Abstract
Background
Reactivation of adult hemoglobin (HbF) is currently a dominant therapeutic approach to sickle cell disease (SCD). In this study, we have investigated among SCD patients from Cameroon, the association of HbF level and variants in the HU-inducible small guanosine triphosphate-binding protein, secretion-associated and RAS-related (SAR1a) protein, previously shown to be associated with HbF after HU treatment in African American SCD patients.
Results
Only patients >5 years old were included; hemoglobin electrophoresis and a full blood count were conducted upon arrival at the hospital. RFLP-PCR was used to describe the HBB gene haplotypes and Gap PCR to investigate the 3.7 kb α-globin gene deletion. The iPLEX Gold Sequenom Mass Genotyping Array and cycle sequencing were used for the genotyping of four selected SNPs in SAR1a (rs2310991; rs4282891; rs76901216 and rs76901220). Genetic analysis was performed using an additive genetic model, under a generalized linear regression framework. 484 patients were studied. No associations were observed between any of the promoter variants and baseline HbF, clinical events or other hematological indices.
Conclusion
The results of this study could be explained by possible population-specificity of some tagging genomic variants associated with HbF production and illustrated the complexity of replicating HbF-promoting variants association results across African populations.
Similar content being viewed by others
Background
Reactivation of adult fetal hemoglobin (HbF) is currently the dominant approach for the treatment of sickle cell disease (SCD). The expression of adult HbF is a quantitative trait that is subject to several predisposing loci affecting the persistence of HbF in adulthood, particularly three principal loci; BCL11A, HBS1L-MYB intergenic variants and the five sequence polymorphisms along the β-globin gene cluster that confer the SCD haplotype [1,2,3]. Taken in sum, these loci have been associated with the disease-ameliorating HbF and account for 10–20% of the variance [4,5,6,7]. Furthermore, the BCL11A erythroid-specific enhancer variants have been shown to account for significant variance in HbF in African American [8, 9], Tanzanian [10] and Cameroonian SCD patient cohorts [11].
HbF response to hydroxyurea (HU), has been shown to be subject to a myriad of genetic variations (SNPs, signalling pathways and pharmacogenomics interactions) and environmental factors (socio-economic factors, quality of care, exposure to malaria and infections) [12]. Furthermore, some of these variants have been associated with favourable pharmacologic response to HU treatment like the small guanosine triphosphate (GTP)-binding protein, secretion-associated and RAS-related (SAR) protein [13]. SAR proteins have been shown to be critical to γ-globin expression [14] via the Giα/JNK/Jun pathway [15] in response to HU. Four variants (rs2310991; rs4282891; rs76901216 and rs76901220) in the SAR1a promoter were associated with significant increases in HbF levels in African American SCD patients on HU for 2 years [13]. Much like variants in BCL11A, MYB and KLF-1 have been shown to be associated to Hb F levels in both HU-exposed and HU-naïve conditions [6, 12], in the present study, we have investigated the relationship between the four SAR1a promoter variants and baseline HbF in SCD patients from Cameroon, without any HU treatment.
Research hypothesis
In this study, we hypothesize that selected variants in SAR1a promoter associated with significant increases in HbF levels in African American SCD patients on HU, are also associated with baseline HbF in SCD patients from Cameroon, without any HU treatment.
Methods
Study population and HbF measurement
Patients’ recruitment occurred at the Yaoundé Central Hospital and Laquintinie Hospital in Douala, Cameroon. Only clinically stable patients, 5 years and older, with no history of blood transfusion, HU treatment, or hospitalisation in the preceding 6 weeks were included and clinical events were prospectively collected (Table 1). Whole blood counts of patients and Hb electrophoresis were conducted on arrival at the hospital, initially using the alkali denaturation test (ADT) in 55.5% (n = 266) of the cohort, and when it became available, high performance liquid chromatography (HPLC). In a previous study of this cohort, the SCD patient cohort was disaggregated based on the technique used for HbF assessment (HPLC vs ADT) and found similar but independently examined associations between HbF levels and BCL11A and HBS1L-MYB intergenic variants [5].
Genotyping
HbS mutation and HBB haplotypes
DNA was extracted from peripheral blood following the manufacturer’s instructions (Puregene Blood Kit, Qiagen®, USA). Molecular analysis to determine the presence of the sickle mutation was carried out on 200 ng DNA by PCR to amplify a 770 bp segment of the β-globin gene, followed by DdeI restriction analysis of the PCR product [16].
Using published primers and methods, five restriction fragment length polymorphism (RFLP) sites in the β-globin gene cluster were amplified [17] to analyse the XmnI (5′Gγ), HindIII (Gγ), HindIII (Aγ), HincII (3˙’Ψβ) and HinfI (5′β) for the HBB haplotype background [18].
Detection of 3.7 kb α-globin gene deletions
Using the expand-long template PCR (Roche®, UK), the 3.7 kb α-globin gene deletion was successfully screened following the instructions reported [19] with some modifications previously published [20].
SNPs
A total of 484 samples were analysed initially using SNaPshot sequencing and capillary electrophoresis (n = 234), then the rest analysed using the iPLEX Gold Sequenom Mass Genotyping Array (Inqaba Biotec, South Africa). The results were validated by direct cycle sequencing of a subset (n = 48; 10%) of the samples using previously reported methods [5].
Data analysis
Descriptive statistics were obtained for all quantitative data using SPSS (IBM, USA version 21.0). A Chi squared test, with 1 degree of freedom, was used to perform the Hardy–Weinberg Equilibrium (HWE) test on the SNPs genotype with three SNPs (rs4282891; rs2310991 and rs76901216) out of HWE (p < 0.05). Using an additive genetic model, under a generalized linear regression framework, we investigated the relationship between the SNPs and HbF levels, using the R statistical package version 3.0.3 (The R Foundation for statistical computing, Vienna, Austria). Significance was set at 5%.
Results
Patient cohort
Table 1 summarises the main characteristics of the cohort. All patients had confirmed SCA diagnosis (HbSS) among whom 50.2% (n = 243) were female and the mean age of the cohort was 17.9 years (±10.6). After genotyping β-globin gene haplotypes for 968 chromosomes, the most prevalent were Benin (72.5%, n = 702) and Cameroon (19.2%, n = 186). Haplotypes given in combinations, the Benin/Benin haplotype was 50.2% (n = 243) and the Benin/Cameroon haplotype 21.7% (n = 105) of the patient cohort (Table 1). The frequency of the 3.7 kb α-globin gene deletion (α3.7) was 22.5% (n = 222) of 968 chromosomes, where 28.5 and 8.6% of patients had co-inherited a single (αα/α3.7) and double (α3.7/α3.7) deletions, respectively (Table 1). The average number of annual reported vaso-occlusive crises was 2.8 (±3.3) with a similar yearly rate of hospital consultation (3.0 ± 3.9) and mean 1.4 (±2.5) hospitalization per year. Overt stroke was reported in 4.5% (n = 22) of the patients.
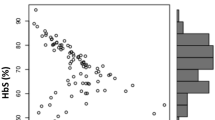
No association between SNPs and HbF
The minor allele frequency (MAF) of the SAR1a promoter SNPs is shown in Table 2. There was no association between the four selected promoter SNPs and HbF levels in the patient cohort neither was there an association with clinical events or hematological indices. The influence of the electrophoretic technique, α-globin genotypes and β-globin haplotypes on the relationship between the SNPs and HbF levels was tested and no significant effect was observed.
Discussion
Four variants (rs2310991; rs4282891; rs76901220 and rs76901216) have previously been associated with higher percent HbF and significant change in HbF levels after HU treatment for 2 years in African American SCA patients enrolled in the National Institutes of Health (NIH)’s Sickle Cell Pulmonary Hypertension Screening Study (ClinicalTrials.org; NCT00011648). It has been reported that SAR1 is induced by HU towards the production of HbF in erythroid cells [14, 15] via activation of the Giα/JNK/Jun pathway. This and other critical signalling pathways in HU-induced HbF as well as genomic variants associated with HbS mutation and the disease course have been reviewed [12]. Given the responsiveness of SAR1 to HU treatment and prior associations with HU-induced HbF, four promoter polymorphisms were investigated in a cohort of SCA patients not treated with HU to determine possible associations between the SNPs and baseline HbF. If these variants result in differential expression of SAR1 and thus HbF, this loci could become a candidate for therapeutic manipulation for ameliorating SCA and other hemoglobinopathies. However, none of the selected SNPs were associated with HbF, other hematological indices or clinical events. Furthermore, the difference between the minor allele frequencies (MAF) in African American SCA patients [13] and results from the present study may be attributed to the well reported high diversity among African population [21, 22] and more specifically to admixture among African Americans, with African ancestry that could vary from 1 to 99% [23, 24]. Replication of association studies across different populations, particularly of varied genetic backgrounds and environmental settings, is imperative to understanding the complex processes of HbF production and genetic polymorphisms predisposing to persistence of adult HbF, more so in sub-Saharan Africa where the burden of disease is highest.
SAR1a is a known regulator of HbF expression under HU therapy [13, 14], previously demonstrated in bone marrow CD34+ and K562 cells [15]. This erythroid binding protein primarily acts through the p-JNK/Jun and GATA-2 pathways alongside a network of various other erythroid regulators for HbF activation such as MYB, BCL11A and MAPKs [12]. Much like variants in BCL11A, MYB and KLF-1 have been shown to be associated to Hb F levels in both HU-exposed and HU-naïve conditions [6, 12, 25, 26], we investigated whether variants at SAR1a could, be equally associated with Hb F level in HU-naïve patients. This is a possible limitation of this exploratory study, but equally strength for this novel investigation with results that have implications for future researches on therapy of SCD. Indeed, showing that variants at SAR1a are not associated in HbF regulation at steady state in SCD patients could be consider interesting; the findings provide further evidence of the complex nature of Hb F regulation, highlighting that steady-state genetic regulators of γ-globin expression are not necessarily best suited targets for therapeutic interventions, therefore suggesting widening of the search for drug-responsive targets for HbF activation.
Conclusion
The present study did not find any association between selected SNPs in the HU-inducible SAR1a promoter polymorphisms, and HbF among SCD patients from Cameroon. The findings provide further evidence of the complex nature of HbF regulation, highlighting that steady-state regulators of γ-globin expression are not necessarily best suited targets for therapeutic interventions, therefore suggesting widening of the search for drug-responsive targets for HbF activation. The results of this study also emphasize the genetic heterogeneity of populations of African ancestry affected by SCD, with regard to HbF-promoting loci, and the need to perform replication studies of key association findings in several SCD populations to fully capture their significance.
Abbreviations
- HbF:
-
hemoglobin F
- SCD:
-
sickle cell disease
- HU:
-
hydroxyurea
- GTP:
-
guanosine triphosphate
- SAR:
-
secretion-associated and RAS-related
- RFLP-PCR:
-
restriction fragment-length polymorphism polymerase chain reaction
- HBB:
-
hemoglobin beta
- SNP:
-
single nucleotide polymorphism
- BCL11A:
-
B-cell lymphoma/leukemia 11A
- HBS1L:
-
hemoglobin S-1 like translational protein
- MYB:
-
myeloblastosis protein family
- Giα/JNK/Jun:
-
mitogen-activated protein kinase pathway
- ADT:
-
alkaline denaturation test
- HPLC:
-
high performance liquid chromatography
- HWE:
-
Hardy–Weinberg equilibrium
- MAF:
-
minor allele frequency
- NIH:
-
National Institutes of Health
References
Labie D, Pagnier J, Lapoumeroulie C, Rouabhi F, Dunda-Belkhodja O, Chardin P, et al. Common haplotype dependency of high G gamma-globin gene expression and high Hb F levels in beta-thalassemia and sickle cell anemia patients. Proc Natl Acad Sci USA. 1985;82(7):2111–4.
Creary LE, Ulug P, Menzel S, McKenzie CA, Hanchard NA, Taylor V, et al. Genetic variation on chromosome 6 influences F cell levels in healthy individuals of African descent and HbF levels in sickle cell patients. PLoS ONE. 2009;4(1):e4218.
Menzel S, Garner C, Gut I, Matsuda F, Yamaguchi M, Heath S, et al. A QTL influencing F cell production maps to a gene encoding a zinc-finger protein on chromosome 2p15. Nat Genet. 2007;39(10):1197–9.
Thein SL, Menzel S, Lathrop M, Garner C. Control of fetal hemoglobin: new insights emerging from genomics and clinical implications. Hum Mol Genet. 2009;18(R2):R216–23.
Wonkam A, Bitoungui VJN, Vorster AA, Ramesar R, Cooper RS, Tayo B, et al. Association of variants at BCL11A and HBS1L-MYB with hemoglobin F and hospitalization rates among sickle cell patients in Cameroon. PLoS ONE. 2014;9(3):e92506.
Lettre G, Sankaran VG, Bezerra MA, Araujo AS, Uda M, Sanna S, et al. DNA polymorphisms at the BCL11A, HBS1L-MYB, and beta-globin loci associate with fetal hemoglobin levels and pain crises in sickle cell disease. Proc Natl Acad Sci USA. 2008;105(33):11869–74.
Makani J, Menzel S, Nkya S, Cox SE, Drasar E, Soka D, et al. Genetics of fetal hemoglobin in Tanzanian and British patients with sickle cell anemia. Blood. 2011;117(4):1390–2.
Bauer DE, Kamran SC, Lessard S, Xu J, Fujiwara Y, Lin C, et al. An erythroid enhancer of BCL11A subject to genetic variation determines fetal hemoglobin level. Science. 2013;342(6155):253–7.
Galarneau G, Palmer CD, Sankaran VG, Orkin SH, Hirschhorn JN, Lettre G. Fine-mapping at three loci known to affect fetal hemoglobin levels explains additional genetic variation. Nat Genet. 2010;42(12):1049–51.
Mtatiro SN, Mgaya J, Singh T, Mariki H, Rooks H, Soka D, et al. Genetic association of fetal-hemoglobin levels in individuals with sickle cell disease in Tanzania maps to conserved regulatory elements within the MYB core enhancer. BMC Med Genet. 2015;16(1):1.
Pule GD, Ngo Bitoungui VJ, Chetcha Chemegni B, Kengne AP, Antonarakis S, Wonkam A. Association between variants at BCL11A erythroid-specific enhancer and fetal hemoglobin levels among sickle cell disease patients in Cameroon: implications for future therapeutic interventions. OMICS. 2015;19(10):627–31.
Pule GD, Mowla S, Novitzky N, Wiysonge CS, Wonkam A. A systematic review of known mechanisms of hydroxyurea-induced fetal hemoglobin for treatment of sickle cell disease. Expert Rev Hematol. 2015;8(5):669–79.
Kumkhaek C, Taylor JG, Zhu J, Hoppe C, Kato GJ, Rodgers GP. Fetal haemoglobin response to hydroxycarbamide treatment and sar1a promoter polymorphisms in sickle cell anaemia. Br J Haematol. 2008;141(2):254–9.
Tang DC, Zhu J, Liu W, Chin K, Sun J, Chen L, et al. The hydroxyurea-induced small GTP-binding protein SAR modulates gamma-globin gene expression in human erythroid cells. Blood. 2005;106(9):3256–63.
Zhu J, Chin K, Aerbajinai W, Kumkhaek C, Li H, Rodgers GP. Hydroxyurea-inducible SAR1 gene acts through the Gialpha/JNK/Jun pathway to regulate gamma-globin expression. Blood. 2014;124(7):1146–56.
Saiki RK, Scharf S, Faloona F, Mullis KB, Horn GT, Erlich HA, et al. Enzymatic amplification of beta-globin genomic sequences and restriction site analysis for diagnosis of sickle cell anemia. Science. 1985;230(4732):1350–4.
Steinberg M, Lu Z, Nagel R, Venkataramani S, Milner P, Huey L, et al. Hematological effects of atypical and cameroon β-globin gene haplotypes in adult sickle cell anemia. Am J Hematol. 1998;59(2):121–6.
Bitoungui VJN, Pule GD, Hanchard N, Ngogang J, Wonkam A. Beta-globin gene haplotypes among cameroonians and review of the global distribution: is there a case for a single sickle mutation origin in Africa? OMICS. 2015;19(3):171–9.
Tan AS, Quah TC, Low PS, Chong SS. A rapid and reliable 7-deletion multiplex polymerase chain reaction assay for alpha-thalassemia. Blood. 2001;98(1):250–1.
Rumaney MB, Bitoungui VJN, Vorster AA, Ramesar R, Kengne AP, Ngogang J, et al. The co-inheritance of alpha-thalassemia and sickle cell anemia is associated with better hematological indices and lower consultations rate in Cameroonian patients and could improve their survival. PLoS ONE. 2014;9(6):e100516.
Sanchez-Mazas A, Poloni ES. Genetic diversity in Africa. eLS. 2008. doi:10.1002/9780470015902.a0020800.
Gurdasani D, Carstensen T, Tekola-Ayele F, Pagani L, Tachmazidou I, Hatzikotoulas K, et al. The African genome variation project shapes medical genetics in Africa. Nature. 2015;517(7534):327–32.
Shriner D, Kumkhaek C, Doumatey AP, Chen G, Bentley AR, Charles BA, et al. Evolutionary context for the association of γ-globin, serum uric acid, and hypertension in African Americans. BMC Med Genet. 2015;16(1):1.
Bryc K, Auton A, Nelson MR, Oksenberg JR, Hauser SL, Williams S, et al. Genome-wide patterns of population structure and admixture in West Africans and African Americans. Proc Natl Acad Sci USA. 2010;107(2):786–91.
Borg J, Papadopoulos P, Georgitsi M, Gutiérrez L, Grech G, Fanis P, et al. Haploinsufficiency for the erythroid transcription factor KLF1 causes hereditary persistence of fetal hemoglobin. Nat Genet. 2010;42:801–5.
Grieco AJ, Billett HH, Green NS, Driscoll MC, Bouhassira EE. Variation in Gamma-Globin expression before and after Induction with Hydroxyurea Associated with BCL11A, KLF1 and TAL1. PLoS ONE. 2015;10:e0129431.
Authors’ contributions
Conceived and designed the experiments: GP, AW. Performed the experiments: GP. Patient recruitment, sample and clinical data collection and processing: VJNB, BCC. Analysed the data: APK, AW. Contributed reagents/materials/analysis tools: VJNB, BCC, APK, AW. Wrote the paper: GP, AW. Revised and approved the manuscript: GP, VJNB, BCC, APK, AW. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank the Division of Human Genetics and the University of Cape Town.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Data will not be shared due to ongoing research and analysis.
Ethics approval and consent
Approval for the study was provided by the University of Cape Town, Faculty of Health Sciences Human Research Ethics Committee (HREC REF: 132/2010) and the National Ethical Committee Ministry of Public Health, Republic of Cameroon (No. 033/CNE/DNM/07). All participants gave informed and signed consent.
Funding
The molecular experiments of the study were funded by the National Health Laboratory Services (NHLS), South Africa; and the NIH, USA, Grant Number 1U01HG007459-01. The student’s bursary was provided by the Oppenheimer Memorial Trust, National Research Foundation, and FirstRand Laurie Dippenaar Scholarship, South Africa. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Pule, G.D., Bitoungui, V.J.N., Chemegni, B.C. et al. SAR1a promoter polymorphisms are not associated with fetal hemoglobin in patients with sickle cell disease from Cameroon. BMC Res Notes 10, 183 (2017). https://doi.org/10.1186/s13104-017-2502-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-017-2502-3