Abstract
Objective
Phase III clinical trials of the tumour necrosis factor inhibitors SB4, SB2, and SB5 (biosimilars to etanercept, infliximab, and adalimumab, respectively) have demonstrated efficacy in moderate-to-severe rheumatoid arthritis (RA). Data from these trials were used to identify baseline characteristics associated with radiographic progression and to build a matrix risk model for its prediction.
Methods
Patients with radiographic progression and baseline demographic and disease characteristic data were pooled across the 3 phase III studies of each biosimilar and its reference product. Baseline demographics and disease characteristics were evaluated for their relationship with radiographic progression (1-year mean change in mTSS > 0); 3 factors were selected based on strongest Pearson’s correlation coefficient with the change in modified Total Sharp Score. Univariate logistic regression was performed to assess the association between each baseline factor and the rate of radiographic progression, with subsequent matrix model development performed using multivariate logistic regression.
Results
A total of 1371 patients were included in the analysis, with a radiographic progression rate of 27.4%. The 3 baseline predictors of radiographic progression, based on Pearson’s correlation coefficient, were 28 swollen joint count (SJC28), C-reactive protein (CRP), and physician global assessment (PhGA). A matrix model showed that the predicted risk of radiographic progression was higher with the increased level of SJC28, CRP, and PhGA (P < 0.001).
Conclusions
In this pooled analysis of phase III clinical trial data of biosimilars for RA, identifiable baseline factors (SJC28, CRP, and PhGA) associated with radiographic progression were similar to those described in prior studies. Even though radiographic progression was minimal, a small number of patients who have increased SJC28, CRP, and PhGA at baseline should be closely monitored and follow treat-to-target approach.
Clinical trial registration numbers
EudraCT 2012-005026-30. Registered 30 April 2013, https://www.clinicaltrialsregister.eu/ctr-search/trial/2012-005026-30/results
EudraCT 2012-005733-37. Registered 10 July 2013, https://www.clinicaltrialsregister.eu/ctr-search/trial/2012-005733-37/results
EudraCT 2013-005013-13. Registered 01 April 2014, https://www.clinicaltrialsregister.eu/ctr-search/trial/2013-005013-13/results
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic disorder that causes clinical symptoms as well as structural joint damage leading to functional disability, poor quality of life, decreased work productivity, and substantial societal cost in terms of both direct and indirect costs [1,2,3,4,5]. Achievement of remission or low disease activity remains the overarching goal of therapy, regardless of whether patients have early or established RA, with therapeutic decisions guided by the extent of disease activity and prognostic factors [6,7,8]. Reducing joint damage progression, as visualised by radiographic changes, is important given its correlation with irreversible functional impairment [9, 10]. The biologic disease-modifying anti-rheumatic drugs (bDMARDs) etanercept, infliximab, and adalimumab are tumour necrosis factor (TNF) inhibitors for which RA is among their approved indications [11,12,13]. Randomised clinical trials of these agents in patients with RA have collectively and consistently demonstrated benefits with respect to reducing disease activity, inhibiting radiographic progression, and inducing clinical remission, with significant advantages for combination therapy versus monotherapy with methotrexate (MTX) or a TNF inhibitor alone [14,15,16,17,18,19,20,21,22,23,24]. Study extension data are also available and have demonstrated the long-term efficacy and safety of TNF inhibitors [25, 26].
Research efforts have identified baseline factors that are predictive of radiographic progression and provide clinical value for identifying patients who require intensive treatment and monitoring from the time of diagnosis. Prior studies of nonbiologic and bDMARDs have revealed certain baseline factors associated with radiographic progression, including baseline swollen joint count (SJC), C-reactive protein (CRP) level, erythrocyte sedimentation rate (ESR), rheumatoid factor (RF) and anti-citrullinated peptide antibody (ACPA) status, and the presence of erosions [27,28,29]. Disease activity, as evaluated by composite indices, has also been found to have a strong association with progression of joint damage [12, 14, 15, 30], though the use of bDMARDs may result in less radiographic progression than MTX alone across different disease activity spectrums [15, 31,32,33,34,35,36].
Risk factors for rapid radiographic progression have been identified in terms of a matrix risk model more than a decade ago [28] and since then have been confirmed [27, 29, 37]. However, these matrix models looked at the risk of patients who were either on placebo with conventional synthetic DMARDs (csDMARDs) like MTX as background therapy or on newly administered MTX and compared this with progression in patients treated with bDMARDs plus MTX. Because radiographic progression is quite intensive with csDMARDs or placebo and progression rates were much higher in earlier years [38], researchers primarily looked at rapid radiographic progression which was defined as an annual progression rate of ≥ 5 modified Sharp/van der Heijde score points per year [28, 29]. However, using this definition can be difficult for patients on anti-TNFs because only a small number of them have such large radiographic progression rates while on anti-TNFs, aside from less progression seen in recent years.
Several previous studies showed a blunted relationship between the progression of joint damage and clinical disease activity during the course of treatment with bDMARDs [15, 31,32,33,34,35,36], and it has not been clarified yet whether bDMARDs reduce or halt progression of damage irrespective of disease activity or there is still a strict relationship to clinical activity. Moreover, having no progression of joint damage is an important aspect, since it provides evidence for a full abrogation, and not just mitigation, of the structural aggressiveness of RA. In the present study, we used a large database collectively derived across the phase III clinical trials of biosimilars SB4, SB2, and SB5 and the reference products etanercept, infliximab, and adalimumab, thus encompassing 3 different TNF-inhibitors to look at whether there are baseline measures that reflect disease activity associated with radiographic progression.
Methods
Data sources
This is a pooled analysis of 3 phase III studies that compared the efficacy and safety of each biosimilar TNF inhibitor (SB4, SB2, and SB5) with its associated reference product (etanercept, infliximab, and adalimumab, respectively) [39,40,41]. All 3 clinical studies were multicentre, randomised, double-blind, and parallel-group in design and enrolled patients with moderately or severely active RA despite MTX treatment, conducted to evaluate the efficacy, pharmacokinetics, safety, and immunogenicity of the biosimilar in comparison with its reference product in these patients.
The methodologies of each of the 3 studies have been published in detail elsewhere [39,40,41]. The eligibility criteria for these 3 studies were similar, resulting in similar patient demographics across studies. In brief, patients were aged 18 to 75 years and had been diagnosed with RA (per American College of Rheumatology 1987 revised classification criteria, in accordance with the respective comparator trials performed with the original agents); all patients had a disease duration of ≥ 6 months, during which they had received MTX for ≥ 6 months and at a stable dosage for ≥ 4 weeks before screening or randomisation. Additional requirements included the presence of active disease as evidenced by ≥ 6 swollen joints and ≥ 6 tender joints and either ESR ≥ 28 mm/h or serum CRP level ≥ 1.0 mg/dL. No prior treatment with biologic agents was allowed.
Since the effects of all 3 TNF inhibitors on radiographic progression were similar and were also shown to be similar between originator and biosimilar TNF blockers [42,43,44], the data of all trial arms were pooled and included all patients who had baseline demographic and disease characteristic data available, as well as radiographic results at baseline and study end (week 52 for SB4/etanercept and SB5/adalimumab studies, week 54 for the SB2/infliximab study).
Data extraction
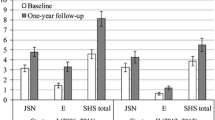
Structural joint damage was assessed from x-rays of both hands and feet. Radiographs were scored at week 0 and the final study week (week 52 for SB4/etanercept and SB5/adalimumab studies, week 54 for the SB2/infliximab study) using the modified Total Sharp Score (mTSS), the sum of the joint erosion score and the joint space narrowing score [45, 46]. X-rays from week 0 and the final study week were scored centrally by 2 independent qualified individuals under blinded conditions. The mean score for the change in mTSS from the 2 assessments was used for the analysis. Radiographic progression was defined as a 1-year mean change in mTSS > 0.
Data analysis
Patients with radiographic data, baseline demographics, and disease characteristics available from each study were pooled and analysed. The 3 individual baseline factors most associated with radiographic progression were identified based on those having the strongest Pearson’s correlation coefficient with the change in mTSS. Various demographic (e.g., age and sex) and disease characteristics (e.g., baseline SJC28, CRP, ESR, and RF positivity) were analysed (see Table 1 for complete list); composite scores (e.g., Simplified Disease Activity Index [SDAI], and Clinical Disease Activity Index [CDAI]) were also analysed, but not selected for baseline factors included in the matrix. We did not primarily employ Disease Activity Score in 28 joints [DAS28] by ESR, since this score should not anymore be used to define remission according to ACR-EULAR remission definitions and newer insights [47, 48]. Univariate logistic regression was performed to assess the association between each baseline factor and the proportion of patients with radiographic progression. Multivariate logistic regression was used to develop the matrix model of the 3 identified individual baseline factors to show the proportion of patients with radiographic progression in trichotomised cutoffs of each baseline factor.
In exploratory analyses, further multivariate logistic analyses were performed based on the identified 3 baseline factors using the same dataset to predict the proportion of patients in remission or low disease activity (LDA) by CDAI, SDAI, and DAS28 at week 24/30. Separate matrices were built on joint space narrowing and joint erosion score, subcomponents of mTSS, and for the proportion of patients with joint erosion score > 0 and joint space narrowing > 0 in trichotomised cutoffs of each baseline factor.
Results
Overall, the analysis included 1371 patients, 376 (27.4%) of whom experienced radiographic progression (> 0) with a mean change in mTSS of 0.41 (SD, 3.21). Of note, while on TNF inhibitor therapy, 121 (8.8%) patients had progression of mTSS ≥ 3. Baseline characteristics for all patients are displayed in Table 1. For all treatments combined, the mean age of participants was 51.4 years and most patients were female (81.7%). The mean duration of RA was 5.9 years, and mean mTSS was 37.9 at baseline. Based on Pearson’s correlation coefficient, the SJC28, CRP, and physician global assessment (PhGA) were determined to be significant baseline predictors of radiographic progression and used for further analysis (Table 1). DAS28, SDAI, and CDAI were also significant with P values < 0.05 (Table 1).
Although RF status (positive [> 14 kIU/L] vs negative) significantly correlated with the presence of radiographic changes (yes/no) (P = 0.002), it did not significantly correlate with the numerical change in mTSS, which was the measurement used to extract individual baseline factors that were most associated based on Pearson’s correlation coefficient (P = 0.7261).
The predicted risk of radiographic progression as a function of SJC28, CRP, and PhGA in the all treatments combined group is shown in Fig. 1a–c. Overall, as SJC28, CRP, and PhGA increased, the predicted risk of radiographic progression likewise increased. A similar pattern was shown for CDAI and SDAI (Supplementary Fig. 1A, B).
Development of the matrix risk model on radiographic progression (Fig. 2) showed that the 3 risk factors were associated with radiographic progression (P < 0.001). The predicted proportion of patients with radiographic progression tended to increase as the matrix moved from the lower to the higher range of each risk factor. As an example, the proportion of radiographic progressors (patients with the 1-year change in mTSS > 0) in the group with the highest cutoff value of SJC28, CRP, and PhGA was 40.7% (95% CI, 35.2%, 46.5%), whereas the proportion of radiographic progressors in the lowest cutoff value of SJC28, CRP, and PhGA was 15.5% (95% CI, 12.0%, 19.8%). In the matrix, CRP had a significant association with radiographic progression (P < 0.0001). P values for SJC28 and the PhGA were 0.139 and 0.140, respectively.
Matrix model of the proportion of patients with radiographic progression based on SJC28, CRP, and PhGA. Data are presented as % (95% confidence interval). Predicted probability of patients with radiographic progression represented by shading: green, < 22.0%; yellow, 22.0–32.0%; red, > 32.0%. CRP, C-reactive protein; SJC28, 28 swollen joint count; PhGA, physician global assessment; VAS, visual analogue scale
In the exploratory analysis, the matrix for the subcomponents of mTSS score was developed, and it showed that the predicted probability of patients with joint erosion score > 0 or joint space narrowing > 0 increased as each baseline factor worsened (Supplementary Fig. 2A, B). Additional analysis was done by disease activity, and the proportion of patients in remission or LDA by CDAI at week 24/30 tended to decrease with higher levels of baseline SJC28, CRP, and PhGA scores (Fig. 3). The proportion of patients in remission or LDA was 34.9% (95% CI, 29.0%, 41.3%) in the highest baseline cutoff value (SJC28 > 12, CRP > 11 mg/L, and PhGA > 80 mm) and 54.7% (95% CI, 47.8%, 61.4%) in the lowest baseline cutoff value (SJC28 < 8, CRP < 3.5 mg/L, and PhGA < 50 mm). Additionally, the proportion of patients in remission or LDA by the SDAI and DAS28 showed a similar pattern (Supplementary Fig. 3A, B). The total numbers of patients in each tertile of the 3 baseline factors in the matrix model are shown in Supplementary Fig. 4.
Matrix model of the proportion of patients in remission or low disease activity by CDAI at week 24/30 based on baseline SJC28, CRP, and PhGA. Data are presented as % (95% confidence interval). Predicted probability of patients in remission or low disease activity represented by shading: green, > 47.0%; yellow, 40.0–47.0%; red, < 40.0%. CDAI, Clinical Disease Activity Index; CRP, C-reactive protein; PhGA, physician global assessment; SJC28, 28 swollen joint count; VAS, visual analogue scale
Discussion
In this pooled study of 1371 patients from the SB4/etanercept, SB2/infliximab, and SB5/adalimumab phase III studies of biosimilars and originators for the treatment of RA, radiographic progression, although present, was minimal overall except a small proportion of patients with progression. Notably, studies involving conventional synthetic DMARDs have shown more significant radiographic progression [27,28,29]. Despite using higher mTSS cutoff values in those studies, the proportion of patients with radiographic progression was higher, which reflects the effectiveness of TNF inhibitors in slowing radiographic progression. Indeed, in previous studies, the effects on rapid radiographic progression were assessed [27,28,29], whereas in this study, we focused on prediction of any damage progression (mean change in mTSS > 0) on TNF inhibitors.
Overall, the findings of the current analyses were consistent with those from previous studies based on conventional DMARDs or reference biologics in identifying CRP levels and SJC28 as significant baseline factors associated with radiographic progression in patients receiving MTX or other csDMARDs [27,28,29, 37] while RF levels were not. The use of bDMARDs is known to blunt the correlation between the baseline disease activities and radiographic progression [15, 31,32,33, 35]. Nevertheless, we observed that baseline CDAI and SDAI still showed a relationship with the change in mTSS based on Pearson’s correlation coefficient (P value 0.004 for SDAI and 0.009 for CDAI) and predicted probability of patients with radiographic progression (yes/no) based on SDAI and CDAI (Supplementary Fig. 1A, B). This is in line with the data obtained from assessing the individual components of these composite measures, since it is postulated from our study that the correlation is due to CRP, SJC28, and to some extent also PhGA which is usually a reflection of SJC and CRP [49, 50]. However, the much stronger significance of the association between composite measures and radiographic progression compared with the individual variables once again confirms the advantage of assessing composite scores. Fautrel et al. sought to develop a predictive algorithm and matrix in patients with early RA initiating synthetic DMARD therapy using SJC, CRP level, RF or ACPA status, and the presence of typical RA erosions as predictors of radiographic progression that were applied in the final multivariate model [27]. Data from clinical trials in which some patients received infliximab were the first used in the development of risk models for rapid radiographic progression [28, 29]. More specifically, matrix modelling based on the ASPIRE study of MTX alone or with infliximab in MTX-naive early RA was developed using SJC28, RF, and either CRP or ESR (with the goal of making the model interchangeable from a clinical practice standpoint), with treatment arm as a dichotomous variable [28]. It showed a dramatic structural advantage of treating patients with a TNFi+MTX vs MTX alone regarding the risk of rapid radiographic progression. When that model was expanded to another study of infliximab (the ATTRACT study of continued MTX with infliximab or placebo in patients with active RA despite stable-dose MTX), the use of the combination was again associated with a low risk of rapid radiographic progression when patients were in the low or intermediate ranges of the baseline risk factors, with high risk limited to those patients at the highest baseline risk ranges. Unlike patients on combination therapy, for patients on MTX monotherapy, risk of rapid radiographic progression was high irrespective of baseline risk factors.
Subsequently, a matrix risk model developed in a post hoc analysis of the BeSt study (evaluating MTX-based therapy, including MTX plus infliximab, for recent-onset RA) confirmed these data by identifying baseline CRP level, RF/ACPA status, and in addition erosion score as independent factors for predicting rapid radiographic progression, defined as an increase in Sharp-van der Heijde score ≥ 5 after 1 year [29].
Thus, matrix modelling demonstrated risk reduction with initial combination therapy that included infliximab or prednisone relative to MTX monotherapy, establishing treatment choice as a main determinant of rapid radiographic progression. However, in contrast to these prior risk models that determined risk by treatment arm, the current analysis did not compare radiographic progression by product or between biosimilars and reference products.
The goal of our study was to determine if one could discern patients at risk for progression of joint damage while on TNF inhibitors, since joint damage is generally a sign of aggressive disease and high inflammatory propensity, especially if cumulative over time.
Therefore, we did not examine rapid radiographic progression, since it is primarily observed upon administration of conventional synthetic DMARDs or placebo. However, since the matrix model shows that TNF inhibitors cannot prevent progression in patients at high risk, such patients may have to receive another treatment than a TNF-blocker, given their significant progression on these drugs. The predicted model also showed that patients with high levels of SJC28, CRP, and PhGA at baseline also showed slightly increased risk of higher disease activity by CDAI at week 24/30. Based on this, one can infer that baseline characteristics have a relationship with radiographic progression and disease activity. This further supports the importance of the treat-to-target approach; if the treatment target of LDA is not met between weeks 12 to 24, advancing to the next line of therapy is recommended [7]. We also demonstrated an association between PhGA and radiographic progression in the setting of RA. In our study, RF levels were not found to be associated with the change in mTSS at 1-year and, therefore, it did not become part of the matrix model. This is likely explained by the fact that anti-TNF blunts the association between RF status and radiographic progression [51], unlike in the studies on conventional synthetic DMARDs. Of note, the presence of RF determines disease activity and, therefore, RF appears to primarily act via increasing inflammation [52,53,54]. The ACPA status was not available and not included in the analysis.
This analysis has several limitations. Most notably, the lack of a placebo or MTX monotherapy group in the phase III studies precludes prediction of radiographic progression in reference to no biologic treatment. Another limitation is that ACPA status was not obtained in the study. Additionally, although the phase III studies had similar designs, patient demographics, and disease characteristics, they were not primarily designed to be combined.
To identify baseline factors for patients on anti-TNFs, a more stringent definition of radiographic progression compared to previous matrix models [28, 29] was employed to reveal a halt, and not just a reduction of damage progression.
Conclusions
Our analysis of phase III clinical trials of biosimilars and reference products for RA identified baseline factors that were consistent with those identified for rapid radiographic progression in previous studies of csDMARD therapy in RA. This signifies that even though radiographic progression is minimal while on anti-TNF, a small proportion of patients still has significant progression, and clinicians should closely monitor patients who have high SJC28, CRP, and PhGA before treatment start whether they are started on csDMARDs or anti-TNFs.
Availability of data and materials
Upon request, and subject to certain criteria, conditions, and exceptions, Samsung Bioepis will provide access to individual de-identified participant data. The de-identified participant data will be made available to researchers whose proposals meet the research criteria and other conditions, and for which an exception does not apply. The proposals should be directed to the corresponding author. To gain access, data requestors must enter into a data access agreement with Samsung Bioepis.
References
Birnbaum H, Pike C, Kaufman R, Marynchenko M, Kidolezi Y, Cifaldi M. Societal cost of rheumatoid arthritis patients in the US. Curr Med Res Opin. 2010;26(1):77–90.
Cross M, Smith E, Hoy D, Carmona L, Wolfe F, Vos T, et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1316–22.
Matcham F, Scott IC, Rayner L, Hotopf M, Kingsley GH, Norton S, et al. The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: a systematic review and meta-analysis. Semin Arthritis Rheum. 2014;44(2):123–30.
van Vilsteren M, Boot CR, Knol DL, van Schaardenburg D, Voskuyl AE, Steenbeek R, et al. Productivity at work and quality of life in patients with rheumatoid arthritis. BMC Musculoskelet Disord. 2015;16:107.
Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: a review. JAMA. 2018;320(13):1360–72.
Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care Res (Hoboken). 2016;68(1):1–25.
Smolen JS, Landewe R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–77.
The National Collaborating Centre for Chronic Conditions. Rheumatoid arthritis: national clinical guideline for management and treatment in adults. London: Royal College of Physicians; 2018.
Aletaha D, Smolen J, Ward MM. Measuring function in rheumatoid arthritis: identifying reversible and irreversible components. Arthritis Rheum. 2006;54(9):2784–92.
Smolen JS, Aletaha D, Grisar JC, Stamm TA, Sharp JT. Estimation of a numerical value for joint damage-related physical disability in rheumatoid arthritis clinical trials. Ann Rheum Dis. 2010;69(6):1058–64.
Royaert S, Jansen J, da Silva DV, de Jesus Branco SM, Livingstone DS 3rd, Mustiga G, et al. Identification of candidate genes involved in Witches’ broom disease resistance in a segregating mapping population of Theobroma cacao L. in Brazil. BMC Genomics. 2016;17:107.
van Riel PL, Renskers L. The Disease Activity Score (DAS) and the Disease Activity Score using 28 joint counts (DAS28) in the management of rheumatoid arthritis. Clin Exp Rheumatol. 2016;34(5 Suppl 101):S40–s4.
Remicade® (infliximab). Full prescribing information. Horsham: Janssen Biotech, Inc.; 2018.
Smolen JS, Van Der Heijde DM, St Clair EW, Emery P, Bathon JM, Keystone E, et al. Predictors of joint damage in patients with early rheumatoid arthritis treated with high-dose methotrexate with or without concomitant infliximab: results from the ASPIRE trial. Arthritis Rheum. 2006;54(3):702–10.
Smolen JS, Han C, Bala M, Maini RN, Kalden JR, van der Heijde D, et al. Evidence of radiographic benefit of treatment with infliximab plus methotrexate in rheumatoid arthritis patients who had no clinical improvement: a detailed subanalysis of data from the anti-tumor necrosis factor trial in rheumatoid arthritis with concomitant therapy study. Arthritis Rheum. 2005;52(4):1020–30.
Breedveld FC, Weisman MH, Kavanaugh AF, Cohen SB, Pavelka K, van Vollenhoven R, et al. The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previous methotrexate treatment. Arthritis Rheum. 2006;54(1):26–37.
Emery P, Breedveld F, van der Heijde D, Ferraccioli G, Dougados M, Robertson D, et al. Two-year clinical and radiographic results with combination etanercept-methotrexate therapy versus monotherapy in early rheumatoid arthritis: a two-year, double-blind, randomized study. Arthritis Rheum. 2010;62(3):674–82.
Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens PJ, Hazes JM, et al. Clinical and radiographic outcomes of four different treatment strategies in patients with early rheumatoid arthritis (the BeSt study): a randomized, controlled trial. Arthritis Rheum. 2005;52(11):3381–90.
Keystone EC, Kavanaugh AF, Sharp JT, Tannenbaum H, Hua Y, Teoh LS, et al. Radiographic, clinical, and functional outcomes of treatment with adalimumab (a human anti-tumor necrosis factor monoclonal antibody) in patients with active rheumatoid arthritis receiving concomitant methotrexate therapy: a randomized, placebo-controlled, 52-week trial. Arthritis Rheum. 2004;50(5):1400–11.
Maini R, St Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT Study Group. Lancet (London). 1999;354(9194):1932–9.
Quinn MA, Conaghan PG, O'Connor PJ, Karim Z, Greenstein A, Brown A, et al. Very early treatment with infliximab in addition to methotrexate in early, poor-prognosis rheumatoid arthritis reduces magnetic resonance imaging evidence of synovitis and damage, with sustained benefit after infliximab withdrawal: results from a twelve-month randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52(1):27–35.
van der Heijde D, Klareskog L, Landewe R, Bruyn GA, Cantagrel A, Durez P, et al. Disease remission and sustained halting of radiographic progression with combination etanercept and methotrexate in patients with rheumatoid arthritis. Arthritis Rheum. 2007;56(12):3928–39.
Weinblatt ME, Keystone EC, Furst DE, Moreland LW, Weisman MH, Birbara CA, et al. Adalimumab, a fully human anti-tumor necrosis factor alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum. 2003;48(1):35–45.
Westhovens R, Yocum D, Han J, Berman A, Strusberg I, Geusens P, et al. The safety of infliximab, combined with background treatments, among patients with rheumatoid arthritis and various comorbidities: a large, randomized, placebo-controlled trial. Arthritis Rheum. 2006;54(4):1075–86.
Klareskog L, Gaubitz M, Rodriguez-Valverde V, Malaise M, Dougados M, Wajdula J, et al. Assessment of long-term safety and efficacy of etanercept in a 5-year extension study in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2011;29(2):238–47.
Weinblatt ME, Keystone EC, Furst DE, Kavanaugh AF, Chartash EK, Segurado OG. Long term efficacy and safety of adalimumab plus methotrexate in patients with rheumatoid arthritis: ARMADA 4 year extended study. Ann Rheum Dis. 2006;65(6):753–9.
Fautrel B, Granger B, Combe B, Saraux A, Guillemin F, Le Loet X. Matrix to predict rapid radiographic progression of early rheumatoid arthritis patients from the community treated with methotrexate or leflunomide: results from the ESPOIR cohort. Arthritis Res Ther. 2012;14(6):R249.
Vastesaeger N, Xu S, Aletaha D, St Clair EW, Smolen JS. A pilot risk model for the prediction of rapid radiographic progression in rheumatoid arthritis. Rheumatology (Oxford). 2009;48(9):1114–21.
Visser K, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Ronday HK, Seys PE, Kerstens PJ, et al. A matrix risk model for the prediction of rapid radiographic progression in patients with rheumatoid arthritis receiving different dynamic treatment strategies: post hoc analyses from the BeSt study. Ann Rheum Dis. 2010;69(7):1333–7.
van der Heijde DM, van't Hof MA, van Riel PL, van Leeuwen MA, van Rijswijk MH, van de Putte LB. Validity of single variables and composite indices for measuring disease activity in rheumatoid arthritis. Ann Rheum Dis. 1992;51(2):177–81.
Aletaha D, Alasti F, Smolen JS. Rituximab dissociates the tight link between disease activity and joint damage in rheumatoid arthritis patients. Ann Rheum Dis. 2013;72(1):7–12.
Smolen JS, Avila JC, Aletaha D. Tocilizumab inhibits progression of joint damage in rheumatoid arthritis irrespective of its anti-inflammatory effects: disassociation of the link between inflammation and destruction. Ann Rheum Dis. 2012;71(5):687–93.
Landewe R, van der Heijde D, Klareskog L, van Vollenhoven R, Fatenejad S. Disconnect between inflammation and joint destruction after treatment with etanercept plus methotrexate: results from the trial of etanercept and methotrexate with radiographic and patient outcomes. Arthritis Rheum. 2006;54(10):3119–25.
Smolen JS, Aletaha D. Challenges of predicting treatment response in patients with rheumatoid arthritis. Nat Clin Pract Rheumatol. 2005;1(2):62–3.
Smolen JS, Han C, van der Heijde DM, Emery P, Bathon JM, Keystone E, et al. Radiographic changes in rheumatoid arthritis patients attaining different disease activity states with methotrexate monotherapy and infliximab plus methotrexate: the impacts of remission and tumour necrosis factor blockade. Ann Rheum Dis. 2009;68(6):823–7.
Emery P, Genovese MC, van Vollenhoven R, Sharp JT, Patra K, Sasso EH. Less radiographic progression with adalimumab plus methotrexate versus methotrexate monotherapy across the spectrum of clinical response in early rheumatoid arthritis. J Rheumatol. 2009;36(7):1429–41.
Hambardzumyan K, Bolce R, Saevarsdottir S, Cruickshank SE, Sasso EH, Chernoff D, et al. Pretreatment multi-biomarker disease activity score and radiographic progression in early RA: results from the SWEFOT trial. Ann Rheum Dis. 2015;74(6):1102–9.
Rahman MU, Buchanan J, Doyle MK, Hsia EC, Gathany T, Parasuraman S, et al. Changes in patient characteristics in anti-tumour necrosis factor clinical trials for rheumatoid arthritis: results of an analysis of the literature over the past 16 years. Ann Rheum Dis. 2011;70(9):1631–40.
Emery P, Vencovsky J, Sylwestrzak A, Leszczynski P, Porawska W, Baranauskaite A, et al. A phase III randomised, double-blind, parallel-group study comparing SB4 with etanercept reference product in patients with active rheumatoid arthritis despite methotrexate therapy. Ann Rheum Dis. 2017;76(1):51–7.
Choe JY, Prodanovic N, Niebrzydowski J, Staykov I, Dokoupilova E, Baranauskaite A, et al. A randomised, double-blind, phase III study comparing SB2, an infliximab biosimilar, to the infliximab reference product Remicade in patients with moderate to severe rheumatoid arthritis despite methotrexate therapy. Ann Rheum Dis. 2017;76(1):58–64.
Weinblatt ME, Baranauskaite A, Niebrzydowski J, Dokoupilova E, Zielinska A, Jaworski J, et al. Phase III randomized study of SB5, an adalimumab biosimilar, versus reference adalimumab in patients with moderate-to-severe rheumatoid arthritis. Arthritis Rheumatol (Hoboken). 2018;70(1):40–8.
Smolen JS, Choe JY, Prodanovic N, Niebrzydowski J, Staykov I, Dokoupilova E, et al. Comparing biosimilar SB2 with reference infliximab after 54 weeks of a double-blind trial: clinical, structural and safety results. Rheumatology (Oxford). 2017;56(10):1771–9.
Weinblatt ME, Baranauskaite A, Dokoupilova E, Zielinska A, Jaworski J, Racewicz A, et al. Switching from reference adalimumab to SB5 (adalimumab biosimilar) in patients with rheumatoid arthritis: fifty-two-week phase III randomized study results. Arthritis Rheumatol (Hoboken). 2018;70(6):832–40.
Emery P, Vencovsky J, Sylwestrzak A, Leszczynski P, Porawska W, Baranauskaite A, et al. 52-week results of the phase 3 randomized study comparing SB4 with reference etanercept in patients with active rheumatoid arthritis. Rheumatology (Oxford). 2017;56(12):2093–101.
van der Heijde D. How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol. 2000;27(1):261–3.
van der Heijde D. How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol. 1999;26(3):743–5.
Aletaha D, Smolen JS. Remission in rheumatoid arthritis: missing objectives by using inadequate DAS28 targets. Nat Rev Rheumatol. 2019;15(11):633–4.
Felson DT, Smolen JS, Wells G, Zhang B, van Tuyl LH, Funovits J, et al. American College of Rheumatology/European League against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann Rheum Dis. 2011;70(3):404–13.
Kaneko Y, Kuwana M, Kondo H, Takeuchi T. Discordance in global assessments between patient and estimator in patients with newly diagnosed rheumatoid arthritis: associations with progressive joint destruction and functional impairment. J Rheumatol. 2014;41(6):1061–6.
Khan NA, Spencer HJ, Abda E, Aggarwal A, Alten R, Ancuta C, et al. Determinants of discordance in patients’ and physicians’ rating of rheumatoid arthritis disease activity. Arthritis Care Res (Hoboken). 2012;64(2):206–14.
Pavelka K, Gatterova J, Tegzova D, Jarosova K, Tomasova Studynkova J, Svobodnik A, et al. Radiographic progression of rheumatoid arthritis in patients from the Czech National Registry receiving infliximab treatment. Clin Exp Rheumatol. 2007;25(4):540–5.
Aletaha D, Alasti F, Smolen JS. Rheumatoid factor, not antibodies against citrullinated proteins, is associated with baseline disease activity in rheumatoid arthritis clinical trials. Arthritis Res Ther. 2015;17:229.
Sokolove J, Johnson DS, Lahey LJ, Wagner CA, Cheng D, Thiele GM, et al. Rheumatoid factor as a potentiator of anti-citrullinated protein antibody-mediated inflammation in rheumatoid arthritis. Arthritis Rheumatology (Hoboken). 2014;66(4):813–21.
Laurent L, Anquetil F, Clavel C, Ndongo-Thiam N, Offer G, Miossec P, et al. IgM rheumatoid factor amplifies the inflammatory response of macrophages induced by the rheumatoid arthritis-specific immune complexes containing anticitrullinated protein antibodies. Ann Rheum Dis. 2015;74(7):1425–31.
Acknowledgements
Editorial support for development of this manuscript was provided by Laurie Orloski, PharmD, for C4 MedSolutions, LLC (Yardley, PA), a CHC Group company, and funded by Samsung Bioepis.
Funding
This work was supported by Samsung Bioepis Co., Ltd.
Author information
Authors and Affiliations
Contributions
JS, YK, WY, PE, MW, EK, MG, GM, and JG contributed to the conception, design of the work, analysis, and interpretation of data. IB contributed to the design of work, acquisition of data, analysis, and interpretation of data. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Three studies included were conducted in compliance with the Declaration of Helsinki and Good Clinical Practice Guidelines established by the International Conference Harmonisation. All subjects provided written informed consent.
Consent for publication
Not applicable
Competing interests
Josef S. Smolen has received personal remuneration from AbbVie, Amgen, Astra-Zeneca, Astro, Bristol-Myers Squibb, Celgene, Celltrion, ILTOO, Janssen, Lilly, MSD, Novartis-Sandoz, Novo-Nordisk, Pfizer, Roche, Samsung, Sanofi, and UCB and research funding from AbbVie, Janssen, Lilly, Novartis-Sandoz, Pfizer, and Roche. Michael E. Weinblatt has received research funding from Bristol-Myers Squibb, Crescendo Bioscience, and Sanofi/Regeneron; has served as a consultant and/or advisory board member for AbbVie, Amgen, Bristol-Myers Squibb, Crescendo Bioscience, Corrona, GSK, Gilead, Lilly, Lycera, Merck, Novartis, Pfizer, Roche, Samsung Bioepis, and Set Point; and has financial interests/stock ownership in Lycera, Canfite, Scipher, and Vorso. Paul Emery has been a clinical trials investigator and advisor to Pfizer, MSD, AbbVie, Bristol-Myers Squibb, UCB, Roche, Novartis, Samsung, Sandoz, and Lilly and has received consulting fees from Bristol-Myers Squibb, AbbVie, Gilead, Pfizer, MSD, Novartis, Roche, and UCB; his employer has received research grants from AbbVie, Bristol-Myers Squibb, Pfizer, MSD, and Roche. Edward C. Keystone has received research funding from AbbVie, Amgen, Lilly, Gilead, Pfizer, PuraPharm, Sanofi, and Merck; has served as a consultant and/or advisory board member for AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celltrion, Crescendo Bioscience, Roche, Genentech, Gilead, Janssen, Lilly, Merck, Pfizer, Sandoz, Sanofi, and Samsung Bioepis; and has received speaker honoraria for Amgen, AbbVie, Bristol-Myers Squibb, Roche, Janssen, Merck, Pfizer, Sanofi, and UCB. Mark C. Genovese has received research funding from AbbVie and has received consulting fees from Samsung Bioepis, Merck, Abbvie, Amgen, and FKB. Gihyun Myung, Inyoung Baek, and Jeehoon Ghil are employees of Samsung Bioepis. Jung-Yoon Choe has no financial disclosures.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1 : Table S1.
Disease activity cut-off values. Fig. S1A. Predicted probability (with 95% confidence limits) of patients with radiographic progression (yes/no) based on CDAI. B. Predicted probability (with 95% confidence limits) of patients with radiographic progression (yes/no) based on SDAI. Fig. S2A. Matrix model of the proportion of patients with joint erosion score > 0 based on SJC28, CRP, and PhGA. Data are presented as % (95% confidence interval). Predicted probability of patients represented by shading: green, < 20.0%; yellow, 20.0–25.0%; red, > 25.0%. B. Matrix model of the proportion of patients with joint space narrowing > 0 based on SJC28, CRP, and PhGA. Data are presented as % (95% confidence interval). Predicted probability of patients represented by shading: green, < 15.0%; yellow, 15.0–21.0%; red, > 21.0%. Fig. S3A. Matrix model of the proportion of patients in remission or low disease activity by SDAI at week 24/30 based on SJC28, CRP, and PhGA. Data are presented as % (95% confidence interval). Predicted probability of patients in remission with low disease activity represented by shading: green, > 47.0%; yellow, 40.0–47.0%; red, < 40.0%. B. Matrix model of the proportion of patients in remission or with low disease activity by DAS28 at week 24/30 based on SJC28, CRP, and PhGA. Data are presented as % (95% confidence interval). Predicted probability of patients in remission with low disease activity represented by shading: green > 32.0%; yellow, 27.0–32.0%; red, < 27.0%. Fig. S4. Number of patients corresponding to each tertile of the 3 baseline factors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Smolen, J.S., Kang, Y., Yoo, WH. et al. Radiographic progression based on baseline characteristics from TNF inhibitor biosimilar studies in patients with rheumatoid arthritis. Arthritis Res Ther 22, 188 (2020). https://doi.org/10.1186/s13075-020-02267-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13075-020-02267-z