Abstract
Background
Early treatment with tranexamic acid may reduce deaths after traumatic brain injury (TBI). In mild and moderate TBI, there is a time to treatment interaction, with early treatment being most beneficial. Time to treatment was recorded by clinicians and is subject to error. Using monitoring data from the CRASH-3 trial, we examine the impact of errors in time to treatment on estimated treatment effects.
Methods
The CRASH-3 trial was a randomised trial of the effect of tranexamic acid on death and vascular occlusive events in 12,737 TBI patients. This analysis includes the 8107 patients with a Glasgow coma scale score of 9 to 15 since previous analyses showed that these patients benefit most from early treatment. Clinician-recorded time to treatment was checked against ambulance and hospital records for 1368/12,737 (11%) patients. Patients who died were preferentially selected for monitoring and we monitored 36% of head injury deaths. We describe measurement errors using Bland-Altman graphs. We model the effect of tranexamic acid on head injury death using logistic regression with a time-treatment interaction term. We use regression calibration, multiple imputation and Bayesian analysis to estimate the impact of time to treatment errors.
Results
Clinicians rounded times to the nearest half or full hour in 66% of cases. Monitored times were also rounded and were identical to clinician times in 63% of patients. Times were underestimated by an average of 9 min (95% CI − 85, 66). There was more variability between clinician-recorded and monitored times in low- and middle-income countries than in high-income countries. The treatment effect estimate at 1 h was greater for monitored times OR = 0.61 (95% CI 0.47, 0.81) than for clinician-recorded times OR = 0.63 (95% CI 0.48, 0.83). All three adjustment methods gave similar time to treatment interactions. For Bayesian methods, the treatment effect at 1 h was OR = 0.58 (95% CI 0.43, 0.78). Using monitored times increased the time-treatment interaction term from 1.15 (95% CI 1.03, 1.27) to 1.16 (95% CI 1.05, 1.28).
Conclusions
Accurate estimation of time from injury to treatment is challenging, particularly in low resource settings. Adjustment for known errors in time to treatment had minimal impact on the trial results.
Trial registration
ClinicalTrials.gov NCT01402882. Registered on 25 July 2011
Similar content being viewed by others
Introduction
In emergency situations, treatment effects may depend on the time delay between the acute event and administration of the trial intervention. The CRASH-3 trial [1] showed that in patients with mild and moderate head injuries, tranexamic acid treatment reduced head injury deaths. As in previous trials of tranexamic acid in life-threatening bleeding, there was a strong time to treatment (TTT) interaction. The CRASH-2 trial [2] examined the effects of tranexamic acid in bleeding trauma patients. The WOMAN trial [3] examined its effects in post-partum haemorrhage. Both trials showed that tranexamic acid reduces death from bleeding when given within 3 h of bleeding onset with no benefit when given after 3 h. An individual patient data meta-analysis [4] found that for every 15-min treatment delay, there was a 10% reduction in effectiveness.
The CRASH-3 trial was conducted in 175 hospitals in 29 countries. Many patients were recruited in countries without formal pre-hospital emergency medical services (e.g. ambulance systems) and patients were often taken to hospital by bystanders or family members in taxis or private vehicles. In these cases, the time of injury was not formally recorded and was estimated by a clinician based on the location of injury and approximate transport times. However, in low- and middle-income countries, patients are often taken to the nearest primary healthcare centre, where they receive basic first aid before transfer to a tertiary hospital. In these situations, estimating the time of injury using location of injury and transportation times can be highly inaccurate.
Random measurement error can bias estimates of regression coefficients, reducing the apparent association between an exposure and outcome [5, 6]. Error in clinician-recorded TTT could obscure or weaken the TTT interaction and this could have clinical implications. In clinical trials, risk-adapted approaches to monitoring include verifying a proportion of participants’ measurements to assess the extent and nature of any errors and to adjust the analysis if necessary [7]. We examined the impact of mismeasurement in clinician-recorded TTT on treatment effects. We used three established statistical methods to correct for mismeasurement in clinician-recorded TTT using a sample of monitored patients.
Methods
We examined data from the CRASH-3 trial, a randomised trial of the effect of tranexamic acid on death, disability and vascular occlusive events in 12,737 TBI patients. The inclusion criteria were: adults with TBI, who had a Glasgow coma scale score (GCS) ≤ 12 or any intracranial bleeding on CT scan and no significant extra-cranial bleeding. The primary outcome was head injury death within 28 days. Of the 12,737 patients randomised, clinician-recorded TTT was monitored for 1368 (11%) patients by comparing clinician-recorded times with those based on data from ambulance and hospital records.
In this analysis, we examine the effect of inaccuracy in TTT estimates in 8107 patients with mild and moderate head injury. In this population, there was evidence of benefit from tranexamic acid treatment and evidence of a time treatment interaction. Patients with mild to moderate TBI had a baseline GCS of 9 to 15, and of these, 456 (6%) were monitored. Patients who died were preferentially chosen for monitoring. Hospitals that recruited a larger number of patients were monitored by visit. Other hospitals were monitored by telephone. All patient details (including TTT, GCS, age and SBP) were checked.
We estimated odds ratios and 95% confidence intervals for the effect of tranexamic acid on head injury deaths according to TTT using a multivariable logistic regression model (1):
(Y = 1 is head injury death within 28 days, X is treatment (tranexamic acid = 1, placebo = 0), T is TTT in hours, A is age in years at the time of the acute event, GCS is Glasgow coma scale and SBP is systolic blood pressure in mmHg). We assume that clinician-recorded time is measured with error and that the monitored time more accurately reflects TTT.
Three methods (regression calibration, multiple imputation and a full Bayesian analysis) were used to adjust for mismeasurement in clinician-recorded time. Each required the following two steps,
-
1)
A model for the association between clinician-recorded and monitored time was estimated from the sample of patients who were monitored and
-
2)
This fitted model was used to impute a monitored time for the patients who were not in the monitoring sample.
Within this framework, monitored time was assumed to have a linear relationship with clinician time.
where e~N(0, σ2), TM is the monitored time and TC is the clinician-recorded time.
First, for regression calibration, model coefficients (Eq. 2) were estimated using the monitored data and used to predict times in the unmonitored population. Confidence intervals were calculated by bootstrapping. Second, we treated unmonitored patients as having missing data and used multiple imputation as described by Bartlett [8, 9]. Third, we examined the impact of measurement error in a full Bayesian model, in which monitored TTT for patients who are not monitored was treated as another parameter to be estimated. For all three methods, the effect of tranexamic acid on death within 28 days was estimated from the model in Eq. 1 based on the actual data for monitored patients and imputed values for unmonitored patients. Further details of the methods are given in the statistical methods section of the Additional file 1.
Results
Of the 8107 patients with mild and moderate head injury, 537 (7%) died from head injury within 28 days. Of the 456 monitored patients, 186 (41%) died from head injury within 28 days. Table 1 shows the characteristics of the included patients stratified by monitoring status. In 63% (287/456) of monitored patients, clinician-recorded times and monitored time were the same. Clinician-recorded times were less than monitored times for 28% (128/456) and more than monitored times for 9% (41/456) of monitored patients.
Figure 1 shows a histogram of clinician-recorded times. The most common TTT is at 2 h with the next most commonly occurring TTT’s being at 3 h, 2 h 30 min, 1 h and 4 h. There was strong digit preference with times rounded to half an hour in 20% and to the hour in 46% of patients. There was also strong digit preference in the monitored times with times rounded to half an hour in 21% and to the hour in 29% of patients (Additional file 1: Figure 1).
The mean difference between clinician-recorded and monitored TTT was − 9 min, indicating that clinicians were more likely to underestimate TTT on average. The differences ranged from the clinician-recorded time being 66 min larger to 85 min smaller than the monitored time (Additional file 1: Figure 2). Figure 2 shows Bland-Altman graphs of clinician-recorded versus monitored TTT by country income level. In low- and middle-income countries, the mean difference was − 10 min. The differences ranged from the clinician-recorded time being 74 min larger to 93 min smaller than the monitored time. In high-income countries, the mean difference was − 9 min. The differences ranged from the clinician-recorded time being 44 min larger to 61 min smaller than the monitored time. The standard deviation of the time difference was 38 min for all countries combined, 42 min in low- and middle-income countries and 27 min in high-income countries. There was strong evidence that this time difference variance was larger in low- and-middle compared to high-income countries (F318,136 = 2.52, p < 0.0001).
Bland-Atman graphs by country income level. The graph on the left is for low- and middle-income countries (N = 319, bias = − 10 min, upper limit of agreement = 74 min, lower limit of agreement = − 93 min). The graph on the right is for high-income countries (N = 137, bias = − 9 min, upper limit of agreement = 44 min, lower limit of agreement = − 61 min). The magnitude of the bias and the gap between the limits of agreement are larger in low- to middle-income compared to high-income countries
Using regression and assuming a linear relationship between monitored and clinician time (Eq. 2) R2 = 0.82.
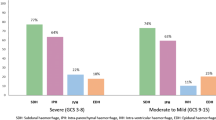
Table 2 and Fig. 4 show the ORs and 95% CIs for the effect of tranexamic acid by TTT based on clinician-recorded time, monitored time and after using the three statistical adjustment methods. The interaction term is larger when monitored times were used. The adjustment methods all give similar results in the CRASH-3 data and increase the time treatment interaction further.
Figure 3 shows the effect of tranexamic acid on head injury death by TTT (and provides a graphical representation of the first column of Table 2). The odds ratio for the treatment effect increases with time. There is a 10% reduction in treatment effectiveness for every 20-min increase in TTT (Fig. 3).
Discussion
In the CRASH-3 trial, clinicians often underestimated TTT with mismeasurement being greater in low- and middle-income countries than in high-income countries. Adjustment for known errors in TTT had little impact on the results although effect estimates were slightly larger. Our results suggest that early treatment with tranexamic acid might be even more important than previously reported.
We restricted our analysis to mild and moderately injured patients since there was a strong time treatment interaction in this subgroup. We excluded severely injured patients because there was no evidence of a time treatment interaction in these patients [1].
In over half of monitored patients, clinician-recorded and monitored times were identical. However, this does not mean that clinician-recorded times are accurate. For many patients, monitors had no additional information on which to base their assessments and so it is not surprising that the clinician-recorded times did not change after monitoring. There was strong digit preference in both clinician-recorded and monitored times which suggest inaccuracy in both sets of measurements. Time of treatment is usually recorded in the patient notes but the time of injury is often uncertain. In high-income countries, ambulance records often provide information on the approximate time of injury, but in low- and middle-income settings, these records are often absent. Accordingly, the variance of the difference between clinician-recorded and monitored TTT was larger in low- and middle-income compared to high-income countries. In low- and middle-income settings, time of injury was often estimated from bystander reports of the location of injury and estimated travel times to the treating hospital. However, because patients are often taken to the nearest healthcare centre before transfer to the randomising hospital, this method can lead to substantial underestimation of the time since injury.
It seems reasonable to assume that clinicians are more likely to underestimate than overestimate TTT. This assumption is consistent with the general psychological literature of time perception and with studies of time to treatment estimation in trauma patients [10,11,12,13,14]. In this study, clinician-recorded TTT was less than monitored TTT for 28% and more than monitored TTT for 9% of monitored individuals. It is well known that random mismeasurement of an exposure variable biases its apparent effect on the outcome variable towards zero [5, 6]. In the CRASH-3 trial, there was a small increase in treatment effect after adjustment for mismeasurement. Because we could not fully adjust for mismeasurement, it is likely that the treatment effect and particularly its interaction with TTT may be underestimated.
Accurate estimation of time to treatment is also important in stroke [15] and myocardial infarction [16] where treatment is only effective if given within a limited time window. In both of these areas, novel alternatives to patient reported times have been proposed [17, 18].
The three statistical methods, each of which assume a linear relationship between monitored and clinician time, gave similar results. Bartlett [19] found that the full Bayesian analysis gave more biased results than regression calibration for small effect sizes when the reliability of the imputation model was low. However, regression calibration can underestimate regression coefficients for large effect estimates [20]. Neither scenario is true for these data. Having 94% missingness is unusual when imputing missing data. However, in this case, we have a large number (456) of monitored times for reliable imputation. The large sample size and the large number of monitored values are important strengths of our study.
Of the three statistical adjustment methods, we found regression calibration the easiest to implement requiring only a small amount of non-standard code to estimate confidence intervals by bootstrapping. For MI and the full Bayesian analysis, a number of freely available software packages are available (for example JAGS [21], OpenBUGS [22], STAN [23], SMCFCS [24]). However, these packages are not routinely used by applied statisticians in trials units.
Conclusions
Randomised trials of potentially time critical treatments need to consider measurement error in estimated TTT. Validation studies may be necessary but identifying the gold standard measurement is challenging in acute settings.
Availability of data and materials
Following publication of the primary and secondary analyses detailed in the statistical analysis plan [25], individual de-identified patient data, including a data dictionary, will be made available via our data sharing portal, The Free Bank of Injury and Emergency Research Data (freeBIRD) website at https://ctu-app.lshtm.ac.uk/freebird/.
Abbreviations
- CRASH-2:
-
Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage
- CRASH-3:
-
Clinical Randomisation of an Antifibrinolytic in Significant Head injury
- GCS:
-
Glasgow coma scale score
- MI:
-
Multiple imputation
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure in mmHg
- TBI:
-
Traumatic brain injury
- TTT:
-
Time to treatment
- WOMAN:
-
World Maternal Antifibrinolytic
References
CRASH-3 Collaborators. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. Lancet. 2019. https://doi.org/10.1016/S0140-6736(19)32233-0.
CRASH-2 trial collaborators, Shakur H, Roberts I, Bautista R, Caballero J, Coats T, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH- 2): a randomised, placebo-controlled trial. Lancet. 2010;376:23–32.
Adeyemi B, Dallaku K, Idris H, Wangui R, Gul J, Jabeen K, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105–16.
Gayet-Ageron A, Prieto-Merino D, Ker K, Shakur H, Ageron FX, Roberts I, et al. Effect of treatment delay on the effectiveness and safety of antifibrinolytics in acute severe haemorrhage: a meta-analysis of individual patient-level data from 40138 bleeding patients. Lancet. 2018;391(10116):125–32.
Hutcheon JA, Chiolero A, Hanley JA. Random measurement error and regression dilution bias. BMJ. 2010;340(jun23 2):c2289. https://doi.org/10.1136/bmj.c2289.
Frost C, Thompson SG. Correcting for regression dilution bias: comparison of methods for a single predictor variable. J R Stat Soc Ser A Stat Soc. 2000;163(2):173–89.
European Medicines Agency: ICH E6 (R2) Good clinical practice. https://www.ema.europa.eu/en/ich-e6-r2-good-clinical-practice#current-version%2D%2D-revision-2-section Accessed 14 Feb 2020.
Bartlett JW, Seaman SR, White IR, et al. Multiple imputation of covariates by fully conditional specification: accommodating the substantive model. Stat Methods Med Res. 2015;24:462–87.
Bartlett JW, Keogh RH. SMCFCS: multiple imputation of covariates by substantive model compatible fully conditional specification, 2019. https://cran.r-project.org/package=smcfcs (Accessed 14 Feb 2020).
‘Vierordt’s law’. Wikipedia. 2020 Available at: https://en.wikipedia.org/wiki/Vierordt%27s_law (Accessed 25 May 2020).
Yarmey AD. Retrospective duration estimations for variant and invariant events in field situations. Appl Cogn Psychol. 2000;14(1):45–57.
Yarmey AD. Accuracy and confidence of duration estimates following questions containing marked and unmarked modifiers. J Appl Soc Psychol. 1990;20(14):1139–49. https://doi.org/10.1111/j.1559-1816.1990.tb00396.x.
Parker BT, Marco C. Emergency department length of stay: accuracy of patient estimates. West J Emerg Med. 2014;15(2):170–5.
Guo Y. Effect of time measurement error on assessing treatments with time dependent effect [Internet]. Vol. 01, MSc Thesis. 2017. Available from: http://hdl.handle.net/1773/40507.
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–35.
Newby K. Clinical outcomes according to time to treatment. Clin Cardiol. 1997;20(S3):11–5.
Wang D, Wang Y. Tissue window, not the time window, will guide acute stroke treatment. Stroke Vasc Neurol. 2019;4(1):1–2.
Mahmoud KD, Hillege HL, Jaffe AS, Lennon RJ, Holmes DR. Biochemical validation of patient-reported symptom onset time in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2015;8(6):778–87.
Bartlett JW, Keogh RH. Bayesian correction for covariate measurement error: a frequentist evaluation and comparison with regression calibration. Stat Methods Med Res. 2018;27(6):1695–708. https://doi.org/10.1177/0962280216667764.
Rosner B, Spiegelman D, Willett WC. Correction of logistic regression relative risk estimates and confidence intervals for measurement error: the case of multiple covariates measured with error. Am J Epidemiol. 1990;132(4):734–45. https://doi.org/10.1093/oxfordjournals.aje.a115715.
Plummer M (2003). JAGS: a program for analysis of Bayesian graphical models using Gibbs sampling, Proceedings of the 3rd International Workshop on Distributed Statistical Computing (DSC 2003), March 20–22, Vienna, Austria. ISSN 1609-395X.
Lunn D, Spiegelhalter D, Thomas A, Best N. The BUGS project: evolution, critique and future directions (with discussion). Stat Med. 2009;28:3049–82.
Stan Development Team 2018. Stan modelling language users guide and reference manual, version 2.18.0 http://mc-stanorg Accessed 14 Feb 2020.
Dewan Y, Komolafe EO, Mejia-Mantilla JH, et al. CRASH-3 - tranexamic acid for the treatment of significant traumatic brain injury: study protocol for an international randomized, double-blind, placebo-controlled trial. Trials. 2012;13:87.
Roberts I, Belli A, Brenner A, Chaudhri R, Fawole B, Harris T, et al. Tranexamic acid for significant traumatic brain injury (The CRASH-3 trial): statistical analysis plan for an international, randomised, double-blind, placebo-controlled trial. Wellcome Open Res. 2018;3:86.
Acknowledgements
The authors would like to thank all those involved in the CRASH-3 trial.
Funding
National Institute for Health Research Health Technology Assessment, JP Moulton Charitable Trust, Department of Health and Social Care, Department for International Development, Global Challenges Research Fund, Medical Research Council and Wellcome Trust (Joint Global Health Trials scheme). The funders of the study had no role in the study design, data collection, data analysis, data interpretation or writing of this manuscript.
Author information
Authors and Affiliations
Contributions
IR and HS-S conceived and designed the CRASH-3 trial. LF, HS-S and IR managed the monitoring process. IR came up with the original idea for this paper. RM and LS developed the concepts and conceived the analyses. RM conducted the analyses. RM, LS and IR interpreted the data and drafted the manuscript. LF and HS-S provided important feedback, revised the manuscript and contributed to the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Medical Research and Ethics Committee and Health Research Authority reviewed the protocol and supporting documents for the CRASH-3 trial and provided a favourable ethical opinion on 19 July 2012 (Research Ethics Committee Reference 12/EE/0274). The Medicines and Healthcare Products Regulatory Agency authorised the CRASH-3 trial on 8 August 2012 (Reference 17072/0007/001-0001). Favourable ethical opinion was received from the Observational/Interventions Research Ethics Committee at the London School of Hygiene and Tropical Medicine (LSHTM) on 17 November 2011 (Reference 6060). The Medical Research and Ethics Committee and Health Research Authority reviewed the protocol and supporting documents for the IBMS and provided a favourable ethical opinion on 8 June 2016 (Research Ethics Committee Reference 12/EE/0274). Favourable ethical opinion was received from the Observational/Interventions Research Ethics Committee at the London School of Hygiene and Tropical Medicine on 24 May 2016 (Reference 11535). Important protocol modifications to the CRASH-3 trial will be submitted to and reviewed by the Medicines and Healthcare Products Regulatory Agency, Medical Research and Ethics Committee and Health Research Authority, and registries updated as appropriate. All ethical approvals have been reviewed in in support of publication of the CRASH-3 trial protocol [24].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mansukhani, R., Frimley, L., Shakur-Still, H. et al. Accuracy of time to treatment estimates in the CRASH-3 clinical trial: impact on the trial results. Trials 21, 681 (2020). https://doi.org/10.1186/s13063-020-04623-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-020-04623-5