Abstract
Background
A. baumannii has emerged as an important nosocomial pathogen with an outstanding ability to acquire multidrug resistant mechanisms. In this study, we investigate the molecular epidemiology and carbapenem resistance mechanisms of A. baumannii in Tripoli, Northern Lebanon.
Methods
One hundred sixteen non-duplicate isolates isolated between 2011 and 2013 in different hospitals in Tripoli, Lebanon from Lebanese patients and wounded Syrian patients during Syrian war were studied. Antibiotic susceptibility testing was determined by agar disc diffusion and Etest. Carbapenemase-encoding genes were investigated by PCR. All isolates were typed by bla OXA-51-like sequence based typing (SBT) and 57 isolates were also analysed by MLST using Pasteur’s scheme followed by eBURST analysis.
Results
Of the 116 isolates, 70 (60 %) showed a carbapenem resistance phenotype. The bla OXA-23 with an upstream insertion of ISAba1 was the major carbapenem resistance mechanism and detected in 65 isolates. Five isolates, including four from wounded Syrian patients and one from a Lebanese patient, were positive for bla NDM-1. bla OXA-51-like SBT revealed the presence of 14 variants, where bla OXA-66 was the most common and present in 73 isolates, followed by bla OXA-69 in 20 isolates. MLST analysis identified 17 sequence types (ST) and showed a concordance with bla OXA-51-like SBT. Each clonal complex (CC) had a specific bla OXA-51-like sequence such as CC2, which harboured bla OXA-66 variant, and CC1 harbouring bla OXA-69 variant. NDM-1 producing isolates belonged to ST85 (4 Syrian isolates) and ST25 (1 Lebanese isolate).
Conclusions
Our results showed a successful predominance of international clone 2 with a widespread occurrence of OXA-23 carbapenemase in Lebanese hospitals. These findings emphasise the urgent need of effective measures to control the spread of A. baumannii in this country.
Similar content being viewed by others
Background
A. baumannii is an opportunistic pathogen mainly involved in healthcare-associated infections, with increased mortality and morbidity [1]. The serious concern associated with this bacterium is the increasing prevalence of multidrug resistant isolates, especially carbapenem resistant ones [2]. Therefore, management of infections due to A. baumannii has become a real public health issue in many countries [3]. In a recent SENTRY Antimicrobial Surveillance program, the percentage of A. baumannii isolates susceptible to meropenem decreased noticeably from 52.9 % in 2009 to 37.7 % in 2011 in European intensive care units [4]. The main mechanism of resistance to carbapenems is the production of oxacillinases encoded mostly by blaOXA-23-like, blaOXA-24-like, blaOXA-58-like and recently blaOXA-143-like and blaOXA-235-like [2, 5–7]. To a lesser degree, carbapenemases from classes A and B have also been involved [2, 5]. New Delhi metallo-ß-lactamase 1 (NDM-1), a recent described metallo-ß-lactamase, has emerged in Enterobacteriaceae as well as in Acinetobacter [8]. Generally, a limited number of clones are responsible for worldwide outbreaks, and international clones I and II are the most common ones [9]. In order to identify and track these clones during hospital outbreaks, numerous molecular typing methods have been proposed such as pulsed-field gel electrophoresis (PFGE), amplified fragment length polymorphism (AFLP), repetitive-sequence-based PCR (rep-PCR), and multilocus sequence typing (MLST) [10–14] . Currently, MLST is the gold standard typing tool for population structure and macro-epidemiological investigations based on sequencing of internal fragments of 7 genes [14]. Two MLST schemes have been developed for Acinetobacter baumannii : Pasteur and Bartual schemes [10, 15]. Overall, the 2 schemes are concordant [14]. However, because of recombination bias observed on some loci in Bartual’s MLST (gyrB and gpi) [16, 17], Pasteur’s MLST has been chosen for this study. Recently, blaOXA-51-like sequence-based typing (SBT), a simple typing method based on sequencing of the full length of blaOXA-51-like gene has been proposed as it has shown a similar discriminatory power than rep-PCR, and MLST [16, 18–20].
In Lebanon, limited numbers of epidemiological studies concerning A. baumannii have been reported, almost in Beyrouth [20–23]. In a previous study, we have described the dominance of international clone II within a set of 42 isolates collected from Beyrouth and North Lebanon between 2009–2012 [20]. In another study, we reported the first detection of four NDM-1 producing isolates isolated in Tripoli-Northern Lebanon from Syrian patients injured during Syrian War [24]. The aim of this study was to characterise A. baumannii molecular epidemiology in Tripoli-Lebanon between 2011–2013 using blaOXA-51-like and Pasteur’s MLST typing and to determine the carbapenem resistance mechanisms.
Results
Bacterial isolates and identification
A total of 116 non-duplicate isolates were obtained between 2011 and 2013 from seven medical institutions in Tripoli: 73 isolates from Tripoli Governmental hospital, 34 from Nini hospital, four from Dar Al Chiffaa hospital, two from Monla, one isolate from each Hanane and Haykal hospitals and one from the private laboratory. Among those isolates, 59 had been obtained from Syrian refugees and 57 from Lebanese patients. They were all confirmed as A. baumannii by bla OXA-51 real time PCR and rpoB gene sequencing. These isolates were recovered from respiratory specimens (25/116; 21.6 %); wound (68/116; 58.6 %); urine (10/116; 8.6 %); catheter tips (8/116; 6.9 %), blood (1/116; 0.9 %) and other locations (3/116; 2.6 %). For one isolate, no information was available. Ninety patients were male and 26 female. Ages were between 1 month and 89 years with a mean of 40 years.
Antibiotic susceptibility and carbapenem resistance mechanisms
Most of the isolates exhibited multidrug-resistant phenotypes. Overall, 70 isolates were carbapenem resistant and among them, 65 carried the bla OXA-23 gene while 5 isolates carried the bla NDM-1 gene. ISAba1 was found in 101 isolates. The presence of ISAba1/bla OXA-23 association was confirmed in all OXA-23 producing isolates. The ISAba1/bla OXA-51 association was not detected. Among carbapenem-resistant A. baumannii, 43 had been isolated from Syrian refugees and 27 from Lebanese patients. The prevalence of carbapenem resistance was significantly higher among A. baumannii isolated from Syrian refugees (74 % vs. 47 %; P < 0.01).
Epidemiological typing
The bla OXA-51-like SBT revealed the presence of 14 different nucleotide variants. Of the 116 isolates, bla OXA-66 variant was the most prevalent and found in 73 isolates, followed by bla OXA-69 (20 isolates), bla OXA-64 (7 isolates), bla OXA-94 (5 isolates) and bla OXA-120 (2 isolates). Other variants, bla OXA-70, bla OXA-71, bla OXA-104, bla OXA-121, bla OXA-132 , bla OXA-406, KF048914, KJ584924, and AKAS01000012 were present sporadically in our collection. bla OXA-406 variant encoded a new protein (OXA-406) described for the first time in this study which differed from OXA-106 protein by a single amino acid at position 146 (lysine instead of asparagine).
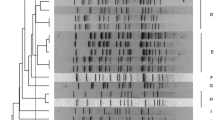
MLST was performed on a set of 57 randomly selected A. baumannii isolates representing all bla OXA-51 variants. A total of 17 ST(s), including 4 new ST(s), were identified (Table 1, Fig. 1). eBURST analysis showed that 12 of the 17 ST(s) were clustered into 9 CCs which were CC1, CC2, CC3, CC25, CC33, CC85, CC149, CC158, CC462. Additionally, ST108, ST150, ST154 were single locus variants of ST112, ST444 and ST611 respectively, and ST103 and ST461 were singletons.
Comparison between MLST and bla OXA-51-like SBT showed that isolates belonging to the same clonal complex carried all the same bla OXA-51 variant. Besides, each of the remaining lineages (single locus variants or singletons) that were identified had additionally a specific bla OXA-51-like variant (Table 1).
Discussion
Our study provided a global view of molecular epidemiology of A. baumannii isolates from hospitals in Tripoli, Lebanon. Tripoli is a city that hosts a large number of refugees and wounded Syrians, which may explain the high number of wound specimens in our collection. Although, A. baumannii is an opportunistic nosocomial pathogen, it is increasingly reported from infections occurring outside hospitals, particularly skin and soft-tissue infections and pneumonia [25]. A. baumannii has also been a well-documented pathogen associated with wound infections in USA troops from the Iraq and Afghanistan wars [26, 27]. The typology of these situations raised questions about their origins and the potential involvement of an environmental reservoir [25]. The origin of infections from Syrian patients was ambiguous. Although it was likely that nosocomial infections occurred, a number of infections were present at the time of admission of the patients in Lebanese hospitals [24]. These infections may have been acquired from environmental sources at the time of injury, during the patient stay in Syrian hospitals, or during a direct evacuation from the theatre of operations to Lebanon. Unfortunately, data concerning the date of injury, the length of hospitalisation, and the conditions of care and treatment in Syrian hospitals are lacking.
Approximately 60 % of our isolates showed a carbapenem resistance phenotype. The production of OXA-23 was the major carbapenem resistance mechanism, with an upstream insertion of ISAba1, thus supporting international data about the worldwide emergence of this carbapenemase [28–30]. Alarmingly, 5 NDM-1 producing isolates have been detected from 4 Syrian patients [24] and one from a Lebanese patient.
bla OXA-51-like is an intrinsic oxacillinase gene naturally occurring in A. baumannii, and more than 95 variants have been identified to date [31]. However, the occasional detection of bla OXA-51 in Acinetobacter nosocomialis and Acinetobacter genomic species “close to 13TU” limit its use as a single identification method. Therefore, it is always combined with others techniques [32, 33]. Genetic diversity of bla OXA-5 gene has been explored and found to be very interesting for identifying epidemic clones [16, 18, 19, 34, 35]. Thus, the full gene sequencing has been proposed as a single typing method for A. baumannii. As being simple and rapid, we have initially screened here the epidemiological belonging of our isolates to the previous identified clonal lineages by bla OXA-51-like SBT. We have then randomly selected isolates from each of the representative bla OXA-51-like sequences for MLST analysis. In our study, bla OXA-51-like gene sequencing correctly assigned all isolates to their corresponding clonal complexes. Here, the bla OXA-66 gene variant, which is associated with ST2 (belonging to CC2) [16, 19, 35, 36], was predominant and found in 63 % of the A. baumannii isolates. The isolates carrying the bla OXA-66 gene variant have been identified in samples obtained from the different hospitals in Tripoli. These findings are consistent with those observed worldwide since CC2 was reported in more than 34 countries in Europe, Asia, Africa, Australia, USA, and South America [36]. Eighty percent of our carbapenem resistant isolates belonged to this clone and OXA-23 was the only carbapenem resistance mechanism found. The high level of antimicrobial resistance may represent one of the main causes for its propensity and its successful predominance in hospitals throughout the world [10, 36]. The bla OXA-69 gene variant was the second gene mostly found in our collection. This gene was commonly associated with ST1 (belonging to CC1) but interestingly, we found two bla OXA-69 isolates belonging to the new sequence type ST460 (SLV of ST1). Both isolates were isolated from wounded Syrian patients. The bla OXA-94 was another bla OXA-51-like gene variant found in our study, it was associated with clonal complex CC85 (named as CC6 in the study of Pournaras et al. [19]). CC85 is currently formed by ST6, ST85, ST464, and ST528. In our study bla OXA-51-like SBT revealed the same sequence bla OXA-94 variant in the two identified sequences ST6 and ST85. We have recently detected ST464 in chicken and we found bla OXA- 94 as a bla OXA-51 variant [37]. Our 4 NDM-1 producing Syrian isolates belonged to ST85. Indeed, this ST has also been responsible for an outbreak in France. It is usually imported from North Africa [38, 39] and seems to be an emerging clone.
bla OXA-64 is a bla OXA-51-like variant associated with CC25 [19]. ST25 (the founder of CC25) was also an emerging clone reported in Europe, Asia, Africa and USA [36, 40], and from pets in Reunion Island, a French territory located in Western Indian Ocean [41].
Different carbapenemases have been identified in this clone, as OXA-23, OXA-24 and OXA-58 [36]. Otherwise, NDM-1 producing ST25 was also detected in Germany and Kenya [41–43]. Within our four identified isolates belonging to ST25, one isolate was a NDM-1 producing isolate recovered from a urine sample of an 80-year-old Lebanese patient suffering from amyloidosis and anaemia at Nini hospital, Tripoli, Lebanon. Finally, compared to carbapenem resistant isolates belonging to successful emerging clones, most of susceptible isolates were very diverse, belonging to different sequence types (Table 1).
Conclusions
In conclusion, this study highlights the emergence of NDM-1 and OXA-23 carbapenemases in Tripoli, Lebanon and the urgent need of effective measures to control the spread of A. baumannii in this country. It is noteworthy that Tripoli is located near the Syrian border and the microbial epidemiology is probably highly impacted by wounded Syrian refugees who can represent a reservoir of multidrug-resistant bacteria in hospitals. The higher prevalence of carbapenem-resistant A. baumannii among isolates from Syrian refugees was consistent with this hypothesis. Besides, we showed that bla OXA-51-like SBT is a reliable and fast method able to assign our isolates to their clonal complexes. Other multicentre studies are required to investigate the situation in other Lebanese cities that are possibly less concerned by the afflux of Syrian refugees fleeing war.
Methods
Bacterial isolates and Identification
The A. baumannii clinical isolates used in this study were collected between 2011 and 2013 from microbiological laboratories covering 6 hospitals in Tripoli, Lebanon: Tripoli Governmental hospital (100 beds), Nini (120 beds), Dar Al Chiffaa (120 beds), Monla (120 beds), Hanane (45 beds), and Haykal (125 beds) hospitals and one private laboratory. Isolates were sent to Azm Center for Research in Biotechnology and its application and stored at-80 °C. This study was also approved by the ethical committee of Azm center under the authorization N° 07/2012. Bacterial identification was initially performed by matrix assisted laser ionization time of flight mass spectrometry (MALDI-TOF MS) using the Vitek®MS (bioMérieux, Marcyl’Étoile, France) and the identification of A. baumannii at species level was confirmed by real time PCR of the bla OXA-51 gene [44] and partial RNA polymerase ß-subunit (rpoB) gene sequencing [45].
Susceptibility testing and detection of carbapenemases
Antibiotic susceptibility testing was performed by the disc diffusion method according to the recommendations of the French Society of Microbiology (www.sfm-microbiologie.org/). A panel of 14 antibiotics was tested including ticarcillin, ticarcillin/clavulanic acid, piperacillin/tazobactam, ceftazidime, imipenem, ciprofloxacin, amikacin, gentamicin, tobramycin, trimethoprim/sulfamethoxazole, colistin, netilmicin, doxycycline and rifampicin. Carbapenem resistance was confirmed by determining minimum inhibitory concentration (MICs) against imipenem, meropenem and doripenem by Etest®strips (bioMérieux). Carbapenem resistant isolates were investigated by PCR assays for the presence of carbapenemase-encoding genes bla OXA-23 [46], bla OXA-24 [46], bla OXA-58 [46], bla OXA-143 [6], bla NDM-1 [47], bla IMP [5], bla VIM [5], bla KPC [48] and the insertion sequence ISAba1 [49]. The presence of ISAba1 upstream bla OXA-23 or bla OXA-51 genes was searched using a combination of ISAba1 primers with reverse primers of bla OXA-23 or bla OXA-51 respectively.
Epidemiological typing
Epidemiological typing of all isolates was carried out by bla OXA-51-like sequence based typing (SBT) as described previously [16]. The sequences were compared to all variants present in BLAST. Each new sequence detected was submitted to GenBank and assigned by Lahey database for beta-lactamase classification (http://www.lahey.org/studies/webt.asp). MLST was performed on a panel of 57 isolates according to the Pasteur scheme (http://www.pasteur.fr/mlst). When a new allele or a new sequence type (ST) was identified, it was submitted to Pasteur Institute MLST Database. eBURST (http://eburst.mlst.net/) was applied to compare identified ST(s) to available ST(s) present in MLST Database (last update 22.10.2014). A clonal complex (CC) was defined as a set formed by the founder ST and its single locus variants (SLV) [10].
Nucleotide sequence accession numbers and novel sequence types
Four newly identified ST(s) have been coded by MLST Pasteur as ST459, ST460, ST461 and ST462. A new nucleotide variant of bla OXA-51 was submitted to GenBank under the submission number [GenBank: KJ584915] and assigned by Lahey center as bla OXA-406.
Statistical analysis
The comparison of the prevalence of carbapenem-resistant A. baumannii in isolates from Syrian refugees and in isolates from Lebanese patients was performed with the Chi-square for test. A P < 0.05 was considered significant.
References
Joly-Guillou M-L. Clinical impact and pathogenicity of Acinetobacter. Clin Microbiol Infect. 2005;11:868–73.
Kempf M, Rolain J-M. Emergence of resistance to carbapenems in Acinetobacter baumannii in Europe: clinical impact and therapeutic options. Int J Antimicrob Agents. 2012;39:105–14.
Hsueh P-R, Teng L-J, Chen C-Y, Chen W-H, Yu C-J, Ho S-W, et al. Pandrug-resistant Acinetobacter baumannii causing nosocomial infections in a university hospital, Taiwan. Emerg Infect Dis. 2002;8:827–32.
Sader HS, Farrell DJ, Flamm RK, Jones RN. Antimicrobial susceptibility of Gram-negative organisms isolated from patients hospitalized in intensive care units in United States and European hospitals (2009–2011). Diagn Microbiol Infect Dis. 2014;78:443–8.
Bonnin RA, Nordmann P, Poirel L. Screening and deciphering antibiotic resistance in Acinetobacter baumannii: a state of the art. Expert Rev Anti Infect Ther. 2013;11:571–83.
Higgins PG, Lehmann M, Seifert H. Inclusion of OXA-143 primers in a multiplex Polymerase Chain Reaction (PCR) for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int J Antimicrob Agents. 2010;35:305–14.
Higgins PG, Pérez-Llarena FJ, Zander E, Fernández A, Bou G, Seifert H. OXA-235, a novel class D β-lactamase involved in resistance to carbapenems in Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57:2121–6.
Dortet L, Poirel L, Nordmann P. Worldwide dissemination of the NDM-Type carbapenemases in Gram-negative bacteria. BioMed Res Int. 2014;2014:249856.
Zarrilli R, Pournaras S, Giannouli M, Tsakris A. Global evolution of multidrug-resistant Acinetobacter baumannii clonal lineages. Int J Antimicrob Agents. 2013;41:11–9.
Diancourt L, Passet V, Nemec A, Dijkshoorn L, Brisse S. The population structure of Acinetobacter baumannii: expanding multiresistant clones from an ancestral susceptible genetic pool. PLoS One. 2010;5, e10034.
Seifert H, Dolzani L, Bressan R, van der Reijden T, van Strijen B, Stefanik D, et al. Standardization and interlaboratory reproducibility assessment of pulsed-field gel electrophoresis-generated fingerprints of Acinetobacter baumannii. J Clin Microbiol. 2005;43:4328–35.
Nemec A, Dijkshoorn L, van der Reijden TJK. Long-term predominance of two pan-European clones among multi-resistant Acinetobacter baumannii strains in the Czech Republic. J Med Microbiol. 2004;53:147–53.
Higgins, Dammhayn C, Hackel M, Seifert H. Global spread of carbapenem-resistant Acinetobacter baumannii. J Antimicrob Chemother. 2010;65:233–8.
Rafei R, Kempf M, Eveillard M, Dabboussi F, Hamze M, Joly-Guillou M-L. Current molecular methods in epidemiological typing of Acinetobacter baumannii. Future Microbiol. 2014;9:1179–94.
Bartual SG, Seifert H, Hippler C, Luzon MAD, Wisplinghoff H, Rodríguez-Valera F. Development of a multilocus sequence typing scheme for characterization of clinical isolates of Acinetobacter baumannii. J Clin Microbiol. 2005;43:4382–90.
Hamouda A, Evans BA, Towner KJ, Amyes SGB. Characterization of epidemiologically unrelated Acinetobacter baumannii isolates from four continents by use of multilocus sequence typing, pulsed-field gel electrophoresis, and sequence-based typing of blaOXA-51-like genes. J Clin Microbiol. 2010;48:2476–83.
Park YK, Jung S-I, Park K-H, Cheong HS, Peck KR, Song J-H, et al. Independent emergence of colistin-resistant Acinetobacter spp. isolates from Korea. Diagn Microbiol Infect Dis. 2009;64:43–51.
Zander E, Nemec A, Seifert H, Higgins PG. Association between β-lactamase-encoding bla(OXA-51) variants and DiversiLab rep-PCR-based typing of Acinetobacter baumannii isolates. J Clin Microbiol. 2012;50:1900–4.
Pournaras S, Gogou V, Giannouli M, Dimitroulia E, Dafopoulou K, Tsakris A, et al. Single locus sequence-based typing of blaOXA-51-like gene for rapid classification of Acinetobacter baumannii clinical isolates to international clones. J Clin Microbiol. 2014;52:1653–7.
Rafei R, Dabboussi F, Hamze M, Eveillard M, Lemarié C, Gaultier M-P, et al. Molecular analysis of Acinetobacter baumannii strains isolated in Lebanon using four different typing methods. PLoS One. 2014;9, e115969.
Zarrilli R, Vitale D, Di Popolo A, Bagattini M, Daoud Z, Khan AU, et al. A plasmid-borne blaOXA-58 gene confers imipenem resistance to Acinetobacter baumannii isolates from a Lebanese hospital. Antimicrob Agents Chemother. 2008;52:4115–20.
Di Popolo A, Giannouli M, Triassi M, Brisse S, Zarrilli R. Molecular epidemiological investigation of multidrug-resistant Acinetobacter baumannii strains in four Mediterranean countries with a multilocus sequence typing scheme. Clin Microbiol Infect. 2011;17:197–201.
Giannouli M, Tomasone F, Agodi A, Vahaboglu H, Daoud Z, Triassi M, et al. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii strains in Intensive Care Units of multiple Mediterranean hospitals. J Antimicrob Chemother. 2009;63:828–30.
Rafei R, Dabboussi F, Hamze M, Eveillard M, Lemarié C, Mallat H, et al. First report of blaNDM-1-producing Acinetobacter baumannii isolated in Lebanon from civilians wounded during the Syrian war. Int J Infect Dis. 2014;21:21–3.
Eveillard M, Kempf M, Belmonte O, Pailhoriès H, Joly-Guillou M-L. Reservoirs of Acinetobacter baumannii outside the hospital and potential involvement in emerging human community-acquired infections. Int J Infect Dis. 2013;17:e802–5.
O’Shea MK. Acinetobacter in modern warfare. Int J Antimicrob Agents. 2012;39:363–75.
Sheppard FR, Keiser P, Craft DW, Gage F, Robson M, Brown TS, et al. The majority of US combat casualty soft-tissue wounds are not infected or colonized upon arrival or during treatment at a continental US military medical facility. Am J Surg. 2010;200:489–95.
Mugnier PD. Worldwide Dissemination of the blaOXA-23 Carbapenemase Gene of Acinetobacter baumannii. Emerg Infect Dis. 2010;16:35–40.
Grosso F, Carvalho KR, Quinteira S, Ramos A, Carvalho-Assef APD, Asensi MD, et al. OXA-23-producing Acinetobacter baumannii: a new hotspot of diversity in Rio De Janeiro? J Antimicrob Chemother. 2011;66:62–5.
Principe L, Piazza A, Giani T, Bracco S, Caltagirone MS, Arena F, et al. Epidemic diffusion of OXA-23-producing Acinetobacter baumannii in Italy: results of the first cross-sectional countrywide survey. J Clin Microbiol. 2014;52:3004–10.
Evans BA, Amyes SGB. OXA β-Lactamases. Clin Microbiol Rev. 2014;27:241–63.
Zander E, Higgins PG, Fernández-González A, Seifert H. Detection of intrinsic blaOXA-51-like by multiplex PCR on its own is not reliable for the identification of Acinetobacter baumannii. Int J Med Microbiol IJMM. 2013;303:88–9.
Lee Y-T, Turton JF, Chen T-L, Wu RC-C, Chang W-C, Fung C-P, et al. First identification of blaOXA-51-like in non-baumannii Acinetobacter spp. J Chemother Florence Italy. 2009;21:514–20.
Aly M, Tayeb HT, Al Johani SM, Alyamani EJ, Aldughaishem F, Alabdulkarim I, et al. Genetic diversity of OXA-51-like genes among multidrug-resistant Acinetobacter baumannii in Riyadh, Saudi Arabia. Eur J Clin Microbiol Infect Dis. 2014;33:1223–8.
Evans BA, Hamouda A, Towner KJ, Amyes SGB. OXA-51-like beta-lactamases and their association with particular epidemic lineages of Acinetobacter baumannii. Clin Microbiol Infect. 2008;14:268–75.
Karah N, Sundsfjord A, Towner K, Samuelsen Ø. Insights into the global molecular epidemiology of carbapenem non-susceptible clones of Acinetobacter baumannii. Drug Resist Updat. 2012;15:237–47.
Rafei R, Hamze M, Pailhoriès H, Eveillard M, Marsollier L, Joly-Guillou M-L, et al. Extrahuman Epidemiology of Acinetobacter baumannii in Lebanon. Appl Environ Microbiol. 2015;81:2359–67.
Decousser J, Jansen C, Nordmann P, Emirian A, Bonnin R, Anais L, et al. Outbreak of NDM-1-producing Acinetobacter baumannii in France, January to May 2013. Euro Surveill. 2013;18:20547.
Bonnin RA, Cuzon G, Poirel L, Nordmann P. Multidrug-resistant Acinetobacter baumannii clone, France. Emerg Infect Dis. 2013;19:822–3.
Revathi G, Siu LK, Lu P-L, Huang L-Y. First report of NDM-1-producing Acinetobacter baumannii in East Africa. Int J Infect Dis. 2013;17:e1255–8.
Belmonte O, Pailhoriès H, Kempf M, Gaultier MP, Lemarié C, Ramont C, et al. High prevalence of closely-related Acinetobacter baumannii in pets according to a multicentre study in veterinary clinics, Reunion Island. Vet Microbiol. 2014;170:446–50.
Pfeifer Y, Wilharm G, Zander E, Wichelhaus TA, Göttig S, Hunfeld K-P, et al. Molecular characterization of blaNDM-1 in an Acinetobacter baumannii strain isolated in Germany in 2007. J Antimicrob Chemother. 2011;66:1998–2001.
Bonnin RA, Poirel L, Naas T, Pirs M, Seme K, Schrenzel J, et al. Dissemination of New Delhi metallo-β-lactamase-1-producing Acinetobacter baumannii in Europe. Clin Microbiol Infect. 2012;18:E362–5.
Kempf M, Rolain J-M, Diatta G, Azza S, Samb B, Mediannikov O, et al. Carbapenem resistance and Acinetobacter baumannii in Senegal: the paradigm of a common phenomenon in natural reservoirs. PLoS One. 2012;7, e39495.
Gundi VAKB, Dijkshoorn L, Burignat S, Raoult D, La Scola B. Validation of partial rpoB gene sequence analysis for the identification of clinically important and emerging Acinetobacter species. Microbiology. 2009;155:2333–41.
Mesli E, Berrazeg M, Drissi M, Bekkhoucha SN, Rolain J-M. Prevalence of carbapenemase-encoding genes including New Delhi metallo-β-lactamase in Acinetobacter species, Algeria. Int J Infect Dis. 2013;17:e739–43.
Bonnin RA, Naas T, Poirel L, Nordmann P. Phenotypic, biochemical, and molecular techniques for detection of Metallo-?-Lactamase NDM in Acinetobacter baumannii. J Clin Microbiol. 2012;50:1419–21.
Hong SS, Kim K, Huh JY, Jung B, Kang MS, Hong SG. Multiplex PCR for rapid detection of genes encoding Class A carbapenemases. Ann Lab Med. 2012;32:359–61.
Ruiz M, Marti S, Fernandez-Cuenca F, Pascual A, Vila J. Prevalence of IS(Aba1) in epidemiologically unrelated Acinetobacter baumannii clinical isolates. Clin Microbiol Infect. 2007;13:1192–8.
Acknowledgements
We thank the team of the curators of the Institut Pasteur MLST system (Paris, France) for importing novel alleles, profiles and/or isolates at http://www.pasteur.fr/mlst.
We are very grateful to all laboratory directors for their collaboration in this study: Dr. Marcel El Achkar, Dr. Fadel Moukkadem, Dr. Ibtihal Kassam, Dr. Rikardo Sarraf, Dr. Nathalie Sapiroua, Dr. Gilbert karayakoupoglou, Dr. Samir Ghanem.
We also thank Catherine Quinqueneau, Catherine Ramont, Cyrielle Lebreton, Mariam Yehya and Taha Abdo for excellent technical assistance. This work was supported in part by AZM and SAADE Association.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RR performed bacterial identifications and antibiograms, carried out molecular studies. HP and MK carried out molecular studies. RR and MK drafted the manuscript. ME, MLJG and MK were involved in revision of the manuscript for important intellectual content. MH, HM and FD isolated bacterial strains in Lebanon. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Rafei, R., Pailhoriès, H., Hamze, M. et al. Molecular epidemiology of Acinetobacter baumannii in different hospitals in Tripoli, Lebanon using bla OXA-51-like sequence based typing. BMC Microbiol 15, 103 (2015). https://doi.org/10.1186/s12866-015-0441-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-015-0441-5