Abstract
Background
Globally, cervical cancer is the fourth most common cancer in women. Here, we report a case of cutaneous lymphangitis carcinomatosa arising from cervical cancer, an extremely rare and treatment-resistant condition.
Case presentation
A 64-year-old Japanese woman presented with genital bleeding. She was diagnosed as having stage IB1 squamous cell cervical cancer and subsequently treated with radiotherapy. Approximately 2 years after the curative radiotherapy, she developed itching, skin rash, and small nodules on her left femoral and pubic area. Slight 18F-fluorodeoxyglucose uptake was detected at her left femoral skin on positron emission tomography with computed tomography. A histopathological examination was performed on a biopsy sample from an erythematous macule on her left femoral skin and vulva. Consequently, she was diagnosed as having cutaneous lymphangitis carcinomatosa arising from cervical cancer. Paclitaxel (135 mg/m2), cisplatin (50 mg/m2), and bevacizumab (15 mg/kg) combination therapy was administered every 21 days. Both itching and rash improved after three treatment cycles. After the completion of six cycles, skin erythema in the femoral and vulval area disappeared completely. Our patient experienced a 25-month symptom-free interval after the last chemotherapy session.
Conclusion
Our findings suggest that combination chemotherapy plus bevacizumab is an effective therapeutic option in patients with cutaneous lymphangitis carcinomatosa arising from cervical cancer.
Similar content being viewed by others
Introduction
Cervical cancer is the fourth most common cancer in women worldwide [1], resulting in approximately 275,000 deaths per year [2]. The incidence and mortality rates of cervical cancer in Japan were 16.1 and 4.4 per 100,000 people, respectively. The recurrence rate of cervical cancer was 8–26%, and overall survival after recurrence ranged from 7 to 12 months [2].
The common sites of recurrence are local, lung, liver, bone, and lymph node metastasis [3]. In contrast, cutaneous metastasis, especially cutaneous lymphangitis carcinomatosa arising from cervical cancer, is extremely rare. It is caused by occlusion of the lymphatic channels of the dermis by cancer cells [4]. Skin metastasis, including cutaneous metastasis due to lymphangitis carcinomatosa, is associated with a poor prognosis. The average survival period after the appearance of skin metastasis is as short as 3 to 8.5 months [5,6,7,8].
The treatment for recurrent cervical cancer depends on the site of recurrence (local or distant recurrence). Systemic chemotherapy is chosen for the treatment of distant recurrence or local recurrence within the irradiation field. In addition, bevacizumab (BV) has been approved for targeted therapy in patients with recurrent or advanced cervical cancer on the basis of the results of the Gynecologic Oncology Group (GOG) 240 trial [9]. BV is a recombinant humanized monoclonal antibody that inhibits vascular endothelial growth factor (VEGF)-A [10]. VEGF-C, a subfamily within the VEGF family, is expressed in human cancers. VEGF-C promotes tumor angiogenesis and lymphangiogenesis in vivo, and drives tumor growth and metastasis [11, 12]. BV has potential antitumor effects against metastatic lesions in the lymph system.
Here, we report a case of cutaneous lymphangitis carcinomatosa arising from cervical cancer that was successfully treated with paclitaxel-cisplatin and BV (TP + BV) combination therapy. We believe that TP + BV therapy can be effective against lymphangitis carcinomatosa arising from cervical cancer.
Case presentation
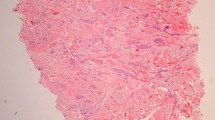
Our patient was a 64-year-old Japanese woman, gravida 2, para 2 (spontaneous deliveries), who presented with genital bleeding. She had asthma but had not received any medication for it. She had no previous history of obstetrics and gynecological issues. She had obtained a diploma in cooking and was a chef. She was from a family of three, and her economic situation was like that of most Japanese people. She was a tobacco smoker. Her family medical history was unremarkable. She was diagnosed as having cervical cancer, International Federation of Gynecology and Obstetrics (FIGO) clinical stage IB1. A histopathological examination was performed on a cervical biopsy sample, resulting in a diagnosis of squamous cell carcinoma. We explained that both surgery and radiation therapy are radical treatments; hence, she received radiation therapy with external irradiation (48 Gy × 24 times) and remote afterloading system (24 Gy × 4 times). Approximately 2 years after curative radiation therapy, she complained of itching, skin rash, and small papules and nodules on her left femoral and vulval skin (Fig. 1); these were edema and dermatitis flare-ups. A biopsy of an erythematous macule on her left femoral and vulval skin was performed. There were a few lymphocytes around the vessels, and a subsequent histopathological examination revealed cytokeratin-positive atypical cells invading the dermis; these were within the thin-walled vessels and expressed D2-40, a marker of lymphatic endothelium [13] (Fig. 2). The atypical cells were similar to the cells in squamous cell carcinoma. Positron emission tomography with computed tomography (PET-CT) revealed slight uptake of 18F-fluorodeoxyglucose (18F-FDG) in her left femoral skin with maximum standardized uptake value (SUVmax) of 1.41 (Fig. 3). Apart from that, she had no other lesion with abnormal 18F-FDG uptake on PET-CT. She was subsequently diagnosed as having cutaneous lymphangitis carcinomatosa arising from cervical cancer. At the time of diagnosis, her muscle, circulatory, and respiratory functions were normal. She had normal blood pressure (129/69 mmHg), heart rate (71 beats per minute), and body temperature (36.9 °C) and did not have anemia (hemoglobin, 13.8 g/dL). Her liver and renal function were normal (total bilirubin, 0.5 mg/dL; aspartate aminotransferase, 19 U/L; alanine aminotransferase, 15 U/L; blood urea nitrogen, 13 mg/dL; and creatinine, 0.52 mg/dL), and her electrolyte levels were normal (sodium, 143 mEq/ml; potassium, 3.9 mEq/ml; and chloride, 109 mEq/ml). Moreover, her urine analysis results were normal (proteinuria, urinary glucose, and ketone were not detected). Paclitaxel (135 mg/m2, for 24 hours)-cisplatin (50 mg/m2, for 2 hours) and BV (15 mg/kg, for 1.5 hours) combination therapy was administered every 21 days. An improvement of both itching and rash was noted after three cycles. After a total of six cycles were administered, the femoral and vulval skin erythema completely disappeared (Fig. 4). Our patient experienced a symptom-free interval of 25 months after the last TP + BV infusion.
Discussion
To the best of our knowledge, this is the first case report on TP + BV therapy for skin metastasis from cervical cancer. Skin metastasis occurs in 0.7–9% of all patients with cancer [14]. Skin metastases have the following distribution in women with primary malignancies: breast (69%), large intestine (9%), melanoma (5%), lung (4%), ovary (4%), sarcoma (2%), pancreas (2%), and uterine cervix (2%) [14]. The most common sites of skin metastases in patients with cervical cancer are the abdominal wall, vulva, anterior chest wall, and lower extremities [14]. Although skin metastasis mainly presents as nodules or masses, these lesions may sometimes appear as nodules or inflammatory disease [5, 14]. The morphologic patterns are nodules, plaques, and inflammatory telangiectatic lesions [6]. It is difficult to distinguish lymphangitis carcinomatosa from dermatitis. If the lesion is refractory dermatitis, a skin biopsy should be performed.
Currently, no effective treatment has been established for cutaneous metastasis due to lymphangitis carcinomatosa of cervical cancer [15, 16]. For recurrent cervical cancer, chemotherapy is one of the options available in Japan [17]. The results of the GOG 240 trial [9] suggested that TP + BV combination therapy can improve the prognosis of recurrent cervical cancer. Furthermore, in another study, the addition of BV to combination chemotherapy in patients with recurrent cervical cancer was associated with an improvement of 3.7 months in median overall survival [18]. There have been several reports describing the use of various regimens, including cisplatin-based chemotherapy and radiotherapy, in patients with recurrent skin metastasis from cervical cancer; however, most of these patients experienced progression of disease after chemotherapy (Table 1) [16, 19,20,21,22,23,24,25]. In this review, all skin metastases arose from squamous cell carcinomas. Only two cases advanced to stage III–IV, and eight cases were in stage I–II. Skin metastasis could arise from stage I–II cervical carcinoma. Skin metastasis from cervical cancer is possible even in the early stage. In addition to the present report, only one other case of complete response to chemotherapy has been reported, wherein the patient was treated with radiotherapy followed by chemotherapy [25]. Although palliative chemotherapy with paclitaxel resulted in complete clinical resolution in one previous case [23], to the best of our knowledge, this is the first report of complete response in a patient with skin metastasis of cervical cancer treated with combination chemotherapy plus BV.
In a mouse model of suture-induced corneal neovascularization, BV decreased cell proliferation of corneal lymphatic vessel cells through an anti-angiogenic effect [26]. Although the evidence supporting the anti-lymphangiogenic effects of BV in cancer is limited [27], BV has an antitumor effect in patients with breast cancer with lymph node metastasis [28]. Regarding lymphangitis carcinomatosa arising from other cancers, long survival has been reported in two cases treated with chemotherapy in combination with BV [29, 30]: paclitaxel and carboplatin (TC) in one patient with lung cancer and 5-fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) in a patient with colorectal cancer. Thus, BV may be more effective in metastases through lymph vessels, including lymphangitis carcinomatosa.
Conclusion
In general, lymphangitis carcinomatosa is resistant to various therapies and has a poor prognosis. In the current case, TP + BV combination therapy was extremely effective against lymphangitis carcinomatosa. Our findings indicate that a chemotherapy regimen that includes bevacizumab should be considered an effective therapeutic option in patients with cutaneous lymphangitis carcinomatosa arising from cervical cancer.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Rosen VM, Guerra I, McCormack M, Nogueira-Rodrigues A, Sasse A, Munk VC, Shang A. Systematic review and network meta-analysis of bevacizumab plus first-line topotecan-paclitaxel or cisplatin-paclitaxel versus non-bevacizumab-containing therapies in persistent, recurrent, or metastatic cervical cancer. Int J Gynecol Cancer. 2017;27:1237–46.
Elit L, Fyles AW, Devries MC, Oliver TK, Fung-Kee-Fung M, Gynecology Cancer Disease Site Group. Follow-up for women after treatment for cervical cancer: a systematic review. Gynecol Oncol. 2009;114:528–35. https://doi.org/10.1016/ygyno.2009.
Cartson V, Delclos L, Fletcher GH. Distant metastases in squamous-cell carcinoma of the uterine cervix. Radiology. 1967;88:961–6. https://doi.org/10.1148/88.5.961.
Nashan D, Muller ML, Braun-Falco M, Reichenberger S, Szeimies RM, Bruckner-Tuderman L. Cutaneous metastases of visceral tumours: a review. J Cancer Res Clin Oncol. 2009;135:1–14.
Malfetano JH. Skin metastasis from cervical carcinoma a fatal event. Gynecol Oncol. 1986;24:177–82.
Imachi M, Tsukamoto N, Kinoshita S, Nakano H. Skin metastasis from carcinoma of the uterine cervix. Gynecol Oncol. 1993;48:349–54.
Yang HI, Lee MC, Kuo TT, Hong HS. Cellulitis-like cutaneous metastasis of uterine cervical carcinoma. J Am Acad Dermatol. 2007;56:S26–8.
Pertzborn S, Buekers TE, Sood AK. Hematogenous skin metastases from cervical cancer at primary presentation. Gynecol Oncol. 2000;76:416–7.
Penson RT, Huang HQ, Wenzel LB, Monk BJ, Stockman S, Long HJ 3rd, et al. Bevacizumab for advanced cervical cancer: patient-reported outcomes of a randomised, phase 3 trial (NRG Oncology-Gynecologic Oncology Group protocol 240). Lancet Oncol. 2015;16:301–11. https://doi.org/10.1016/S1470-2045(15)70004-5.
Shin T, Lindley C. Bevacizumab: an angiogenesis inhibitor for the treatment of solid malignancies. Clin Ther. 2006;28:1779–802. https://doi.org/10.1016/j.clinthera.2006.11.015.
Skobe M, Hawighorst T, Jackson DG, Prevo R, Janes L, Velasco P, Riccardi L, Alitalo K, Claffey K, Detmar M. Induction of tumor lymphangiogenesis by VEGF-C promotes breast cancer metastasis. Nat Med. 2001;7:192–8. https://doi.org/10.1038/84643.
Mandriota SJ, Jussila L, Jeltsch M, Compagni A, Baetens D, Prevo R, Banerji S, Huarte J, Montesano R, Jackson DG, et al. Vascular endothelial growth factor-C-mediated lymphangiogenesis promotes tumor metastasis. EMBO J. 2001;20:672–82. https://doi.org/10.1093/emboj/20.4.672.
Fukunaga M. Expression of D2-40 in lymphatic endothelium of normal tissues and in vascular tumours. Histopathology. 2005;46:396–402.
Schwartz RA. Cutaneous metastatic disease. J Am Acad Dermatol. 1995;33:161–84.
Agrawal A, Yau A, Magliocco A, Chu P. Cutaneous metastatic disease in cervical cancer: a case report. J Obstet Gynaecol Can. 2010;32:467–72.
Behtash N, Mehrdad N, Shamshirsaz A, Hashemi R, Amouzegar Hashemi F. Umblical metastasis in cervical cancer. Arch Gynecol Obstet. 2008;278:489–91.
Ebina Y, Yaegashi N, Katabuchi H, Nagase S, Udagawa Y, Hachisuga T, et al. Japan Society of Gynecologic Oncology guidelines 2011 for the treatment of uterine cervical cancer. Int J Clin Oncol. 2015;20:240–8. https://doi.org/10.1007/s10147-015-0806-7.
Tewari KS, Sill MW, Long HJ 3rd, Penson RT, Huang H, Ramondetta LM, Landrum LM, Oaknin A, Reid TJ, Leitao MM, et al. Improved survival with bevacizumab in advanced cervical cancer. N Engl J Med. 2014;370:734–43.
Özcan HÇ, Mustafa A, Bozdağ Z, Sucu S, Uğur MG, Balat Ö. Early vulvar and umbilical incisional scar recurrence of cervical squamous cell carcinoma: earlier than usually expected. Turk J Obstet Gynecol. 2017;14:141–4. https://doi.org/10.4274/tjod.40225.
Benoulaid M, Elkacemi H, Bourhafour I, Khalil J, Elmajjaoui S, Khannoussi B, et al. Skin metastases of cervical cancer: two case reports and review of the literature. J Med Case Rep. 2016;10:265. https://doi.org/10.1186/s13256-016-1042-0.
Basu B, Mukherjee S. Cutaneous metastasis in cancer of the uterine cervix: a case report and review of the literature. J Turk Ger Gynecol Assoc. 2013;14:174–7. https://doi.org/10.5152/jtgga.2013.62444. eCollection 2013
Behtash N, Ghaemmaghami F, Yarandi E, Ardalan FA, Khanafshar N. Cutaneous metastasis from carcinoma of the cervix at the drain site. Gynecol Oncol. 2002;85:209–11. https://doi.org/10.1006/gyno.2001.6559.
Palaia I, Angioli R, Cutillo G, Manci N, Panici PB. Skin relapse from cervical cancer. Gynecol Oncol. 2002;87:155–6.
Kagen MH, Ruhl KK, Aghajanian C, Myskowski PI. Squamous cell carcinoma of the cervix metastatic to the skin. J Am Acad Drmatol. 2001;45:133–5. https://doi.org/10.1067/mid2001.1123489.
Freeman CR, Rozenfeld M, Schopflocher P. Cutaneous metastases from carcinoma of the cervix. Arch Dermatol. 1982;118:40–1.
Tan JC, Mann S, Coronea MT. Successful treatment of conjunctival lymphangiectasia with subconjunctival injection of bevacizumab. Cornea. 2016;35:1375–7. https://doi.org/10.1097/ICO.0000000000000899.
Stacker SA, Achen MG. The VEGF signaling pathway in cancer: the road ahead. Chin J Cancer. 2013;32:297–302. https://doi.org/10.5732/cjc.012.10319.
Min Kim H, Hasegawa J, Hirota M, Matsunami N, Mikata S, Shimizu J, et al. A case of sigmoid colon cancer with Virchow's lymph node metastasis successfully treated with chemotherapy. Gan To Kagaku Ryoho. 2012;39:2249–51.
Sogabe S, Yuki S, Takagi T, Miyazaki T, Takano H, Kuwamoto Y, et al. A case of sigmoid colon cancer with lymphangitis carcinomatosa successfully treated with chemotherapies including molecular targeting drugs. Gan To Kagaku Ryoho. 2010;37:535–8.
Suzuki E, Tanahashi M, Yukiue H, Yohii N, Shitara M, Fujino T, Niwa H. A patient with lung adenocarcinoma, lymphangitis carcinomatosa, and multiple bone metastases who achieved long-term survival after successful treatment with carboplatin, paclitaxel, and bevacizumab. Gan To Kagaku Ryoho. 2016;43:617–20.
Acknowledgements
None.
Funding
No funding available.
Author information
Authors and Affiliations
Contributions
All authors analyzed the patient data regarding the disease and conducted patient care. FN collected patient data, described it in the case report with literature review. FN, MS, and SN performed literature review and made significant contributions to the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Author, S Nagase, received lecture fees from Chugai Pharmaceutical Co., Ltd. and AstraZeneca. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nakamura, F., Seino, M., Suzuki, Y. et al. Successful management of cutaneous lymphangitis carcinomatosa arising from cervical cancer with paclitaxel-cisplatin and bevacizumab combination therapy: a case report and review of the literature. J Med Case Reports 13, 328 (2019). https://doi.org/10.1186/s13256-019-2262-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-019-2262-x