Abstract
Background
The clinical effectiveness of neurally adjusted ventilatory assist (NAVA) has yet to be demonstrated, and preliminary studies are required. The study aim was to assess the feasibility of a randomized controlled trial (RCT) of NAVA versus pressure support ventilation (PSV) in critically ill adults at risk of prolonged mechanical ventilation (MV).
Methods
An open-label, parallel, feasibility RCT (n = 78) in four ICUs of one university-affiliated hospital. The primary outcome was mode adherence (percentage of time adherent to assigned mode), and protocol compliance (binary—≥ 65% mode adherence). Secondary exploratory outcomes included ventilator-free days (VFDs), sedation, and mortality.
Results
In the 72 participants who commenced weaning, median (95% CI) mode adherence was 83.1% (64.0–97.1%) and 100% (100–100%), and protocol compliance was 66.7% (50.3–80.0%) and 100% (89.0–100.0%) in the NAVA and PSV groups respectively. Secondary outcomes indicated more VFDs to D28 (median difference 3.0 days, 95% CI 0.0–11.0; p = 0.04) and fewer in-hospital deaths (relative risk 0.5, 95% CI 0.2–0.9; p = 0.032) for NAVA. Although overall sedation was similar, Richmond Agitation and Sedation Scale (RASS) scores were closer to zero in NAVA compared to PSV (p = 0.020). No significant differences were observed in duration of MV, ICU or hospital stay, or ICU, D28, and D90 mortality.
Conclusions
This feasibility trial demonstrated good adherence to assigned ventilation mode and the ability to meet a priori protocol compliance criteria. Exploratory outcomes suggest some clinical benefit for NAVA compared to PSV. Clinical effectiveness trials of NAVA are potentially feasible and warranted.
Trial registration
ClinicalTrials.gov, NCT01826890. Registered 9 April 2013.
Similar content being viewed by others
Background
Neurally adjusted ventilatory assist (NAVA) uses electromyographic signals from the diaphragm (Edi) detected via a specialized naso-gastric feeding catheter (Getinge, Solna, Sweden), as a measure of neural respiratory drive and as a means of controlling the delivery of inspiratory support by a mechanical ventilator [1]. Over the last 12 years, studies have suggested several important physiological benefits associated with NAVA, including improved breath synchronization and effective assist that is proportional to neural respiratory drive [2, 3]. Studies have not yet, however, demonstrated improved patient outcomes as was originally suggested [1], with only two, relatively small trials finding non-statistically significant effects on secondary outcomes [3, 4].
Although there is a demand for adequately powered trials of NAVA [5], uncertainties remain in relation to its use over prolonged durations. Estimates of intervention adherence and protocol compliance provide critical information for the calculation of statistical power [6]. Randomized controlled clinical trials are expensive [7], and poor adherence risks a type II error, with an intervention deemed ineffective when it was actually not delivered with sufficient fidelity [8, 9]. Although good NAVA mode adherence was observed up to 48 h from randomization in a recent efficacy RCT [3], conflicting results were reported in a subsequent physiological RCT where NAVA failed in 7/20 (35%) participants across the same time period. To date, no trial has investigated adherence to a NAVA trial protocol beyond 48 h or determined the reasons for adherence or lack thereof.
The primary aim of this study was, therefore, to assess the feasibility of a trial protocol comparing NAVA to PSV, via an assessment of mode adherence. Our primary feasibility objectives were to assess mode adherence (proportion of time adherent to assigned mode) and protocol compliance (binary—≥ 65% mode adherence) during the entire study period. In contrast to previous trials, recruitment was commenced soon after intubation (ability to trigger the ventilator was not a requirement for inclusion), and the intervention was continued to the end of MV support or D28. In addition, reasons for mode cross-over and poor adherence were recorded. Some study results have been previously reported in the form of abstracts [10, 11].
Methods
An open-label, parallel-group, randomized feasibility trial was undertaken in four ICUs (surgical, general medical, neuro/trauma, and liver) comprising 75 beds at a university-affiliated hospital in London, UK. The trial was prospectively registered (NCT01826890) and was approved by the London Westminster ethics committee (13/LO/0012).
Participants
The inclusion criteria were as follows: adults receiving invasive MV with at least one of the following risk factors for prolonged MV [12]: (1) COPD, (2) heart failure (HF), or (3) acute respiratory distress syndrome (ARDS). Diagnoses by senior grade specialist physicians (respiratory, cardiac, intensivist) or by a non-specialist physician combined with either objective test results (spirometry, a CT scan, lung biopsy, cardiac echocardiogram) and/or prescribed treatment were required prior to enrolment (Additional file 1). The exclusion criteria were as follows: expected extubation, death, or treatment withdrawal within 48 h; > 96 h from intubation; > 24 h of spontaneously triggered ventilation mode support; suspected or proven hypoxic brain injury; high spinal injury; severe traumatic brain injury; neurological cause of ventilator dependency such as Guillain-Barré syndrome or Myasthenia Gravis; contraindication to nasogastric tube insertion; requirement for domiciliary ventilation; enrolment in any other interventional clinical trial; non-English speakers with inadequate translation available to allow informed consent; and pregnancy.
Research staff obtained informed consent from the participant’s legally authorized representative or proxy, and participant consent was sought once capacity was regained as required by the UK law [13].
Randomization
Using a 1:1 allocation ratio, treatment order was randomized with permuted blocks of random sizes using online randomization software, managed by an independent clinical trial unit [14]. The study intervention could not be blinded; treating clinicians, researchers, participants, families, and outcome assessors were aware of study group allocations.
Procedures
In the NAVA group, NAVA catheters were inserted within 4 h of randomization. Clinicians were instructed to record the maximum Edi hourly, to use the NAVA mode in place of PSV, and to target an Edi of ≥ 8 μV by adjustment of sedation dose and/or adjustment of MV settings where appropriate. A lower target level of 8 μV was set following basic analysis of existing literature and local audit data to avoid over-ventilation and over-sedation. NAVA parameters were set by clinicians according to a pragmatic protocol (Additional file 1), which involved matching hypothetical to actual pressure delivery (NAVA preview mode) and a brief period of observation to ensure stability. In the PSV group, ventilation settings were adjusted according to tidal volumes, clinicians were advised to review cycling criteria to optimize synchrony, and participants were otherwise ventilated according to local practice.
In both groups, protective tidal volumes of between 6 and 8 ml/kg of predicted body weight were recommended (Additional file 2, Table 4). Weaning guidelines included performing an assessment of readiness for a spontaneous mode, gradual stepwise reduction in ventilation support, sedation limitation according to Richmond Agitation and Sedation Scale (RASS) targets [16], and daily consideration of sedation holds and spontaneous breathing trials determined by the clinical team. Extubation readiness and practice were determined by clinicians. A full description of the weaning process is provided in Additional file 1. Study documents also guided troubleshooting of NAVA technical difficulties. The protocol was continued for up to 28 days from randomization.
Outcomes
The primary feasibility outcome was the proportion of MV time spent in assigned mode from randomization to extubation, death, or D28. Continuous MV (CMV) modes and CPAP were permitted in both groups, but no other exclusively spontaneously triggered modes were allowed. A priori, we considered a participant to be protocol compliant if mode adherence was ≥ 65% (binary) and the trial to be feasible if ≥ 65% of participants were compliant. Secondary feasibility outcomes were the proportion of participants with mode cross-over, duration of cross-over, reasons for cross-over, protocol acceptability (participant consent/physician refusal rates), and recruitment rates. Secondary exploratory outcomes included ventilator-free days (VFDs) to D28 and D90 and duration of MV from randomization; ICU, hospital, D28, and D90 mortality; ICU and hospital length-of-stay from randomization; mean RASS; and sedation dose and bolus dose frequency per infusion day. Safety outcomes included ventilator-associated pneumonia (VAP), pneumothoraxes, and incidence of unplanned extubation (Additional file 1).
Sample size and statistical analyses
Using 65% as the lower bound of the confidence interval (CI) (the minimum acceptable proportion to indicate trial feasibility) and an expected attrition of 5% (i.e. no NAVA or PSV weaning), a sample size of 76 patients (38 in each arm) would estimate a protocol compliance of 75% to within a 95% CI of ± 10% [17]. Descriptive statistics were used to characterize the sample. Categorical data were compared using chi-square or Fisher exact tests and continuous variables using Mann-Whitney or independent samples t tests as appropriate. Effect sizes are reported as median difference (MD) using the Hodges-Lehmann estimating method [15] for continuous variables, and as relative risk (RR) for binary data [18]. Effect estimates are reported with 95% CIs [18, 19]. Time to breathing without assistance and live ICU discharge are displayed using Kaplan-Meier curves with log-rank tests. A two-sided P value of < 0.05 was considered statistically significant. Analysis of clinical outcomes was exploratory and uncorrected for multiple comparisons; therefore, the statistically significant results could be due to chance. Qualitative descriptions of cross-over were categorized using content analysis [20]. Statistical analyses were performed using GraphPad Prism version 7.04 (GraphPad Software, La Jolla, CA, USA).
Results
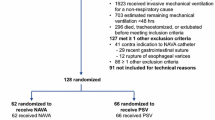
Over a 45-month enrolment period, 774 invasively ventilated patients with COPD, HF, or ARDS were identified, 112 eligible patients were approached, and 78 participants (39 NAVA and 39 PSV) were recruited, a consent rate of 72% (3 patients consented outside the recruitment window and were subsequently excluded) (Fig. 1). Baseline characteristics of the two groups were similar (Table 1) with good balance across groups for COPD (stratification factor), HF, and ARDS diagnoses. Median durations of MV in any mode and in PSV before randomization were similar (Table 1).
Feasibility outcomes
The average recruitment rate was 1.7 patients per month. Low rates of physician enrolment refusal (15 patients, 11.8%) (Fig. 1) suggests the trial was acceptable to clinical staff. Of the 78 randomized participants, one withdrew consent and five (three NAVA, two PSV) did not commence weaning and were excluded from the adherence analysis. In the 72 participants in whom weaning was attempted, median (95% CI) proportion of time in assigned ventilator mode from randomization to extubation, death, or D28 was 83.1% (64.0 to 97.1%) (NAVA) and 100% (100 to 100%) (PSV). Compliance, i.e. ≥ 65% adherence to assigned mode, was met in 82.2% (95% CI 71.7 to 89.4%) of all participants, 66.7% of NAVA participants (95% CI 50.3 to 80.0%), and 100% of PSV participants (95% CI 89.0 to 100.0%). Mode cross-over occurred in 28 (71.8%) NAVA and 3 (8.3%) PSV participants; the proportion of time cross-over from randomization to extubation, death, or D28 was 17.7% (95% CI 3.2 to 51.4%) and 0% (95% CI 0 to 0%) respectively (Table 2).
The main reasons for crossover in the NAVA arm were Edi signal noise or interference causing loss of synchrony (8/28, 22.2%), clinical team preference for use of PSV during deterioration or instability (7/28, 19.4%), lack of trial awareness (5/28, 3.6%), and clinical inexperience leading to delayed application of NAVA (4/28, 14.3%). The three cross-overs in the PSV arm were due to perceived ventilator dyssynchrony (Table 2).
Exploratory clinical outcomes
Median (IQR) VFDs to D28 were greater in NAVA with a median difference of 3.0 VFDs (95% CI to 0.011.0; p = 0.04), 15.5 VFDs in NAVA (0.0 to 23.0) compared to 0 VFDs (0.0 to 20.5) in PSV (Table 3). The median (IQR) time to first extubation was 3.7 days (1.9 to 4.9) (NAVA) versus 4.4 days (1.9 to 7.9) (PSV) (MD 1.0 day, 95% CI 0.8 to 3.0; p = 0.23). The overall median (IQR) duration of MV was 4.9 days (2.8 to 15.7) (NAVA) versus 9.8 days (3.6 to 25.9) (PSV) (MD 3.0 days, 95% CI 0.4 to 8.6; p = 0.13). Time to breathing without ventilator assistance and time to alive ICU discharge were shorter in NAVA (log-rank tests, p = 0.01 and p = 0.02 respectively, Fig. 2). Hospital mortality was lower in the NAVA group (9 deaths, 23.1%) compared to the PSV group (19 deaths, 50.0%) (RR 0.5, 95% CI 0.2 to 0.9; p = 0.032). No significant difference was observed in ICU mortality (8 deaths [20.5%] versus 15 deaths [39.5%]; p = 0.085), 28-day mortality (8 deaths [20.5%] versus 11 deaths [28.9%]; p = 0.44), and D90 mortality (9 deaths [24.3%] versus 17 deaths [44.7%]; p = 0.09) (Table 3) in the NAVA and PSV groups respectively (Table 3).
Kaplan-Meier estimates of probability of unassisted breathing and live discharge from ICU from randomization to D28. In keeping with previous trials [21, 22], unassisted breathing is defined as (1) extubated with supplemental oxygen or room air, or (2) open T-tube breathing, or (3) tracheostomy mask breathing, or (4) continuous positive airway pressure (CPAP) ≤ 5 cm H20 without pressure support and with no return to assisted breathing or death within 48 h. Participants receiving pressure support via non-invasive ventilation or CPAP > 5 cm H2O via any medium were defined as receiving assisted ventilation. NAVA = neurally adjusted ventilatory assist; PSV = pressure support ventilation
Mean hourly RASS scores were closer to zero in the NAVA mode (RASS recorded in NAVA mode in the NAVA arm: − 0.5 [− 1.6 to − 0.1], n = 33; compared to RASS recorded in PSV mode in the PSV arm: − 1.4 [− 2.5 to − 0.8], n = 35; MD − 0.8, 95% CI − 1.4 to − 0.1; p = 0.020), indicating less sedation while ventilated using NAVA (Table 4). However, no difference between the groups was observed in mean RASS while invasively ventilated including all modes, sedative, or analgesic infusion doses by infusion day, or in the mean number of bolus doses administered per day (Table 4). Incidence of VAP and self/unplanned extubation were similar between groups (Table 3). There were no other adverse events recorded suggesting the trial protocol was safe.
Discussion
This four ICU, single-centre, parallel group, RCT has demonstrated protocol feasibility by achieving acceptable adherence to the assigned mode and an acceptable proportion of compliant patients. The study has also demonstrated protocol acceptability by low rates of physician recruitment refusal and high participant consent rates and protocol safety via the absence of adverse events. Acknowledging the possibility of chance findings in this relatively small study, the exploratory clinical outcomes suggest increased VFDs, reduced time to breathing without assistance and reduced time to ICU discharge in the NAVA group, and improved sedation management while in the NAVA mode. These feasibility data improve our understanding of NAVA compared to PSV beyond 48 h of application, improving the chances of success in any subsequent trial. The clinical results are consistent with those reported by Demoule et al. [3] and suggest that a fully powered trial is justified.
Despite satisfactory mode adherence and protocol compliance across groups, these proportions were lower in the NAVA group, and substantial (albeit for a short duration) cross-over from NAVA was observed. Of the reported reasons for cross-over, human factors such as trial awareness, clinician preference, and lack of NAVA experience were most common, implying low confidence in the application of NAVA and need for further training. These issues may have been expected in a large group of clinical staff (over 300) despite attempts to embed NAVA technology into unit practice. This finding also highlights the complexity of NAVA and the likely variation in clinical application caused by ICU contexts and human interactions.
While the influence of human factors described above may be modified with increased/improved training and changes to study documents, of more concern for trial feasibility is the difficulty in acquiring and maintaining a satisfactory Edi signal, which occurred in 10 out of 36 (27.8%) NAVA participants. Edi signal problems have been reported previously. Di Mussi et al. reported NAVA mode failure in seven out of 20 patients (35%) due to loss of ‘Edi synchrony’ or low Edi activity, despite having obtained a reliable Edi signal at baseline [23]. Demoule et al. reported high levels of mode adherence across the first 48 h in NAVA (median 44.1 h [IQR 33 to 47.8]), but do not report on cross-over or its reasons. Recruitment after successful commencement of PSV in the study by Demoule et al. may be relevant. However, the reasons for the disparities between these trials and for the Edi difficulties described remain unclear. Varying levels of clinical expertise across a large staff group may be expected and relevant, but the results may also suggest limitations in NAVA technology (including anatomical abnormalities such as hiatal hernia) and/or a technical complexity in its clinical application over and above those associated with PSV. Notably, both trials were conducted in academic centres; therefore, these issues may be further magnified in non-academic centres with less experience of MV and NAVA.
In contrast to previous studies, the exploratory analysis of ventilation and clinical outcomes found potential benefit in the NAVA arm with increased VFDs to D28, decreased time to breathing without assistance and to alive ICU discharge, and reduced hospital mortality. Acknowledging the low power of these analyses, certain characteristics of our study that are different to previous studies may be relevant to the interpretation of these results. We specifically selected patients with risk factors for prolonged MV [12] and conditions where NAVA has potential physiological benefits [24,25,26]. In addition, Edi monitoring was used in the NAVA arm only, meaning the trial assessed the combined effects of monitoring and NAVA. Neural respiratory drive (Edi) monitoring is a potential advantage of NAVA [27] as it may encourage adjustment and improvement of ventilator settings, decrease sedative use, and expedite clinical assessment of weaning readiness. Clinical factors such as renal replacement therapy for example, which differed between the groups, or the lack of an extubation protocol, may also be of relevance to the results. Accepting the need for cautious interpretation, outcomes favouring NAVA are consistent with most published physiological data on NAVA and with trends toward superior clinical outcomes in two previous NAVA RCTs [3, 4]. As such, our findings strengthen the support of a future definitive, adequately powered RCT.
In addition to benefits in ventilation and clinical outcomes and despite no difference in sedation dose and RASS during in all MV modes, RASS scores were closer to zero in the NAVA mode compared to the PSV mode (p = 0.020), potentially indicating improved sedation management. Decreases in sedation may be driven by the need to optimise the Edi signal and ensure optimal levels of respiratory drive are present prior to the initiation of NAVA [28, 29]. Improved synchrony and patient comfort when in the NAVA mode may further reduce sedative requirements. Reduced sedation [30] and improved COMFORT scores [31,32,33] have been suggested in paediatric trials, but there are limited data available from adult studies. Demoule et al. [3] showed improved dyspnoea at day 1, but no overall difference in adaptation to intensive care environment (ATICE) comfort scores [34] in patients ventilated with NAVA versus PSV. Coisel et al. [35] found no difference in RASS in a small randomized cross-over study in 14 patients ventilated post-operatively. However, while sedation load and RASS outcomes may provide insight into the potential mechanisms underlying beneficial effects of NAVA, the individual clinical relevance and relative clinical value remain unclear.
Strengths and limitations
A key strength of this study is the description of mode adherence and reasons for poor adherence over prolonged durations. The use of a pragmatic protocol ensures that these adherence data are relevant to the real-world application of NAVA. The study successfully recruited patients at risk of prolonged MV, and treatment separation was improved due to the application of Edi monitoring in the NAVA arm only. While early recruitment during acute critical illness allowed assessment of Edi in CMV modes and NAVA from the very start of spontaneous breathing, it also led to the inclusion of some patients who did not commence weaning and potentially increased the rate of short-term NAVA failure during efforts to commence weaning.
Despite conducting the trial in four distinct units, the interpretation of the results and the degree to which the results are generalizable is limited due to its relatively small size and conduct at a single institution. As in the Demoule trial, the study site is an academic centre with relatively high levels of MV experience, which may limit the generalisability of results to less experienced centres. NAVA was introduced 5 years prior to the start of the trial in 2008; approximately 50% of staff were trained and 70% had clinical experience of NAVA. NAVA training and experience was similar across the four ICUs.
An analysis of ventilator synchronisation was beyond the scope of this study, and the absence of these data may further limit the interpretation of the exploratory outcomes. Improved synchrony in NAVA compared to PSV has, however, long been established [3, 4, 23, 28, 35,36,37,38,39,40,41], and dysynchrony is recognised as being associated with worse patient outcomes [42, 43]. As is common to many MV studies, blinding the clinical team was not possible. Outcome assessors and data analyses were also unblinded, although ventilator downloads verified objective outcomes, partially limiting the potential for bias.
A further potential source of error in the determination of NAVA compliance is the rate of automatic switching to PSV as a NAVA back-up mode, which was not possible to capture during the current trial. Although previous reports suggest levels of automatic switching to PSV of only 0.5 to 2% of total time in NAVA [3, 33], it remains a concern when considering the effect on clinical outcomes being attributed to NAVA ventilation in the current study.
As discussed above, NAVA is a complex intervention and its application will vary with human interactions and ICU context. Therefore, to enable interpretation of a multi-site trial a process, a process evaluation will be essential to determine whether the intervention was delivered as intended and to provide descriptive information relating to the research context [44].
Conclusions
This study is the first to our knowledge to report NAVA mode adherence rates beyond 48 h and reasons for cross-over, methodological evidence which is key to the success of future clinical trials. Together with the clinical benefit suggested in secondary outcomes, this study suggests that it is both feasible and justified to conduct a definitive randomized controlled trial to establish the effectiveness of NAVA in patients with a high likelihood of prolonged MV.
Availability of data and materials
The datasets generated analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- ARDS:
-
Acute respiratory distress syndrome
- CRRT:
-
Continuous renal replacement therapy
- CI:
-
Confidence interval
- CMV:
-
Continuous mandatory ventilation
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- Edi:
-
Electrical activity of the diaphragm
- HF:
-
Heart failure
- ICU:
-
Intensive care unit
- IQR:
-
Intra-quartile range
- MD:
-
Median difference
- MV:
-
Mechanical ventilation
- NAVA:
-
Neurally adjusted ventilatory assist
- PEEP:
-
Positive end expiratory pressure
- PSV:
-
Pressure support ventilation
- RASS:
-
Richmond Agitation and Sedation Scale
- RCT:
-
Randomised controlled trial
- RR:
-
Relative risk
- SD:
-
Standard deviation
- VAP:
-
Ventilator-associated pneumonia
- VFDs:
-
Ventilator-free days
References
Sinderby CN, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L. Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999;5(12):1433–6.
Colombo DC, Cammarota G, Bergamaschi V, De Lucia M, Della Corte F, Navalesi P. Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med. 2008;34(11):2010–8.
Demoule AC, Clavel M, Rolland-Debord C, Perbet S, Terzi N, Kouatchet A, Wallet F, Roze H, Vargas F, Guerin C, Dellamonica J, Jaber S, Brochard L, Similowski T. Neurally adjusted ventilatory assist as an alternative to pressure support ventilation in adults: a French multicentre randomized trial. Intensive Care Med. 2016;42(11):1723–32.
Kuo NYT, Tu ML, Hung TY, Liu SF, Chung YH, Lin MC, Wu CC. A randomized clinical trial of neurally adjusted ventilatory assist versus conventional weaning mode in patients with COPD and prolonged mechanical ventilation. Int J Chronic Obstr. 2016;11:945–51.
Terzi NP, Piquilloud L, Roze H, Mercat A, Lofaso F, Delisle S, Jolliet P, Sottiaux T, Tassaux D, Roesler J, Demoule A, Jaber S, Mancebo J, Brochard L, Richard JC. Clinical review: update on neurally adjusted ventilatory assist - report of a round-table conference. Crit Care. 2012;16(3):225.
Chan A-WT, Jennifer M, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, Hróbjartsson A, Mann H, Dickersin K, Berlin JA, Doré CJ, Parulekar WR, Summerskill WSM, Groves T, Schulz KF, Sox HC, Rockhold FW, Rennie D, Moher D. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Inter Med. 2013;158(3):200–7.
Thabane L, Lancaster G. Improving the efficiency of trials using innovative pilot designs: the next phase in the conduct and reporting of pilot and feasibility studies. Pilot Feasibility Stud. 2017;4:14.
Writing Group for the PReVENT Investigators. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS: a randomized clinical trial effect of low vs intermediate tidal volumes ventilation on patients without ARDS effect of low vs intermediate tidal volumes ventilation on patients without ARDS. JAMA. 2018;320(18):1872–80.
Shehabi Y, Howe BD, Bellomo R, Arabi YM, Bailey M, Bass FE, Bin Kadiman S, McArthur CJ, Murray L, Reade MC, et al. Early sedation with dexmedetomidine in critically ill patients. N Engl J Med. 2019;380(26):2506–17.
Hadfield D, Hopkins PA, Hart N, Reid F, Finney C, Penhaligon B, Molai J, Rafferty GF, King’s college hospital ACET research group: Neurally adjusted ventilatory assist versus pressure support in prolonged mechanical ventilation: a randomised feasibility study. Am J Respir Crit Care Med 2018, 197:A2551; A2104.
Hadfield D, Hopkins P, Hart N, Finney C, Penhaligon B, Molai J, Reid F, Rafferty G: ESICM LIVES 2018 : Paris, France. 20-24 October 2018. Intensive Care Med Exp 2018, 6(Suppl 2):40 (0052).
Boles JMB, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, Welte T. Weaning from mechanical ventilation. Eur Respir J. 2007;29(5):1033–56.
The Mental Capacity Act. In. London: HMSO; 2005.
King’s College London: King’s Clinical Trials Unit Online Randomisation Service v1.2. http://www.ctu.co.uk/. In. London; 2014.
Hodges JLL, Lehmann EL. Estimates of location based on rank-tests. Ann Math Stat. 1963;34(2):598 &.
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK. The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–44.
Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, Robson R, Thabane M, Giangregorio L, Goldsmith CH. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1.
Schulz KFA, Altman DG, Moher D. Consort Group: CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726–32.
Gardner MJA, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J (Clin Res Ed). 1986;292(6522):746–50.
Cole FL. Content analysis: process and application. Clin Nurse Spec. 1988;2(1):53–7.
National Heart L, Blood Institute Acute Respiratory Distress Syndrome Clinical Trials N, Matthay MA, Brower RG, Carson S, Douglas IS, Eisner M, Hite D, Holets S, Kallet RH, et al. Randomized, placebo-controlled clinical trial of an aerosolized β2-agonist for treatment of acute lung injury. Am J Respir Crit Care Med. 2011;184(5):561–8.
McAuley DF, Laffey JG, O'Kane CM, Perkins GD, Mullan B, Trinder TJ, Johnston P, Hopkins PA, Johnston AJ, McDowell C, et al. Simvastatin in the acute respiratory distress syndrome. N Engl J Med. 2014;371(18):1695–703.
Di Mussi RS, Spadaro S, Mirabella L, Volta CA, Serio G, Staffieri F, Dambrosio M, Cinnella G, Bruno F, Grasso S. Impact of prolonged assisted ventilation on diaphragmatic efficiency: NAVA versus PSV. Crit Care. 2016;20(1):1.
Liu LX, Xia F, Yang Y, Longhini F, Navalesi P, Beck J, Sinderby C, Qiu H. Neural versus pneumatic control of pressure support in patients with chronic obstructive pulmonary diseases at different levels of positive end expiratory pressure: a physiological study. Crit Care. 2015;19:244.
Berger DB, Bloechlinger S, Takala J, Sinderby C, Brander L. Heart-lung interactions during neurally adjusted ventilatory assist. Crit Care. 2014;18(5):499.
Doorduin JS, Sinderby CA, Beck J, van der Hoeven JG, Heunks LM. Assisted ventilation in patients with acute respiratory distress syndrome: lung-distending pressure and patient-ventilator interaction. Anesthesiology. 2015;123(1):181–90.
Goligher ECD, Douflé G, Fan E. Update in mechanical ventilation, sedation, and outcomes 2014. Am J Respir Crit Care Med. 2015;191(12):1367–73.
Vaschetto R, Cammarota G, Colombo D, Longhini F, Grossi F, Giovanniello A, Della Corte F, Navalesi P. Effects of propofol on patient-ventilator synchrony and interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit Care Med. 2014;42(1):74–82.
Skorko A, Hadfield D, Shah A, Hopkins P. Advances in ventilation - neurally adjusted ventilatory assist (NAVA). J Intensive Care Soc. 2013;14(4):317–23.
Kallio MP, Peltoniemi O, Anttila E, Pokka T, Kontiokari T. Neurally adjusted ventilatory assist (NAVA) in pediatric intensive care--a randomized controlled trial. Pediatr Pulmonol. 2015;50(1):55–62.
Ambuel B, Hamlett KW, Marx CM, Blumer JL. Assessing distress in pediatric intensive care environments: the COMFORT scale. J Pediatr Psychol. 1992;17(1):95–109.
de la Oliva P, Schüffelmann C, Gómez-Zamora A, Villar J, Kacmarek RM. Asynchrony, neural drive, ventilatory variability and COMFORT: NAVA versus pressure support in pediatric patients. A non-randomized cross-over trial. Intensive Care Med. 2012;38(5):838–46.
Piastra MDL, De Luca D, Costa R, Pizza A, De Sanctis R, Marzano L, Biasucci D, Visconti F, Conti G. Neurally adjusted ventilatory assist vs pressure support ventilation in infants recovering from severe acute respiratory distress syndrome: nested study. J Crit Care. 2014;29(2):312.e1-5.
De Jonghe B, Cook D, Griffith L, Appere-de-Vecchi C, Guyatt G, Theron V, Vagnerre A, Outin H. Adaptation to the Intensive Care Environment (ATICE): development and validation of a new sedation assessment instrument. Crit Care Med. 2003;31(9):2344–54.
Coisel YC, Chanques G, Jung B, Constantin JM, Capdevila X, Matecki S, Grasso S, Jaber S. Neurally adjusted ventilatory assist in critically ill postoperative patients: a crossover randomized study. Anesthesiology. 2010;113(4):925–35.
Mauri TB, Bellani G, Confalonieri A, Bombino M, Grasselli G, Foti G, Patroniti N, Pesenti A. Neurally adjusted ventilatory assist (NAVA) improves patient-ventilator interaction in severe ARDS patients undergoing ECMO. Am J Respir Crit Care Med. 2011;183:Meeting abstract p. A1710.
Moorhead KTP, Piquilloud L, Lambermont B, Roeseler J, Chiew YS, Chase JG, Revelly JP, Bialais E, Tassaux D, Laterre PF, Jolliet P, Sottiaux T, Desaive T. NAVA enhances tidal volume and diaphragmatic electro-myographic activity matching: a Range90 analysis of supply and demand. J Clin Monit Comput. 2013;27(1):61–70.
Patroniti NB, Bellani G, Saccavino E, Zanella A, Grasselli G, Isgro S, Milan M, Foti G, Pesenti A. Respiratory pattern during neurally adjusted ventilatory assist in acute respiratory failure patients. Intensive Care Med. 2012;38(2):230–9.
Piquilloud LV, Vignaux L, Bialais E, Roeseler J, Sottiaux T, Laterre PF, Jolliet P, Tassaux D. Neurally adjusted ventilatory assist improves patient-ventilator interaction. Intensive Care Med. 2011;37(2):263–71.
Schmidt MK, Kindler F, Cecchini J, Poitou T, Morawiec E, Persichini R, Similowski T, Demoule A. Neurally adjusted ventilatory assist and proportional assist ventilation both improve patient-ventilator interaction. Crit Care. 2015;19:56.
Spahija J, de Marchie M, Albert M, Bellemare P, Delisle S, Beck J, Sinderby C. Patient-ventilator interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit Care Med. 2010;38(2):518–26.
Thille AW, Cabello B, Galia F, Lyazidi A, Brochard L. Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med. 2008;34(8):1477–86.
de Wit MM, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK. Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med. 2009;37(10):2740–5.
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, Moore L, O'Cathain A, Tinati T, Wight D, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258.
Acknowledgements
The authors would like to thank the Anaesthetics, Critical Care, Emergency Medicine and Trauma (ACET) research team, the London Respiratory Muscle Research Group, and all staff within the Critical Care Units at King’s College Hospital for their support of this project.
Funding
This report is independent research supported by a National Institute for Health Research and Health Education England Clinical Doctoral Research Fellowship (D.J.H., CDRF-2014-05-056). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Additional funding was received from The Moulton Foundation and Guy’s and St Thomas’ Biomedical Research Centre. The funding sources had no role in the study design, data collection, analysis, interpretation, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
DJH, PAH, GFR, and NH obtained funding and contributed to the conception and design of the study. DJH was responsible for designing and revising study documentation, database management, and manuscript preparation. DJH, CF, BP, CH, SS, JS, LJ, JM, EC, LT, and HN undertook data acquisition. DJH, VC, and FR were responsible for the statistical plan and data analysis. DH, PAH, GFR, NH, LR, and FR revised the manuscript for important intellectual content. GFR and PAH contributed equally. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This trial was approved by London Westminster ethics committee (13/LO/0012). Informed consent was obtained from the participant’s legally authorized representative or proxy and from participants once capacity was regained.
Consent for publication
Not applicable.
Competing interests
D.J.H. has received funds from Maquet/Getinge to cover the travel, accommodation, and registration for conferences and meetings prior to 2016. All other authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Additional methods information.
Additional file 2.
Supplemental data tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hadfield, D.J., Rose, L., Reid, F. et al. Neurally adjusted ventilatory assist versus pressure support ventilation: a randomized controlled feasibility trial performed in patients at risk of prolonged mechanical ventilation. Crit Care 24, 220 (2020). https://doi.org/10.1186/s13054-020-02923-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-020-02923-5