Abstract
Background
Molecular analysis of carbapenem-resistant genes in Acinetobacter baumannii, an emerging pathogen, is less commonly reported from Nepal. In this study we determined the antibiotic susceptibility profile and genetic mechanism of carbapenem resistance in clinical isolates of A. baumannii.
Methods
A. baumannii were isolated from various clinical specimens and identified based on Gram staining, biochemical tests, and PCR amplification of organism specific 16S rRNA and bla OXA-51 genes. The antibiotic susceptibility testing was performed using disc diffusion and E-test method. Multiplex PCR assays were used to detect the following β-lactamase genes: four class D carbapenem hydrolyzing oxacillinases (bla OXA-51, bla OXA-23, bla OXA-24 and bla OXA-58). Uniplex PCRs were used to detect three class B metallo-β-lactamases genes (bla IMP, bla VIM and bla NDM-1), class C cephalosporin resistance genes (bla ADC), aminoglycoside resistance gene (aphA6), and ISAba1 of all isolates. Insertion sequence ISAba125 among NDM-1 positive strains was detected. Clonal relatedness of all isolates were analyzed using repetitive sequence-based PCR (rep-PCR).
Results
Of total 44 analyzed isolates, 97.7% (n = 43) were carbapenem-resistant A. baumannii (CR-AB) and 97.7% (n = 43) were multidrug resistant A. baumannii (MDR-AB). One isolate was detected to be extremely drug resistant A. baumannii (XDR-AB). All the isolates were fully susceptible to colistin (MICs < 2 μg/ml). The bla OXA-23 gene was detected in all isolates, while bla NDM-1 was detected in 6 isolates (13.6%). Insertion sequence, ISAba1 was detected in all of bla OXA-23 positive isolates. ISAba125 was detected in all bla NDM-1 positive strains. The bla ADC and aphA6 genes were detected in 90.1 and 40.1%, respectively. The rep-PCR of all isolates represented 7 different genotypes.
Conclusion
We found high prevalence of CR-AB and MDR-AB with bla OXA-23 gene in a tertiary care hospital in Nepal. Systemic network surveillance should be established for monitoring and controlling the spread of these resistant strains.
Similar content being viewed by others
Background
Acinetobacter baumannii, an emerging pathogen of healthcare centers, shows intrinsic as well as acquired drug-resistance mechanisms [1]. Multidrug-resistant A. baumannii can be resistant to all of the currently available antibiotics, and in its deadliest form these are only susceptible to potentially toxic polymyxins and colistins, leaving limited options for treatment [2]. Infections with carbapenem- and colistin-resistant A. baumannii are emerging globally [3].
Carbapenem resistance in A. baumannii encompasses production of class B, C and class D carbapenemase, decreased membrane permeability, altered penicillin-binding proteins, and overexpression of efflux pumps [4, 5]. Most commonly, Acinetobacter spp. develop carbapenem resistance by production of OXA-type carbapenemase and metallo-β-lactamases (MBLs) [6, 7]; bla OXA-23-like, bla OXA-40-like, bla OXA-58-like and bla OXA-51-like carbapenemases are broadly reported, where bla OXA-51-like β-lactamases, intrinsic to A. baumannii, is used for species identification [8–10]. Among multiple MBL genes, bla IMP and bla VIM types (chromosomal or plasmid encoded) encode carbapenemase in A. baumannii [9]. A. baumannii harboring plasmid encoded New Delhi metallo-β-lactamase-1 (NDM-1), a novel carbapenemase gene, is reported from many countries [11, 12]. In addition, detection of class C β-lactamase genes (bla ADC) which mediated cephalosporin resistances and aminoglycoside resistant genes (aphA6) has increased in recent years in A. baumannii clinical isolates [13, 14].
A. baumannii remains a critical problem in many healthcare settings throughout the world despite the implementation of infection control practices. There are limited data on carbapenem-resistant A. baumannii in Nepal. The objective of this study was to determine antibiotic susceptibility profile, antibiotic resistance genes and genetic mechanism of carbapenem resistance of A. baumannii in clinical isolates at a tertiary care hospital, Nepal.
Methods
Bacterial isolation and identification
A. baumannii isolates were collected from inpatient units of a tertiary hospital, Nepal. Forty-four non-duplicate isolates were collected (24 male and 20 female; age range between 24 to 80 years) over 9 months periods (October 2014 to June 2015). All isolates were identified by classical biochemical methods and confirmed by PCR method for detecting 16S rRNA gene and bla OXA-51 gene [15, 16]. Isolates were identified as A. baumannii by PCR result of positive for both PCRs.
Antibiotic susceptibility testing
The antibiotic susceptibility of amikacin (30), cefotaxime (30), ceftazidime (30), ceftriaxone (30), cefepime (30), ciprofloxacin (5), gentamicin (10), imipenem (10), meropenem (10), trimethoprim/sulfamethoxazole (1.25/23.75), tetracycline (30), and piperacillin/tazobactam (100/10) (Oxoid) was determined on Mueller Hinton Agar (High Media, India) according to the antibiotic disk diffusion method [17]. The plates were incubated at 37 °C for 24 h. The zones of inhibition were determined whether the microorganism was susceptible, intermediately resistant, or resistant to each antibiotic according to Clinical and Laboratory Standards Institute (CLSI) guidelines. E-test was performed to determine the Minimum inhibitory concentration (MIC) of ceftazidime, imipenem, tigecycline and colistin (High Media, India) according to manufacturer instructions and interpreted as per CLSI guidelines except for tigecycline. Multidrung-resistant A. baumannii (MDR-AB) was defined when A. baumannii resistant to multiple antibiotics, often defined as three or more antibiotic classes. Extensively drug resistant A. baumannii (XDR-AB) was defined when A. baumannii was resistant to all antimicrobial agents except polymyxins (colistin) [18].
PCR amplification of antibiotic resistance genes
PCR assays to detect bla OXA-23, bla OXA-24, bla OXA-51, bla OXA-58, bla IMP, bla VIM, bla NDM, bla ADC and ahpA6 genes were performed using primers as describe previously (Table 1). The amplification reaction was performed using A. baumannii cell lysate as DNA template. Each PCR was performed in triplicate in a thermocycler with a PCR condition as described previously [14, 16, 19–21]. All PCR assays used 16S rRNA or bla OXA-51 genes as the internal control. The ISAba1 of bla OXA-23 gene was detected using combination of primers ISAba1-F/ISAba1-R and ISAba1-F/bla OXA-23-R (Table 1) [22]. The ISAba125 of bla NDM-1 gene were determined in all bla NDM-1 positive strains using combination of primers ISA125-F/ISA125-R and ISA125-F/bla NDM-R (Table 1). PCR products of the bla NDM-1 genes were purified and sequenced. BLAST was used to compare the sequences of bla NDM-1 genes against the GenBank Database. PCR products were analyzed by electrophoresis in 1% agarose gel containing 0.5 μg/ml ethidium bromides.
IPM-EDTA combined disk test
All bla NDM-1 positive strains were tested for MBL production by IPM-EDTA combined disk test. The test was performed as previously described [23]. After 24 h incubation, the difference of inhibition zone diameter between IPM-EDTA disk and IPM disk alone (≥7 mm) was considered the positive criteria for the presence of MBL.
Repetitive element PCR-mediated DNA fingerprinting (rep-PCR)
Genomic DNA of each isolates was extracted from the overnight cultures using GF-1 bacterial DNA extraction kit (Vivantis, Malaysia). Rep-PCR was performed by using genomic DNA as a template for PCR amplification with the ERIC-2 primer (Table 1) using condition as describe previously [24, 25]. PCR-banding patterns and rep-PCR types were analyzed and interpreted as previously described [25].
Results
Demographic characteristic of patients
Demographic characteristics of the inpatients with A. baumannii infection were analyzed; 24 (54.5%) were male and 20 (45.5%) were female. Most of the specimens were from ICU wards (n = 27, 61.4%) (Fig. 1). Isolates were collected from sputum (n = 26, 59.1%), tracheal aspirates (n = 9, 20.4%), catheter tip, (n = 4, 9.1%), pus (n = 4, 9.1%) and urine (n = 1, 2.3%) (Fig. 1).
Antibiotic susceptibility
Of the 44 isolates, resistance was found against ciprofloxacin (n = 43, 97.7%), cefotaxime (n = 43, 97.7%), ceftazidime (n = 42, 95.4%), ceftriaxone (n = 41, 93.2%), cefepime (n = 39, 88.6%), amikacin (n = 19, 43.2%), gentamicin (n = 23, 52.3%), trimethoprim/sulfamethoxazole (n = 41, 93.2%), tetracycline (n = 21, 47.7%) and piperacillin/tazobactam (n = 43, 97.7%). Only one isolate of A.baumannii was susceptible to all tested antibiotics. Most isolates (97.7%, n = 43) were carbapenem resistant A. baumannii (CR-AB); all CR-AB were MDR-AB. One isolate was detected to be XDR-AB. All the isolates were fully susceptible to colistin (MICs < 2 μg/ml) and MIC of tigecycline was determined to be <2.5 μg/ml (Table 2).
Antibiotic resistance genes and IS element in A. baumannii
Aminoglycoside resistance gene, aphA6 and cephalosporin resistance genes, bla ADC were detected in 40.1% (18/44) and 90.1% (40/44), respectively. The bla OXA-23 was present in all isolates. Other class D β-lactamase genes, including bla OXA-24 and bla OXA-58, markers of carbapenem resistance in A. baumannii, were not detected in analyzed isolates. ISAba1 was detected in all of bla OXA-23 positive isolates (100%). Of total analyzed isolates, 6 (13.6%) also harbored bla NDM-1 gene in addition to bla OXA-23 and bla OXA-51. All NDM-1 positive strains exhibited insertion sequence ISAba125 detecting with primers ISA125-F/ISA125-R. All isolates also detected a band of 1.6 kb in a PCR using ISA125-F/bla NDM-R primers. Metallo-β-lactamase (MBL) genes, including bla VIM and bla IMP, were not detected in all isolates. The sequences of the bla NDM-1 gene yielded 99-100% sequence identity to the bla NDM-1 gene from Acinetobacter lwoffii strain WJ10621 plasmid pNDM-BJ01 (Accession: JQ001791) obtained from the GenBank Database.
MBL production
Six A. baumannii isolates harbored bla NDM-1 gene were detected for MBL production. All of bla NDM-1 positive strains were positive for MBL production. MBL positive strains showed resistance to fluoroquinolones and β-lactam.
Epidemiological typing
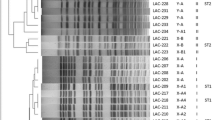
Clonal relationship among isolates were studied using rep-PCR typing. The fingerprinting represented 7 different DNA patterns consisting of 2 to 5 DNA fragment sizes. The amplicons size for ERIC-2 PCR was 500–4000 bp. The genotype was named A-G as shown in Fig. 2. The high prevalence genotype was type C (n = 14; 31.8%) and D (n = 12; 27.3%). Genotype A, B, C and D were disseminated in all isolated ward (ICU, general ward and post-operative ward). Among 44 isolates, one isolate of type F (2.3%) and G (2.3%) was found. Type F was obtained from a catheter tip specimen from the ICU ward. Type G was obtained from sputum of a patient from a general ward. All NDM-1 positive strains exhibited genotype A (n = 1), B (n = 1), C (n = 3) and D (n = 1).
Discussions
A. baumannii harboring bla OXA-51-like gene has been identified as a marker for species identification. An intrinsic bla OXA-51-like gene detected in all isolates in this study supports the use of this gene as a surrogate marker of A. baumannii identification [8–10]. High prevalence of cephalosporin resistance genes, bla ADC (90.1%) was found in this study. In addition, we found a high rate of cepharosporin resistant antibiotics (cefotaxime, ceftazidime, ceftriaxone) using the disk diffusion method. These data indicated that cephalosporins no longer work to treat A. baumannii isolated from Nepal. Carbapenem resistance in A. baumannii is a major concern and is most often associated with class D β-lactamases and MBLs. The full susceptibility of all CR-AB to colistin in this study indicates that colistin is still an option of drug for the treatment of infections caused by A. baumannii in Nepal hospital.
OXA-type carbapenemases are predominant in A. baumannii [6, 7]. In agreement with this finding, high prevalence of bla OXA-23 carrying A. baumannii strains has been reported in Nepalese patients [26]. The acquired bla OXA-23 is the dominant genetic determinant in Asia. The bla OXA-23 gene located on plasmid can be transferred between A. baumannii through conjugation. Thus, antibiotic resistant bacteria have been rapidly increasing worldwide [27]. The bla OXA-24 and bla OXA-58 were not detected in any isolates from this study. The bla OXA-24/40 and bla OXA-58 genes were common in A. baumannii isolated from Europe [2, 28]. Recently, bla OXA-143 and bla OXA-235, which are novel class D β-lactamase genes in A. baumannii have been identified. To date, these determinants were detected only in Brazil, Mexico and the USA [29, 30]. ISAba1 was detected in widespread clones of A. baumannii worldwide. Our study found ISAba1 upstream of bla OXA-23 in all A. baumannii isolates. A correlation between A. baumannii clusters carrying the ISAba1/bla OXA-23 gene and increased minimal inhibitory concentrations for carbapenems was reported [31]. One isolate (AB-13) that was recovered from catheter tips of long-stay hospital patients showed an extreme drug resistance pattern (Additional file 1: Table S1). This isolate represented bla OXA-23, bla ADC and aphA6 genes. Further molecular study to detect other antibiotic resistance genes is needed to explain what factors correlated with extreme drug resistance. We also found one isolate (AB-25) harboring bla OXA-23, bla ADC and aphA6 genes was sensitive to all tested drugs (Additional file 1: Table S1). This may be due to the lack of promoter or mutation of ISAba1 or bla OXA-23 gene. Further study is needed to warrant the conclusion.
The bla NDM-1 carrying A. baumannii has recently been emerged in many countries, including Germany, Spain, Israel, Egypt, Switzerland, Libya, India, Pakistan and Nepal [11, 26, 32, 33]. The bla NDM-1 gene has been identified as a chimeric gene constructed by the fusion of the aminoglycoside-resistance gene aphA6 with a mannose-binding lectin gene. This event most likely occurs in Acinetobacter spp., indicating that these bacteria are likely the origin of this gene [34]. In this study, we identified 13.6% of A. baumannii carrying bla NDM-1 gene. Previous study has identified high prevalence (24.6%) of the A. baumannii harbored the bla NDM-1 gene in Nepal in 2013–2014 [26]. Taking into consideration the relationship between India, China and Nepal, the spread of bla NDM-1 is likely to occur rapidly, mostly through A. baumannii rather than Enterobacteriaceae. A. baumannii able to transfer the bla NDM-1 gene via conjugation to the recipients and Tn125 appears to be the main vehicle for dissemination of the bla NDM-1 genes in A. baumannii [35]. Poirel et al. reported that the bla NDM-1 gene was located within the composite transposon Tn125 bracketed by two copies of a strong promoter of bla NDM-1 gene called ISAba125 [11]. This report was correlated with our finding that found ISAba125 in 100% of NDM-1 producing A. baumannii.
The previous study reported that the most of A. baumannii isolates harboring bla NDM-1 belonged to ST85 and ST25 [35–37]. In Libyan hospital, Libya, the main clone of imipenem-resistant NDM-1-producing A. baumannii belonged to ST2 [33]. We used rep-PCR typing to determine the clonal relationship in NDM-1 producing A. baumannii. Our study highlighted that most of NDM-1-producing A. baumannii isolates belonged to 4 genotypes using rep-PCR. Rep-PCR is a method that generates DNA fingerprints to discriminate between bacterial strains, and has been used to characterize A. baumannii isolates from hospitalized patients [38]. Our rep-PCR typing represented a high genetic diversity (A-G) among A. baumannii isolates from Nepal. Some clonally related groups (A, B, C and D) were observed in the all wards represented the disseminated of these clones in the hospital. Four genotypes (A, B, C, and D) of co-existence of bla OXA-23 and bla NDM-1 A. baumannii isolates were found. In addition, dissemination of these four genotypes into different wards also confirms as a major epidemic. Since rep-PCR is less discriminatory for molecular typing of bacterial strains, further study using multi-locus sequence typing could be useful for epidemiological investigations.
Conclusion
Antibiotic resistance in A. baumannii is considered to be a major future challenge in Nepal. Beyond OXA-type carbapenemase, there is no doubt the emergence and spreads of NDM-1 encoding A. baumannii–a superbug–will further limit chemotherapeutic options and threaten the public health of Nepal. The mechanism of hospital adaptiveness beyond antibiotic resistance will be more demanded in order to fully understand and combat MDR and XDR A. baumannii.
Abbreviations
- CR-AB:
-
Carbapenem-resistant Acinetobacter baumannii
- ICU:
-
Intensive care unit
- IPM-EDTA:
-
Imipenem-ethylenediaminetetraacetic acid
- MBL:
-
Metallo-beta-lactamase
- MDR-AB:
-
Multidrug-resistant Acinetobacter baumannii
- MIC:
-
Minimum inhibitory concentration
- NDM:
-
New Delhi metallo-beta-lactamase
- PCR:
-
Polymerase chain reaction
- XDR-AB:
-
Extremely drug resistant Acinetobacter baumannii
References
Yamamoto M, Nagao M, Matsumura Y, Matsushima A, Ito Y, Takakura S, et al. Interspecies dissemination of a novel class 1 integron carrying bla IMP-19 among Acinetobacter species in Japan. J Antimicrob Chemother. 2011;66:2480–3.
Villalon P, Valdezate S, Medina-Pascual MJ, Carrasco G, Vindel A, Saez-Nieto JA. Epidemiology of the Acinetobacter-derived cephalosporinase, carbapenem-hydrolysingoxacillinase and metallo-beta-lactamase genes, and of common insertion sequences, in epidemic clones of Acinetobacter baumannii from Spain. J Antimicrob Chemother. 2013;68:550–3.
Agodi A, Voulgari E, Barchitta M, Quattrocchi A, Bellocchi P, Poulou A, et al. Spread of a carbapenem- and colistin-resistant Acinetobacter baumannii ST2 clonal strain causing outbreaks in two Sicilian hospitals. J Hosp Infect. 2014;86:260–6.
Heritier C, Poirel L, Lambert T, Nordmann P. Contribution of acquired carbapenem-hydrolyzing oxacillinases to carbapenem resistance in Acinetobacter baumannii. Antimicrob Agents Chemother. 2005;49:3198–202.
Quale J, Bratu S, Landman D, Heddurshetti R. Molecular epidemiology and mechanisms of carbapenem resistance in Acinetobacter baumannii endemic in New York City. Clin Infect Dis Off Publ Infect Dis Soc Am. 2003;37:214–20.
Amudhan MS, Sekar U, Kamalanathan A, Balaraman S. bla IMP and bla VIM mediated carbapenem resistance in Pseudomonas and Acinetobacter species in India. J Infect Develop Ctries. 2012;6:757–62.
Thomson JM, Bonomo RA. The threat of antibiotic resistance in Gram negative pathogenic bacteria: beta-lactams in peril! Curr Opin Microbiol. 2005;8:518–24.
Cicek AC, Saral A, Iraz M, Ceylan A, Duzgun AO, Peleg AY, et al. OXA- and GES-type beta-lactamases predominate in extensively drug-resistant Acinetobacter baumannii isolates from a Turkish University Hospital. Clin Microbiol Infect. 2014;20:410–5.
Tsakris A, Ikonomidis A, Pournaras S, Tzouvelekis LS, Sofianou D, Legakis NJ, et al. VIM-1 metallo-beta-lactamase in Acinetobacter baumannii. Emerg Infect Dis. 2006;12:981–3.
Kusradze I, Diene SM, Goderdzishvili M, Rolain JM. Molecular detection of OXA carbapenemase genes in multidrug-resistant Acinetobacter baumannii isolates from Iraq and Georgia. Int J Antimicrob Agents. 2011;38:164–8.
Poirel L, Bonnin RA, Boulanger A, Schrenzel J, Kaase M, Nordmann P. Tn125-related acquisition of blaNDM-like genes in Acinetobacter baumannii. Antimicrob Agents Chemother. 2012;56:1087–9.
Abbas M, Cherkaoui A, Fankhauser C, Schrenzel J, Harbarth S. Epidemiology and clinical implications of carbapenemase-producing bacteria in Switzerland. Rev Med Suisse. 2012;8:882–4.
Sarhaddi N, Soleimanpour S, Farsiani H, Mosavat A, Dolatabadi S, Salimizand H, et al. Elevated prevalence of multidrug-resistant Acinetobacter baumannii with extensive genetic diversity in the largest burn centre of northeast Iran. J Glob Antimicrob Resist. 2016;8:60–6.
Hujer KM, Hujer AM, Hulten EA, Bajaksouzian S, Adams JM, Donskey CJ, et al. Analysis of antibiotic resistance genes in multidrug-resistant Acinetobacter sp. isolates from military and civilian patients treated at the Walter Reed Army Medical Center. Antimicrob Agents Chemother. 2006;50:4114–23.
Misbah S, Hassan H, Yusof MY, Hanifah YS, Abu-Bakar S. Genomic species identification of Acinetobacter of clinical isolates by 16S rDNA sequencing. Singapore. Med J. 2005;46:461–4.
Woodford N, Ellington MJ, Coelho JM, Turton JF, Ward ME, Brown S, et al. Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int J Antimicrob Agents. 2006;27:351–3.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing, document M100-24. Wayne: Clinical and Laboratory Standards Institute; 2014.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268–81.
Liu Y, Liu X. Detection of AmpC β-lactamases in Acinetobacter baumannii in the Xuzhou region and analysis of drug resistance. Exp Ther Med. 2015;10:933–6.
Ellington MJ, Kistler J, Livermore DM, Woodford N. Multiplex PCR for rapid detection of genes encoding acquired metallo-beta-lactamases. J Antimicrob Chemother. 2007;59:321–2.
Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011;70:119–23.
Ruiz M, Marti S, Fernandez-Cuenca F, Pascual A, Vila J. Prevalence of IS (Aba1) in epidemiologically unrelated Acinetobacter baumannii clinical isolates. FEMS Microbiol Lett. 2007;274:63–6.
Yong D, Lee K, Yum JH, Shin HB, Rossolini GM, Chong Y. Imipenem-EDTA disk method for differentiation of metallo-beta-lactamase-producing clinical isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2002;40:3798–801.
Vila J, Marcos MA, Jiminez de Anta MT. A comparative study of different PCR-based DNA fingerprinting techniques for typing of the Acinetobacter calcoaceticus-A. baumannii complex. J Med Microbiol. 1996;44:482–9.
Grundmann HJ, Towner KJ, Dijkshoorn L, Gerner-Smidt P, Maher M, Seifert H, et al. Multicenter study using standardized protocols and reagents for evaluation of reproducibility of PCR-based fingerprinting of Acinetobacter spp. J Clin Microbiol. 1997;35:3071–7.
Shrestha S, Tadab T, Miyoshi-Akiyamac T, Oharad H, Shimadab K, Satoue K, et al. Molecular epidemiology of multidrug-resistant Acinetobacter baumannii isolates in a university hospital in Nepal reveals the emergence of a novel epidemic clonal lineage. Int J Antimicrob Agents. 2015;46:526–31.
Bertini A, Poirel L, Mugnier PD, Villa L, Nordmann P, Carattoli A. Characterization and PCR-based replicon typing of resistance plasmids in Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54:4168–77.
Cherkaoui A, Emonet S, Renzi G, Schrenzel J. Characteristics of multidrug-resistant Acinetobacter baumannii strains isolated in Geneva during colonization or infection. Ann Clin Microbiol Antimicrob. 2015;11:14–42.
Higgins PG, Pérez-Llarena FJ, Zander E, Fernández A, Bou G, Seifert H. OXA-235, a novel class D β-lactamase involved in resistance to carbapenems in Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57:2121–6.
Zander E, Bonnin RA, Seifert H, Higgins PG. Characterization of bla OXA-143 variants in Acinetobacter baumannii and Acinetobacter pittii. Antimicrob Agents Chemother. 2014;58:2704–8.
Viana GF, Zago MC, Moreira RR, Zarpellon MN, Menegucci TC, Cardoso CL, et al. ISAba1/bla OXA-23: A serious obstacle to controlling the spread and treatment of Acinetobacter baumannii strains. Am J Infect Control. 2016;44:593–5.
Decousser JW, Jansen C, Nordmann P, Emirian A, Bonnin RA, Anais L, et al. Outbreak of NDM-1-producing Acinetobacter baumannii in France, January to May 2013. Eurosurveillance. 2013;18. doi:10.2807/1560-7917.ES2013.18.31.20547
Mathlouthi N, El Salabi AA, Ben Jomàa-Jemili M, Bakour S, Al-Bayssari C, Zorgani AA, et al. Early detection of metallo-β-lactamase NDM-1- and OXA-23 carbapenemase-producing Acinetobacter baumannii in Libyan hospitals. Int J Antimicrob Agents. 2016;48:46–50.
Toleman MA, Spencer J, Jones L, Walsh TR. bla NDM-1 is a chimera likely constructed in Acinetobacter baumannii. Antimicrob Agents Chemother. 2012;56:2773–76.
Ramoul A, Loucif L, Bakour S, Amiri S, Dekhil M, Rolain JM. Co-occurrence of bla NDM-1 with bla OXA-23 or bla OXA-58 in clinical multidrug-resistant Acinetobacter baumannii isolates in Algeria. J Glob Antimicrob Resist. 2016;6:136–41.
Rafei R, Pailhoriès H, Hamze M, Eveillard M, Mallat H, Dabboussi F, et al. Molecular epidemiology of Acinetobacter baumannii in different hospitals in Tripoli, Lebanon using bla OXA-51-like sequence based typing. BMC Microbiol. 2015;15:11–7.
Bakour S, Touati A, Bachiri T, Sahli F, Tiouit D, Naim M, et al. First report of 16S rRNA methylase ArmA-producing Acinetobacter baumannii and rapid spread of metallo-β-lactamase NDM-1 in Algerian hospitals. 2014. J Infect Chemother. 2014;20:696–701.
Pasanen T, Koskela S, Mero S, Tarkka E, Tissari P, Vaara M, et al. Rapid molecular characterization of Acinetobacter baumannii clones with rep-PCR and evaluation of carbapenemase genes by new multiplex PCR in hospital district of Helsinki and Uusimaa. Plos One. 2014;9:e85854.
Acknowledgements
We thank Dr. Basant Pant, Neurosurgeon, Annapurna Neurological Institute and Allied Sciences for providing laboratory facility and moral support. We also acknowledge Nepal Health Research Council for approving this study.
Funding
This study was partial funding by Thailand Research Fund (RSA5780015).
Availability of data and materials
Please contact author for data requests.
Authors’ contributions
PRJ and MA designed the study, collected data, analyzed the data and prepared the manuscript, TK supervised the study, UL and RT collected data, SS, analyzed the data, supervised the study and prepared the manuscript. All authors read and approved the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical approval was obtained from the Ethical Review Board of Nepal Health Research Council (NHRC) (Reg. 27/2015). Informed consent was taken from all the patients or patients’ guardians. The research was in compliance with the Helsinki Declaration.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Type of clinical specimen, ward, antibiotic susceptibility patterns, rep-PCR types, resistance genes and MIC of 44 A. baumannii isolates. (DOCX 23 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Joshi, P.R., Acharya, M., Kakshapati, T. et al. Co-existence of bla OXA-23 and bla NDM-1 genes of Acinetobacter baumannii isolated from Nepal: antimicrobial resistance and clinical significance. Antimicrob Resist Infect Control 6, 21 (2017). https://doi.org/10.1186/s13756-017-0180-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-017-0180-5