Abstract
Backgrounds
To explore the genetic correlation between schizophrenia (SCZ) and osteoporosis (OP).
Design, setting, participants, measurements
We conducted a trans-ethnic two-stage genetic correlation analysis of OP and SCZ, totally invoking 2286 Caucasia subjects in discovery stage and 4124 Chinese subjects in replication stage. The bone mineral density (BMD) and bone area values of ulna & radius, hip and spine were measured using Hologic 4500W dual energy X-ray absorptiometry machine. SCZ was diagnosed according to DSM-IV criteria. For the genome-wide association study (GWAS) of Caucasian OP, Chinese OP and Chinese SCZ, SNP genotyping was performed using Affymetrix SNP 6.0 array. For the GWAS of Caucasian SCZ, SNP genotyping was conducted using the Affymetrix 5.0 array, Affymetrix 6.0 array and Illumina 550 K array. Polygenetic risk scoring (PRS) analysis was conducted by PRSice software. Also, Linkage disequilibrium score regression (LD Score regression) analysis was performed to evaluate the genetic correlation between OP and SCZ. Multi-trait analysis of GWAS (MTAG) was performed to detect novel candidate genes for osteoporosis and SCZ.
Results
In the Caucasia discovery samples, significant genetic correlations were observed for ulna & radius BMD vs. SCZ (P value = 0.010), ulna & radius area vs. SCZ (P value = 0.031). In the Chinese replication samples, we observed significant correlation for ulna & radius area vs. SCZ (P value = 0.019). In addition, LD Score regression also identified significant genetic correlations between SCZ and bone phenotypes in Caucasian and Chinese sample respectively. MTAG analysis identified several novel candidate genes, such as CTNNA2 (MTAG P value = 2.24 × 10−6) for SCZ and FADS2 (MTAG P value = 2.66 × 10−7) for osteoporosis.
Conclusions
Our study results support the overlapped genetic basis for osteoporosis and SCZ, and provide novel clues for elucidating the biological mechanism of increased osteoporosis risk in SCZ patients.
Similar content being viewed by others
Background
Schizophrenia (SCZ) is a psychiatric disorder characterized by delusions, hallucinations and cognitive deficits [1]. The estimated life time risk of SCZ is about 1% in the general population [2]. SCZ usually first occurs in the young adulthood with ages ranging from 16 to 30 years. The clinical manifestations of SCZ mainly include false beliefs, confused thinking, phonism, reduced social engagement and emotional expression. SCZ patients usually have additional mental problems, such as depressive, anxiety and substance-use disorders. It has been demonstrated that SCZ is a highly heritable psychiatric disorder [2, 3]. The estimated heritability of SCZ achieved 31% and 44% for nuclear and extended families [4]. Extensive efforts have been paid to reveal the genetic basis of SCZ as well as it genetic relationships with other diseases or traits, such as amyotrophic lateral sclerosis [5], smoking behaviors [6] and age at first birth in women [7].
Osteoporosis (OP) is a metabolic bone disease mainly characterized by low bone mass and high bone fragility [8, 9]. Osteoporosis is one of the most serious public health problems around the world, resulting in millions of fractures annually, high mortality and excessive therapeutic cost [10, 11]. Bone mineral density (BMD) is the most widely used predictor for osteoporosis with estimated heritability more than 50% [12]. Significant genetic correlations have been observed between osteoporosis and other disorders, such as coronary artery disease [13] and Kashin-Beck disease (KBD) [14].
It has been reported that SCZ patients exhibited increased risk of osteoporosis [15, 16]. This phenomenon was originally attributed to polydipsia and increased urinary calcium excretion in SCZ patients [17]. However, inconsistent results were reported by the following studies [18]. Subsequently, antipsychotics treatment was regarded as an important cause of the correlation between osteoporosis and SCZ [19,20,21]. But no significant relevance of antipsychotics use with SCZ was also reported in the SCZ patients undergoing antipsychotic treatment for a long time [22]. Additionally, eating disorder, lack of sunlight exposure and insufficient exercise caused by negative symptom were suggested to increase the risk of osteoporosis in SCZ patients [23]. But the biological mechanism underlying the correlation between osteoporosis and SCZ remains elusive now. Given the complicated biological processes implicated in the development of osteoporosis and SCZ, it was suggested that multiple factors should be considered for understanding the relationships between osteoporosis and SCZ [23]. Recently, the genetic correlations of complex diseases are extensively explored, demonstrating the generality of shared genetic basis among various complex disorders [24]. Given the high heritability and clinically observed correlation of osteoporosis and SCZ [4, 12, 15, 16], it is interesting and helpful to investigate the genetic relationship between osteoporosis and SCZ. However, to the best of our knowledge, few efforts have been paid to explore the possible genetic basis shared by osteoporosis and SCZ.
In this study, a trans-ethnic two-stage genetic correlation analysis of osteoporosis and SCZ was first conducted, totally invoking 2286 Caucasian subjects in discovery stage and 4124 Chinese subjects in replication stage. Multi-trait analysis of genome-wide association study (GWAS) approach was then applied to the GWAS summary datasets of osteoporosis and SCZ to detect novel candidate genes for osteoporosis and SCZ. We hope that our study results provide novel clues for understanding the biological mechanism underlying the relationship between osteoporosis and SCZ.
Materials and methods
Ethics statement
This study was approved by the Institutional Review Board of Xi’an Jiaotong University and University of Missouri-Kansas City. Signed informed-consent documents were obtained from all study participants before entering the study.
Caucasians discovery samples for osteoporosis (Caucasian OP)
A total of 2286 unrelated Caucasians subjects living in Kansas City and its surrounding areas were collected. Nurse-administered questionnaires were used to obtain the clinical data of each study subject, including self-reported ethnicities, lifestyle characteristics, health statuses, family and medical histories. We excluded the subjects with chronic diseases, conditions and drug use that might affect bone growth and metabolism. Hologic 4500W dual energy X-ray absorptiometry (Hologic Inc., Bedford, MA, USA) was used to measure the BMD and bone areas at ulna & radius, hip and spine. SNP genotyping was performed using Genome-Wide Human SNP Array 6.0 (Affymetrix, Santa Clara, CA, USA). Arrays were scanned using GeneChip Scanner 3000 7G. For quality control, we excluded the SNPs with Hardy–Weinberg equilibrium (HWE) testing P values < 0.0001 and minor allele frequencies (MAF) < 0.01 and genotyping call rate < 95% in this study. Detailed description of sample characteristics, experimental design and quality control can be found in our previous study [25].
Chinese replication samples for osteoporosis (Chinese OP)
The Chinese replication GWAS samples of osteoporosis consists of 1627 Han Chinese subjects (including 802 males and 825 females), collecting at Xi’an city and Changsha city of China. Nurse-administered questionnaires were used to obtain the clinical data of each study subject, including self-reported ethnicities, lifestyle characteristics, health statuses, family and medical histories. We excluded the subjects with chronic diseases and conditions that might affect bone growth and metabolism. The BMD and bone area values of ulna & radius, hip and spine were measured using Hologic 4500W dual energy X-ray absorptiometry machine (Hologic Inc., Bedford, MA, USA). Genome-wide SNP genotyping was performed using Genome-Wide Human SNP Array 6.0 (Affymetrix, Santa Clara, CA, USA), and scanned using the GeneChip Scanner 3000 7G. For quality control, the SNPs with HWE testing P value < 0.0001, MAF < 0.01 and genotyping call rate < 95% were excluded from this study. Detailed description of sample characteristics, experimental design and quality control can be found in our previous study [26].
Chinese replication sample for SCZ (Chinese SCZ)
The Chinese SCZ samples were collected at the First Affiliated Hospital of Xi’an Jiaotong University. It consists of 1475 SCZ patients and 1022 unrelated healthy controls. Nurse-administered questionnaires were used to obtain the clinical data of each study subject, including self-reported ethnicities, lifestyle characteristics, health statuses, family and medical histories. SCZ was diagnosed according to according to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV criteria by two psychiatrists [27]. We excluded the subjects with other psychiatric disorders, conditions and drug use that might affect mental status. Genome-wide SNP genotyping was performed using Genome-Wide Human SNP Array 6.0 (Affymetrix, Santa Clara, CA, USA), and scanned using the GeneChip Scanner 3000 7G. For quality control, the SNPs with HWE testing P value < 0.0001, MAF < 0.01 and genotyping call rate < 95% were excluded from this study.
GWAS summary dataset 1 of SCZ (GWASSCZ1)
The Caucasian GWAS summary data of SCZ was driven from a large-scale GWAS meta-analysis of SCZ [2]. Briefly, this GWAS dataset comprised of 49 non-overlapping case–control samples (including 34,241 cases and 45,604 controls from 46 cohorts of European and 3 cohorts of East Asian ancestry) and 3 family-based samples (including 1235 parent affected-offspring trios from 17 separate GWAS of European ancestry). Genotyping was originally conducted using commercial platforms, such as Affymetrix 5.0 array, Affymetrix 6.0 array and Illumina 550K array. Genotypes from all studies were processed by the Psychiatric Genomics Consortium (PGC) using unified quality control procedures. Meta-analysis of all individual GWAS was performed using an inverse-weighted fixed effects model. Detailed description of sample characteristics, experimental design, statistical analysis and quality control can be found in the previous study [2].
Polygenetic risk scoring (PRS) analysis
PRS analysis is a powerful approach and widely applied for detecting shared genetic aetiology among traits [4]. PRSs are an estimate of disease risk conducted by the individual based on the risk alleles and the corresponding effect sizes obtained from the GWAS summary statistics. PRS analysis uses the beta coefficients from the GWAS as weight for each SNP allele in order to calculate an overall risk score for each individual subject in an independent sample.
PRS analysis of Caucasian OP vs. GWASSCZ1 and Chinese OP vs. Chinese SCZ were conducted by the PRSice software, respectively (https://github.com/choishingwan/PRSice) [28]. PRSice performs clumping to remove ambiguous SNPs that are in LD with each other as a default [28]. Furthermore, it can calculate PRS at any number of P-value thresholds in order to provide the most predictive (precise) threshold and best-fit PRS [28]. By utilizing the GWAS results of base traits, and individual genotyping data of target traits, PRSice is capable of calculating the PRS of the base phenotype, and then the calculated PRS were used as the predictors of the target phenotype in a regression model [29].
Linkage disequilibrium score regression (LD Score regression)
Following the standard approach recommended by the developers, LD Score regression software (https://github.com/bulik/ldsc) was used here to evaluate the genetic correlation between OP and SCZ in Caucasian discovery samples and Chinese replication samples separately. LD Score regression is a powerful approach for genetic correlation analysis of complex diseases or traits [30]. LD Score regression is robust to the confounding biases caused by cryptic relatedness and population stratification. Inflated distribution of test statistics in GWAS can be caused by polygenicity (many small genetic effects) and confounding biases (cryptic relatedness and population stratification) [30]. LD Score regression can quantify these differences and the contribution of each factor by detecting regression relationships between linkage disequilibrium and test statistics [30].
Besides the PRS, LD Score regression provides an alternative way to measure the genetic correlation between BMD and SCZ. In PRS analysis, in order to optimize prediction power, only the significant SNPs were used, while LD Score regression analysis utilized whole genome SNPs data for genetic correlation analysis.
Multi-trait analysis of GWAS
Utilizing the GWAS summary datasets of Chinese OP and Chinese SCZ, MTAG approach was applied to identify novel candidate genes for osteoporosis and SCZ [31]. MTAG extended the inverse-variance-weighted meta-analysis to jointly analyze the GWAS summary data of multiple traits (https://github.com/omeed-maghzian/mtag). MTGA can integrate the information contained in the GWAS summaries of related traits, and increase the statistical power for detect novel causal loci for each trait analyzed [31]. MTAG will output trait-specific SNP association testing statistics for OP and SCZ, respectively. Real data analysis results demonstrated the good performance of MTAG for identifying novel causal loci for genetically correlated complex diseases [31].
Functional gene sets enrichment analysis
Identified candidate genes for each pair of SCZ and osteoporosis related traits were subjected to gene set enrichment analysis, implemented by the GENE2FUNC of the FUMA tool. FUMA is a platform [32] that has been widely used to annotate, prioritize, visualize and interpret GWAS findings [33]. For every input gene, GENE2FUNC provides information about tissue specificity, the enrichment of publicly available gene sets, and the expression of different tissue types. Significant gene sets were chosen with an adjusted P value < 0.05.
Results
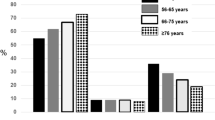
Table 1 summarizes the polygenetic risk scoring analysis results both of Caucasian discovery samples and Chinese replication samples. We observed genetic associations between osteoporosis phenotypes (ulna & radius area) and SCZ in both discovery and replication samples, suggesting the common genetic factors shared by osteoporosis and SCZ.
In the Caucasian discovery samples (Caucasian OP vs. GWASSCZ1), significant genetic correlations were observed for ulna & radius BMD vs. SCZ (P value = 0.010) and ulna & radius area vs. SCZ (P value = 0.031). In the replication study of Chinese OP vs. Chinese SCZ, significant correlation was observed for ulna & radius area vs. SCZ (P value = 0.019), as well as suggestive correlation signals for Hip total BMD vs. SCZ (P value = 0.061) and Hip neck BMD vs. SCZ (P value = 0.061).
For LD Score regression analysis, as expected, we found significant genetic correlation between hip total BMD and SCZ (P value = 0.0272) in Caucasians discovery samples. In Chinese replication samples, two significant genetic correlation signals were also observed, including ulna & radius BMD vs. SCZ (P value = 0.0042), whole body BMD vs. SCZ (P value = 0.0027).
To detect novel candidate genes for osteoporosis and SCZ, we conducted MTAG analysis utilizing the Chinese GWAS summarizes of BMD, bone and SCZ. For each pair of SCZ and osteoporosis related traits, MTGA output SNP association testing statistics for each analyzed trait, respectively. MTAG analysis results were summarized in Table 2. For osteoporosis-related traits, the most strong association signal was observed at the rs174577 of FADS2 gene (MTAG P value = 2.66 × 10−7). For SCZ, the most strong association signal was observed at the rs17018359 of CTNNA2 gene (MTAG P value = 2.24 × 10−6).
In addition, we performed FUMA analysis for seven pairs of SCZ and osteoporosis related traits, including Hip total area vs. SCZ, Hip total BMD vs. SCZ, Hip neck Area vs. SCZ, Hip neck BMD vs. SCZ, Spine area vs. SCZ, Spine BMD vs. SCZ, ulna & radius area vs. SCZ, respectively. FUMA analysis detected multiple candidate gene sets or pathways for the identified seven associations (Additional file 1: Table S1, Additional file 2: Table S2, Additional file 3: Table S3, Additional file 4: Table S4, Additional file 5: Table S5, Additional file 6: Table S6, Additional file 7: Table S7). Among them, the results of Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway were summarized at Table 3.
Discussions
To the best of our knowledge, few efforts have been paid to investigate the genetic relationships between osteoporosis and SCZ. In our study, a trans-ethnic two-stage genetic correlation analysis of osteoporosis OP and SCZ was performed. In the first stage, we conducted a PRS analysis to test the association between SCZ and OP in Caucasian discovery samples and replicated in Chinese replication samples. In short, we calculated SCZ-PRS to predict OP status in Caucasian discovery samples while used OP-PRS to predict SCZ status in Chinese replication samples. PRS analysis is a powerful approach, and widely used in current genetic studies of human complex diseases or traits [34, 35]. In addition, we also perform the LD score regression analysis, a genome-wide genetic correlation analysis, between BMD and SCZ in Chinese and Caucasian subject, respectively. In the second stage, we performed MTAG [31] analysis to detect novel candidate genes for OP and SCZ, respectively. And then these identified candidate genes for each pair of SCZ and osteoporosis related traits were subjected to gene set enrichment analysis via FUMA. We hope that our study results provide novel clues for understanding observed clinical correlation between osteoporosis and SCZ.
It has been a long time that researchers observed increased risks of osteoporosis in SCZ patients [15, 16]. Different hypothesis have been proposed, such as antipsychotics treatment, lack of sunlight exposure and insufficient exercise [23]. However, to the best of our knowledge, limited studies were conducted to figure out the potential genetic relationship between osteoporosis and SCZ. In this study, we observed genetic correlations between multiple osteoporosis-related traits and SCZ, suggesting the common genetic mechanism shared by osteoporosis and SCZ.
SNPs that were common in two or more populations often differed significantly in frequency between populations [36]. Even if alleles have similar frequencies among different populations, the effects of alleles on risk might be specific to certain populations. For causal variants, there are many reasons for the heterogeneity of genetic effects across populations, including clinical heterogeneity, differences in pathophysiology, gene–environment interaction and gene–gene interactions [37]. Recently, Lam et al. and his colleagues compared the genetic architectures of SCZ in two major world populations-East Asian and European samples, and the results indicating the common variant genetic architecture of SCZ outside of the major histocompatibility complex (MHC) region is highly consistent across East Asian and European populations [37]. Nevertheless, they also found the polygenic risk calculated for East Asians are different from the Europeans, which can be explained by ancestry-related differences in allele frequencies, LD and other factors [37]. In addition, existing studies showed there are some differences for osteoporosis between East and West. For example, the secular changes in hip fracture rates differed between East and West, with rates currently declining in North America, Oceana, Northern Europe, Hong Kong, Taiwan, and in most of Central Europe, but with increasing rates of hip fractures in much of Asia, Southern Europe, and South America, indicating close relationships between rising rates of urbanization and hip fractures across disparate geographic locations and cultures [38]. Another study identified significantly differentially expressed genes in circulating monocytes between the high and low BMD groups in Chinese Han females and validated the significant expression in Caucasian women, and they found STAT1 gene was upregulated in the low and the high BMD groups in both Chinese and Caucasians [39]. Furthermore, they also found COL1A1 gene may have significantly association with bone geometry in both Caucasians and Chinese, but AHSG gene may be linked to bone geometry in Caucasians, not in Chinese [40]. These evidences showed there might be a similar pattern between Chinese population and West population. In this study, we observed the genetic correlation of OP-related phenotypes and SCZ in Caucasians population and validated it in the Chinese population.
The potential molecular mechanism of the genetic correlation between osteoporosis and SCZ was largely unknown now. Recent studies may provide some helpful clues. For instance, it is well known that vitamin D and vitamin D metabolism related genes play import roles in the development of bone and osteoporosis [41]. Valipour et al. observed strong association between serum vitamin D level and schizophrenia [42]. Amato et al. detected significant overlap between vitamin D metabolism related genes and SCZ associated genes [43]. Additionally, Beydoun et al. found that vitamin D status was negatively correlated with cognitive decline in US urban adults [44]. Coşkun et al. observed significant association between vitamin D receptor gene polymorphism and the risk of autism spectrum disorder [45]. Mokry et al. evaluated the impact of vitamin D metabolism associated genes on the risks of Alzheimer disease [46]. Their genetic analysis results support 25-hydroxyvitamin D as a causal risk factor for Alzheimer disease [46].
The genetic correlation between osteoporosis and SCZ may also attribute to the exposure of common environment risk factors, such cigarette smoking and alcohol drinking, which are under genetic control. The significant impact of cigarette smoking and alcohol drinking on the development of osteoporosis has been well documented [47]. Furthermore, GWAS found that the risk of schizophrenia was associated with a cluster of genes (CHRNA5, CHRNA3 and CHRNB5) on chromosome 15 [2], which was also suggested to be associated with both early age at onset of cigarette smoking and heavy cigarette smoking [48, 49]. Alcohol drinking disorder is the most common co-occurring disorder in the people with SCZ [50]. GWAS also detected alcohol drinking associated genetic loci, the most robust ones of which were in GABAergic system GABRA2 and alcohol-metabolizing enzymes ALDH2, ADH1B, and ADH1C [51, 52]. Zai et al. suggested that neural plasticity and transmission related genes BDNF and DRD3 gene polymorphisms were significantly associated with alcohol drinking in SCZ patients [53].
MTAG analysis also identified several candidate genes for osteoporosis and SCZ. For instance, we found that CTNNA2 was associated with SCZ in this study. CTNNA2 encodes catenin alpha 2 protein, which was suggested as a candidate genes for SCZ [54]. CTNNA2 is critical for maintaining the stability of dendritic spines in rodent hippocampal neurons [55]. CTNNA2 knockout mice exhibited hippocampal pyramidal cell disorganization and deficits in prepulse inhibition of the startle response, which were also observed in SCZ patients [56]. It is more interesting that cigarette smoking was capable of regulating the expression of CTNNA2 in SCZ patients [57].
In this study, we aimed to explain the relationship between SCZ and OP from the perspective of genetics, which was usually not affected by the environmental confounding factors. Using the powerful PRS and MTAG approaches, we explored the genetic association of SCZ and OP in both Caucasian discovery samples and Chinese replication samples. Furthermore, the large sample sizes and discovery-replication study design ensured the accuracy of our study results. As far as we know, this is the first systemic study exploring the potential association between SCZ and OP from the genetic term, and this is the main difference between our study and previous study.
Several issues of this study should be noted. First, the Chinese replication sample sizes for osteoporosis (1627 subjects) and SCZ (2497 subjects) was relatively small in the MTAG analysis. The candidate genes identified by MTAG for osteoporosis and SCZ should be interpreted with caution. Second, the observed genetic correlations between osteoporosis and SCZ appeared to be skeletal site specific, mainly limited to ulna & radius and hip. Skeletal site specific effects of genetic factors on skeletal growth & development and osteoporosis had been demonstrated in previous genetic studies [58, 59]. Also, as an important limitation of our study, the target molecules identified in our study should be validated in mechanism-based studies. In the further analysis, cells as well as animal experiments and annotation analysis are warranted to confirm our finding and clarify the biological mechanism of the identified molecules contributing to the development of SCZ and OP in our study.
In conclusion, we conducted a trans-ethnic two-stage genetic correlation analysis of osteoporosis and SCZ. We observed genetic correlations between multiple osteoporosis related traits and SCZ, suggesting the overlapped genetic mechanism shared by osteoporosis and SCZ. We hope that our study results may help to elucidate the mechanism of increased osteoporosis risk in SCZ patients.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SCZ:
-
Schizophrenia
- OP:
-
Osteoporosis
- GWAS:
-
Genome-wide association study
- MTAG:
-
Multi-trait analysis of GWAS
- BMD:
-
Bone mineral density
- MAF:
-
Minor allele frequencies
- PGC:
-
Psychiatric Genomics Consortium
- PRSice:
-
Polygenic risk score software
References
Vita A, Barlati S, De Peri L, Deste G, Sacchetti E (2016) Schizophrenia. Lancet 388:1280
Schizophrenia Working Group of the Psychiatric Genomics C (2014) Biological insights from 108 schizophrenia-associated genetic loci. Nature. 511:421–427
Owen MJ, Sawa A, Mortensen PB (2016) Schizophrenia. Lancet 388:86–97
Light G, Greenwood TA, Swerdlow NR et al (2014) Comparison of the heritability of schizophrenia and endophenotypes in the COGS-1 family study. Schizophr Bull 40:1404–1411
McLaughlin RL, Schijven D, van Rheenen W et al (2017) Genetic correlation between amyotrophic lateral sclerosis and schizophrenia. Nat Commun 8:14774
Hartz SM, Horton AC, Hancock DB et al (2017) Genetic correlation between smoking behaviors and schizophrenia. Schizophr Res 194:86–90
Mehta D, Tropf FC, Gratten J et al (2016) Evidence for genetic overlap between schizophrenia and age at first birth in women. JAMA Psychiatry. 73:497–505
Medina-Gomez C, Kemp JP, Trajanoska K et al (2018) Life-course genome-wide association study meta-analysis of total body BMD and assessment of age-specific effects. Am J Hum Genet 102:88–102
Hu Y, Tan LJ, Chen XD et al (2018) Identification of novel potentially pleiotropic variants associated with osteoporosis and obesity using the cFDR method. J Clin Endocrinol Metab 103:125–138
Shepstone L, Lenaghan E, Cooper C et al (2017) Screening in the community to reduce fractures in older women (SCOOP): a randomised controlled trial. Lancet. 391:741–747
Zhao LJ, Liu XG, Liu YZ et al (2010) Genome-wide association study for femoral neck bone geometry. J Bone Miner Res 25:320–329
Ralston SH, Uitterlinden AG (2010) Genetics of osteoporosis. Endocr Rev 31:629–662
Peng C, Shen J, Lin X et al (2017) Genetic sharing with coronary artery disease identifies potential novel loci for bone mineral density. Bone 103:70–77
Wen Y, Guo X, Hao J et al (2016) Integrative analysis of genome-wide association studies and gene expression profiles identified candidate genes for osteoporosis in Kashin-Beck disease patients. Osteoporos Int 27:1041–1046
Halbreich U, Palter S (1996) Accelerated osteoporosis in psychiatric patients: possible pathophysiological processes. Schizophr Bull 22:447–454
Lee TY, Chung MY, Chung HK, Choi JH, Kim TY, So HS (2010) Bone density in chronic schizophrenia with long-term antipsychotic treatment: preliminary study. Psychiatry Investig 7:278–284
Delva NJ, Crammer JL, Jarzylo SV et al (1989) Osteopenia, pathological fractures, and increased urinary calcium excretion in schizophrenic patients with polydipsia. Biol Psychiatry 26:781–793
Wyszogrodzka-Kucharska A, Rabe-Jablonska J (2005) Calcium balance and regulation in schizophrenic patients treated with second generation antipsychotics. Psychiatria Pol 39:1157–1171
Keely EJ, Reiss JP, Drinkwater DT, Faiman C (1997) Bone mineral density, sex hormones, and long-term use of neuroleptic agents in men. Endocr Pract 3:209–213
Halbreich U, Rojansky N, Palter S et al (1995) Decreased bone mineral density in medicated psychiatric patients. Psychosom Med 57:485–491
Gammon GD (1981) Neuroleptics and decreased bone density in women. Am J Psychiatry 138:1517
Howes OD, Wheeler MJ, Meaney AM et al (2005) Bone mineral density and its relationship to prolactin levels in patients taking antipsychotic treatment. J Clin Psychopharmacol 25:259–261
Halbreich U (2007) Osteoporosis, schizophrenia and antipsychotics: the need for a comprehensive multifactorial evaluation. CNS Drugs 21:641–657
Bulik-Sullivan B, Finucane HK, Anttila V et al (2015) An atlas of genetic correlations across human diseases and traits. Nat Genet 47:1236–1241
Yang TL, Guo Y, Li J et al (2013) Gene-gene interaction between RBMS3 and ZNF516 influences bone mineral density. J Bone Miner Res 28:828–837
Deng FY, Lei SF, Chen XD, Tan LJ, Zhu XZ, Deng HW (2011) An integrative study ascertained SOD2 as a susceptibility gene for osteoporosis in Chinese. J Bone Miner Res 26:2695–2701
Li Z, Chen J, Yu H et al (2017) Genome-wide association analysis identifies 30 new susceptibility loci for schizophrenia. Nat Genet 49:1576–1583
Euesden J, Lewis CM, O’Reilly PF (2015) PRSice: polygenic Risk Score software. Bioinformatics 31:1466–1468
Ruisch IH, Dietrich A, Klein M et al (2020) Aggression based genome-wide, glutamatergic, dopaminergic and neuroendocrine polygenic risk scores predict callous-unemotional traits. Neuropsychopharmacology. https://doi.org/10.1038/s41386-020-0608-0
Bulik-Sullivan BK, Loh P-R, Finucane HK et al (2015) LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet 47:291–295
Turley P, Walters RK, Maghzian O et al (2018) Multi-trait analysis of genome-wide association summary statistics using MTAG. Nat Genet 50:229–237
Watanabe K, Taskesen E, van Bochoven A, Posthuma D (2017) Functional mapping and annotation of genetic associations with FUMA. Nat Commun 8:1826
Howles SA, Wiberg A, Goldsworthy M et al (2019) Genetic variants of calcium and vitamin D metabolism in kidney stone disease. Nat Commun 10:5175
Duncan L, Shen H, Gelaye B et al (2019) Analysis of polygenic risk score usage and performance in diverse human populations. Nat Commun 10:3328
Markota M, Coombes BJ, Larrabee BR et al (2018) Association of schizophrenia polygenic risk score with manic and depressive psychosis in bipolar disorder. Transl Psychiatry 8:188
Guthery SL, Salisbury BA, Pungliya MS, Stephens JC, Bamshad M (2007) The structure of common genetic variation in United States Populations. Am J Hum Genet 81:1221–1231
Lam M, Chen C-Y, Li Z et al (2019) Comparative genetic architectures of schizophrenia in East Asian and European populations. Nat Genet 51:1670–1678
Ballane G, Cauley JA, Luckey MM, Fuleihan GEH (2014) Secular trends in hip fractures worldwide: opposing trends east versus west. J Bone Miner Res 29:1745–1755
Chen XD, Xiao P, Lei S-F et al (2010) Gene expression profiling in monocytes and SNP association suggest the importance of the STAT1 gene for osteoporosis in both Chinese and Caucasians. J Bone Miner Res 25:339–355
Jiang H, Lei SF, Xiao SM et al (2007) Association and linkage analysis of COL1A1 and AHSG gene polymorphisms with femoral neck bone geometric parameters in both Caucasian and Chinese nuclear families. Acta Pharmacol Sin 28:375–381
Xu XH, Dong SS, Guo Y et al (2010) Molecular genetic studies of gene identification for osteoporosis: the 2009 update. Endocr Rev 31:447–505
Valipour G, Saneei P, Esmaillzadeh A (2014) Serum vitamin D levels in relation to schizophrenia: a systematic review and meta-analysis of observational studies. J Clin Endocrinol Metab 99:3863–3872
Amato R, Pinelli M, Monticelli A, Miele G, Cocozza S (2010) Schizophrenia and vitamin D related genes could have been subject to latitude-driven adaptation. BMC Evol Biol 10:351
Beydoun MA, Hossain S, Fanelli-Kuczmarski MT et al (2018) Vitamin D status and intakes and their association with cognitive trajectory in a longitudinal study of urban adults. J Clin Endocrinol Metab 103:1654–1668
Coskun S, Simsek S, Camkurt MA, Cim A, Celik SB (2016) Association of polymorphisms in the vitamin D receptor gene and serum 25-hydroxyvitamin D levels in children with autism spectrum disorder. Gene 588:109–114
Mokry LE, Ross S, Morris JA, Manousaki D, Forgetta V, Richards JB (2016) Genetically decreased vitamin D and risk of Alzheimer disease. Neurology. 87:2567–2574
Deng HW, Chen WM, Conway T et al (2000) Determination of bone mineral density of the hip and spine in human pedigrees by genetic and life-style factors. Genet Epidemiol 19:160–177
Hartz SM, Short SE, Saccone NL et al (2012) Increased genetic vulnerability to smoking at CHRNA5 in early-onset smokers. Arch Gen Psychiatry 69:854–860
Gage SH, Munafo MR (2015) Rethinking the association between smoking and schizophrenia. Lancet Psychiatry 2:118–119
Green AI, Drake RE, Brunette MF, Noordsy DL (2007) Schizophrenia and co-occurring substance use disorder. Am J Psychiatry 164:402–408
Enoch MA (2013) Genetic influences on the development of alcoholism. Curr Psychiatry Rep 15:412
Gelernter J, Kranzler HR, Sherva R et al (2014) Genome-wide association study of alcohol dependence:significant findings in African- and European-Americans including novel risk loci. Mol Psychiatry. 19:41–49
Zai CC, Manchia M, Zai GC et al (2018) Association study of BDNF and DRD3 genes with alcohol use disorder in Schizophrenia. Neurosci Lett 671:1–6
Mexal S, Berger R, Pearce L et al (2008) Regulation of a novel alphaN-catenin splice variant in schizophrenic smokers. Am J Med Genet Part B Neuropsychiatr Genet 147B:759–768
Abe K, Chisaka O, Van Roy F, Takeichi M (2004) Stability of dendritic spines and synaptic contacts is controlled by alpha N-catenin. Nat Neurosci 7:357–363
Grillon C, Ameli R, Charney DS, Krystal J, Braff D (1992) Startle gating deficits occur across prepulse intensities in schizophrenic patients. Biol Psychiatry 32:939–943
Mexal S, Frank M, Berger R et al (2005) Differential modulation of gene expression in the NMDA postsynaptic density of schizophrenic and control smokers. Brain Res Mol Brain Res 139:317–332
Livshits G, Deng HW, Nguyen TV, Yakovenko K, Recker RR, Eisman JA (2004) Genetics of bone mineral density: evidence for a major pleiotropic effect from an intercontinental study. J Bone Miner Res 19:914–923
Judex S, Garman R, Squire M, Donahue LR, Rubin C (2004) Genetically based influences on the site-specific regulation of trabecular and cortical bone morphology. J Bone Miner Res 19:600–606
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Scientific Foundation of China [81472925, 81673112]; the Key projects of international cooperation among governments in scientific and technological innovation [2016YFE0119100]; the Natural Science Basic Research Plan in Shaanxi Province of China [2017JZ024]; and the Fundamental Research Funds for the Central Universities. QT, HS and HWD were spartially supported by grants from the National Institutes of Health [R01AR057049, R01AR059781, D43TW009107, P20 GM109036, R01MH107354, R01MH104680, and R01GM109068], the Edward G. Schlieder Endowment fund and the Tsai and Kung endowment fund to Tulane University.
Author information
Authors and Affiliations
Contributions
LL and YJN drafted the manuscript, FZhang and YW designed the study, FZhu provided the key datasets regarding our manuscript. XCM, TLY, XDC, LJT, SQC, XQ, CJL, LZ, MM and PL performed the experimental analyses and statistical analyses. BLC, HWD, QT, HS provided feasible advice on data analysis and drafting manuscript. All authors read and approved the final manuscript. All authors discussed the results and commented on the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Xi’an Jiaotong University and University of Missouri-Kansas City. Signed informed-consent documents were obtained from all study participants before entering the study.
Consent for publication
Not applicable.
Competing interests
The authors report no financial interests or potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
FUMA gene set enrichment analysis results for the association between hip total area and SCZ.
Additional file 2: Table S2.
FUMA gene set enrichment analysis results for the association between hip neck area and SCZ.
Additional file 3: Table S3.
FUMA gene set enrichment analysis results for the association between hip neck BMD and SCZ.
Additional file 4: Table S4.
FUMA gene set enrichment analysis results for the association between hip total BMD and SCZ.
Additional file 5: Table S5.
FUMA gene set enrichment analysis results for the association between spine area and SCZ.
Additional file 6: Table S6.
FUMA gene set enrichment analysis results for the association between spineBMD and SCZ.
Additional file 7: Table S7.
FUMA gene set enrichment analysis results for the association between Ulna & Radius area and SCZ.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, L., Wen, Y., Ning, Y. et al. A trans-ethnic two-stage polygenetic scoring analysis detects genetic correlation between osteoporosis and schizophrenia. Clin Trans Med 9, 21 (2020). https://doi.org/10.1186/s40169-020-00272-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40169-020-00272-y