markers. 2015;2015:951532. https://doi.org/10.1155/2015/951532.
Yang Y, Xie J, Guo F, Longhini F, Gao Z, Huang Y, et al. Combination of C-reactive protein, procalcitonin and sepsis-related organ failure score for the diagnosis of sepsis in critical patients. Ann Intensive Care. 2016;6:51. https://doi.org/10.1186/s13613-016-0153-5.
Giacobbe DR, Mikulska M, Tumbarello M, Furfaro E, Spadaro M, Losito AR, et al. Combined use of serum (1, 3)-β-D-glucan and procalcitonin for the early differential diagnosis between candidaemia and bacteraemia in intensive care units. Crit Care. 2017;21:176. https://doi.org/10.1186/s13054-017-1763-5.
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96. https://doi.org/10.1097/01.CCM.0000217961.75225.E9.
Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH. Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother. 2005;49:1306–11. https://doi.org/10.1128/AAC.49.4.1306-1311.2005.
Linscheid P, Seboek D, Schaer DJ, Zulewski H, Keller U, Müller B. Expression and secretion of procalcitonin and calcitonin gene-related peptide by adherent monocytes and macrophage-activated adipocytes. Crit Care Med. 2004;32:1715–21. 15286549
Schuetz P, Raad I, Amin DN. Using procalcitonin-guided algorithms to improve antimicrobial therapy in ICU patients with respiratory infections and sepsis. Curr Opin Crit Care. 2013;19:453–60. https://doi.org/10.1097/MCC.0b013e328363bd38.
Gilbert DN. Use of plasma procalcitonin levels as an adjunct to clinical microbiology. J Clin Microbiol. 2010;48:2325–9. https://doi.org/10.1128/JCM.00655-10.
Cabral L, Afreixo V, Almeida L, Paiva JA. The use of procalcitonin (PCT) for diagnosis of sepsis in burn patients: a meta-analysis. PLoS One. 2016;11(12):e0168475. https://doi.org/10.1371/journal.pone.0168475.
Sandquist M, Wong HR. Biomarkers of sepsis and their potential value in diagnosis, prognosis and treatment. Expert Rev Clin Immunol. 2014;10:1349–56. https://doi.org/10.1586/1744666X.2014.949675.
Ruiz-Rodríguez JC, Caballero J, Ruiz-Sanmartin A, Ribas VJ, Pérez M, Bóveda JL, et al. Usefulness of procalcitonin clearance as a prognostic biomarker in septic shock. A prospective pilot study. Med Int. 2012;36:475–80. https://doi.org/10.1016/j.medin.2011.11.024.
Schuetz P, Maurer P, Punjabi V, Desai A, Amin DN, Gluck E. Procalcitonin decrease over 72 hours in US critical care predicts fatal outcomes in sepsis patients. Crit Care Res. 2013;28(6):776–90. https://doi.org/10.1097/BCR.0b013e3181599bc9.
Greenhalgh DG. Sepsis in the burn patient: a different problem than sepsis in the general population. Burns Trauma. 2017;5:23–32. https://doi.org/10.1186/s41038-017-0089-5.
Greenhalgh DG, Saffle JR, Holmes JH 4th, Gamelli RL, Palmieri TL, Horton JW, et al. American burn association consensus conference to define sepsis and infection in burns. J Burn Care Res. 2007;17:R115. https://doi.org/10.1097/BCR.0b013e3181599bc9.
Tobiasen J, Hiebert JM, Edlich RF. The abbreviated burn severity index. Ann Emerg Med. 1982;11:260–2.
Grissom RJ, Kim JJ. Effect sizes for research: univariate and multivariate applications. 2nd ed. New York: Taylor & Francis; 2012.
Williams FN, Herndon DN, Hawkins HK, Lee JO, Cox RA, Kulp GA, et al. The leading causes of death after burns injury in a single pediatric burn centre. Crit Care. 2009;13:183. https://doi.org/10.1186/cc8170.
Schultz L, Walker SA, Elligsen M, Walker SE, Simor A, Mubareka S, et al. Identification of predictors of early infection in acute burn patients. Burns. 2013;39:1355–66. https://doi.org/10.1016/j.burns.2013.04.009.
von Heimburg D, Stieghorst W, Khorram-Sefat R, Pallua N. Procalcitonin—a sepsis parameter in severe burn injuries. Burns. 1998;24:745–50.
Lavrentieva A, Kontakiotis T, Lazaridis L, Tsotsolis N, Koumis J, Kyriazis G, et al. Inflammatory markers in patients with severe burn injury: what is the best indicator of sepsis? Burns. 2007;33:189. https://doi.org/10.1016/j.burns.2006.07.001.
Mann EA, Wood GL, Wade CE. Use of procalcitonin for the detection of sepsis in the critically ill burn patient: a systematic review of the literature. Burns. 2011;37:549–58. https://doi.org/10.1016/j.burns.2010.04.013.
Lavrentieva A, Papadopoulou S, Kioumis J, Kaimakamis E, Bitzani M. PCT as a diagnostic and prognostic tool in burn patients. Whether time course has a role in monitoring sepsis treatment. Burns. 2012;38:356–63. https://doi.org/10.1016/j.burns.2011.08.021.
Mokline A, Garsallah L, Rahmani I, Jerbi K, Oueslati H, Tlaili S, et al. Procalcitonin: a diagnostic and prognostic biomarker of sepsis in burned patients. Ann Burns Fire Disasters. 2015;28:116–20. PMC:4837487
Ren H, Li Y, Han C, Hu H. Serum procalcitonin as a diagnostic biomarker for sepsis in burned patients: a meta-analysis. Burns. 2015;41:502–9. https://doi.org/10.1016/j.burns.2014.08.019.
Cabral L, Afreixo V, Santos F, Almeida L, Paiva JA. Procalcitonin for the early diagnosis of sepsis in burn patients: a retrospective study. Burns. 2017; https://doi.org/10.1016/j.burns.2017.
Egea-Guerrero J, Rodríguez-Rodríguez A. Sepsis biomarkers in severe burn patients: cut-off point or time profile? Med Int. 2016;40:595–6. https://doi.org/10.1016/j.medine.2016.11.003.
Vincent JL, Teixeira L. Sepsis biomarkers. Value and limitations. Am J Respir Crit Care Med. 2014;190:1081–2. https://doi.org/10.1164/rccm.201410-1895ED.
Huang DT, Weissfeld LA, Kellum JA, Yealy DM, Kong L, Martino M, et al. Risk prediction with procalcitonin and clinical rules in community-acquired pneumonia. Ann Emerg Med. 2008;52:48–58. https://doi.org/10.1016/j.annemergmed.2008.01.003.
Tromp M, Lansdorp B, Bleeker-Rovers CP, Gunnewiek JM, Kullberg BJ, Pickkers P. Serial and panel analyses of biomarkers do not improve the prediction of bacteremia compared to one procalcitonin measurement. J Inf Secur. 2012;65:292–301. https://doi.org/10.1016/j.jinf.2012.06.004.
Jain S, Sinha S, Sharma SK, Samantaray JC, Aggrawal P, Vikram NK, et al. Procalcitonin as a prognostic marker for sepsis: a prospective observational study. BMC Research Notes. 2014;7:458. https://doi.org/10.1186/1756-0500-7-458.
Liu D, Su L, Han G, Yan P, Xie L. Prognostic value of procalcitonin in adult patients with sepsis: a systematic review and meta-analysis. PLoS One. 2015;10:e0129450. https://doi.org/10.1371/journal.pone.0129450.
Claeys R, Vinken S, Spapen H, ver Elst K, Decochez K, Huyghens L, et al. Plasma procalcitonin and C-reactive protein in acute septic shock: clinical and biological correlates. Crit Care Med. 2002;30:757–62. 11940741
Mat-Nor MB, Ralib AM. Procalcitonin clearance for early prediction of survival in critical ill patients with severe sepsis. Crit Care Res Pract. 2014;2014 https://doi.org/10.1155/2014/819034.
Wunder C, Eichelbrönner O, Roewer N. Are IL-6, IL-10 and PCT plasma concentrations reliable for outcome prediction in severe sepsis? A comparison with APACHE III and SAPS II. Inflamm Res. 2004;53:158–63. https://doi.org/10.1007/s00011-003-1239-3.
Charles PE, Kus E, Aho S, Prin S, Doise JM, Olssonet NO, et al. Serum procalcitonin for the early recognition of nosocomial infection in the critically ill patients: a preliminary report. BMC Infect Dis. 2009;9:49. https://doi.org/10.1186/1471-2334-9-49.
Karlsson S, Heikkinen M, Pettilä V, Alila S, Väisänen S, Pulkki K, et al. Predictive value of procalcitonin decrease in patients with severe sepsis: a prospective observational study. Crit Care. 2010;14:R205. https://doi.org/10.1186/cc9327.
Giamarellos-Bourboulis EJ, Tsangaris I, Kanni T, Mouktaroudi M, Pantelidou I, Adamis G, et al. Procalcitonin as an early indicator of outcome in sepsis: a prospective observational study. J Hosp Infect. 2011;77:58–63. https://doi.org/10.1016/j.jhin.2010.07.026.
Ríos-Toro J-J, Márquez-Coello M, García-Álvarez J-M, Martín-Aspas A, Rivera-Fernández R, Sáez de Benito A, et al. Soluble membrane receptors, interleukin 6, procalcitonin and C reactive protein as prognostic markers in patients with severe sepsis and septic shock. PLoS One. 2017;12(4):e0175254. https://doi.org/10.1371/journal.pone.0175254.
Giamarellos-Bourboulis EJ, Mega A, Grecka P, Scarpa N, Koratzanis G, Thomopoulos G, et al. Procalcitonin: a marker to clearly differentiate systemic inflammatory response syndrome and sepsis in the critically ill patient? Intensive Care Med. 2002;28:1351–6. https://doi.org/10.1007/s00134-002-1398-z.
Pettilä V, Hynninen M, Takkunen O, Kuusela P, Valtonen M. Predictive value of procalcitonin and interleukin 6 in critically ill patients with suspected sepsis. Intensive Care Med. 2002;28:1220–5. https://doi.org/10.1007/s00134-002-1416-1.
Silvestre J, Póvoa P, Coelho L, Almeida E, Moreira P, Fernandes A, et al. Is C-reactive protein a good prognostic marker in septic patients? Intensive Care Med. 2009;35:909–13. https://doi.org/10.1007/s00134-009-1402-y.
Ciriello V, Gudipati S, Stavrou PZ, Kanakaris NK, Bellamy MC, Giannoudis PV. Biomarkers predicting sepsis in polytrauma patients: current evidence. Injury. 2013;44:1680–92. https://doi.org/10.1016/j.injury.2013.09.024.
Meisner M. Update on procalcitonin measurements. Ann Lab Med. 2014;34:263–73. https://doi.org/10.3343/alm.2014.34.4.263.
Lipińska-Gediga M, Mierzchała-Pasierb M, Durek G. Procalcitonin kinetics—prognostic and diagnostic significance in septic patients. Arch Med Sci. 2016;12:112–9. https://doi.org/10.5114/aoms.2016.57587.
Kim HS, Yang HT, Hur J, Chun W, Ju YS, Shin SH, et al. Procalcitonin levels within 48 hours after burn injury as a prognostic factor. Ann Clin Lab Sci. 2012;42:57–64. 22371911
Piroglu ID, Tulgar S, Piroglu MD, Thomas DT, Karakilic E, Gergeli K, et al. Do early procalcitonin levels aid in predicting mortality in burn patients? Int J Clin Exp Med. 2016;9:6947–6.
Sridharan P, Chamberlain RS. The efficacy of procalcitonin as a biomarker in the management of sepsis: slaying dragons or tilting at windmills? Surg Infect. 2014;14:489–511. https://doi.org/10.1089/sur.2012.028.
Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med. 2008;177:498–505. https://doi.org/10.1164/rccm.200708-1238OC.
Hochreiter M, Koehler T, Schweiger AM, Bein B, Keck FS, von Spiegel T. Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomized prospective controlled trial. Crit Care. 2009;13:R83. https://doi.org/10.1186/cc7903.
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375:463–74. https://doi.org/10.1016/S0140-6736(09)61879-1.
Georgopoulou AP, Savva A, Giamarellos-Bourboulis EJ, Georgitsi M, Raftogiannis M, Antonakos N, et al. Early changes of procalcitonin may advise about prognosis and appropriateness of antimicrobial therapy in sepsis. J Crit Care. 2011;26:331.e1–7. https://doi.org/10.1016/j.jcrc.2010.07.01.
de Jong E, van Oers JA, Beishuizen A, Vos P, Vermeijden WJ, Haas LE, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16:819–27. https://doi.org/10.1016/S1473-3099(16)00053-0.
Stocker M, van Herk W, el Helou S, Dutta S, Fontana MS, Schuerman FA, et al. Procalcitonin-guidede decision making for durations of antibiotic therapy in neonates with suspected early-onset sepsis: a multicentre, randomised controlled trial (NeoPIns). Lancet. 2017;390(10097):871–81. https://doi.org/10.1016/S0140-6736(17)31444-7.
Kopterides P, Siempos II, Tsangaris I, Tsantes A, Armaganidis A. Procalcitonin-guided algorithms of antibiotic therapy in the intensive care unit: a systematic review and meta-analysis of randomized controlled trials. Crit Care Med. 2010;38:2229–41. https://doi.org/10.1097/CCM.0b013e3181f17bf9.
Agarwal R, Schwartz DN. Procalcitonin to guide duration of antimicrobial therapy in intensive care units: a systematic review. Clin Infect Dis. 2011;53:379–87. https://doi.org/10.1093/cid/cir408.
Schuetz P, Chiappa V, Briel M, Greenwald JL. Procalcitonin algorithms for antibiotic therapy decisions: a systematic review of randomized controlled trials and recommendations for clinical algorithms. Arch Intern Med. 2011;171:1322–31. https://doi.org/10.1001/archinternmed.2011.318.
Heyland DK, Johnson AP, Reynolds SC, Muscedere J. Procalcitonin for reduced antibiotic exposure in the critical care setting: a systematic review and an economic evaluation. Crit Care Med. 2011;3:1792–9. https://doi.org/10.1097/CCM.0b013e31821201a5.
Prkno A, Wacker C, Brunkhorst FM, Schlattmann P. Procalcitonin-guided therapy in intensive care unit patients with severe sepsis and septic shock—a systematic review and meta-analysis. Crit Care. 2013;17:R291. https://doi.org/10.1186/cc13157.
Hoeboer SH, van der Geest PJ, Nieboer D, Groeneveld AB. The diagnostic accuracy of procalcitonin for bacteraemia: a systematic review and meta-analysis. Clin Microbiol Infect. 2015;21:474–81. https://doi.org/10.1016/j.cmi.2014.12.026.
Bloos F, Trips E, Nierhaus A, Briegel J, Heyland DK, Jaschinski U, et al. Effect of sodium selenite administration and procalcitonin-guided therapy on mortality in patients with severe sepsis or septic shock—a randomized clinical trial. JAMA Intern Med. 2016;176:1266–76. https://doi.org/10.1001/jamainternmed.2016.2514.
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42:1749–55. https://doi.org/10.1097/CCM.0000000000000330.
Weiss SL, Fitzgerald JC, Balamuth F, Alpern ER, Lavelle J, Chilutti M, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med. 2014;42:2409–17. https://doi.org/10.1097/CCM.0000000000000509.
Spellberg B, Gilbert DN. The future of antibiotics and resistance: a tribute to a career of leadership by John Bartlett. Clin Infect Dis. 59(Suppl 2):S71–5. https://doi.org/10.1093/cid/ciu392.
Schuetz P, Mueller B, Trampuz A. Serum procalcitonin for discrimination of blood contamination from bloodstream infection due to coagulase-negative staphylococci. Infection. 2007;35:352–5. https://doi.org/10.1007/s15010-007-7065-0.
Müller B, Harbarth S, Stolz D, Bingisser R, Mueller C, Leuppal J, et al. Diagnostic and prognostic accuracy of clinical and laboratory parameters in community-acquired pneumonia. BMC Infect Dis. 2007;7:10. https://doi.org/10.1186/1471-2334-7-10.
Becker KL, Snider R, Nylen ES. Procalcitonin in sepsis and systemic inflammation: a harmful biomarker and a therapeutic target. Br J Pharm. 2010;159:253–64. https://doi.org/10.1111/j.1476-5381.2009.00433.x.
Riedel S. Procalcitonin and the role of biomarkers in the diagnosis and management of sepsis. Diagn Microbiol Infect Dis. 2012;73:221–7. https://doi.org/10.1016/j.diagmicrobio.2012.05.002.
Sager R, Kutz A, Mueller B, Schuetz P. Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Medicine2017;15:15. https://doi.org/10.1186/s12916-017-0795-7.
Jensen JU, Hein L, Lundgren B, Bestle MH, Mohr TT, Andersen MH, et al. Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: a randomized trial. Crit Care Med. 2011;39:2048–58. https://doi.org/10.1097/CCM.0b013e31821e8791.
Rhee C. Using procalcitonin to guide antibiotic therapy. Open Forum Infect Dis. 2017;4(1):ofw249. https://doi.org/10.1093/ofid/ofw249.
Hohn A, Schroeder S, Gehrt A, Bernhardt K, Bein B, Wegscheider K, et al. Procalcitonin-guided algorithm to reduce length of antibiotic therapy in patients with severe sepsis and septic shock. BMC Infect Dis. 2013;13:158. https://doi.org/10.1186/1471-2334-13-158.
Soni NJ, Samson DJ, Galaydick JL, Vats V, Huang ES, Aronson L, et al. Procalcitonin-guided antibiotic therapy: a systematic review and meta-analysis. J Hosp Med. 2013;8:530–40. https://doi.org/10.1002/jhm.2067.
Wilke MH, Grube RF, Bodmann KF. The use of a standardized PCT-algorithm reduces costs in intensive care in septic patients—a DRG-based simulation model. Eur J Med Res. 2011;16:543–8. https://doi.org/10.1186/2047-783X-16-12-543.
Schuetz P. Economic evaluation of procalcitonin-guided antibiotic therapy in acute respiratory infections: a US health system perspective. Clin Chem Lab Med. 2015;53:583–92. https://doi.org/10.1515/cclm-2014-1015.
Kip M, Kusters R, Ijzerman M, Steuten L. A PCT algorithm for discontinuation of antibiotic therapy is a cost-effective way to reduce antibiotic exposure in adult intensive care patients with sepsis. J Med Econ. 2015;18:944–53. https://doi.org/10.3111/13696998.2015.1064934.
Steuten L, Mantjes G. Economic value of procalcitonin guidance. Lancet Infect Dis. 2016;16(9):1000. https://doi.org/10.1016/S1473-3099(16)30258-4.
Balk RA, Kadri SS, Cao Z. Effect of procalcitonin testing on health-care utilization Coste in critically ill patients in the United States. Chest. 2017;151:23–33. https://doi.org/10.1016/j.chest.2016.06.046.
Lavrentieva A, Kontou P, Soulountsi V, Kioumis J, Chrysou O, Bitzani M. Implementation of a procalcitonin-guided algorithm for antibiotic therapy in the burn intensive care unit. Ann Burns Fire Disasters. 2015;28:163–70. PMC4883599
Chamberlain RS, Shayota BJ, Nyberg C, Sridharan P. The utility of procalcitonin as a biomarker to limit the duration of antibiotic therapy in adult sepsis patients. Surg Sci. 2014;5(8):48679. https://doi.org/10.4236/ss.2014.58057.
Lam SW, Bauer SR, Dugga A. Procalcitonin-based algorithms to initiate or stop antibiotic therapy in critically ill patients: is it time to rethink our strategy? Int J Antimicrob Agents. 2016;47:20–7. https://doi.org/10.1016/j.ijantimicag.2015.10.017.
Schuetz P, Müeller B. Procalcitonin in critically ill patients: time to change guidelines and antibiotic use in practice. Lancet Infect Dis. 2016;16:758–60. https://doi.org/10.1016/S1473-3099(16)00064-5.
Vincent JL. The clinical challenge of sepsis identification and monitoring. PLoS Med. 2016;13(5):e1002022. https://doi.org/10.1371/journal.pmed.1002022.
Schuetz P, Müeller B. Procalcitonin-guided antibiotic stewardship from newborns to centennials. Lancet, 2017;390:826–9. https://doi.org/10.1016/S0140-6736(17)31628-8.
Paiva JA, Laupland KB. Real-time PCR for early microbiological diagnosis: is it time? Intensive Care Med. 2017; https://doi.org/10.1007/s00134-017-4793-1.
Mickiewicz B, Tam P, Jenne CN, Leger C, Wong J, Winston BW, et al. Integration of metabolic and inflammatory mediator profiles as a potential prognostic approach for septic shock in the intensive care unit. Crit Care. 2015;19:11. https://doi.org/10.1186/s13054-014-0729-0.
Hazeldine J, Hampson P, Lord JM. The diagnostic and prognostic value of systems biology research in major traumatic and thermal injury: a review. Burns Trauma. 2016;4:33. https://doi.org/10.1186/s41038-016-0059-3.
Nunez-Lopes O, Cambiaso-Daniel J, Branski LK, Norbury WB, Herndon DH. Predicting and managing sepsis in burn patients: current perspectives. Ther Clin Risk Manag. 2017;13:1107–17. https://doi.org/10.2147/TCRM.S119938.
Acknowledgements
The authors acknowledge Dr. Filipe Santos, from the National Statistical Institute of Portugal (Instituto Nacional de Estatítisca (INE)), for his technical help in the gathering of data and making of some graphics.
Funding
VA work was supported by Portuguese funds through the Center for Research and Development in Mathematics and Applications (CIDMA) by the Portuguese Foundation for Science and Technology (Fundação para a Ciência e a Tecnologia (FCT)), within project ID/MAT/04106/2013.
On behalf of all the other authors, the corresponding author states that none of them has received any funding for this work.
Availability of data and materials
The data that support the findings of this study are available from the datasets of the Informatics Department of Coimbra University Hospital Centre but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors, upon a reasonable request and after permission of the Ethics Committee from Coimbra University Hospital Centre.
Author information
Authors and Affiliations
Contributions
LC and VA designed the study, interpreted the data, and draft the manuscript. VA was responsible for most of the statistical analysis. RM, MV, CC, and MC were responsible for the data acquisition, search of literature, and made suggestions for its integration along the manuscript. CC and MC made also substantial intellectual contributions for the “Background” and “Discussion” sections of the manuscript. LA and JAP reviewed the manuscript and made useful suggestions for the “Discussion” and “Conclusions” sections. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Being a retrospective observational study of patients from an anonymized dataset, involving only recording data from the medical record, the Ethics Committee from Coimbra University Hospital Centre (CHUC) waived the need of informed consent according to the Declaration of Helsinki and the Council for International Organizations of Medical Sciences (CIOMS) International Ethics Guidelines.
Consent for publication
As all data was anonymized, this study does not contain any individual person’s data in any form (including individual details, images, or videos) and accordingly consent for publication was waived.
Competing interests
The authors declare that they have no competing interests.
Additional file
Additional file 1:
Annex 1. Abbreviated Burn Severity Index. (DOCX 19 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cabral, L., Afreixo, V., Meireles, R. et al. Checking procalcitonin suitability for prognosis and antimicrobial therapy monitoring in burn patients. Burn Trauma 6, 10 (2018). https://doi.org/10.1186/s41038-018-0112-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41038-018-0112-5