Abstract
The main objective of this study was to determine whether the common Y-haplogroups were be associated with the risk of developing severe COVID-19 in Spanish male. We studied 479 patients who required hospitalization due to COVID-19 and 285 population controls from the region of Asturias (northern Spain), They were genotyped for several polymorphisms that define the common European Y-haplogroups. We compared the frequencies between patients and controls aged ≤ 65 and >65 years. There were no different haplogroup frequencies between the two age groups of controls. Haplogroup R1b was less common in patients aged ≤65 years. Haplogroup I was more common in the two patient´s groups compared to controls (p = 0.02). Haplogroup R1b was significantly more frequent among hypertensive patients, without difference between the hypertensive and normotensive controls. This suggested that R1b could increase the risk for severe COVID-19 among male with pre-existing hypertension. In conclusion, we described the Y-haplogroup structure among Asturians. We found an increased risk of severe COVID-19 among haplogroup I carriers, and a significantly higher frequency of R1b among hypertensive patients. These results indicate that Y-chromosome variants could serve as markers to define the risk of developing a severe form of COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main objective of this study was to determine whether the common European chromosome Y-haplogroups were associated with the risk of developing a severe form of COVID-19.
The coronavirus disease-2019 (COVID-19) caused by the SARS-Cov-2 is characterised by a wide array of symptoms: while many individuals remain asymptomatic or showed a mild disease, others develop a severe pneumonia and complications in other organs that require hospitalization and increase the risk of death (Zeng et al. 2021). Risk factors such as advanced age, male sex, obesity, pre-existing cardiovascular and lung disease, have been associated with a higher risk of developing severe COVID-19 (Holt et al. 2022; Coto et al. 2021).The heterogeneous symptoms could be partially explained by the individual’s genetic background, and several genetic variants have been associated with the risk of developing severe COVID-19 and the risk of death (Ellinghaus et al. 2020; Cuesta-Llavona et al. 2021; Butler-Laporte et al. 2022). Male are at increased risk of developing severe COVID-19 compared to female and sex-specific genetic factors could thus contribute to the extent of disease symptoms (Peckham et al. 2020; Cruz et al. 2022).
Genes that regulate the immune response against viral infection are strong candidates to be associated with the risk of severe COVID-19 (Asano et al. 2021). Studies in rodents support that Y-chromosome genes play a role in the variability found between male and female immunity (Teuschert et al. 2006; Wesley et al. 2007). Animal studies also showed that Y-chromosome plays a significant role in the regulation of blood pressure and T-cell infiltration in tissues key to the cardiovascular function (Davidson et al. 1995; Khan et al. 2019). Y-chromosome variation in a murine model influence pathogenesis of the influenza A virus, increasing the susceptibility to the virus, immune response in lungs and T-lymphocyte activation, with higher IL-17 levels (Krementsov et al. 2017). In this regard, the presence of chromosome Y could explain in part the higher risk of severe COVID-19 among male. Y-chromosome could also contribute to COVID-19 through the risk of developing cardiovascular traits that increase the risk of suffering a severe form of the disease (Kloc et al. 2020).
Blood cells from male who developed a severe disease showed higher frequency of loss of Y (LOY) compared to healthy donors, and LOY has been associated with changes in immune gene transcription and increased risk for mortality in several diseases (Barros et al. 2020; Loftfield et al. 2019). LOY may also be associated to increased genome instability and impaired leucocyte immune responses (Thompson et al. 2019; Dumanski et al. 2021). At least one study reported loss of Y in leukocytes as a risk factor for critical COVID-19 in men (Bruhn-Olszewska et al. 2022).
Approximately 95% of the Y-sequence does not undergo recombination with the X-chromosome and is thus transmitted in full from father to son. These non-recombinant regions have accumulated nucleotide changes that originated in a particular population and passed down from a common male ancestor, spreading around the world through migrations. Groups of different Y-single nucleotide polymorphisms (SNPs) define the Y-haplogroups, with frequencies that are characteristic of each human population. For example, Y-R (defined by SNP M207 = rs2032658) originated about 30 thousand years ago and is the prevalent haplogroup among Europeans. More than half of the Spanish male carry haplogroup Y-R1b, defined by SNPs rs2032624 (R1) + rs9786153 (R1b), which had its origin in the upper paleolithic (approx. 25,000 years ago) in the Caucasus region (Myres et al. 2011). A sub-lineage of R1b known as DF27 (R1b1a2a1a2a) surged about 4200 years ago and is currently the prevalent among Spanish male (Solé-Morata et al. 2017; Villaescusa et al. 2017). Therefore, the analysis of this Y-variants allows to obtain information about population events throughout human history (Jobling and Tyler-Smith 2003; Parker et al. 2020; Underhill et al. 2000).
Y-haplogroups have been also associated with differences in inflammatory responses and cytokine production and several studies found significant association between some haplogroups and cardiovascular traits (Khan et al. 2019; Bloomer et al. 2014; Maan et al. 2017; Kuroki and Fukami 2023). Haplogroup I has been associated with coronary artery disease (CAD), and men with this haplogroup presented changes in expression of genes involved in atherosclerosis, response to viral infection, lipid metabolism, coagulation and haemostasis (Charchar et al. 2012; Bloomer et al. 2013; Voskarides et al. 2014; Eales et al. 2019; Maan et al. 2017; Lorca et al. 2023). Y-I was also associated with a lower immune response and a faster disease progression and mortality in HIV infected men (Sezgin et al. 2009).
Based on the role of Y-chromosome in the extent of immune responses and the risk of cardiovascular traits, we hypothesised that Y-haplogroups could explain in part the risk of developing severe COVID-19 among male. Thus, we evaluated the association between the common European Y-haplogroups and severe COVID-19 in a cohort of Spanish male.
Material and methods
Study subjects
The study was approved by the Ethics Committee of Principado de Asturias (Oviedo, Spain) and all the participants gave their consent to participate in the study. All the participants were > 18 years old and of Spanish ascent residents in the region of Asturias (northern Spain, total population 1 million).
We studied 479 male patients who required hospitalization due to COVID-19 between March 2020 and April 2021. They were followed till disease remission with hospital discharge or death. Data about pre-existing hypertension was obtained from the clinical history at hospital admission. Following previously reported criteria we considered early-onset COVID-19 as an age at hospitalization ≤65 years (Niemi et al. 2022).
The controls (N = 285; 38% ≤65 years) were recruited from the general population with the main purpose of defining the Y-variant frequencies in our region. Although the existence of SARS-CoV-2 infection was not determined in the controls, none of them required hospitalization due to COVID-19. The main values in the study cohort are summarised in Table 1.
Y-haplogroups determination
All the participants were genotyped for single nucleotide polymorphisms (SNPs) that defined the most common European Y-haplogroups (Table 2). The nucleotides were determined by real-time PCR with Taqman assays in an ABI7500 equipment and following the manufacturer instructions (Fisher Scientific). The allele frequencies among Europeans were obtained from the Ensembl database (www.ensembl.org).
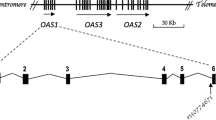
The genotyping of the DF27 sub-clade (SNP rs577478344 A/G) was performed by PCR with primers specific for the target region 5′TGTTAAAGTCCTGCGCTATTATGGTGT and 5′AAATATAGACGAATGCATAACTAGAATAACC, followed by Sanger sequencing in a capillary electrophoresis equipment (ABI3130xl, Thermo Fisher) (Suppl. Figure 1).
The presence of haplogroup I was confirmed by Sanger sequencing of PCR fragments containing the rs111665403 SNP, in complete linkage disequilibrium with rs2032597 (Suppl. Figure 2).
Statistical analysis
Statistical analysis was performed with R (version R-4.3.3 for Windows; https://www.r-project.org). All the values were collected in an excel file. Descriptive data are presented as total values and %. Patients and controls were classified as ≤65 and >65 years and the Y-haplogroup frequencies were compared between the groups with logistic regression. A p value below 0.05 was considered significant. Odds ratio´s (OR) and 95% confidence intervals (CI) were also calculated.
The presence of hypertension and the association of this variable with the Y-haplogroups was also determined in patients and controls.
Results
The prevalence of the different Y-chromosome haplogroups in the Asturias controls and COVID-19 patient’s are shown in Table 3. As expected, haplogroup R was the most frequent in our population with haplogroup R1b present in 66% and 63% of the controls >65 and ≤65 years, respectively (p = 0.25). There were no difference for the other haplogroups between the two control age-groups. The Y-R1b was significantly decreased in the younger vs. older patients (59% vs. 69%; p = 0.007; OR = 0.60, 95%CI = 0.41–0.87). We compared the patients with their age-matched controls. Y-R1b frequencies were no different between patients and controls ≤60 years (p = 0.78), and >60 (p = 0.52) (Table 3). We determined the frequency of the DF-27 subtype (SNP rs577478344) by sequencing all the R1b patients and controls. DF-27 was present in 83% and 84% of the R1b controls aged ≤60 and >60 years, and in 81% and 82% of the R1b patients aged ≤60 and >60 years. Thus, there were no difference for the DF-27 frequencies between the R1b groups but this marker was significantly less frequent in total patients ≤65 vs. >65 years (Table 3).
For the non-R1b haplogroups we found higher frequencies of Y-I in the two patients compared to control groups. Y-I was found in 9% of the patients and 4% of the controls (p = 0.02) with OR = 2.19 (95%CI = 1.13–4.22). Thus, in our population haplogroup Y-I could represent a risk marker for severe COVID-19 in male, although the reduced frequency of this haplogroup in our population is a study limitation. We compared the R1b and I between four age groups in the patients. While Y-I frequencies did not differ between the groups the R1b frequency showed an increased value with the age, ranging from 55% in the patients ≤55 years (N = 118) to 73% in patients aged >76 years (N = 92) (Fig. 1; Suppl. Table 1).
Hypertension is a well characterized risk factor for developing severe COVID-19. We sought to investigate whether the Y-haplogroups were associated with the presence of hypertension in our patients and controls. We found higher frequencies of R1b among the hypertensives in the two patients groups (≤65 years, p = 0.16; >65 years, p = 0.04), without difference between hypertensive and normotensive controls (Table 4).This suggested that individuals with pre-existing hypertension who are Y-R1b could have an increased risk of severe COVID-19 (Suppl. Table 2). In reference to Y-I, we found no different frequencies in the two patients groups regardless of the hypertension status.
There were a total of 56 deaths (12%) among the patients, 10 in the ≤65 years (4%) and 46 in the >65 years (20%). For the whole cohort there were no difference in haplogroup frequencies between deaths and survivors (Fig. 2).
Discussion
Chromosome-Y has been involved in the regulation of immune pathways, and this could explain in part the differences observed between male and female for several traits (Maan et al. 2017). Human chromosome-Y polymorphisms define the Y-haplogroups, which frequencies are population-specific. Several studies supported the association between some Y-haplogroups and common human diseases (Barros et al. 2020; Kuroki and Fukami 2023). Among others, haplogroup Y-I was associated with an increased risk for atherosclerosis (Charchar et al. 2012). This haplogroup was associated with significant different expression of several genes in macrophages, a cell type that plays an important role in the development of atherosclerosis (Bloomer et al. 2013). Moreover, compared to other haplogroups macrophages from Y-I men showed suppression of adaptive immunity and upregulation of pro-inflammatory response pathways (Charchar et al. 2012).
Due to the role of chromosome-Y in immunity the Y-haplogroups could be associated with differences in the extent of anti-viral responses. Rodent studies showed that the Y-chromosome modulates viral infection through RNAs that regulate the expression of several genes relevant to lymphocyte activation and recruitment (Krementsov et al. 2017). In this regard, Y-I male showed accelerated progression toward AIDS and reduced response to retroviral therapy (HAART) among HIV-infected male (Sezgin et al. 2009). Some studies showed that Y-chromosome takes part in chromatin modification mechanisms regulating the global gene expression in immune cells (Case et al. 2013). An study showed that male with Y-I had increased active chromatin sites associated with promoters and enhancers (Eales et al. 2019).
There are several mechanisms by which chromosome-Y variants could contribute to the severity of COVID-19. Male represent approximately 75% of the cases with critical COVID-19 in our population (Coto et al. 2021). The extent of the immune activity could be different between the Y-haplogroups and this would affect the response to SARS-CoV-2 among male. In the other hand, some chromosome Y variants could increase the risk for developing cardiovascular diseases that are associated with a higher risk of suffering severe COVID-19 (Bloomer et al. 2014). We found a significantly decreased frequency of R1b among the younger patients. The Y-haplogroup frequencies in our controls were similar to the reported by others, with R1b as the most common among Asturias male, and we did not find significant differences between controls aged ≤65 and >65 years. Thus, it was unlikely that the differences between the age groups of the patients could be explained by an age-effect in the general population. We found a higher frequency of R1b among patients with pre-existing hypertension. However, this haplogroup was not associated with hypertension among the controls (Table 4). This suggested that the common R1b haplogroup could be a risk factor for severe COVID-19 among hypertensives, instead of increasing the risk of hypertension in the general population. Hypertension was more frequent among the elderly patients and this could explain the higher frequency of R1b among these compared to the younger patients.
To our knowledge there are no studies supporting a significant functional effect of this haplogroup that could explain the association with COVID-19. However, some authors suggested that the rate of SARS-CoV-2 infection and mortality by COVID-19 was positively correlated with R1b, since populations with the highest R1b showed the highest rates of severe disease (Delanghe et al. 2020; Ibrahim and Salih 2021). Our study supports this hypothesis, but was based a single population and would require the genotyping of patients and controls from other European regions.
The main limitation of our study was the sample size that could reduce the power of the statistical analysis. This could be relevant for haplogroups with a low population frequency, that would require larger cohorts to confirm a genetic association. In particular, haplogroup I has a frequency of 5% in our population, much lower than that described in other populations where a positive association with cardiovascular traits was observed (Charchar et al. 2012). Our work requires validation in other populations as well as studies to determine the functional link between chromosome Y variants and COVID-19.
In conclusion, we report the chromosome Y haplogroup frequencies in controls and severe COVID-19 patients from the region of Asturias. Haplogroup Y-I could contribute to the risk of developing severe COVID-19, while haplogroup R1b was associated with an increased risk for severe disease among individuals with pre-existing hypertension. This work suggested that chromosome Y variants might serve as biological markers for the risk of developing severe COVID-19 in male.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. An Excel file with the raw data would be available for meta-analysis research.
References
Asano T, Boisson B, Onodi F, Matuozzo D, Moncada-Velez M, MagloriusRenkilaraj MRL et al (2021) X-linked recessive TLR7 deficiency in ~1% of men under 60 years old with life-threatening COVID-19. Sci Immunol 6:eabl4348. https://doi.org/10.1126/sciimmunol.abl4348
Barros B, Morais M, Teixeira AL, Medeiros R (2020) Loss of chromosome Y and its potential applications as biomarker in health and forensic sciences. Cytogenet Genome Res 160:225–237. https://doi.org/10.1159/000508564
Bloomer LD, Nelson CP, Eales J, Denniff M, Christofidou P, Debiec R et al (2013) Male-specific region of the Y chromosome and cardiovascular risk: phylogenetic analysis and gene expression studies. Arterioscler Thromb Vasc Biol 33:1722–1727. https://doi.org/10.1161/ATVBAHA.113.301608
Bloomer LD, Nelson CP, Denniff M, Christofidou P, Debiec R, Thompson J et al (2014) Coronary artery disease predisposing haplogroup I of the Y chromosome, aggression and sex steroids—genetic association analysis. Atherosclerosis 233:160–164. https://doi.org/10.1016/j.atherosclerosis.2013.12.012
Bruhn-Olszewska B, Davies H, Sarkisyan D, Juhas U, Rychlicka-Buniowska E, Wójcik M et al (2022) Loss of Y in leukocytes as a risk factor for critical COVID-19 in men. Genome Med 14(1):139. https://doi.org/10.1186/s13073-022-01144-5
Butler-Laporte G, Povysil G, Kosmicki JA, Cirulli ET, Drivas T, Furini S et al (2022) Exome-wide association study to identify rare variants influencing COVID-19 outcomes: results from the host genetics initiative. PLoS Genet 18:e1010367. https://doi.org/10.1371/journal.pgen.1010367
Case LK, Wall EH, Dragon JA, Saligrama N, Krementsov DN, Moussawi M, Zachary JF, Huber SA, Blankenhorn EP, Teuscher C (2013) The Y chromosome as a regulatory element shaping immune cell transcriptomes and susceptibility to autoimmune disease. Genome Res 23:1474–1485. https://doi.org/10.1101/gr.156703.113
Charchar FJ, Bloomer LD, Barnes TA, Cowley MJ, Nelson CP, Wang Y et al (2012) Inheritance of coronary artery disease in men: an analysis of the role of the Y chromosome. The Lancet 379(9819):915–922. https://doi.org/10.1016/S0140-6736(11)61453-0
Coto E, Avanzas P, Gómez J (2021) The renin–angiotensin–aldosterone system and coronavirus disease. Eur Cardiol 16:e07. https://doi.org/10.15420/ecr.2020.30
Cruz R, Diz-de Almeida S, López de Heredia M, Quintela I, Ceballos FC et al (2022) Novel genes and sex differences inCOVID-19 severity. Hum Mol Genet 31:3789–3806. https://doi.org/10.1093/hmg/ddac132
Cuesta-Llavona E, Gómez J, Albaiceta GM, Amado-Rodríguez L, García-Clemente M, Gutiérrez-Rodríguez J et al (2021) Variant-genetic and transcript-expression analysis showed a role for the chemokine-receptor CCR5 in COVID-19 severity. Int Immunopharmacol 98:107825. https://doi.org/10.1016/j.intimp.2021.107825
Davidson AO, Schork N, Jaques BC, Kelman AW, Sutcliffe RG, Reid JL, Dominiczak AF (1995) Blood pressure in genetically hypertensive rats. Influence of the Y chromosome. Hypertension 26:452–459. https://doi.org/10.1161/01.hyp.26.3.452
Delanghe JR, De Buyzere ML, De Bruyne S, Van Criekinge W, Speeckaert MM (2020) The potential influence of human Y-chromosome haplogroup on COVID-19 prevalence and mortality. Ann Oncol 31(11):1582–1584. https://doi.org/10.1016/j.annonc.2020.08.2096
Dumanski JP, Halvardson J, Davies H, Rychlicka-Buniowska E, Mattisson J, Moghadam BT et al (2021) Immune cells lacking Y chromosome show dysregulation of autosomal gene expression. Cell Mol Life Sci 78(8):4019–4033. https://doi.org/10.1007/s00018-021-03822-w
Eales JM, Maan AA, Xu X, Michoel T, Hallast P, Batini C et al (2019) Human Y chromosome exerts pleiotropic effects on susceptibility to atherosclerosis. Arterioscler Thromb Vasc Biol 39(11):2386–2401. https://doi.org/10.1161/ATVBAHA.119.312405
Ellinghaus D, Degenhardt F, Bujanda L, Buti M, Albillos A, Invernizzi P (2020) Genome wide association study of severe covid-19 with respiratory failure. N Engl J Med 383(16):1522–1534. https://doi.org/10.1056/NEJMoa2020283
Holt H, Talaei M, Greenig M, Zenner D, Symons J, Relton C et al (2022) Risk factors for developing COVID-19: a population-based longitudinal study (COVIDENCE UK). Thorax 77:900–912. https://doi.org/10.1136/thoraxjnl-2021-217487
Ibrahim M, Salih A (2021) The Y chromosome ancestry marker R1b1b2: a surrogate of the SARS-CoV-2 population affinity. Hum Genome Var 8:11. https://doi.org/10.1038/s41439-021-00141-1
Jobling MA, Tyler-Smith C (2003) The human Y chromosome: an evolutionary marker comes of age. Nat Rev Genet 4:598–612. https://doi.org/10.1038/nrg1124
Khan SI, Andrews KL, Jennings GL, Sampson AK, Chin-Dusting JPF (2019) Y chromosome, hypertension and cardiovascular disease: is inflammation the answer? Int J Mol Sci 20:2892. https://doi.org/10.3390/ijms20122892
Kloc M, Ghobrial RM, Kubiak JZ (2020) The role of genetic sex and mitochondria in response to COVID-19 infection. Int Arch Allergy Immunol 181:629–634. https://doi.org/10.1159/000508560
Krementsov DN, Case LK, Dienz O, Raza A, Fang Q, Ather JL et al (2017) Genetic variation in chromosome Y regulates susceptibility to influenza A virus infection. Proc Natl Acad Sci USA 114:3491–3496. https://doi.org/10.1073/pnas.1620889114
Kuroki Y, Fukami M (2023) Y chromosome genomic variations and biological significance in human diseases and health. Cytogenet Genome Res 163:5–13. https://doi.org/10.1159/000531933
Loftfield E, Zhou W, Yeager M, Chanock SJ, Freedman ND, Machiela MJ (2019) Mosaic Y loss is moderately associated with solid tumor risk. Cancer Res 79:461–466. https://doi.org/10.1158/0008-5472.CAN-18-2566
Lorca R, Aparicio A, Salgado M, Álvarez-Velasco R, Pascual I, Gomez J et al (2023) Chromosome Y haplogroup R was associated with the risk of premature myocardial infarction with ST-elevation: data from the CholeSTEMI Registry. J Clin Med 12:4812. https://doi.org/10.3390/jcm12144812
Maan AA, Eales J, Akbarov A, Rowland J, Xu X, Jobling MA, Charchar FJ, Tomaszewski M (2017) The Y chromosome: a blueprint for men’s health? Eur J Hum Genet 25:1181–1188. https://doi.org/10.1038/ejhg.2017.128
Myres NM, Rootsi S, Lin AA, Järve M, King RJ, Kutuev I et al (2011) A major Y-chromosome haplogroup R1b Holocene era founder effect in Central and Western Europe. Eur J Hum Genet 19:95–101. https://doi.org/10.1038/ejhg.2010.146
Niemi MEK, Daly MJ, Ganna A (2022) The human genetic epidemiology of COVID-19. Nat Rev Genet 23:533–546. https://doi.org/10.1038/s41576-022-00478-5
Parker K, Erzurumluoglu AM, Rodriguez S (2020) The Y chromosome: a complex locus for genetic analyses of complex human traits. Genes (basel) 11:1273. https://doi.org/10.3390/genes11111273
Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, Rosser EC, Webb K, Deakin CT (2020) Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 11:6317. https://doi.org/10.1038/s41467-020-19741-6
Sezgin E, Lind JM, Shrestha S, Hendrickson S, Goedert JJ, Donfield S et al (2009) Association of Y chromosome haplogroup I with HIV progression, and HAART outcome. Hum Genet 125:281–294. https://doi.org/10.1007/s00439-008-0620-7
Solé-Morata N, Villaescusa P, García-Fernández C, Font-Porterias N, Illescas MJ, Valverde L et al (2017) Analysis of the R1b-DF27 haplogroup shows that a large fraction of Iberian Y-chromosome lineages originated recently in situ. Sci Rep 7:7341. https://doi.org/10.1038/s41598-017-07710-x
Teuschert C, Noubade R, Spach K, McElvany B, Bunn JY, Fillmore PD, Zachary JF, Blankenhorn EP (2006) Evidence that the Y chromosome influences autoimmune disease in male and female mice. Proc Natl Acad Sci USA 103:8024–8029. https://doi.org/10.1073/pnas.0600536103
Thompson DJ, Genovese G, Halvardson J, Ulirsch JC, Wright DJ, Terao C et al (2019) Genetic predisposition to mosaic Y chromosome loss in blood. Nature 575:652–657. https://doi.org/10.1038/s41586-019-1765-3
Underhill PA, Shen P, Lin AA, Jin L, Passarino G, Yang WH et al (2000) Y chromosome sequence variation and the history of human populations. Nat Genet 26:358–361. https://doi.org/10.1038/81685
Villaescusa P, Illescas MJ, Valverde L, Baeta M, Nuñez C, Martínez-Jarreta B, Zarrabeitia MT, Calafell F, de Pancorbo MM (2017) Characterization of the Iberian Y chromosome haplogroup R-DF27 in northern Spain. Forensic Sci Int Genet 27:142–148. https://doi.org/10.1016/j.fsigen.2016.12.013
Voskarides K, Hadjipanagi D, Papazachariou L, Griffin M, Panayiotou AG (2014) Evidence for contribution of the Y chromosome in atherosclerotic plaque occurrence in men. Genet Test Mol Biomarkers 18:552–556. https://doi.org/10.1089/gtmb.2014.0020
Wesley JD, Tessmer MS, Paget C, Trottein F, Brossay L (2007) A Y chromosome-linked factor impairs NK T development. J Immunol 179:3480–3487. https://doi.org/10.4049/jimmunol.179.6.3480
Zeng H, Ma Y, Zhou Z, Liu W, Huang P, Jiang M, Liu Q, Chen P, Luo H, Chen Y (2021) Spectrum and clinical characteristics of symptomatic and asymptomatic coronavirus disease 2019 (COVID-19) with and without pneumonia. Front Med (lausanne) 8:645651. https://doi.org/10.3389/fmed.2021.645651
Acknowledgements
This work was supported by a grant from the Spanish Plan Nacional de I+D+I Ministerio de Economía y Competitividad and the European FEDER, grants ISCIII-PI21/00971 (E.C.), RICORS2040- RD21/0005/0011 (E.C.), FI-23/00207 (D.V.C.). And a grant from Gobierno del Principado de Asturias FICYT-AYUD/2021/520148 (G.M.A).
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
Lead researcher: EC; study design: EC, JG; patient assessment and data acquisition: MGF, DVC, GMA, LAR, MGC, JG; database: MGF, DVC, EC, GMA, LAR; genotyping: MGC, DVC, LVC, CFL, EC; data filtering and analysis: MGF, DVC, EC; statistical analysis: MGF, DVC, EC; analysis of results: EC; writing the manuscript: MGF, EC; revision of manuscript: all the authors.
Corresponding author
Ethics declarations
Conflict of interests
None of the authors have competing interests related to this work.
Ethics and consent
This study was approved by the clinical research ethics committee of Hospital Universitario Central Asturias (HUCA). All the participants gave their consent to participate in the study. Data were handled in observance of Spanish legislation on data protection. The study complies with the principles of the Declaration of Helsinki (“Recommendations guiding doctors in biomedical research involving human subjects”).
Additional information
Communicated by Boon Peng Hoh.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
González-Fernández, M., Vázquez-Coto, D., Albaiceta, G.M. et al. Chromosome-Y haplogroups in Asturias (Northern Spain) and their association with severe COVID-19. Mol Genet Genomics 299, 49 (2024). https://doi.org/10.1007/s00438-024-02143-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00438-024-02143-4