Abstract
Background
Hypertensive intracerebral haemorrhage (HICH) is the most common form of haemorrhagic stroke with the highest morbidity and mortality of all stroke types. The choice of surgical or conservative treatment for patients with HICH remains controversial. In recent years, minimally invasive surgeries, such as endoscopic evacuation and stereotactic aspiration, have been attempted for haematoma removal and offer promise. However, research evidence on the benefits of endoscopic evacuation or stereotactic aspiration is still insufficient.
Methods/design
A multicentre, randomised controlled trial will be conducted to compare the efficacy of endoscopic evacuation, stereotactic aspiration and craniotomy in the treatment of supratentorial HICH. About 1350 eligible patients from 10 neurosurgical centres will be randomly assigned to an endoscopic group, a stereotactic group and a craniotomy group at a 1:1:1 ratio. Randomisation is undertaken using a 24-h randomisation service accessed by telephone or the Internet. All patients will receive the corresponding surgery based on their grouping. They will be followed-up at 1, 3 and 6 months after surgery. The primary outcome is the modified Rankin Scale at 6-month follow-up. Secondary outcomes include: haematoma clearance rate; Glasgow Coma Scale 7 days after surgery; rebleeding rate; intracranial infection rate; hospitalisation time; mortality at 1 month and 3 months after surgery; the Barthel Index and the WHO quality of life at 3 months and 6 months after surgery.
Discussion
The trial aims to investigate whether endoscopic evacuation and stereotactic aspiration could improve the outcome of supratentorial HICH compared with craniotomy. The trial will help to determine the best surgical method for the treatment of supratentorial HICH.
Trial registration
ClinicalTrials.gov, ID: NCT02811614. Registered on 20 June 2016.
Similar content being viewed by others
Background
Hypertensive intracerebral haemorrhage (HICH) is a crucially important neurological emergency characterised by high fatality and disability rates. HICH accounts for about 70% of all intracerebral haemorrhage (ICH) cases. It affects about four million people worldwide each year and the median mortality at 1 month is 40% [1, 2]. Many survivors remain severely disabled, and only 12% of the survivors could live independently with minor handicap after 6 months, posing a huge burden on society and families [3, 4].
Theoretically, surgery has the potential to improve neurological recovery after ICH since early removal of the haematoma might reduce nerve tissue damage, possibly by relieving local ischemia or the removal of noxious chemicals [5,6,7]. However, the effectiveness of surgery (mainly refers to craniotomy) in the treatment of ICH remains controversial [8]. Several prospective randomised controlled trials (RCTs) have been undertaken during the past four decades, but the results of most individual trials have failed to demonstrate improvement in outcome in surgically treated patients [9,10,11,12,13,14,15]. Results of the International Surgical Trial in Intracerebral Haemorrhage (STICH) trial indicate that patients with spontaneous, supratentorial ICH in neurosurgical units show no overall benefit from early surgery when compared with initial conservative treatment [15]. The STICH II trial, a study based on subgroup analysis of the STICH trial, confirms that early surgery does not increase the rate of death or disability at 6 months and might have a small but clinically significant survival advantage for patients with spontaneous, superficial ICH [16].
Minimally invasive surgery generally refers to the concept of creating minimal trauma to normal brain tissue during the process of removing haematoma. This stands in distinction to open craniotomy in which a large bone flap is created, the brain is exposed, retracted and manipulated to inspect the site of bleeding, and blood is suctioned from multiple areas [5]. Two main types of minimally invasive surgery have been attempted for haematoma removal: endoscopic evacuation and stereotactic aspiration. In endoscopic evacuation, a small burr hole is created and an endoscope is inserted through normal brain tissue into the haematoma with the help of an introducer. Suction and irrigation are applied to remove the haematoma. Auer reported the first randomised trial of endoscopic-guided haemorrhage evacuation with a sample size of 100 [9]. Results indicated that endoscopic surgical evacuation offered promise as a means to maximise haematoma evacuation while minimising damage to normal tissue. Stereotactic aspiration involves using image guidance to place a catheter into the main body of the haematoma and aspirating blood. A catheter is left in the body of the haematoma, and during the course of several days, repeated small doses of thrombolytic agents are instilled via the catheter into the brain to clear the left haematoma slowly. Recently, several studies exploring the efficacy of minimally invasive surgery compared with craniotomy or medical treatment have been carried out, but none of them provided sufficient evidence regarding the choice of treatment [17,18,19,20]. Until now, no results of large-scale RCTs comparing the efficacy of endoscopic evacuation, stereotactic aspiration and craniotomy in patients with ICH have been reported. Here, we designed a multicentre, RCT to compare and verify the safety and efficacy of endoscopic evacuation and stereotactic aspiration.
Methods/design
Objectives
This trial primarily aims to investigate whether, and to what extent, endoscopic evacuation and stereotactic aspiration could improve the outcome of supratentorial HICH compared with craniotomy. This trial will also help to better define the indications for different surgical methods and help to determine the best surgical method for the treatment of supratentorial HICH. Another objective is to evaluate the separate effects of different surgical treatments on patients’ independency, activities of daily living, and quality of life.
Study design
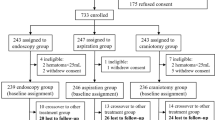
This is a multicentre, randomised controlled, open-label, sequentially designed nonprofit study (ClinicalTrials.gov ID: NCT02811614) involving 10 neurosurgical centres. Patients with newly diagnosed supratentorial HICH according to our inclusion criteria will be enrolled in this study. A follow-up period of 6 months will be sufficient to show the outcome and prognosis of surgical treatment. A flowchart of this study is shown in Fig. 1 and the Standard Protocol Items: Recommendations for Interventional Trials 2013 (SPIRIT) Checklist is presented as Additional file 1. The SPIRIT schedule of enrolment, interventions and assessment is given in Fig. 2.
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) figure: the schedule of enrolment, interventions and assessments. Abbreviations: h hour, mo month, mons months, GCS Glasgow Coma Scale, mRS modified Rankin Scale, WHOQOL the World Health Organisation Quality of Life questionnaire
The trial will be conducted in the departments of neurosurgery at 10 Chinese hospitals: (1) The Chinese PLA General Hospital, Beijing, (2) The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, (3) The First Hospital of Jilin University, Changchun, (4) The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, (5) The Second Hospital of Jilin University, Changchun, (6) Tianjin Huanhu Hospital, Tianjin, (7) Jinzhou Central Hospital, Jinzhou, (8) Jingzhou Central Hospital, Jingzhou, (9) Dalian Central Hospital, Dalian and (10) Wuhan Integrated TCM and Western Medicine Hospital, Wuhan. All surgeons taking part in the trial have been trained by an annually held national continuing education program by the Chinese PLA General Hospital on endoscopic evacuation and stereotactic aspiration. These three surgical techniques have been routinely used in all centres prior to the start of the trial. Patients who refuse surgery and patients from the Department of Neurology with matched basic clinical characteristics will be assigned to a group for future statistical analysis.
Eligibility criteria
Inclusion criteria
-
1.
Men and women aged 18–75 years old
-
2.
Presenting with supratentorial HICH confirmed by brain computed tomography (CT) scan, haematoma volume ≥30 mL
-
3.
Glasgow Coma Scale (GCS) score ≥5
-
4.
Patients are admitted to the above-mentioned hospitals within 24 h of ictus
-
5.
Patients or their dependents (when patients are in coma) provide written consent
Exclusion criteria
-
1.
The haemorrhage is caused by a cerebral tumor, coagulopathy, aneurysm or arteriovenous malformation
-
2.
If there is concurrent head injury or history of head injury
-
3.
If there are multiple hemorrhagic lesions
-
4.
Patients with severe dementia or disability
-
5.
Patients who already have indications of terminal brain herniation
-
6.
Patients with concomitant diseases that will affect their life expectancy
-
7.
Main body of the haematoma is located in the ventricular system
-
8.
Pregnant women
Sample size and randomisation
Sample size
It has been reported that the rate of poor outcome of patients receiving craniotomy with a supratentorial haematoma volume >30 mL was 49 to 67% and minimally invasive surgery might decrease the rate of poor outcome by about 8 to 22% compared with craniotomy [21,22,23]. Our recent retrospective study showed that endoscopic surgery lowered the risk of poor outcome in patients with supratentorial HICH by nearly 28% in comparison with craniotomy [24]. We assume that the neuroendoscopic surgery and stereotactic aspiration could reduce the risk of poor outcome from 58 to 49%. A sample size of 1230 would be required to show a 9% benefit from minimally invasive surgery (two-way P < 0.05) with 80% power. A sample size of 1350 (450 for each group) was chosen to allow for some loss to follow-up and a small crossover rate.
Randomisation
To minimise selection bias and accidental bias, patients will be randomised to an endoscopic evacuation group, a stereotactic aspiration group or a craniotomy group by means of central simple randomisation after the informed consent has been signed. Neither the neurosurgeons nor the patients could know the grouping beforehand. Randomisation will be performed using a web-based 24-h randomisation system. Randomisation must take place within 24 h of ictus and patients will be operated on within 12 h of randomisation. During the randomisation process the neurosurgeon is informed of the treatment group the patient is allocated to and should record this. Best medical treatment must begin as soon as possible and continue throughout follow-up in all patients.
Surgical procedures
Endoscopic evacuation
In this intervention group, patients will receive endoscopic surgery under general anesthesia. A 3-cm skin incision is made according to the position of the haematoma on brain CT scan. The approaches include the middle frontal gyrus approach for anterior basal ganglia haemorrhages that are not elongated but rather are more spherical; a parietooccipital burr hole is created to treat posterior basal ganglia and thalamic haemorrhages. In cases involving superficial lobar haemorrhages, a burr hole is used directly at the location where the lesion comes closest to the surface [25]. Then, a bone flap of about 2 cm in diameter is made and the dura mater incised in a cruciate fashion. Using a newly developed endoscopic introducer (China National Invention Patent: 201210066281.1) an appropriate working channel for the endoscope is made. First, the blunt puncturing lever is used to make an entry incision impaled in a predetermined position and then the inner core is removed. Second, syringe suction is used to determine whether the puncture lever has been positioned in the right place. After confirmation, the transparent cannula is placed outside along the puncture lever. Through the space made by the transparent introducer, we can carefully evacuate the intracerebral haematoma under endoscopic surveillance. Plasminogen activator (urokinase) will not be injected after endoscopic surgery.
Stereotactic aspiration
This group of patients will receive haematoma evacuation by stereotactic aspiration under local anesthesia and intravenous sedation. First, the patient will undergo a brain CT scan with slice thickness less than 5 mm and the CT imaging data in Digital Imaging and Communications in Medicine (DICOM) format will be collected. Then, the neurosurgeon will make a three-dimensional reconstructed image of haematoma using 3D Slicer version 4.5 software (http://www.slicer.org/; Harvard University, Boston, MA, USA) and measure the puncture depth from the puncture site to the target point. The target point is chosen on the CT scan with the largest expansion of the hematoma and special attention is paid to stay away from important cortical function areas. The puncture site is measured and marked on the head, then a puncture needle with a catheter is inserted to the premeasured depth. The hematoma will be withdrawn gently using a syringe (diluted with saline if the blood is thickened) until no more blood can be withdrawn. Urokinase will be injected through the catheter into the haematoma to dissolve the residual haematoma afterward. Three thousand to six thousand units urokinase will be injected into the haematoma two or three times daily for 2–4 days. A CT scan should be performed 24 and 72 h after surgery. The drilling catheter will be removed when more than 80% of the original haematoma volume has been removed or no more haematoma can be aspirated.
Craniotomy
Patients in this group will receive haematoma evacuation by craniotomy under general anesthesia. Well-trained neurosurgeons will decide the surgical approach according to haematoma location and size on CT scan. To minimise the damage to normal brain tissue, the operative incision should be made as small as possible. After removing the bone and incising the dura mater, the cortex is incised to reach the haematoma on the basis of protecting the functional cortical areas and blood vessels. The haematoma will be evacuated as much as possible with the help of an operative microscope. After careful hemostasis, the blood pressure should be moderately elevated to confirm that there has been no bleeding site. If the brain tissue swells significantly after haematoma evacuation, then the bone flap should be abandoned. A drainage catheter is left in the haematoma cavity and will be pulled out at 24–48 h after surgery. Urokinase will not be injected afterward.
Concomitant care and interventions
All patients will be cared for in a neurosurgical intensive care unit (NICU) until they are considered stable enough to move to an intermediate care or general unit. Neurological status will be monitored in the NICU using the GCS and hourly neurological evaluation which includes vital signs, level of consciousness and limb muscular strength.
Outcome measurements
The primary outcome of this study is the degree of disability estimated using the modified Rankin Scale (mRS) 6 months after ictus. A poor outcome is defined as death or dependency with a mRS of 3–6. Living patients’ independence in activities of daily lives and quality of life will be a highlight of this study. We will also measure patients’ quality of life and their performance in activities of daily living using the Barthel Index and the World Health Organisation (WHO) Quality of Life-BREF at 3- and 6-month follow-ups. Other clinical information that will also be measured include: haematoma clearance rate evaluated at 72 h after surgery, operation time, intraoperative blood loss, postoperative GCS score 7 days after surgery, rebleeding rate, days of NICU stay, intracranial infection rate during hospitalisation, 1-month mortality, 3-month mortality, and mRS scores at 3 months.
Data collection and follow-up
A Case report Form (CRF) with detailed record rules has been developed in order to ensure accurate data collection. Patients’ personal data are made anonymous and numbered by the system. A list of patient names and study numbers is kept in a separate file to ensure that patients’ confidentiality is maintained. Demographic, clinical and neurological data are recorded at the time of enrolment and throughout follow-ups. The filled CRFs should be sent to the trial secretary expeditiously.
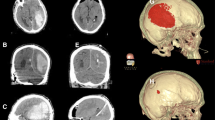
Copies of the CT scans at enrolment, 1 day, 3 days and 7 days after surgery will be sent to the trial secretary together with the CRFs. The preferred method of sending a CT scan is in DICOM-compatible format. DICOM images are sent anonymously with only the patient identifier visible. The images will be analysed by trained readers blinded to treatment group and patient identifier. In past studies, almost all haematoma volumes have been calculated by the ABC/2 formula. However, there is significant estimation error using the ABC/2 formula to calculate haematoma volume, especially in large, irregular haematomas [26]. In this trial, we will use a precise and free method, the software 3D Slicer, to measure both preoperative and postoperative haematoma volumes (Fig. 3).
Follow-up data will be collected at 1 month, 3 months and 6 months after onset. All patients are encouraged to make a regular return visit to the hospital. Patients who cannot make a regular return visit will be followed-up through telephone or postal questionnaires. Our goal is to achieve more than 95% follow-up by means of full cooperation of all the investigators.
Statistical analysis
Statistical analysis will be on a “intention-to-treat” basis. Measurement data will be described using mean and standard deviation or median and interquartile range, while count data will be described using indexes such as percentage, ratio and relative risk. The primary analysis will be a simple categorical frequency comparison using the chi-squared test for prognosis based on favourable and unfavourable outcomes at 6 months. The continuous variables will be analysed by one-way analysis of variance (ANOVA). Logistic regression analysis will be undertaken to adjust for covariates. Subgroup analyses include age, haematoma volume, haematoma location, time from ictus to surgery, GCS at hospitalisation, different centres, and the presence of an intraventricular haemorrhage, etc. All statistical analyses will be performed using SPSS statistics 22 (IBM Corp., Armonk, NY, USA). A value of two-side P < 0.05 was considered statistically significant.
Data monitoring and quality control
The Data Monitoring Committee considers data from interim analyses and reports to the Trial Steering Committee. Interim analyses are strictly confidential and the committee will only recommend stopping the trial early if one or other treatment shows an advantage at a very high significance level. The coordinating centre (Chinese PLA General Hospital, Beijing) is responsible for maintaining computerised databases containing all data related to the trial, the quality of computerised information, conducting statistical analyses, preparing reports for the Data Monitoring Committee, and all correspondence in relation to the trial. To better control the quality of this study, all neurosurgeons performing the operation will be given a short-term centralism training before the trial begins.
Discussion
ICH has always been a controversial topic in neurology and neurosurgery. Endoscopic evacuation and stereotactic aspiration have been investigated by comparison with conservative treatment or traditional craniotomy [9, 20, 27,28,29,30,31]. However, since most studies are nonrandomised and retrospective, the advantage of minimally invasive surgery remains unproven. Furthermore, the optimal timing of haematoma evacuation and the optimal time to maximum haematoma removal remains unclear. Endoscopic evacuation is a rapid process of haematoma volume reduction while stereotactic aspiration is a gradual process of haematoma volume reduction. It is still very difficult to select individualised treatment for each patient. By subgroup analyses of our large-scale multicentre RCT, we will try to find out the answers to these questions. Besides, with the improvement of living standards and the development of medical science, patients’ quality of life is attracting more and more attention. In this study we will make a study of quality of life in surviving HICH patients and investigate the factors that influence quality of life. Although it is controversial, surgical treatment still plays an important role in the management of HICH. Exploring a more efficient surgical method in order to improve clinical outcome and prognosis of HICH is essential and urgent. We hope that our findings may be of benefit to HICH patients and will provide further evidence for neurosurgeons and HICH patients when choosing surgical options.
Trial status
The trial was first designed in July 2016 and subject recruitment began in November 2016.
Abbreviations
- 3D:
-
Three-dimensional
- ANOVA:
-
Analysis of variance
- BI:
-
Barthel Index
- CRF:
-
Case Report Form
- CT:
-
Computed tomography
- DICOM:
-
Digital Imaging and Communications in Medicine
- GCS:
-
Glasgow Coma Scale
- HICH:
-
Hypertensive intracerebral haemorrhage
- IBM:
-
International Business Machine
- ICH:
-
Intracerebral haemorrhage
- IRB:
-
Institutional Review Board
- mRS:
-
Modified Rankin Scale
- NICU:
-
Neurosurgical intensive care unit
- PLA:
-
People’s Liberation Army
- SPSS:
-
Statistic Package for Social Science
- STICH:
-
International surgical trial in intracerebral haemorrhage
- WHO:
-
World Health Organisation
References
Feign VL, Lawes CMM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the 20th century. Lancet Neurol. 2003;2:43–53.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9:167–76.
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344:1450–60.
Weimar C, Kleine-Borgmann J. Epidemiology, prognosis and prevention of non-traumatic intracerebral hemorrhage. Curr Pharm Des. 2016 [Epub ahead of print].
Vespa PM, Martin N, Zuccarello M, Awad I, Hanley DF. Surgical trials in intracerebral hemorrhage. Stroke. 2013;44:S79–82.
Siddique MS, Fernandes HM, Arene NU, Wooldridge TD, Fenwick JD, Mendelow AD. Changes in cerebral blood flow as measured by HMPAO SPECT in patients following spontaneous intracerebral haemorrhage. Acta Neurochir Suppl. 2000;76:517–20.
Xi G, Keep RF, Hoff JT. Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol. 2006;5:53–63.
Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–60.
Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: a randomized study. J Neurosurg. 1989;70:530–5.
Batjer HH, Reisch JS, Allen BC, Plaizier LJ, Su CJ. Failure of surgery to improve outcome in hypertensive putaminal hemorrhage. A prospective randomized trial. Arch Neurol. 1990;47:1103–6.
Juvela S, Heiskanen O, Poranen A, Valtonen S, Kuurne T, Kaste M, et al. The treatment of spontaneous intracerebral hemorrhage. A prospective randomized trial of surgical and conservative treatment. J Neurosurg. 1989;70:755–8.
Morgenstern LB, Frankowski RF, Shedden P, Pasteur W, Grotta JC. Surgical treatment for intracerebral hemorrhage (STICH): a single-center, randomized clinical trial. Neurology. 1998;51:1359–63.
Zuccarello M, Brott T, Derex L, Kothari R, Sauerbeck L, Tew J, et al. Early surgical treatment for supratentorial intracerebral hemorrhage: a randomized feasibility study. Stroke. 1990;30:1833–9.
Teernstra O, Evers S, Lodder J, Leffers P, Franke CL, Blaauw G, et al. Stereotactic treatment of intracerebral hematoma by means of a plasminogen activator: a multicenter randomized controlled trial (SICHPA). Stroke. 2003;34:968–74.
Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005;365:387–97.
Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013;382:397–408.
Hattori N, Katayama Y, Maya Y, Gatherer A. Impact of stereotactic hematoma evacuation on activities of daily living during the chronic period following spontaneous putaminal hemorrhage: a randomized study. J Neurosurg. 2004;101:417–20.
Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016;15:1228–37.
Wang WZ, Jiang B, Liu HM, Li D, Lu CZ, Zhao YD, et al. Minimally invasive craniopuncture therapy vs. conservative treatment for spontaneous intracerebral hemorrhage: results from a randomized clinical trial in China. Int J Stroke. 2009;4:11–6.
Sun H, Liu H, Li D, Liu L, Yang J, Wang W. An effective treatment for cerebral hemorrhage: minimally invasive craniopuncture combined with urokinase infusion therapy. Neurol Res. 2010;32:371–7.
Zhou X, Chen J, Li Q, Ren G, Yao G, Liu M, et al. Minimally invasive surgery for spontaneous supratentorial intracerebral hemorrhage: a meta-analysis of randomized controlled trials. Stroke. 2012;43:2923–30.
Zhou H, Zhang Y, Liu L, Han X, Tao Y, Tang Y, et al. A prospective controlled study: minimally invasive stereotactic puncture therapy versus conventional craniotomy in the treatment of acute intracerebral hemorrhage. BMC Neurol. 2011;11:76.
Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Inao S, Wakabayashi T. Early recovery and better evacuation rate in neuroendoscopic surgery for spontaneous intracerebral hemorrhage using a multifunctional cannula: preliminary study in comparison with craniotomy. J Stroke Cerebrovasc Dis. 2011;20:208–13.
Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, et al. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage a comparison with craniotomy. J Neurosurg [epub ahead of print; 7 Apr 2017. doi: 10.3171/2016.10.JNS161589.]
Dye JA, Dusick JR, Lee DJ, Gonzalez NR, Martin NA. Frontal bur hole through an eyebrow incision for image-guided endoscopic evacuation of spontaneous intracerebral hemorrhage. J Neurosurg. 2012;117:767–73.
Xu XH, Chen XL, Zhang J, Zheng Y, Sun GC, Yu XG, et al. Comparison of the Tada formula with software slicer: precise and low-cost method for volume assessment of intracerebral hematoma. Stroke. 2014;45:3433–5.
Schaller C, Rodhe V, Meyer B, Hassler W. Stereotactic puncture and lysis of spontaneous intracerebral hemorrhage using recombinant tissue-plasminogen activator. Neurosurgery. 1995;36:328–35.
Rohde V, Rohde I, Thiex R, Ince A, Jung A, Dückers G, et al. Fibrinolysis therapy achieved with tissue plasminogen activator and aspiration of the liquefied clot after experimental intracerebral hemorrhage: rapid reduction in hematoma volume but intensification of delayed edema formation. J Neurosurg. 2002;97:954–62.
Barrett RJ, Hussain R, Coplin WM, Berry S, Keyl PM, Hanley DF, et al. Frameless stereotactic aspiration and thrombolysis of spontaneous intracerebral hemorrhage. Neurocrit Care. 2005;3:237–45.
Cho DY, Chen CC, Chang CS, Lee WY, Tso M. Endoscopic surgery for spontaneous basal ganglia hemorrhage: comparing endoscopic surgery, stereotactic aspiration, and craniotomy in noncomatose patients. Surg Neurol. 2006;65:547–55.
Nishihara T, Morita A, Teraoka A, Kirino T. Endoscopy-guided removal of spontaneous intracerebral hemorrhage: comparison with computer tomography-guided stereotactic evacuation. Childs Nerv Syst. 2007;23:677–83.
Acknowledgements
We would like to acknowledge all the participants in this work. Special thanks are to Ming Luo, Qiang Cai, Nu Zhang, Yunqian Li, Wei Yan, Wenming Guan, Jie Zhuo, Yanlong Yang and Jianhua Xiong, who actively participate in this project and offered their valuable time during the whole study.
Funding
This work was supported by the Science Technological Innovation Nursery Fund of the PLA General Hospital (grant number: 16KMM14).
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
XLC was the chief investigator and leads the trial. XHX and YZ contributed in developing and writing most of the protocol. FYL was responsible for the statistical analysis. HPZ and XG contributed to the conception and management of the trial. All authors participated in drafting and revising the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by a central ethics committee, the Institutional Review Board (IRB) of The Chinese PLA General Hospital (approval number: S2016-074-01). Any amendment will be submitted to the Local Ethics Committee. All participants will be told about the benefits, risks, rights and responsibilities of the trial and informed consent will be signed before enrolment.
Consent for publication
Not applicable. Once patients are recruited into the study, we will use numbers to represent patients’ names.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
SPIRIT Checklist. (PDF 83 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xu, X., Zheng, Y., Chen, X. et al. Comparison of endoscopic evacuation, stereotactic aspiration and craniotomy for the treatment of supratentorial hypertensive intracerebral haemorrhage: study protocol for a randomised controlled trial. Trials 18, 296 (2017). https://doi.org/10.1186/s13063-017-2041-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-017-2041-1