Abstract
Background
Gestational diabetes (GDM) is increasingly common and has significant implications during pregnancy and for the long-term health of the mother and offspring. However, it is a heterogeneous condition with inter-related factors including ethnicity, body mass index and gestational weight gain significantly modifying the absolute risk of complications at an individual level. Predicting the risk of pregnancy complications for an individual woman with GDM presents a useful adjunct to therapeutic decision-making and patient education. Diagnostic prediction models for GDM are prevalent. In contrast, prediction models for risk of complications in those with GDM are relatively novel. This study will systematically review published prognostic prediction models for pregnancy complications in women with GDM, describe their characteristics, compare performance and assess methodological quality and applicability.
Methods
Studies will be identified by searching MEDLINE and Embase electronic databases. Title and abstract screening, full-text review and data extraction will be completed independently by two reviewers. The included studies will be systematically assessed for risk of bias and applicability using appropriate tools designed for prediction modelling studies. Extracted data will be tabulated to facilitate qualitative comparison of published prediction models. Quantitative data on predictive performance of these models will be synthesised with meta-analyses if appropriate.
Discussion
This review will identify and summarise all published prognostic prediction models for pregnancy complications in women with GDM. We will compare model performance across different settings and populations with meta-analysis if appropriate. This work will guide subsequent phases in the prognosis research framework: further model development, external validation and model updating, and impact assessment. The ultimate model will estimate the absolute risk of pregnancy complications for women with GDM and will be implemented into routine care as an evidence-based GDM complication risk prediction model. It is anticipated to offer value to women and their clinicians with individualised risk assessment and may assist decision-making. Ultimately, this systematic review is an important step towards a personalised risk-stratified model-of-care for GDM to allow preventative and therapeutic interventions for the maximal benefit to women and their offspring, whilst sparing expense and harm for those at low risk.
Systematic review registration
PROSPERO registration number CRD42019115223
Similar content being viewed by others
Background
Gestational diabetes (GDM) is a state of carbohydrate intolerance resulting in hyperglycaemia that commences or is first recognised during pregnancy [1]. The prevalence of GDM is rising in the context of increasing maternal age and obesity, and introduction of new diagnostic criteria [2], representing a public health concern internationally [1]. Recent data found the prevalence of GDM to be approximately 13% [3], while in high-risk populations including some ethnic groups, prevalence is as high as 30% [4].
A diagnosis of GDM implies a state of glucometabolic dysfunction which is associated with an increased risk of pregnancy complications affecting the mother and fetus as well as having significant implications for the long-term health of the mother and offspring [5]. Landmark randomised controlled trials have demonstrated reduction in pregnancy risks with GDM management consisting of lifestyle modification and pharmacologic therapy, albeit based on less inclusive diagnostic criteria [6, 7].
New consensus-based diagnostic criteria were developed by the International Association of Diabetes in Pregnancy Study Groups (IADPSG) [8]. These criteria that generally include lower glucose cut-off levels are based on observational data [9] and remain highly controversial. These were endorsed by the World Health Organisation (WHO) and subsequently recommended by some [10] but not all professional societies [11]. Other societies acknowledge that different diagnostic criteria exist and that the optimal diagnostic strategies may vary depending on the characteristics of the local population [12,13,14].
Contemporary approaches to the diagnosis and management of GDM, regardless of diagnostic criteria, are glucocentric [15, 16]. Risks related to glucometabolic dysfunction are dichotomised on blood glucose levels into a binary yes/no GDM state. A one-size-fits-all model of intervention is then implemented, targeting glucose levels alone. This approach fails to appreciate the continuum of risk associated with blood glucose levels and the increased clinical heterogeneity of this condition, related primarily to ethnicity [17], increasing obesity [18, 19] and increasing excess gestational weight gain (GWG) [20]. These risk factors independently affect risk of diagnosis of GDM and short and long-term health outcomes for affected women [17,18,19,20]. This heterogeneity is likely explained by emerging physiologic data suggesting highly variable degrees of beta-cell function and insulin resistance amongst women diagnosed with this condition [21].
Limitations of this glucocentric approach and lack of risk stratification are evident from epidemiologic outcome data following the adoption of the new IADPSG diagnostic criteria. As expected, the application of these criteria have led to an increase in GDM incidence, with maternity centres reporting increases in the number of diagnoses by 28 to 74% [22,23,24,25]. This increasing incidence is most likely due to a change from a two- to one-step testing procedure and more inclusive blood glucose level criteria rather than changes in population characteristics. As such, a greater proportion of pregnancies are identified as being at high risk and treated with a package of care that includes additional education, lifestyle modification and pharmacologic therapy. However, intervening in a greater proportion of pregnancies has not led to an overall reduction in pregnancy complications [22, 26, 27] yet has increased the overall costs of GDM care [22] and psychosocial burden for affected women [28]. Therefore, there is a mandate to develop a more sophisticated prognosis and risk-stratified focused approach to GDM considering other relevant clinical factors driving adverse outcomes in addition to glycaemic measures.
A suitable and effective prognostic prediction model will allow calculation of the absolute risk of pregnancy complications for women with GDM who present for pregnancy-care based on their unique individual characteristics including BMI, GWG, ethnicity and obstetric history. Calculation of absolute risk of complications can then facilitate the development of stratified models-of-care that better meet the needs of women with this heterogeneous condition. This personalised medicine approach will facilitate the transition to a model-of-care where education, resources and specialist-care can be directed to those women most likely to benefit and sparing expense and unnecessary treatment from those who will not.
This review will answer the question, what prognostic prediction models have been developed for application to pregnancies affected by GDM to predict pregnancy complications and inform clinical therapeutic decision-making?
The objectives of this systematic review are
-
1.
To identify existing prognostic prediction models for pregnancy complications in women with GDM;
-
2.
To describe characteristics of the identified prognostic prediction models qualitatively;
-
3.
To compare the performance of identified prognostic prediction models quantitatively across different settings and populations with the use of meta-analysis if appropriate;
-
4.
To critically assess the conduct and reporting of methods of these prediction studies.
Methods/design
This protocol is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) guideline [29] and the corresponding checklist used (Additional file 2). This systematic review protocol was registered on the PROSPERO international registry of systematic reviews on January 18, 2019 (CRD42019115223).
A systematic review of prediction modelling studies for pregnancy complications in women with GDM will be conducted to identify eligible studies published before December 2018. This review forms the foundations of a broader research program guided by the recommendations of The PROGnosis RESearch Strategy (PROGRESS) Partnership, an international, interdisciplinary collaboration that has published a framework to improve the standards of prognosis research to improve its translational impact. The framing of the review question (Table 1), study design, data extraction and appraisal will be guided by recent developments in prognosis research methodology, which seek to improve rigour and reproducibility. This includes the Cochrane Prognosis Methods Group Protocol Template [33], the TRIPOD statement (transparent reporting of a multivariable prediction model for individual prognosis or diagnosis) [34], the CHARMS checklist (checklist for critical Appraisal and data extraction for systematic reviews of prediction modelling studies) [30] and the PROBAST tool (prediction model risk of bias assessment) [35].
Eligibility criteria
Study selection will be based on pre-determined eligibility criteria framed using the PICOTS system [36] (Table 2). PICOTS is a modification of the established PICO system tailored to the specific requirements of systematic reviews of prediction models with additional consideration for timing (both for the time period of the prediction and the time point at which the prediction model is to be used) and clinical setting [35].
Population
Studies reporting on prediction models proposed for pregnant women with GDM will be considered for inclusion. GDM may have been diagnosed by any criteria. Studies proposing models for pregnant women with pre-gestational diabetes (type 1 and type 2 diabetes) will be excluded.
Intervention
Prediction model development studies with and without external validation and external model validation studies with or without model updating will be considered for inclusion if they are intended to inform clinicians’ therapeutic decision making regarding the management of a pregnancy affected by GDM.
Outcomes
The included pregnancy complications related to GDM and their prioritisation were aligned with those agreed by consensus of the Cochrane Pregnancy and Childbirth Group responsible for systematic reviews for prevention and treatment of GDM and pre-existing diabetes [31, 32] and drew on published search strategies for similar review questions [20, 38]. The timing and effect measures for each outcome will be as defined by the study’s authors. Complications potentially related to the treatment of GDM such as maternal hypoglycaemia and glycaemic control were not included. GWG was not included as it is also likely to be a predictor of the outcomes of interest.
Timing
Included studies need to report on prediction models for complications occurring during pregnancy or the postpartum period or affecting the neonate. The standard definition of neonate will be used, that is, an infant during the first 28 days after birth. Prediction models for complications with onset after this period will be excluded.
Setting
Prediction models that are intended to be used by healthcare professionals in the antenatal clinic setting, at any time during pregnancy will be considered for inclusion. Models intended to be used before (pre-conception) or after (post-partum) will be excluded.
Types of studies and limits
Any study design including primary research (e.g. randomised controlled trial or observational study) that reports on one or more statistical models, tools or scores with at least two predictors proposed to predict an individual’s risk of a future outcome (prediction modelling studies) will be considered for inclusion. Other names for prediction models include prognostic model, prognostic (or prediction) index or rule, risk (or clinical) prediction model and predictive model. Risk predictions are usually expressed in absolute terms as a probability, i.e. 0 to 100% (but can be relative (risk score) [39]. Any identified and relevant review articles will be used to identify eligible primary studies.
Studies will be limited to those conducted in humans by applying The Cochrane Group’s filter for Humans not Animals filter [40]. There will be no limits on the year of publication hence included articles will be from all years in the MEDLINE (from 1946) and Embase (from 1947) databases. No restriction to language of publication will be applied.
Search methods for identification of studies
Information sources
The following electronic databases will be searched to identify eligible studies:
-
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process and Other Non-Indexed Citations, Daily and Versions(R) on OvidSP (from 1946 to present)
-
Embase Classic+Embase on OvidSP (from 1947 to present)
The reference list of included studies will be hand searched for additional potentially relevant citations.
Search strategy
A sensitive search strategy, based on the eligibility criteria and combining subject indexing terms (i.e. MeSH) and free-text search terms in the title and abstract fields, will be developed for MEDLINE using the OvidSP platform. The search strategy, specifically, subject indexing terms will be translated appropriately for Embase.
The search strategy will be iteratively developed and refined with the assistance of clinical advisors (HJT, JAB and GS), a medical librarian and an evidence synthesis expert. The final search strategy will combine concepts related to prognostic factors and prediction modelling studies, GDM and pregnancy complications. The updated version of a validated filter for prediction modelling studies published by Geersing and colleagues [41] (based on the original published by Ingui and colleagues [42]) will be used. For GDM, a search strategy published in a peer-reviewed systematic review of treatments for this condition will be used [43]. These two concepts will be combined with a bespoke search strategy for pregnancy complications related to GDM defined as the outcomes of interest in the eligibility criteria (Table 2). The draft search strategy is provided in Additional file 1: Table S1.
A backward citation search will be conducted on all model development studies. All retrieved studies will be reviewed to identify all relevant external validation studies.
Data collection and analysis
Data management
Retrieved studies will be imported into Endnote reference manager software. (Version X8.2, Clarivate Analytics, Philadelphia, USA. Available at https://endnote.com/) Duplicate records will be identified and excluded using a systematic, rigorous and reproducible method utilising a sequential combination of fields including author, year, title, journal and pages [44]. Covidence systematic review software will be used to manage records throughout the review. (Veritas Health Innovation, Melbourne, Australia. Available at http://www.covidence.org).
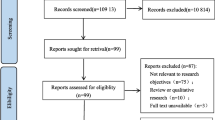
Selection process
Two reviewers (SDC, LAW) will independently screen the titles and abstracts of every article retrieved by the search strategy according to the selection criteria (Table 2). Full text of the articles will be retrieved for further assessment if the information given suggests that the study meets the selection criteria or if there is any doubt regarding eligibility of the article based on the information given in the title and abstract. Any disagreement will be resolved by discussion to reach a consensus and consultation with an advisor (HJT) if required. For publications in languages other than English portions of the title, abstract and full-text article will be translated as necessary. A record of all retrieved studies will be maintained and reasons for exclusion documented.
Data extraction
Two reviewers (SDC, LAW) will independently extract the data from the included studies using a standardised electronic form developed with reference to the CHecklist for critical Appraisal and data extraction for systematic Reviews of prediction Modelling Studies (CHARMS) [30]. Variables for which data will be sought will include information on objective, source of data, participants, outcome(s) to be predicted, candidate predictors, sample size, missing data, model development, model performance (discrimination, calibration and measures of case-mix variation), results including final multivariable models and interpretation of presented models [30]. Data on diagnostic approach for GDM used (diagnostic criteria, testing procedures and screening policies), whether population was treated and treatment type will also be extracted. Any disagreement will be resolved by discussion to reach a consensus and consultation with an advisor (HJT) if required. Missing data will be obtained from the authors wherever possible; if insufficient information is obtained the study will be excluded.
Critical appraisal
The methodological quality (risk of bias) and relevance (applicability) to the review question of included studies will be systematically assessed using the prediction model risk of bias assessment tool (PROBAST) [35]. This tool is structured around four key domains: participants, predictors, outcome and analysis. Each domain is rated as “high”, “low” or “unclear” risk of bias. Two reviewers (SDC, LAW) will independently evaluate the risk of bias and applicability of each included study. Any disagreement will be resolved by discussion to reach a consensus and consultation with an advisor (HJT) if required. Results will be presented graphically with each study given a rating of low, unclear or high risk for each of the four domains.
Qualitative data synthesis of prediction models
All extracted data on prediction models from included studies will be tabulated to facilitate comparison of outcomes to be predicted, predictors included in the final model and performance measures [30, 38]. Measures of uncertainty will be reported when published or approximated using published methods [36]. Where reported, classification measures such as sensitivity, specificity, positive predictive value and negative predictive value will also be included [30, 38]. A descriptive analysis of key items will also be presented.
Quantitative analysis and comparison of the predictive performance of prediction models
The nature of the quantitative analysis will be dependent on the number of prediction models identified in the systematic review and the type of prediction modelling study (i.e. development or validation).
Data will be synthesised by performing meta-analysis by type of prediction modelling study if feasible and identified prediction models are sufficiently homogenous. Clinical homogeneity will be satisfied if the review identifies:
-
a)
Multiple validation studies for a common prediction model are identified or
-
b)
Multiple development studies where the target population to whom the model applies, outcome to be predicted and intended moment of using the model are considered similar.
Meta-analysis and investigation of heterogeneity
Where meta-analysis is feasible, performance measures such as discrimination (e.g. concordance (c) statistic or area under the curve) and calibration (e.g. total number of observed to expected events ratio [total O:E ratio]] and calibration slope) will be will be pooled and analysed using a random-effects meta-analysis model to provide estimates of the average performance of the model across the included studies. To estimate the between-study heterogeneity and the 95% confidence intervals for this average performance, the restricted maximum likelihood and the Hartung-Knapp-Sidik-Jonkman methods will be used respectively [36]. Meta-analysis will be conducted with reference to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group guidelines [45] using the metareg module in Stata (StataCorp).
Heterogeneity in performance measures is anticipated and will likely reflect the heterogeneity of study design and population [36]. The range of potential model performance in a different population in a new validation study will be estimated by calculating an approximate 95% prediction interval [36]. Case-mix variation within each study will be quantified by estimating the standard deviation of the linear predictor [36]. When performance measures or measures of uncertainty have not been reported, they will be approximated where possible using appropriate methods [36]. Statistical homogeneity will be assessed using the I2 test where I2 values over 50% indicate moderate to high heterogeneity [46]. Potential sources of heterogeneity will be investigated by undertaking a meta-regression analysis.
Analysis of subgroups
Where there are sufficient number of included studies sub-group analyses will be undertaken.
Subgroup analyses will be conducted according to the type of prediction modelling study (development and/or validation), target population to whom the prediction model applies as defined by diagnostic approach to GDM (diagnostic criteria, testing procedures and screening policies), testing procedures or screening policies for GDM used, whether population was treated (yes/no), treatment type, outcome to be predicted, intended moment of using the model and study quality (risk of bias).
Sensitivity analysis
Sensitivity analyses will be performed for studies at lower and higher risk of bias to explore the influence of risk of bias on effect size [36].
Reporting and presentation of findings
Reporting and presentation of results will be guided by the PRISMA statement (preferred reporting items for systematic reviews and meta-analyses) [47]. Relevant recommendations from the TRIPOD statement (transparent reporting of a multivariable prediction model for individual prognosis or diagnosis) [34] will also be considered.
The GRADE approach (grading of recommendations, assessment, development and evaluation) will be applied to determine confidence in estimates [48, 49].
Discussion
This systematic review will identify all published prognostic prediction models for pregnancy complications in women with GDM. These prognostic prediction models will be comprehensively summarised and their performance compared across different settings and populations with meta-analysis if appropriate.
A prognostic prediction model for GDM that is intended to aid therapeutic decision-making during pregnancy would ideally integrate clinically meaningful and patient aligned outcomes including pregnancy complications affecting mother and baby. Long-term outcomes affecting maternal health such as progression to type 2 diabetes and resultant increased cardiovascular risk for mother and affecting offspring health such as increased risk of childhood obesity for offspring are important. However, they are less likely to have a significant bearing on clinical decision-making during the pregnancy itself. Rather prediction of long-term risks should facilitate the targeting of preventative interventions post-partum.
Prognosis-related research in GDM is a relatively novel field of enquiry. The glucometabolic health and outcomes of a pregnant woman are influenced by a number of clinical factors, including glucose levels, body mass index (BMI), GWG and ethnicity [17,18,19,20]. These predictors have been incorporated into prediction models but to date, the focus has been on GDM diagnosis rather than prognosis after GDM diagnosis. Diagnostic prediction models seek to predict the risk of GDM diagnosis based on routinely available clinical parameters with a view to directing screening and/or primary prevention efforts. Multiple diagnostic prediction models have been developed [38], including our own [50], and 12 were recently externally validated and compared head-to-head in a prospective cohort [51].
The utility of diagnostic prediction models for GDM diagnosis is limited in contemporary clinical practice because case-finding based on high-predicted risk of diagnosis has been superseded by universal screening at 24–28 weeks gestation in most guidelines. Furthermore, guidelines are increasingly recommending first-trimester screening for type 2 diabetes in women at high risk, identified by the presence of one or more risk factors [10, 12, 13]. Although widely assumed in routine clinical practice the benefit of early diagnosis and treatment is yet to be demonstrated and thus is currently subject to a randomised controlled trial [52].
This review will make an important contribution to the understanding of the risk of pregnancy complications for women with GDM. Furthermore, it will promote the consideration of the broad continuum of risk related to this condition in routine clinical practice. If this review does not identify any applicable models or applicable models have poor performance and or methodological quality, then these results will provide rationale and guidance for model development and/or updating. Conversely, if this review identifies a prognostic model with high predictive performance, applicability and methodological quality, then such a model could be implemented and would be valuable to clinicians caring for women with GDM. It would allow clinicians to predict an individual’s absolute risk of pregnancy complications. This prediction could also help affected women understand the implications of GDM on their pregnancy and in doing so, promote shared decision-making with clinicians that consider individual risk estimated objectively and systematically. At a health service level, the implementation of such prediction models would support a personalised risk-stratified model-of-care, which would ultimately better direct finite health resources to women at high-risk and most likely to benefit from intervention.
As such, this systematic review serves as the foundation for a body of work to develop, validate, implement and evaluate the impact of a prognostic prediction model for pregnancy complications related to GDM across the four themes of the PROGRESS prognosis research framework [53]. Theoretical prediction models not implemented into clinical practice are a waste of research effort and resources. Hence, the authors’ will adopt a model aggregation approach to develop a meta-model which optimally captures prior knowledge by combining model validation and updating of the existing prediction models identified in this review [54]. The performance of the meta-model will be compared to existing single models identified in this review, facilitating the selection of the prognostic prediction model most suitable for application into clinical practice. This model will become the subject of implementation research. An impact study will be designed and conducted to compare a model-of-care based on the directive use of the prediction model to stratify women to targeted interventions based on their risk of pregnancy complications compared to usual care [55]. Such a study would also facilitate evaluation of the implementation of this prognostic model into the model-of-care including its acceptability to clinicians and impact on health service utilisation and costs.
Ultimately, this systematic review is an important step towards developing and implementing personalised risk-stratified models-of-care for GDM. This will allow preventative and therapeutic interventions to be precisely targetted at women most likely to benefit, and sparing expense and harm for those who will not.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed.
Abbreviations
- BMI:
-
Body mass index
- CHARMS:
-
CHecklist for critical Appraisal and data extraction for systematic Reviews of prediction Modelling Studies
- GDM:
-
Gestational diabetes mellitus
- GRADE:
-
Grading of Recommendations, Assessment, Development and Evaluation
- GWG:
-
Gestational weight gain
- IADPSG:
-
The International Association of Diabetes in Pregnancy Study Groups
- MOOSE:
-
Meta-analysis of Observational Studies in Epidemiology
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-analyses
- PROGRESS:
-
PROGnosis RESearch Strategy
- TRIPOD:
-
Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis
References
National Institutes of Health consensus development conference statement: diagnosing gestational diabetes mellitus, March 4–6, 2013. Obstet Gynecol. 2013;122(2 Pt 1):358–69.
Nankervis A, McIntyre HD, Moses RG, Ross GP, Callaway LK. Testing for gestational diabetes mellitus in Australia. Diabetes Care. 2013;36(5):e64.
Moses RG, Wong VC, Lambert K, Morris GJ, San GF. The prevalence of hyperglycaemia in pregnancy in Australia. Aust N Z J Obstet Gynaecol. 2016;56(4):341–5.
Wong VW, Lin A, Russell H. Adopting the new World Health Organization diagnostic criteria for gestational diabetes: how the prevalence changes in a high-risk region in Australia. Diabetes Res Clin Pract. 2017;129:148–53.
Buchanan TA, Xiang AH, Page KA. Gestational diabetes mellitus: risks and management during and after pregnancy. Nat Rev Endocrinol. 2012;8(11):639–49.
Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352(24):2477–86.
Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009;361(14):1339–48.
International Association of Diabetes Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–82.
Hapo Study Cooperative Research Group, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002.
Nankervis A, McIntyre HD, Moses RG, Ross GP, Callaway LK, Porter C, et al. ADIPS consensus guidelines for the testing and diagnosis of hyperglycaemia in pregnancy in Australia and New Zealand; 2014.
National Institute for Health and Care Excellence. Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period. Diabetes in pregnancy: Management of diabetes and its complications from preconception to the postnatal period. London: National Institute for Health and Care Excellence: Clinical Guidelines; 2015.
American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S13–28.
Diabetes Canada Clinical Practice Guidelines Expert C, Feig DS, Berger H, Donovan L, Godbout A, Kader T, et al. Diabetes and pregnancy. Can J Diabetes. 2018;42(Suppl 1):S255–S82.
Committee on Practice Bulletins-Obstetrics. ACOG practice bulletin no. 190: gestational diabetes mellitus. Obstet Gynecol. 2018;131(2):e49–64.
Long H. Diagnosing gestational diabetes: can expert opinions replace scientific evidence? Diabetologia. 2011;54(9):2211–3.
Moses RG. Gestational diabetes mellitus: implications of an increased frequency with IADPSG criteria. Diabetes Care. 2012;35(3):461–2.
Yuen L, Wong VW, Simmons D. Ethnic disparities in gestational diabetes. Curr Diab Rep. 2018;18(9):68.
Scifres C, Feghali M, Althouse AD, Caritis S, Catov J. Adverse outcomes and potential targets for intervention in gestational diabetes and obesity. Obstet Gynecol. 2015;126(2):316–25.
Huet J, Beucher G, Rod A, Morello R, Dreyfus M. Joint impact of gestational diabetes and obesity on perinatal outcomes. J Gynecol Obstet Hum Reprod. 2018;47(9):469-76.
Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of Gestational Weight Gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317(21):2207–25.
Powe CE, Allard C, Battista MC, Doyon M, Bouchard L, Ecker JL, et al. Heterogeneous contribution of insulin sensitivity and secretion defects to gestational diabetes mellitus. Diabetes Care. 2016;39(6):1052–5.
Cade TJ, Polyakov A, Brennecke SP. Implications of the introduction of new criteria for the diagnosis of gestational diabetes: a health outcome and cost of care analysis. BMJ Open. 2019;9(1):e023293.
Abell SK, Teede HJ. The IADPSG diagnostic criteria identify women with increased risk of adverse pregnancy outcomes in Victoria. Aust N Z J Obstet Gynaecol. 2017;57(5):564-8.
Koning SH, van Zanden JJ, Hoogenberg K, Lutgers HL, Klomp AW, Korteweg FJ, et al. New diagnostic criteria for gestational diabetes mellitus and their impact on the number of diagnoses and pregnancy outcomes. Diabetologia. 2018;61(4):800–9.
Behboudi-Gandevani S, Amiri M, Bidhendi Yarandi R, Ramezani TF. The impact of diagnostic criteria for gestational diabetes on its prevalence: a systematic review and meta-analysis. Diabetol Metab Syndr. 2019;11:11.
McIntyre HD, Jensen DM, Jensen RC, Kyhl HB, Jensen TK, Glintborg D, et al. Gestational diabetes mellitus: does one size fit all? A challenge to uniform worldwide diagnostic thresholds. Diabetes Care. 2018;41(7):1339-42.
Bodmer-Roy S, Morin L, Cousineau J, Rey E. Pregnancy outcomes in women with and without gestational diabetes mellitus according to the International Association of the Diabetes and Pregnancy Study Groups criteria. Obstet Gynecol. 2012;120(4):746–52.
Morrison MK, Lowe JM, Collins CE. Australian women's experiences of living with gestational diabetes. Women Birth. 2014;27(1):52–7.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Moons KG, de Groot JA, Bouwmeester W, Vergouwe Y, Mallett S, Altman DG, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med. 2014;11(10):e1001744.
Shepherd E, Gomersall JC, Tieu J, Han S, Crowther CA, Middleton P. Combined diet and exercise interventions for preventing gestational diabetes mellitus. Cochrane Database Syst Rev. 2017;11:CD010443.
Martis R, Brown J, Alsweiler J, Downie MR, Crowther CA. Treatments for women with gestational diabetes mellitus: an overview of cochrane systematic reviews. Cochrane Database Syst Rev. 2016;(8). Art. No.: CD012327.
Cochrane Prognosis Methods Group. Cochrane prognosis methods group protocol template: the Cochrane collaboration; 2018. [updated 20 November 2018. Available from: https://methods.cochrane.org/prognosis/sites/methods.cochrane.org.prognosis/files/public/uploads/protocol_template_prognosis_reviews.doc
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162(1):55–63.
Moons KM, Wolff RF, Riley RD, et al. Probast: a tool to assess risk of bias and applicability of prediction model studies: explanation and elaboration. Ann Intern Med. 2019;170(1):W1–W33.
Debray TP, Damen JA, Snell KI, Ensor J, Hooft L, Reitsma JB, et al. A guide to systematic review and meta-analysis of prediction model performance. BMJ. 2017;356:i6460.
Steyerberg EW, Moons KG, van der Windt DA, Hayden JA, Perel P, Schroter S, et al. Prognosis research strategy (PROGRESS) 3: prognostic model research. PLoS Med. 2013;10(2):e1001381.
Lamain-de Ruiter M, Kwee A, Naaktgeboren CA, Franx A, Moons KGM, Koster MPH. Prediction models for the risk of gestational diabetes: a systematic review. Diagnost Prognost Res. 2017;1(1):3.
Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925–31.
Cochrane handbook for systematic reviews of interventions: The Cochrane Collaboration; 2011. Available from: http://handbook-5-1.cochrane.org/.
Geersing GJ, Bouwmeester W, Zuithoff P, Spijker R, Leeflang M, Moons KG. Search filters for finding prognostic and diagnostic prediction studies in medline to enhance systematic reviews. PLoS One. 2012;7(2):e32844.
Ingui BJ, Rogers MA. Searching for clinical prediction rules in MEDLINE. J Am Med Inform Assoc. 2001;8(4):391–7.
Farrar D, Simmonds M, Bryant M, Sheldon TA, Tuffnell D, Golder S, et al. Treatments for gestational diabetes: a systematic review and meta-analysis. BMJ Open. 2017;7(6):e015557.
Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104(3):240–3.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–12.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ. 2015;350:h870.
GRADE Handbook. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach: the GRADE working group; 2013. Available from: https://gdt.gradepro.org/app/handbook/handbook.html
Teede HJ, Harrison CL, Teh WT, Paul E, Allan CA. Gestational diabetes: development of an early risk prediction tool to facilitate opportunities for prevention. Aust N Z J Obstet Gynaecol. 2011;51(6):499–504.
Lamain-de Ruiter M, Kwee A, Naaktgeboren CA, de Groot I, Evers IM, Groenendaal F, et al. External validation of prognostic models to predict risk of gestational diabetes mellitus in one Dutch cohort: prospective multicentre cohort study. BMJ. 2016;354:i4338.
Simmons D, Hague WM, Teede HJ, Cheung NW, Hibbert EJ, Nolan CJ, et al. Hyperglycaemia in early pregnancy: the treatment of booking gestational diabetes mellitus (TOBOGM) study. A randomised controlled trial. Med J Aust. 2018;209(9):405-6.
Hemingway H, Croft P, Perel P, Hayden JA, Abrams K, Timmis A, et al. Prognosis research strategy (PROGRESS) 1: a framework for researching clinical outcomes. BMJ. 2013;346:e5595.
Debray TP, Koffijberg H, Nieboer D, Vergouwe Y, Steyerberg EW, Moons KG. Meta-analysis and aggregation of multiple published prediction models. Stat Med. 2014;33(14):2341–62.
Poldervaart JM, Reitsma JB, Koffijberg H, Backus BE, Six AJ, Doevendans PA, et al. The impact of the HEART risk score in the early assessment of patients with acute chest pain: design of a stepped wedge, cluster randomised trial. BMC Cardiovasc Disord. 2013;13:77.
Acknowledgements
The authors thank Ms. Anne Young, Medical Librarian at Monash University, and Dr. Marie Misso, Head of Evidence Program at the Monash Centre for Health Research and Implementation for their expertise in developing the search strategy and systematic review methodology.
Funding
SDC is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship, a Diabetes Australia Research Program Top-up Scholarship and the Australian Academy of Science’s Douglas and Lola Douglas Scholarship. JAB is supported by a Career Development Fellowship funded by the NHMRC. HJT is supported by a NHMRC Fellowship funded by the Medical Research Future Fund. The funders had no role in the study design or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
SDC conceived and coordinated this project. SDC, HJT JAB and GS contributed to the development of the protocol. SDC developed the search strategies with guidance from HJT, JAB and GS. SDC and LAW screened the retrieved studies. SDC wrote the original manuscript, and all authors critically reviewed and approved the final version. SDC is the guarantor of this protocol.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Table S1. Search strategy for MEDLINE. Figure S1. Draft PRISMA Flow Diagram for the systematic review process.
Additional file 2:
PRISMA-P 2015 Checklist.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cooray, S.D., Boyle, J.A., Soldatos, G. et al. Prognostic prediction models for pregnancy complications in women with gestational diabetes: a protocol for systematic review, critical appraisal and meta-analysis. Syst Rev 8, 270 (2019). https://doi.org/10.1186/s13643-019-1151-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-019-1151-0