Background
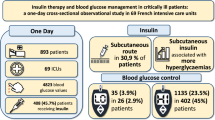
Glucose control is an important issue in post-operative patients. The objective here was to compare two insulin infusion lines by syringe pumps to assess the impact of medical devices on glycaemic variability in surgical patients under intensive insulin therapy. This open, prospective, single-centre randomised study was conducted in a fifteen-bed perioperative high dependency unit (HDU) in a university hospital. In total, 172 eligible patients receiving insulin therapy agreed to participate in the study. Subcutaneous continuous glucose monitoring was set up for all patients and an optimised system with a dedicated insulin infusion line for half of the patients.
Results
Eighty-six patients were infused via the optimised infusion line and 86 patients via the standard infusion line. No significant difference was found according to the glycaemic lability index score [mean difference between groups (95% CI): −0.09 (−0.34; 0.16), p = 0.49 after multiple imputation]. A glucose control monitoring system indicated a trend towards differences in the duration of hypoglycaemia (blood glucose level below 70 mg dl−1 (3.9 mmol l−1) over 1000 h of insulin infusion (9.7 ± 25.0 h in the standard group versus 4.4 ± 14.8 h in the optimised group, p = 0.059) and in the number of patients experiencing at least one hypoglycaemia incident (25.7 vs. 12.9%, p = 0.052). Time in the target range was similar for both groups.
Conclusions
The use of optimised infusion line with a dedicated insulin infusion line did not reduce glycaemic variability but minimised the incidence of hypoglycaemia events. The choice of the medical devices used to infuse insulin seems important for improving the safety of insulin infusion in perioperative HDU.
Similar content being viewed by others
Background
Glucose control is an important issue in post-operative patients. In 2001, special attention was paid to glycaemic variability. Although tight glycaemic control improved the outcome of critically ill patients in a surgical intensive care unit (ICU) [1], the NICE-SUGAR study demonstrated that intensive glucose control increased mortality when compared to conventional glucose control [2]. Patients require continuous intravenous insulin infusion to control glucose level, but intensive insulin therapy (IIT) is often associated with an increased risk of hypoglycaemia [3, 4]. A recent study contrasted the importance of glycaemic control in critically ill patients with the occurrence of hypoglycaemia which impacts on the mortality of diabetics in general, but especially of those at risk [5, 6].
In the above works, the issue of insulin administration methods was not addressed. Yet, many parameters can affect the drug delivery of narrow therapeutics where multiple infusions are involved, as in ICUs. The main parameter to be considered seems to be the common space volume within the infusion line between drugs simultaneously infused, as shown by Lovich et al. [7, 8]. The time to reach a steady state after initiating or ceasing drug infusion is considerably reduced with a low common volume manifold compared to a high volume design [9]. Several studies have shown the benefits of a reduction in infusion line common volume in predicting drug delivery and so avoiding incidents such as unexpected drug bolus [7,8,9,10,11,12,13,14,15,16].
In the case of insulin, rationalisation of the infusion system could eliminate the unwanted insulin bolus that causes hypoglycaemic events. This approach was studied by Maury et al. [17] in a retrospective study in a medical ICU, and thanks to an optimised insulin infusion line, they were able to limit hypoglycaemia occurrence during IIT. This work opened the way to our prospective study assessing the impact of such a system on glycaemic control and variability.
Two tubing systems of insulin infusion by syringe pumps were compared to assess the impact of medical devices on glycaemic variability in surgical patients under IIT admitted to a high dependency unit (HDU). The evolution in patients’ blood glucose levels was followed in two ways: by glucometer and by continuous glucose monitoring (CGM), the latter being more accurate as it is continuous [18].
Our main objective was to determine whether an optimised infusion line for insulin therapy had any impact on glycaemic variability and patient outcome. Secondary objectives were to study the effects of other blood glucose parameters.
Methods
Protocol
This open, prospective, single-centre randomised study was performed in a perioperative HDU at the Lille University Hospital between September 2012 and December 2013. The perioperative HDU has 15 beds and admits all surgical patients requiring organ support after vascular, endocrine and digestive surgery with an average annual admission rate of 1076 patients. The protocol was approved by the patients’ protection committee (CPP Nord-Ouest IV) and registered with the US clinical trials database (ClinicalTrials.gov ID NCT02812927) and with the French medicine agency (ID-RCB number 2012-A00188-35, ANSM). Signed informed consent was obtained from patients or next of kin before randomisation, in conformity with national regulations. The study sponsor had no role in supervising the study or interpreting data.
Patients
Inclusion criteria were: age from 18 to 80; patients undergoing elective or emergency vascular or abdominal surgery and requiring post-operative admission to the HDU; treatment with insulin on a bi-lumen central venous catheter for more than 48 h; eligibility for interstitial glucose monitoring; and blood glucose control every 3 h.
Exclusion criteria were: pregnant or breastfeeding women; patients unwilling to participate in the study or participating in another biomedical study; patients unable to understand the study and its objectives or under guardianship; patients malnourished (BMI < 18 kg m−2) or with morbid obesity (BMI > 40 kg m−2); patients in shock (septic or haemodynamic); and patients refusing to sign the Medtronic consent on the storage of personal data.
Measures
Blood glucose was measured by two methods: the first by drawing samples from the fingertip using a glucometer device (StatStrip Xpress, Nova Biomedical, Les Ulis, France) every 3 h and for the second another medical device (iPro2, Medtronic, Boulogne-Billancourt, France) was used to continuously and blindly record interstitial glucose level. Insulin therapy was adapted only from blood glucose levels read on the glucometer according to HDU protocol. CGM data were used blindly only after removing the patient’s CGM.
The primary endpoint was the glycaemic lability index (GLI), which assesses glycaemic variability [19].
The secondary endpoints were: mean blood glucose; glucose variability assessed by the standard deviation (SD) of blood glucose (BG) values and the mean amplitude glycaemic excursions (MAGE) score; hypoglycaemic incidence and events; time spent in the hypoglycaemic/hyperglycaemic target range; amount of insulin; number of interventions on the infusion line (i.e. start/stop of drug infusion and change in flow rate); and number of insulin flow rate changes.
Hypoglycaemia was defined as blood glucose level below 70 mg dl−1 (3.9 mmol l−1), hyperglycaemia as over 180 mg dl−1 (10.0 mmol l−1). The rate of hypoglycaemic or hyperglycaemic events was defined as the percentage of patients experiencing at least one episode of either detected by one of the two glucose control devices. The time spent in hypoglycaemia, hyperglycaemia or in the target range per 1000 h of insulin therapy was determined from iPro2 data. The mean and SD of BG were calculated from the data of the two glucose control devices. GLI and MAGE were calculated from the glucometer data.
Patient outcome was recorded until discharge from hospital or until the 28th day after HDU admission if the patient had not been discharged before this day.
Study design
Upon HDU admission, patients were randomly assigned in a ratio of 1:1 to be infused by the conventional insulin infusion system or by the optimised system with dedicated insulin infusion. Randomisation was carried out using sequentially numbered, sealed, opaque envelopes containing treatment group assignments obtained from computer-generated random numbers provided by an independent statistician. The patient was declared randomised when the seal was broken. The HDU pharmacist opened the envelope when the patient left the operating room and was directly hospitalised in the HDU unit. After randomisation, the HDU nurse set up the appropriate infusion line and the iPro2 device.
The protocol was implemented for at least 48 h or until the end of insulin therapy.
Regular human insulin (1 IU ml−1) was administered by continuous intravenous infusion via syringe pumps. Infusion was systematically started after surgery and adjusted according to patient blood glucose level: 1 IU h−1 between 80 (4.4) and 120 (6.7) mg dl−1 (mmol L−1), 2 IU h−1 between 121 (6.7) and 180 (10.0) mg dl−1 (mmol l−1), 3 IU h−1 between 181 (10.0) and 220 (12.2) mg dl−1 (mmol l−1), 4 IU h−1 between 221 (12.2) and 300 (16.7) mg dL−1 (mmol l−1) and 5 IU h−1 ≥ 301 (16.7) mg dl−1 (mmol l−1). Insulin infusion was stopped when blood glucose was ≤80 (4.4) mg dl−1 (mmol l−1) and 30% dextrose was given when blood glucose was ≤60 (3.3) mg dl−1 (mmol l−1).
The standard insulin infusion line consisted of a six-stopcock manifold connected to the distal port of a multilumen central venous catheter by 150 cm tubing with an internal diameter of 2.5 mm (RPB6315, Cair LGL, Lissieu, France) (Fig. 1a). The common volume between infused drugs was roughly 8.5 ml. Insulin was systematically infused via the proximal port of the manifold; carrier was infused through the manifold via a pump; all other drugs were infused through the other five stopcocks.
Schematic representation of the two infusion lines assessed. a Standard insulin infusion line using a six-stopcock manifold connected to the distal line of a multilumen central venous catheter by 150 cm tubing (RPB6315, Cair LGL, Lissieu, France). b Optimised insulin infusion line using a multilumen device (Edelvaiss Multiline-8, Doran International, Toussieu, France)
The optimised insulin infusion line was a multilumen device (Edelvaiss Multiline-8, Doran International, Toussieu, France) (Fig. 1b) [14]. This device has ports for eight infusions, which run through separate channels within a 150 cm flexible plastic tube. Fluids from the individual channels do not meet until they exit the distal tip (dead volume of 0.9 ml). Carrier was infused through the high flow (HF) line (dead volume of 2.9 ml), and insulin was infused systematically next to the HF line port. All other drugs were administered via adjacent ports on the Multiline-8. The common volume between infused drugs was reduced to that of the internal lumen alone of the central venous catheter.
Statistical analysis
The study was designed to have a statistical power of 80% with a two-sided alpha level of 0.05 to show the superiority of the optimised infusion line over the standard line in controlling glycaemic variability, assessed by GLI (primary endpoint). Sample size was calculated using the mean (±standard deviation, SD) of GLI assessed in 26 consecutive patients treated at our HDU centre with the standard insulin infusion system. In this unpublished cohort, the mean ± SD of GLI was 1070 ± 743 (mg dl−1)2/hj−1. Assuming an improvement of 30% in GLI values with the optimised infusion line (corresponding to a mean difference of 321), we estimated that 86 patients per group (a total of 172 patients) were necessary.
Analyses were performed on all patients in their original randomised group (respecting the intention-to-treat principle). Qualitative variables were expressed as frequencies and percentages. Quantitative variables were expressed as mean ± SD and medians with interquartile range. Normality of distribution was assessed graphically and using the Shapiro–Wilk test.
All analyses of GLI values (primary endpoint) were performed on log-transformed values in view of skewed distribution. Any difference between groups was calculated as a mean difference (optimised infusion line versus standard line) with a 95% confidence interval and tested using the Student t test. Missing data for the primary endpoint were treated by multiple imputations, using a regression-switching approach (chained equation with m = 20 imputations obtained with the R statistical software version 3.03). Imputation procedure was performed under the missing-at-random assumption, using all patients’ characteristics on inclusion as covariates (see Table 1) with a predictive mean matching method for continuous variables and logistic regression models (binary, ordinal or polynomial) for qualitative variables [20]. Estimates from each imputed dataset were combined using Rubin’s rules [21]. Complete case analysis was performed as a sensitivity analysis.
Between-group comparisons for secondary endpoints were made using the Chi-square test (or Fisher’s exact test when the expected cell frequency was <5) for qualitative endpoints and the Student t test (or Mann–Whitney U test in the case of non-Gaussian distribution) for quantitative endpoints. No adjustment was made for multiple comparisons.
Statistical testing was performed at the two-tailed α level of 0.05. Data were analysed using the SAS software package, release 9.3 (SAS Institute, Cary, NC).
Results
A total of 172 eligible patients accepted the protocol and agreed to participate in the study: 86 patients were treated with the optimised infusion line and 86 patients the standard infusion line (Fig. 2).
Baseline characteristics
Baseline characteristics were well balanced over the two study groups (Table 1). Before entering the HDU, patients had undergone mainly oesophageal and hepatic surgery; 78% in a context of scheduled surgery.
Glycaemic outcomes
No significant difference was found between the two groups as regards GLI score (mean difference between groups (95% CI): −0.09 (−0.34; 0.16), p = 0.49 after multiple imputation) (Table 2). The mean BG was no different with either glucometer or iPro2 (Fig. 3). No significant differences were found in the standard deviation of BG values or the MAGE score. The number of patients experiencing at least one hypoglycaemic event was no different from one group to the other. However, iPro2 indicated a trend towards a difference in the time spent in hypoglycaemia during 1000 h of insulin infusion and the number of patients experiencing at least one hypoglycaemia event. The time spent in the target range was similar for the two groups. Twenty-three hypoglycaemic events were detected by glucometer during the study. In 16 of the 23 cases (69.6%), medication (e.g. 50 mL gravity fed infusion bag in 30 min, change in total parenteral nutrition bag, syringe changeover) had been administered during the three preceding hours through the line connected to the distal line of the central venous catheter.
Other outcomes
Table 3 reveals no differences in clinical outcomes between the groups. The length of stay in the HDU and in hospital was similar. Neither was there any difference in the insulin amount infused over 48 h between the standard infusion line [70.7 ± 25.9 IU (70.0)] and the optimised infusion line [78.0 ± 29.5 IU (78.0)] (p = 0.10), nor in the number of insulin flow rate changes over 48 h [6.3 ± 2.7 (6.0) vs 7.0 ± 3.2 (7.0), p = 0.13]. Insulin flow rates were between 1 and 5 ml h−1, with a mean flow rate at 2 ml h−1. However, there was a slight difference in the number of interventions on the infusion line, the number being high for the optimised infusion line (25.5 ± 8.3 vs. 22.9 ± 7.8, p = 0.039).
Discussion
This is the first study, to our knowledge, to make a prospective comparison of two insulin infusion lines as well as of two glycaemic monitoring systems. The population consisted of high-risk patients undergoing, for the most part, oesophagectomy and extensive liver surgery. Such procedures leave a high risk of post-operative complications [22, 23], and so in our hospital, these patients are routinely treated in an HDU during the first 48 h of the post-operative period.
The first endpoint of the study concerned the lability index. There was no significant difference between the two infusion systems as regards the usual parameters to assess patients’ glycaemic variability. Glycaemic variability data can be compared to that already published. GLI values appeared to be similar to those reported by Dungan et al. in patients suffering type 2 diabetes and heart failure but inferior to Ali et al. data obtained in a population with sepsis [24]. MAGE values appeared slightly lower than those found by Hermanides et al. [25] in medical and surgical ICU patients. SD values were close to data published by Van den Berghe et al. [26] in 2006 concerning the same population.
The second endpoint of the study concerned hypoglycaemic events. A strong tendency to minimise hypoglycaemia was observed with optimised tubing. Data obtained from CGM showed an increase in the frequency of glycaemic events approaching the significance level just as in the time spent in hypoglycaemia during 1000 h of IIT. This trend was not linked with differences in patient outcomes. Reducing the incidence of potentially harmful events such as hypoglycaemia is clinically relevant. Baghshaw et al. [27] previously showed that early hypoglycaemia was associated with significantly higher ICU and hospital mortality rates, even after adjustment for available confounding factors. Moreover, blood glucose level around 7.0 mmol/l is associated with a measurable increase in the odds of survival, if hypoglycaemia is avoided [28]. In our study, CGM data analysis showed that the use of the optimised system with dedicated insulin infusion halved the number of patients experiencing at least one hypoglycaemic event. This result paves the way to a new study to assess this outcome with a greater number of patients.
This study is a follow-up to the retrospective study in a medical ICU published by Maury et al. in which authors compared two insulin infusion lines. The use of a dedicated line was linked to a significant decrease in the incidence of hypoglycaemic events. An important result of this study was confirmation of a trend towards a significant difference in the time spent in hypoglycaemia during 1000 h of IIT. The authors explained that their results were based on minimising insulin mass flow rate disturbances caused by multiple intravenous medications infused on the same infusion line as that of insulin. They showed that another drug had been administered through the insulin infusion line during the hour preceding the hypoglycaemic event in more than 8 of 10 events. In our study, more than two-thirds of hypoglycaemic events were correlated with the start of another drug administration on the infusion line in the 3 h preceding the event. This concords with our hypothesis at the beginning of this study based on in vitro works that showed the impact of common space volumes on mass flow rate disturbances when several medications are on the same infusion line [8, 11, 12].
The way to minimise the occurrence of hypoglycaemia lies in the infusion line. This is evident in the in vitro works cited above concerning the simultaneous infusion of several medications on the same infusion line [7, 11, 12]. The occurrence of hypoglycaemia is not linked with differences in morbidity and mortality between the groups.
An original aspect of this study was to use an innovative medical device, the Edelvaiss Multiline-8 which dedicates an infusion line to each drug. In this way, interactions between simultaneously infused medications are minimised. Its advantage has been demonstrated in preventing drug incompatibilities [13, 14] as well as mass flow rate disturbances both in vitro and on animals [7, 8, 14]. Our work supports its use in an HDU context and suggests a link between minimising interactions of simultaneous infused drugs and time spent in hypoglycaemia.
The difference between Maury’s study and ours cannot be accounted for by more intensive insulin treatment. It seems to be due to different recruitment, with ICU patients presenting gravity scores higher than our HDU population. High blood glucose seems to be correlated with a high APACHE II score and a more serious degree of disease such as a higher incidence of respiratory infection [29]. Glycaemic variability and hypoglycaemia therefore differ from ICU to HDU patients as the risk of severe hyperglycaemic stress response is higher in patients with organ failure than in those without [30]. Knowing that insulin bolus increases glycaemic variability and hypoglycaemia, the risk will be lesser in HDU patients [31]. Lower hyperglycaemic stress and less risk of bolus induced by other intravenous agents could explain the discrepancy with our results.
The other original aspect is the use of two methods to monitor patients’ glycaemic status. Control of the interstitial glucose level seems to increase sensitivity for detecting hypoglycaemic events as the real time spent in and out of the range of targeted glycaemic values can be calculated more precisely.
Better insulin dose adjustment is therefore possible, which would impact the time spent on therapeutic targets and patient survival [32]. Tight glycaemic control of critically ill patients has no effect on mortality but causes five times as much hypoglycaemia compared to mild or very mild control [33, 34]. Ways have to be found to limit hypoglycaemia occurrence, such as minimising infusion volume and monitoring glucose levels.
It can therefore be noted that the optimised infusion line is responsible for fewer hypoglycaemic events. The choice of the medical devices used to infuse insulin seems important for improving the safety of insulin infusion in a perioperative HDU. It could be worthwhile to develop a new clinical protocol integrating hypoglycaemic events as the primary endpoint and to compare patients’ outcome according to insulin infusion modalities.
Abbreviations
- ASA:
-
physical status score defined by the American Society of Anesthesiologists
- BG:
-
blood glucose
- BMI:
-
body mass index
- CGM:
-
controlled glucose monitoring
- CRFs:
-
cardiovascular risk factors
- GLI:
-
glycaemic lability index
- HDU:
-
high dependency unit
- ICU:
-
intensive care unit
- IIT:
-
intensive insulin therapy
- ITT:
-
intended-to-treat
- IU:
-
international unit
- MAGE:
-
mean amplitude glycaemic excursions
- SAPS II:
-
simplified acute physiological score
- SD:
-
standard deviation
- SOFA:
-
sequential organ failure assessment
References
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–67.
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY-S, Blair D, Foster D, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97.
Preiser J-C, Devos P, Ruiz-Santana S, Mélot C, Annane D, Groeneveld J, et al. A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009;35:1738–48.
Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132:268–78.
Egi M, Bellomo R, Stachowski E, French CJ, Hart GK, Taori G, et al. Hypoglycemia and outcome in critically ill patients. Mayo Clin Proc. 2010;85:217–24.
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Lovich MA, Doles J, Peterfreund RA. The impact of carrier flow rate and infusion set dead-volume on the dynamics of intravenous drug delivery. Anesth Analg. 2005;100:1048–55.
Lovich MA, Pezone MJ, Maslov MY, Murray MR, Wakim MG, Peterfreund RA. Infusion system carrier flow perturbations and dead-volume: large effects on drug delivery in vitro and hemodynamic responses in a swine model. Anesth Analg. 2015;120:1255–63.
Lovich MA, Wakim MG, Wei A, Parker MJ, Maslov MY, Pezone MJ, et al. Drug infusion system manifold dead-volume impacts the delivery response time to changes in infused medication doses in vitro and also in vivo in anesthetized swine. Anesth Analg. 2013;117:1313–8.
Pezone MJ, Peterfreund RA, Maslov MY, Govindaswamy RR, Lovich MA. Infusion system architecture impacts the ability of intensive care nurses to maintain hemodynamic stability in a living swine simulator. Anesthesiology. 2016;124:1077–85.
Lannoy D, Decaudin B, Simon N, Barthelemy C, Debaene B, Odou P. The impact on drug mass flow rate of interrupting and resuming carrier fluid flow. Anesth Analg. 2012;114:328–32.
Décaudin B, Dewulf S, Lannoy D, Simon N, Secq A, Barthélémy C, et al. Impact of multiaccess Infusion devices on in vitro drug delivery during multi-infusion therapy. Anesth Analg. 2009;109:1147–55.
Perez M, Décaudin B, Abou Chahla W, Nelken B, Barthélémy C, Lebuffe G, et al. In vitro analysis of overall particulate contamination exposure during multidrug IV therapy: impact of infusion sets. Pediatr Blood Cancer. 2015;62:1042–7.
Foinard A, Décaudin B, Barthélémy C, Debaene B, Odou P. The impact of multilumen infusion devices on the occurrence of known physical drug incompatibility: a controlled in vitro study. Anesth Analg. 2013;116:101–6.
Genay S, Décaudin B, Scoccia S, Barthélémy C, Debaene B, Lebuffe G, et al. An in vitro evaluation of infusion methods using a syringe pump to improve noradrenaline administration. Acta Anaesthesiol Scand. 2015;59:197–204.
Genay S, Décaudin B, Ethgen S, Barthélémy C, Odou P, Lebuffe G. Impact of noradrenaline infusion set on mean arterial pressure: a retrospective clinical study. Ann Fr Anesthèsie Rèanimation. 2013;32:e159–62.
Maury E, Vitry P, Galbois A, Ait-Oufella H, Baudel J-L, Guidet B, et al. Continuous insulin administration via complex central venous catheter infusion tubing is another risk factor for blood glucose imbalance. A retrospective study. Ann Intensive Care. 2012;2:16.
Preiser J-C, Chase JG, Hovorka R, Joseph JI, Krinsley JS, De Block C, et al. Glucose control in the ICU: a continuing story. J Diabetes Sci Technol. 2016;10:1372–81.
Ali NA, O’Brien JM, Blum W, Byrd JC, Klisovic RB, Marcucci G, et al. Hyperglycemia in patients with acute myeloid leukemia is associated with increased hospital mortality. Cancer. 2007;110:96–102.
Van Buuren S, Groothuis-Oudshoorn K. MICE: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987.
Gemmill EH, Humes DJ, Catton JA. Systematic review of enhanced recovery after gastro-oesophageal cancer surgery. Ann R Coll Surg Engl. 2015;97:173–9.
Yin Z, Huang X, Ma T, Jin H, Lin Y, Yu M, et al. Postoperative complications affect long-term survival outcomes following hepatic resection for colorectal liver metastasis. World J Surg. 2015;39:1818–27.
Ali NA, O’Brien JM, Dungan K, Phillips G, Marsh CB, Lemeshow S, et al. Glucose variability and mortality in patients with sepsis. Crit Care Med. 2008;36:2316–21.
Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, DeVries JH. Glucose variability is associated with intensive care unit mortality*. Crit Care Med. 2010;38:838–42.
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61.
Bagshaw SM, Bellomo R, Jacka MJ, Egi M, Hart GK, George C, et al. The impact of early hypoglycemia and blood glucose variability on outcome in critical illness. Crit Care Lond Engl. 2009;13:R91.
Penning S, Pretty C, Preiser J-C, Shaw GM, Desaive T, Chase JG. Glucose control positively influences patient outcome: A retrospective study. J Crit Care. 2015;30:455–9.
Kang L, Han J, Yang Q-C, Huang H-L, Hao N. Effects of different blood glucose levels on critically Ill patients in an intensive care unit. J Mol Microbiol Biotechnol. 2015;25:388–93.
Clain J, Ramar K, Surani SR. Glucose control in critical care. World J Diabetes. 2015;6:1082–91.
Gunst J, Van den Berghe G. Blood glucose control in the ICU: don’t throw out the baby with the bathwater! Intensive Care Med. 2016;42:1478–81.
Krinsley JS, Preiser J-C. Time in blood glucose range 70 to 140 mg/dl > 80% is strongly associated with increased survival in non-diabetic critically ill adults. Crit Care Lond Engl. 2015;19:179.
Yamada T, Shojima N, Noma H, Yamauchi T, Kadowaki T. Glycemic control, mortality, and hypoglycemia in critically ill patients: a systematic review and network meta-analysis of randomized controlled trials. Intensive Care Med. 2016;43:1–15.
Yatabe T, Inoue S, Sakaguchi M, Egi M. The optimal target for acute glycemic control in critically ill patients: a network meta-analysis. Intensive Care Med. 2016;43:16–28.
Authors’ contributions
SG, BD, GL conceived and designed the study. SG, SE, AA, EB collected the data. SG, BD analysed the data. SG wrote the first draft of the paper. SG, BD wrote the final draft of the paper. JL, HB performed statistical analysis. MCV, PO, GL revised the manuscript. All authors gave final approval for manuscript publication and agree to be accountable for all aspects of this work. All authors read and approved the final manuscript.
Acknowledgements
We thank Doran International for providing Edelvaiss Multiline-8 for the study. English language editing assistance was provided by Alexandra Tavernier.
Competing interests
The study was supported by intramural funds. Doran International provided Edelvaiss Multiline-8 medical devices for the study. S.Genay, B.Décaudin, and P.Odou report receiving travel expense reimbursements from Doran International.
Availability of data and materials
The dataset supporting the conclusions of this article is available by contacting the corresponding author.
Ethics approval and consent to participate
The protocol was approved by the patients’ protection committee (CPP Nord-Ouest IV) and registered with the US clinical trials database (ClinicalTrials.gov ID NCT02812927) and with the French medicine agency (ID-RCB number 2012-A00188-35, ANSM). Signed informed consent was obtained from patients or next of kin, in conformity with national regulations before randomisation.
Funding
The study was supported by intramural funds. Medical devices were provided Edelvaiss Multiline-8 for the study by Doran International.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Genay, S., Décaudin, B., Ethgen, S. et al. Effect of insulin infusion line on glycaemic variability in a perioperative high dependency unit (HDU): a prospective randomised controlled trial. Ann. Intensive Care 7, 74 (2017). https://doi.org/10.1186/s13613-017-0298-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-017-0298-x